Abstract
Orthognathic surgery treatment (OGS) after orthodontic treatment of dentofacial deformities is a widely performed procedure, often accompanied by a bilateral sagittal split osteotomy (BSSO). Positioning of the condyle during this procedure is a crucial step for achieving optimal functional and anatomical results. Intraoperatively poorly positioned condyles can have a negative effect on the postoperative result and the patient’s well-being. Changes of the condylar position during OGS Procedures and its effects on the temporomandibular joint in orthognathic surgical interventions (OGS) are subject of scientific discussions. However, up to date, no study has investigated the role of condyle position in the surgery first treatment concept. The aim of this study was to investigate the influence of OGS on the three-dimensional position of the condyle in the joint in a surgery first treatment concept without positioning device and to record the change in position quantitatively and qualitatively. Analysis of our data indicated that OGS in surgery first treatment concept has no significant effect on the position of the condyle and the anatomy of the temporomandibular joint.
Introduction
In patients with dentofacial deformities (DFD) and temporomandibular joint disorders (TMD), orthognathic surgery (OGS) is performed to improve masticatory function and aesthetics.
It is known, that orthognathic surgery affects the temporomandibular joint (TMJ); how DFD and TMD effect each other is still poorly understood and in the focus of research1,2.
A variety of studies have reported that temporomandibular joint (TMJ) or temporomandibular disk displacement causes skeletal Class II deformities as well as hyper-divergent facial deformities. These deformities are likely to progress with age3, and can even cause mandibular midline asymmetry1, if left untreated2,4,5.
Thus, the role of orthognathic surgery in DFD and TMD needs to be further investigated6–8 OGS procedures aim to resolve these issues by means of mono- or bimaxillary osteotomy of the facial skeleton accompanied by orthodontic treatment.
Only very few studies elucidate the long-term impact of orthognathic surgery on the temporomandibular joints’ structure and function9,10. Some authors postulate that mispositioning of the condyle after bilateral sagittal split osteotomy (BSSO) of the mandible leads to morphologic changes of the condyle, temporomandibular dysfunction or skeletal relapse11–14. A change in the position of the condyle may occur during surgery for any number of reasons. The recumbent position of the patient, paralysis of masticatory muscles due to anesthetization, joint edema, malalignment of bone ligaments, methods of positioning the condyle, and fixation methods can all lead to deviations in position of the condyle. It has been shown that our ability to reproduce condylar position even when no surgery is performed can be altered by patient position and relaxation of the masticatory muscles. Hence, numerous devices have been designed to maintain the preoperative position of the condyle during orthognathic surgery15,16.
Despite the rich literature and numerous disputes on the effects of orthognathic surgery especially regarding DFD/TMD, there are only a few reports that focus on the changes and symptoms of the condyle positions after orthognathic surgery. It is still unclear how orthognathic surgical procedures change the condylar position, and whether these changes vary significantly from the preoperative TMJ position14. Minor positional adjustments of the condyle can be characterized and quantified by three-dimensional imaging, including conventional fan-beam computed tomography (CT) or cone-beam computed tomography (CBCT)17.
This study aims to clarify if there are significant changes in condyle position after free hand repositioning of the condyle during OGS, since these changes may affect the function of the TMJ and impair masticatory function of the patients after surgery. We postulate that free hand repositioning does not alter the condyle position after surgery.
Materials and Methods
This prospective study was conducted after approval of the Ethics Committee of the Medical University of Vienna, Austria (1449/2013) and is in compliance with the Helsinki Declaration. Written, informed consent was obtained from all patients that were included in our study. The study was carried out on CT scans of patients >18 years of age, suffering from front open bite. The patients were operated between June 2013 and August 2014 at the Department of Oral and Maxillofacial Surgery of the Medical University of Vienna. All patients had undergone orthognathic surgery before orthodontic treatment, and all operations were conducted by an experienced surgeon. Maxillary treatment was performed doing a Le Fort I osteotomy, using four L-shaped mini-plates with four screws each for fixation. Mandibular treatment was done by the standard bilateral sagittal split osteotomy (BSSO) technique according to Hunsuck and Epker18,19. All condyle bearing segments were positioned free-hand without positioning devices, using three bicortical setscrews with lengths from 12 mm–16 mm for rigid fixation.
Data Collection
A CT scan of the skull (Philips Brilliance 64, Amsterdam, Holland; technical data see Table 1) was performed before surgery according to a standardized protocol with the patient in natural head position and gently biting in centric relation, resting his lips in a relaxed position. All data were saved in the Vienna General Hospital (Allgemeines Krankenhaus Wien, AKH) Picture Archiving Communication System (PACS), and later saved on a CD Rom for data analysis.
Table 1.
Technical data of CT Philips Brilliance® 64.
| Philips Brilliance® 64 | |
|---|---|
| Tube voltage (kV) | 80, 120, 140 kV |
| Tube current (mA) | 20–500 mA |
| Detector elements | 43.008 |
| Gantry opening | 700 mm |
| Gantry slope | −30/+30 increment 0.5 |
| Scan time | Up to 100 sec |
| Scan length | 1750 mm |
| Slice thickness | 0.55–7.5 mm |
| Rotation time | 0.4, 0.5, 0.75, 1, 1.5, 2 sec for 360° scans 0.28, 0.33 sec for 240° scans |
| pitch | 0.13–1.5 |
| collimation | 64 × 0.625 mm, 40 × 0.625 mm, 32 × 1.25 mm, 16 × 2.5 mm, 2 × 0.5 mm |
| Field of view (FOV) | 250 or 500 |
| Image/sec | 20 |
Each operation was performed according to a standardized protocol by two experienced surgeons using a traditionally fabricated surgical splint for guidance.
Six months after surgery, another CT scan was performed according to the protocol described in Table 1. The condyle position was evaluated bilaterally and compared with the postoperative CT with the program Slicer 3D (V.4.4.0 http://www.slicer.org/)20, reconstructing three-dimensional datasets for quantitative morphometric analysis.
Only bone kernel data visible to the human eye (Table 2) were used for reconstructing a raw data set of the mandible. Data were thresholded, thus Hounsfield Unit scale (HU) below 60 are projected in white color, and all parameters above 80 HU are projected in black color. Alterations of the TMJ were quantified by determining preoperative to postoperative differences between previously defined adjacent anatomical landmarks: F1(right), F1′(left)- most lateral point of the condyle, F2(right), F2′(left) - most anterior point of the condyle, F3 (right), F3′(left) - most medial point of the condyle, F4(right), F4′(left) - most posterior point of the Condyle. Then distance was measured between the most medial point of the condyles (F3-F3′) and between the most lateral point of the condyles (F1-F1′). In addition, the distance of both condylar longitudinal axes was calculated and the cutting angle between the axes (Intercondylar Angle) was calculated and measured. All measurements are in millimeters (mm), Angles are measured in degrees (see Fig. 1).
Table 2.
Exam parameters used for quantitative analysis.
| Tube voltage (kV) | 120–140 kV |
|---|---|
| Tube current (mAs) | 50–150 mAs |
| Slice thickness | 0.8–3 mm |
| increment | 0.4–3 mm |
| collimation | 64 × 0.625 |
| Dose-length product | 221.9–479.4 mGy cm |
Figure 1.
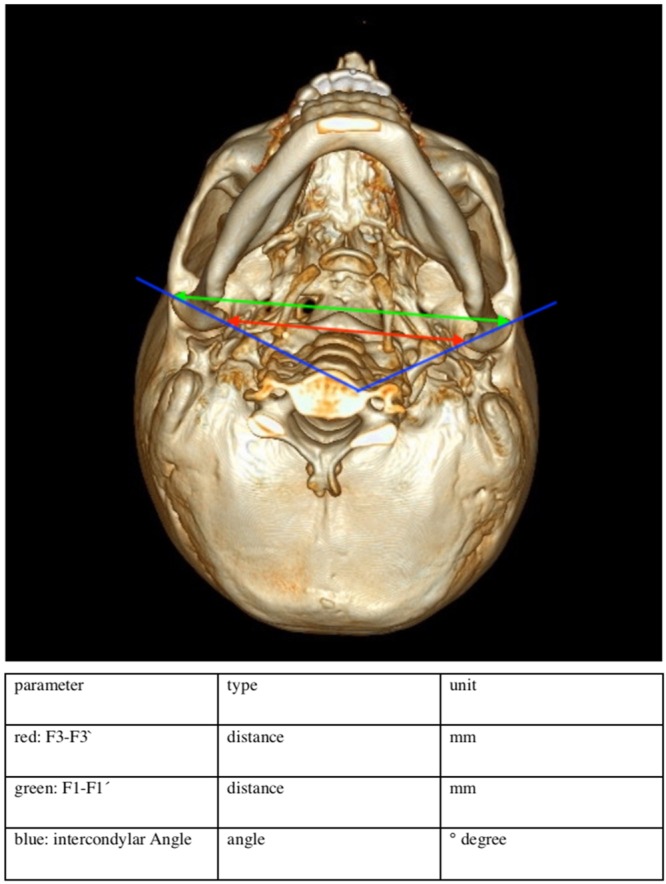
Variables assessed for quantitative morphological analysis.
CT Scans before and after surgery where analyzed according to these steps:
Importing pre, and postoperative DICOM to Slicer 4.4.0
Defining anatomical landmarks of the mandibular condyle
Conversion of all RAS (Right, Anterior, Superior) coordinates corresponding fiducial marks (F) and migration into a.csv data set.
Calculation of the differences with the open source statistical programming environment R 3.1.1(33).
Statistical Analysis
Descriptive statistics were used to summarize the clinical characteristics of the study cohort. Assessed variables were the intercondylar distance (F1 to F1′; F3 to F3′), and the position of the condyles before and after surgery by means of an angle measured between the left (Co si.) and the right condyle (Co dext.). All data where imported into MS Excel 15.6 for Mac from the Slicer 3D 4.4.0 program for statistic calculation.
We postulated that there is no significant difference in the condyle position after surgery. The position and the anatomical shape of the condyle where analyzed before and after surgery in a three-dimensional manner as described earlier. Then changes between the condylar position and condylar shape after surgery where analyzed and compared statistically. First, we performed a Shapiro Wilk Test to test whether the difference of the condyle position before and after surgery was within a standard distribution. If this was the case, we performed a paired t-test. If this was not the case, we performed a Wilcoxon-Mann-Whitney-Test. Statistical significance was defined as a two-sided p-value < 0.05. Statistical analysis of data was performed using the open source statistical programming environment R 3.1.121.
Results
A total of 16 patients with malocclusion who underwent orthognathic surgery met the eligibility criteria for this study.
All 16 patients were Caucasian aged 17–35, mean age 26,10 ± 5.1 years. Eight of them were women (aged 24.8 ± 5.3 ranging from 17.0 to 34.0 years) and eight were men (aged 27.3 ± 4.7 ranging from 22.2 to 35.7 years). There was no difference in age between men and women (Welch two sample t-test: −0.985, df = 13.723, p-value = 0.342).
14 patients with complex dysgnathia underwent bimaxillary treatment. Two patients underwent osteotomy of the maxilla only. Mandibular retrognathism was diagnosed in 11 patients (6 female, 5 male), demanding surgical advancement of the mandible. Five patients (2 female, 3 male) were diagnosed with mandibular prognathism and underwent a mandibular setback operation. Three patients underwent an additional genioplasty.
Analysis revealed no significant differences of the inter-condyle angle between bimaxillary and LeFort I osteotomy patients: Bimaxillary osteotomy patients showed an inter-condyle angle change of 3.3° ± 7.7 whereas LeFort I osteotomy patients showed an inter-condyle angle change of 2.8° ± 3.6. LeFort I osteotomy in comparison to bimaxillary osteotomy and mandibular set-back in comparison to mandibular advancement did not account for significant differences of inter-condyle angle change (see Table 3).
Table 3.
Analysis of Variance of inter-condyle angle change (=postoperative intercondyle angle - preoperative intercondyle angle). Le Fort only and Angle class III vs. II were tested as factors.
| Response: Inter-condyle angle change | Df | Sum Sq | Mean Sq | F value | Pr(>F) |
|---|---|---|---|---|---|
| Le Fort | 1 | 0.41 | 0.405 | 0.0072 | 0.9337 |
| Angle Class III vs II | 1 | 47.59 | 47.590 | 0.8453 | 0.3746 |
| Residuals | 13 | 731.91 | 56.301 |
Df: Degrees of freedom, Sum Sq: Sum of Squares, Mean Sq: Mean Square, F value: F-Statistic, Pr(>F): p-value.
Inter- and extra-condylar distance
Distance between the most medial points of both condyles was measured before and after surgery to evaluate whether the inter-condylar distance was affected by the operation. The mean intercondylar distance was 79.0 mm before and 80.4 mm after surgery (see Fig. 2).
Figure 2.
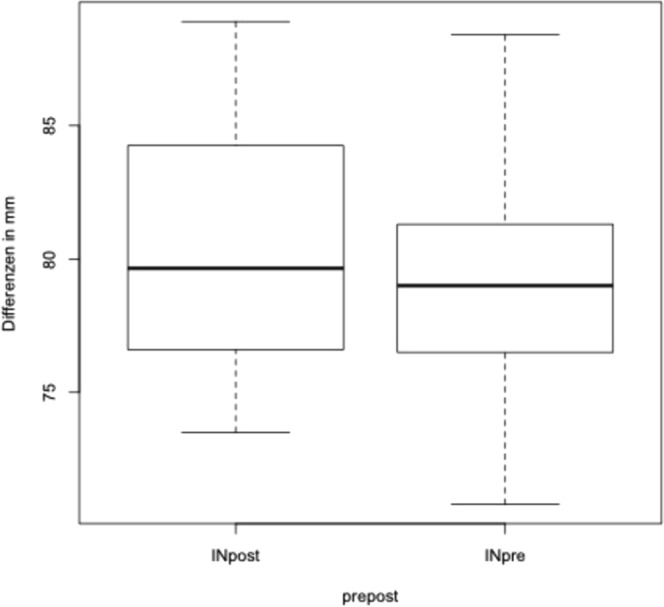
Analysis of changes of the intra condylar distance before and after surgery.
We performed the same calculation for the most lateral points of the condyles; the mean distance was 114.3 mm before, and 115.6 mm after surgery (see Fig. 3). The Shapiro Wilk test revealed that distances were not within a standard distribution (p = 0.0022). The paired T-test did not confirm significant changes between the distance of the lateral condyle position (p = 0.2114).
Figure 3.
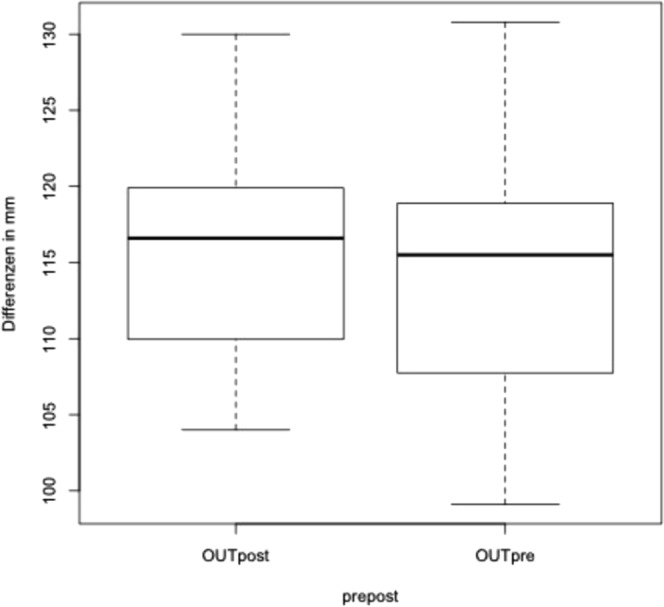
Analysis of changes of the extra condylar distance before and after surgery.
The angle between the condyles was measured at the crossing of the lines along the longitudinal axis of the condyle. The mean angle was 146.0 ± 14.8° before and 142.7 ± 16.0° after surgery (see Fig. 4). Since the inter-condylar angle did not follow a standard distribution (Shapiro-Wilk normality test: W = 0.90758, p-value = 0.0097). The angular change was compared pairwise before and after surgery, using a paired Wilcox signed rank test. The paired Wilcoxon signed rank test did not confirm significant changes between the angle of the lateral condyles before and after osteotomy (paired Wilcoxon signed rank test: V = 93, p = 0.2114).
Figure 4.
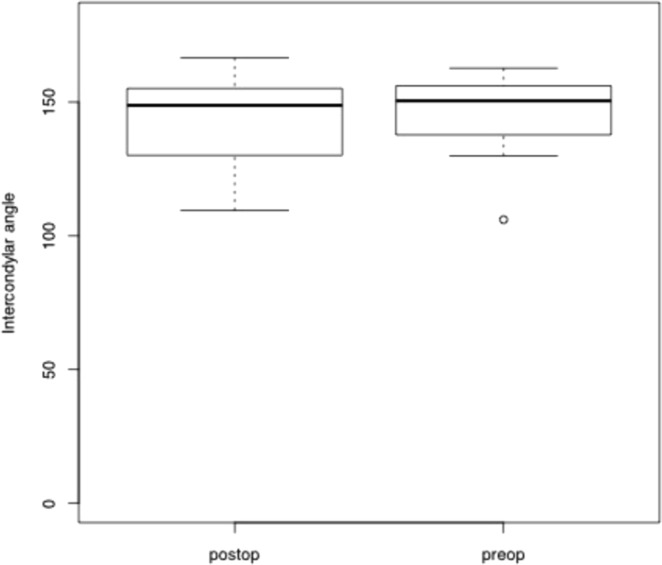
Analysis of changes of the intercondylar angle before and after surgery.
Discussion
The mechanisms underlying the correlation between pre- and postoperative condylar position changes have not been clarified yet. Hence, the aim of the present study was to examine the positional changes of the condyles in a group of 16 uniformly treated DFD patients with a follow-up of six months.
Numerous studies have shown that the amount of change in condyle position varies in each individual and is influenced by numerous factors, such as surgical procedure, experience of the surgeon and patient anatomy3,10,14,15,22. In the present study however, no significant changes in the position of the condyle were measured six months after surgery. Our findings are supported by Tabrizi et al., who observed that the distance of the condyle to the superior in the external auditory meatus in the coronal plane underwent significant movements compared to the preoperative position on both sides. Furthermore, they found that the condyle was displaced inferiorly in the sagittal plane one month after mandibular advancement with maxillary superior repositioning. Then, it moved superiorly approximately in the initial position. In the second measurement, a month after surgery, the condyle displaced laterally in the sagittal plane and repositioned to its original position after nine months. In the third measurement, the condyle displaced anteriorly one month after the surgery; then it positioned more posteriorly than its initial position nine months after the surgery. Changes in the sagittal plane were controlled by evaluation of condylar changes to the superior point of the external auditory meatus in the coronal plane23.
Our findings are also in line with the findings of a study by Chen et al., who found that the condyles tended to be positioned in a concentric position in relation to the glenoid fossa three months after the surgery and remained stable during the 1-year follow-up24. Contrarily, Harris et al. detected that 8 weeks after the SSO and mandibular advancement, most cases showed displacement of the condyle medially, posteriorly, superiorly, and angled medially25. Although these findings are contrary to the results of our study, they might be explained by the fact that their measurements were carried out 4 month earlier than ours.
Contrary to our results, some studies demonstrated inward rotation of the condyle after BSSO26–28. These contrary results might be explained due to different surgical techniques used during the operation, the use of different fixation systems after BSSO (rigid vs. semi-rigid vs. non rigid fixation), or different parameters measured at different times after surgery. Since our measurements where performed 6 month after surgery, we might not have detected positional changes of the condyle as physiologic adaptive bone remodeling, induced by the recovery of masticatory functions might already have taken place29.
Experimental and clinical studies have demonstrated that there is a close relation between condylar position in patients suffering from DFD and TMJ disorders1–4,30–34. Although OGS is a standardized and safe procedure, it has been shown that there is a correlation between OGS and TMJ symptoms in 2% of patients after surgery, especially in those patients who were already affected by TMJ disorders prior to surgery7,34. To prevent changes in TMJ position during surgery, several mechanical and computational devices have been developed to prevent the condyles from moving away from their original position, trying to address the correlation between OGS and TMJ symptoms35,36.
In this study no condylar positioning device was used, but surgery was carried out by two experienced surgeons to prevent extended condylar movement during the procedure and preserve the anatomical relation to reduce the influence on condyle anatomy and TMJ Function37,38. Our 3D analysis of condylar positional and volumetric changes shows, that there is no significant change in condylar position or anatomy after surgery. This finding is supported by current literature, which suggests that patients do not benefit from the use of condylar positioning devices9,10,14,15,39. In accordance with recent research we can postulate that there is only little change in mandibular structure and function after OGS32,33. This is supported by other studies, revealing that small positional changes of the condyle are not associated with early skeletal relapse11.
A unique aspect of surgery before orthodontic treatment is the possibility to evaluate the preoperative position of the condyle and the TMJ in its natural relation before orthodontic action. Although all measurements where done in a three-dimensional manner, this study is still subject to inherent limitations. All CT scans are prone to evaluation errors of condylar changes after orthognathic surgery. These errors are related to slice thickness, window level and width, matrix size, and rendering technique40. Another limitation is the small sample size, and the surgery first treatment concept as orthodontic treatment after surgery might have an impact on the position of the condyle. Another limitation of our study is that this method of measurement showed changes of intercondylar angles of 2.8 ± 3.6° in the LeFort I - only patients, although they underwent no relevant changes in the mandible. Consequently, this has to be interpreted as a measurement error or the effect of orthodontic treatment.
Conclusion
The present study revealed the clinical significance of changes to the TMJ after OGS in patients with DFD. We were able to demonstrate that free hand condyle positioning during orthognathic surgery has little effect on the natural condyle position in patients without orthodontic treatment. Further studies are needed to confirm the findings of this study.
Statement of Clinical Relevance
Freehand positioning of the condylar segments during a bilateral sagittal split osteotomy of the mandible in surgery first treatment concept, does not significantly change the position of the condyles.
Author Contributions
D.H. contributed to design of the work, data acquisition, and drafting of the article. K.W. contributed to data acquisition, data analysis, interpretation of data and revised this article. G.M. contributed to data analysis. K.S. contributed to the conception and revised this article. E.B. revised the article. F.W. revised the article. R.S. contributed to conception, drafting the article, data analysis, and statistics. All of the authors approved to submission of the final version of the manuscript.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Legrell PE, Isberg A. Mandibular length and midline asymmetry after experimentally induced temporomandibular joint disk displacement in rabbits. Am J Orthod Dentofacial Orthop. 1999;115:247–253. doi: 10.1016/S0889-5406(99)70325-2. [DOI] [PubMed] [Google Scholar]
- 2.Bryndahl F, Eriksson L, Legrell PE, Isberg A. Bilateral TMJ disk displacement induces mandibular retrognathia. J Dent Res. 2006;85:1118–1123. doi: 10.1177/154405910608501210. [DOI] [PubMed] [Google Scholar]
- 3.Jung WS, Kim H, Jeon DM, Mah SJ, Ahn SJ. Magnetic resonance imaging-verified temporomandibular joint disk displacement in relation to sagittal and vertical jaw deformities. Int J Oral Maxillofac Surg. 2013;42:1108–1115. doi: 10.1016/j.ijom.2013.03.012. [DOI] [PubMed] [Google Scholar]
- 4.Byun ES, Ahn SJ, Kim TW. Relationship between internal derangement of the temporomandibular joint and dentofacial morphology in women with anterior open bite. Am J Orthod Dentofacial Orthop. 2005;128:87–95. doi: 10.1016/j.ajodo.2004.01.028. [DOI] [PubMed] [Google Scholar]
- 5.Yang IH, Moon BS, Lee SP, Ahn SJ. Skeletal differences in patients with temporomandibular joint disc displacement according to sagittal jaw relationship. J Oral Maxillofac Surg. 2012;70:e349–360. doi: 10.1016/j.joms.2011.08.027. [DOI] [PubMed] [Google Scholar]
- 6.Firoozei G, Shahnaseri S, Momeni H, Soltani P. Evaluation of orthognathic surgery on articular disc position and temporomandibular joint symptoms in skeletal class II patients: A Magnetic Resonance Imaging study. J Clin Exp Dent. 2017;9:e976–e980. doi: 10.4317/jced.53824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Iannetti G, Fadda TM, Riccardi E, Mitro V, Filiaci F. Our experience in complications of orthognathic surgery: a retrospective study on 3236 patients. Eur Rev Med Pharmacol Sci. 2013;17:379–384. [PubMed] [Google Scholar]
- 8.Dujoncquoy JP, Ferri J, Raoul G, Kleinheinz J. Temporomandibular joint dysfunction and orthognathic surgery: a retrospective study. Head Face Med. 2010;6:27. doi: 10.1186/1746-160X-6-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kuehle R, Berger M, Saure D, Hoffmann J, Seeberger R. High oblique sagittal split osteotomy of the mandible: assessment of the positions of the mandibular condyles after orthognathic surgery based on cone-beam tomography. Br J Oral Maxillofac Surg. 2016;54:638–642. doi: 10.1016/j.bjoms.2016.03.017. [DOI] [PubMed] [Google Scholar]
- 10.Sander AK, Martini M, Konermann AC, Meyer U, Wenghoefer M. Freehand Condyle-Positioning During Orthognathic Surgery: Postoperative Cone-Beam Computed Tomography Shows Only Minor Morphometric Alterations of the Temporomandibular Joint Position. J Craniofac Surg. 2015;26:1471–1476. doi: 10.1097/scs.0000000000001781. [DOI] [PubMed] [Google Scholar]
- 11.Zafar H, Choi DS, Jang I, Cha BK, Park YW. Positional change of the condyle after orthodontic-orthognathic surgical treatment: is there a relationship to skeletal relapse? J Korean Assoc Oral Maxillofac Surg. 2014;40:160–168. doi: 10.5125/jkaoms.2014.40.4.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Arnett GW. A redefinition of bilateral sagittal osteotomy (BSO) advancement relapse. Am J Orthod Dentofacial Orthop. 1993;104:506–515. doi: 10.1016/0889-5406(93)70076-Z. [DOI] [PubMed] [Google Scholar]
- 13.Goncalves JR, et al. Temporomandibular joint condylar changes following maxillomandibular advancement and articular disc repositioning. J Oral Maxillofac Surg. 2013;71(1759):e1751–1715. doi: 10.1016/j.joms.2013.06.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ueki K, et al. Changes in temporomandibular joint and ramus after sagittal split ramus osteotomy in mandibular prognathism patients with and without asymmetry. J Craniomaxillofac Surg. 2012;40:821–827. doi: 10.1016/j.jcms.2012.03.003. [DOI] [PubMed] [Google Scholar]
- 15.Ellis, E. 3rd. Condylar positioning devices for orthognathic surgery: are they necessary? J Oral Maxillofac Surg52, 536–552; discussion 552–534 (1994). [DOI] [PubMed]
- 16.Costa F, et al. Condylar positioning devices for orthognathic surgery: a literature review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:179–190. doi: 10.1016/j.tripleo.2007.11.027. [DOI] [PubMed] [Google Scholar]
- 17.Cevidanes LH, et al. Three-dimensional cone-beam computed tomography for assessment of mandibular changes after orthognathic surgery. Am J Orthod Dentofacial Orthop. 2007;131:44–50. doi: 10.1016/j.ajodo.2005.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hunsuck EE. A modified intraoral sagittal splitting technic for correction of mandibular prognathism. J Oral Surg. 1968;26:250–253. [PubMed] [Google Scholar]
- 19.Epker BN. Modifications in the sagittal osteotomy of the mandible. J Oral Surg. 1977;35:157–159. [PubMed] [Google Scholar]
- 20.Fedorov A, et al. 3D Slicer as an image computing platform for the Quantitative Imaging Network. Magn Reson Imaging. 2012;30:1323–1341. doi: 10.1016/j.mri.2012.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.R: A language and environment for statistical computing (Foundation for Statistical Computing: Vienna, Austria, 2014).
- 22.Kim YJ, et al. Condylar positional changes up to 12 months after bimaxillary surgery for skeletal class III malocclusions. J Oral Maxillofac Surg. 2014;72:145–156. doi: 10.1016/j.joms.2013.07.031. [DOI] [PubMed] [Google Scholar]
- 23.Tabrizi R, Shahidi S, Bahramnejad E, Arabion H. Evaluation of Condylar Position after Orthognathic Surgery for Treatment of Class II Vertical Maxillary Excess and Mandibular Deficiency by Using Cone-Beam Computed Tomography. J Dent (Shiraz) 2016;17:318–325. [PMC free article] [PubMed] [Google Scholar]
- 24.Chen S, et al. Short- and long-term changes of condylar position after bilateral sagittal split ramus osteotomy for mandibular advancement in combination with Le Fort I osteotomy evaluated by cone-beam computed tomography. J Oral Maxillofac Surg. 2013;71:1956–1966. doi: 10.1016/j.joms.2013.06.213. [DOI] [PubMed] [Google Scholar]
- 25.Harris, M. D., Van Sickels, J. E. & Alder, M. Factors influencing condylar position after the bilateral sagittal split osteotomy fixed with bicortical screws. J Oral Maxillofac Surg57, 650–654, discussion 654–655 (1999). [DOI] [PubMed]
- 26.Ghang MH, et al. Three-dimensional mandibular change after sagittal split ramus osteotomy with a semirigid sliding plate system for fixation of a mandibular setback surgery. Oral surgery, oral medicine, oral pathology and oral radiology. 2013;115:157–166. doi: 10.1016/j.oooo.2012.02.022. [DOI] [PubMed] [Google Scholar]
- 27.Ueki K, Marukawa K, Shimada M, Nakagawa K, Yamamoto E. Change in condylar long axis and skeletal stability following sagittal split ramus osteotomy and intraoral vertical ramus osteotomy for mandibular prognathia. J Oral Maxillofac Surg. 2005;63:1494–1499. doi: 10.1016/j.joms.2005.06.013. [DOI] [PubMed] [Google Scholar]
- 28.Nishimura, A., Sakurada, S., Iwase, M. & Nagumo, M. Positional changes in the mandibular condyle and amount of mouth opening after sagittal split ramus osteotomy with rigid or nonrigid osteosynthesis. J Oral Maxillofac Surg55, 672–676, discussion 677–678 (1997). [DOI] [PubMed]
- 29.Park SB, et al. Effect of bimaxillary surgery on adaptive condylar head remodeling: metric analysis and image interpretation using cone-beam computed tomography volume superimposition. J Oral Maxillofac Surg. 2012;70:1951–1959. doi: 10.1016/j.joms.2011.08.017. [DOI] [PubMed] [Google Scholar]
- 30.Hellsing G, Holmlund A. Development of anterior disk displacement in the temporomandibular joint: an autopsy study. J Prosthet Dent. 1985;53:397–401. doi: 10.1016/0022-3913(85)90521-9. [DOI] [PubMed] [Google Scholar]
- 31.Ahn, S. J., Kim, T. W. & Nahm, D. S. Cephalometric keys to internal derangement of temporomandibular joint in women with Class II malocclusions. Am J Orthod Dentofacial Orthop126, 486–494, discussion 494–485, 10.1016/S0889540604004457 (2004). [DOI] [PubMed]
- 32.Schellhas KP, Piper MA, Omlie MR. Facial skeleton remodeling due to temporomandibular joint degeneration: an imaging study of 100 patients. Cranio. 1992;10:248–259. doi: 10.1080/08869634.1992.11677918. [DOI] [PubMed] [Google Scholar]
- 33.Schellhas KP, Pollei SR, Wilkes CH. Pediatric internal derangements of the temporomandibular joint: effect on facial development. Am J Orthod Dentofacial Orthop. 1993;104:51–59. doi: 10.1016/0889-5406(93)70027-L. [DOI] [PubMed] [Google Scholar]
- 34.Jung HD, Kim SY, Park HS, Jung YS. Orthognathic surgery and temporomandibular joint symptoms. Maxillofac Plast Reconstr Surg. 2015;37:14. doi: 10.1186/s40902-015-0014-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Funayama A, et al. A simple technique for repositioning of the mandible by a surgical guide prepared using a three-dimensional model after segmental mandibulectomy. Maxillofac Plast Reconstr Surg. 2017;39:16. doi: 10.1186/s40902-017-0113-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Savoldelli C, Chamorey E, Bettega G. Computer-assisted teaching of bilateral sagittal split osteotomy: Learning curve for condylar positioning. PLoS One. 2018;13:e0196136. doi: 10.1371/journal.pone.0196136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mousoulea S, Kloukos D, Sampaziotis D, Vogiatzi T, Eliades T. Condylar resorption in orthognathic patients after mandibular bilateral sagittal split osteotomy: a systematic review. Eur J Orthod. 2017;39:294–309. doi: 10.1093/ejo/cjw045. [DOI] [PubMed] [Google Scholar]
- 38.Vandeput, A. S. et al. Condylar changes after orthognathic surgery for class III dentofacial deformity: a systematic review. Int J Oral Maxillofac Surg, 10.1016/j.ijom.2018.06.008 (2018). [DOI] [PubMed]
- 39.Kim YI, Cho BH, Jung YH, Son WS, Park SB. Cone-beam computerized tomography evaluation of condylar changes and stability following two-jaw surgery: Le Fort I osteotomy and mandibular setback surgery with rigid fixation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111:681–687. doi: 10.1016/j.tripleo.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 40.Kawamata A, et al. Three-dimensional computed tomography evaluation of postsurgical condylar displacement after mandibular osteotomy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85:371–376. doi: 10.1016/S1079-2104(98)90059-2. [DOI] [PubMed] [Google Scholar]


