Abstract
Background:
This study aimed to evaluate the effect of self-care educational/training interventions on gestational diabetes.
Methods:
In this review, we searched the ERIC, Clinical Key, Cochrane, Scopus, PubMed, and ISI databases as well as Iranian databases from 1990 until Jan 2017. Having evaluated 3267 articles by three of the authors, 20 clinical trials with educational/training approach remained for analysis. In this study, CONSORT checklist, JADAD scale and Cochrane handbook were used to evaluate the validity of articles.
Results:
The quality of 34% of articles was found to be poor due to probability of bias in designing the interventions and the effect of absence of blinding of personnel and participants. However, absence of blinding had a low impact on the results of most studies carried out on objective scales like blood glucose levels, or maternal and neonatal results. Moreover, 66% of studies were assessed to be at a good level of quality.
Conclusion:
There are few articles with educational/training approach on self-care in gestational diabetes mellitus, but based on the homogeneity of participants and significant results of self-care interventions, especially lifestyle ones, self-care guidelines can be developed for gestational diabetes mellitus.
Keywords: Gestational diabetes mellitus, Self-care, Education, Training
Introduction
Gestational diabetes mellitus (GDM) is a kind of diabetes that is first identified in pregnancy with an increase in blood glucose level (1). GDM is accompanied by maternal and neonatal complications, also usually disappears after birth, but the mother and child are prone to develop type II diabetes for the rest of their lives. The prevalence of GDM is on the rise, followed by increased type II diabetes (2,3). Using new criteria in an international multi-center study, 18% of pregnancies were accompanied by GDM (3). An incidence of 3.4% for GDM was reported in Iran (maximum and minimum levels to be 18.6 and 1.3%, respectively), which is in line with the report in Kermanshah, Iran as well as the results of the systematic review (4–6).
Although the increased incidence of GDM has caused serious concerns for the health system around the world (7), there is strong evidence suggesting that a proper management can yield better results for the mother and child (8). Hence, women should receive education on diabetes self-care according to national standards after diagnosis and based on their requirements (9). The self-care approach was evaluated to diabetes changes during 1970–1990 from the patient’s passive participatory approach to patient’s empowerment and active participation in management of their disease (10), an approach we expect to occur in providing healthcare to mothers with GDM. With regard to GDM increase rate, few studies have been performed on each domains of self-care in gestational diabetes. The need for a new insight into the necessity of self-care educational program for GDM along with the current approach of the international community made the researchers in this study to carry out a systematic review to evaluate the effect of self-care educational/training interventions on GDM.
Methods
The research question in this study was: What is the effect of self-care education interventions on pregnancy outcomes in women with gestational diabetes versus routine training and services?
Strategy of search
Educational interventions included those performed with educational, teaching, instructional, training or counseling methods in the self-care domains of GDM. At baseline, using mesh and keywords of several articles, the keywords compatible with the research objectives in English and Persian. The keywords were searched in the educational resources information center (ERIC), Clinical Key, Cochrane, Scopus, PubMed, and ISI databases as well as Iranian databases, including Magiran, SID and Iran Medex until Jan 2017. Advanced search was carried out in the PubMed database using the operators AND/OR, keywords derived from the MESH and studies related, and limitations of the clinical trial articles without time limitations. With finding more relevant keywords, such as “self-care education”, “self- care education /training” and “gestational diabetes”, search done in other databases (English and Persian).
Keywords were gestational diabetes mellitus, diabetes pregnancy, self-care, self-management, education, training.
Selection of studies
The articles were screened by their titles and abstracts. The studies conducted on the women diagnosed with GDM were selected for analysis. The inclusion criteria consisted of articles with a relevant subject, a randomized clinical trial method, a full text and written in English or Persian language, determining the research question with PICOS model, the precise design of a randomized controlled clinical trial, without limitation of print time, paper or dissertation approved in academic centers. The educational interventions on self-care by every member of the healthcare team, by every educational/training method, in group or individuals were included in the study. Further, the studies with interventions approved by the ethical committee of research were selected for analysis.
For grey literature, Persian dissertations and unpublished researches through the National Library of the Islamic Republic of Iran and the Iranian Institute of Science and Technology (Iran Doc) and library resources of the universities as well as the WHO and Iranian Center of Clinical Trials Registration were searched. For English dissertations and unpublished researches we searched various sources, including the dissertation.com site, as well as the WHO and US Center of Clinical Trials Registration.
All stages of assessment of the quality of articles were carried out by two independent researchers. In the case of disagreement between the reviewers, a third reviewer refereed the articles.
Validity assessment of articles
CONSORT checklist (11), JADAD scale (12,13) and Cochrane handbook (14) were used to evaluate the validity of articles. CONSORT checklist was first used to assess the quality of the selected papers, out of which only two articles were found to have less than half of the items. JADAD scale is scored from 0 to 5 according to the probability of bias in the sampling process, sample loss and correct blinding. Studies with a score of ≥3 have a good quality (12,13). In addition, different kinds of bias defined in Cochrane handbook were used to assess the internal validity of articles (14). The external validity of the articles was also analyzed, and the papers with participants representing the target population as well as the samples randomly accessible from the population were selected for analysis. In most of the studies, the participants included those referring to the clinics and university hospitals from others prenatal clinics or offices.
Risk of bias
In the selection bias, the random sequence generation item was evaluated to be at low risk due to the use of one random replacement method in all studies. As for allocation concealment, 14 articles were assessed to be unknown and 6 articles were evaluated to be at low risk. In examining the performance bias, the blinding of participants and personnel was found to be unknown in 15 articles and at low risk in 5 articles. As for detection bias, all cases were found to be at low risk. In attrition bias, 4 papers were reported to be at high risk and 16 papers were at low risk. In reporting bias, due to the presence of all primary and secondary results in the report, all papers were evaluated to be at low risk. (Table 1). The quality of 35% of articles was found to be poor due to probability of bias in designing the interventions and the effect of absence of blinding of personnel and participants. Bias was possible to occur in the studies using self-reporting scales with no blinding of participants. However, absence of blinding had a low impact on the results in most studies carried out on objective scales like blood glucose levels or maternal and neonatal results, and the rest of studies were assessed to be at a good level of quality.
Table 1:
Cochrane bias risk assessment for included studies
| Reference | Random sequence generation | Allocation concealment | Blinding of participants and personnel | Blinding of Incomplete outcome assessment | outcome data | Selective reporting | Other sourcesof bias |
|---|---|---|---|---|---|---|---|
| Mendelson et al 2008 | L | U | U | L | L | L | L |
| Cao et al 2012 | L | U | U | L | L | L | L |
| Youngwanichsetha et al 2014 | L | L | U | L | L | L | L |
| Abirami et al 2014 | L | U | U | L | L | L | L |
| Petkova et al 2011 | L | U | U | L | H | L | H |
| Viswanath et al 2014 | L | U | U | L | H | L | H |
| Amason 2013 | L | U | U | L | L | L | H |
| Valipur et al 2014 | L | U | L | L | L | L | L |
| Reader et al 2006 | L | U | U | L | L | L | L |
| Hasle et al 2015 | L | L | U | L | L | L | L |
| De Barros et al 2010 | L | L | L | L | L | L | L |
| Brankston et al 2004 | L | L | U | L | L | L | H |
| Avery et al 1997 | L | U | U | L | L | L | H |
| Ferrara et al 2011 | L | U | L | L | L | L | H |
| Yang et al 2014 | L | U | L | L | H | L | H |
| Bo et al 2014) | L | L | L | L | L | L | L |
| Kaviani et al 2014 | L | U | U | L | L | L | L |
| Khadivzadeh et al 2015 | L | L | U | L | L | L | L |
| Kaveh et al 2012 | L | U | U | L | H | L | L |
| Homko 2002 | L | U | U | L | L | L | L |
L= Low Risk H= High Risk U= Unclear
Results
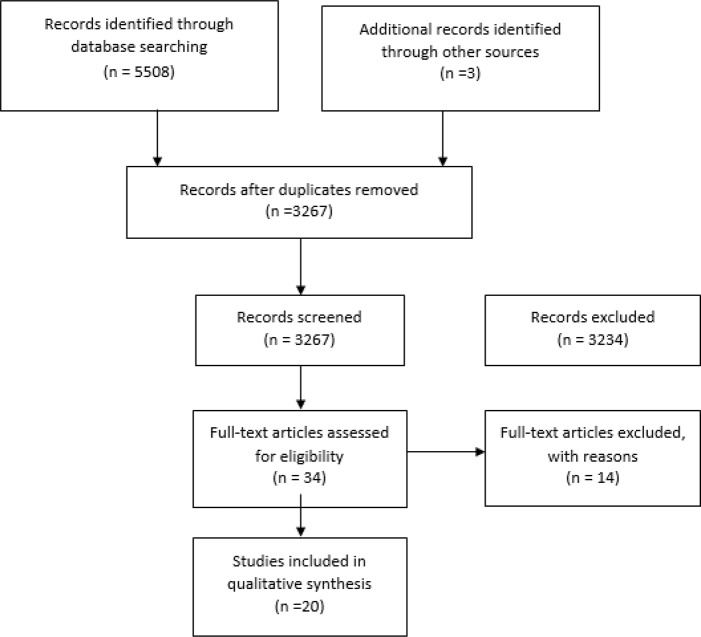
From 5508 articles found, 3267 articles remind after excluding the repetitive ones. In the search for the theses, two English and one Persian thesis were found. The titles and abstracts of the articles were then studied and those irrelevant to the research objectives were excluded and the full text of the relevant and probably relevant articles along with their references were evaluated to include other possible sources in the analysis. The articles lacking the full text (10 articles) were excluded due to the absence of adequate information in the abstract. After excluding the abstracts, non-clinical trials and studies irrelevant to the self-care educational/training interventions (32 articles), 34 articles remained. Of these, the clinical trials without randomization were excluded from the study (14 articles). Finally, 20 articles with educational/training approach remained three in Persian and the rest in English language. The algorithm of analysis is indicated in Fig. 1.
Fig. 1:
Flow diagram of the literature review process (PRISMA)
The outcomes under analysis comprised of knowledge level, self-care behaviors, glycemic control, neonatal, maternal, and obstetric results.
Characteristics of studies
Table 2 illustrates the features of the selected papers. This systematic review included 20 studies on 2698 women with GDM (1354 in intervention group and 1344 in control group). The intervention providers in these studies comprised of nurses, nutritionists and counselors, pharmacologists, doctors, midwives, and sports physiologists. Interventions were performed on different domains of knowledge, lifestyle modification, nutritional modification, physical activity, relaxation and blood glucose self-monitoring.
Table 2:
Characteristics and key results of included studies
| First author & year | Intervention type | Participants IG (intervention group) CG (control group) | Target population | Gestational week at start | results |
|---|---|---|---|---|---|
| Self- care education Interventions | |||||
| Khadivzadeh, T. 2015 | Education of self-care | 30 GDM women in each group | GDM* women referred to Ommolbanin hospital- Mashhad-IRAN | 24–30 |
|
| Viswanath, L 2014 | Teaching on self-care, monitoring of dietary log, guidance for diet planning and lifestyle change | 20 GDM women in each group | GDM women attending the Obstetrical unit of Amrita Institute of Medical Sciences, Kochi- Kerala-INDIA | 24–28 |
|
| Informational Interventions | |||||
| Amason, J.S. 2013 | Education for knowledge increase | 18 in IG 5 in CG |
GDM women at the Obstetric /Gynecology offices in the southeastern United States | 32–36 |
|
| Mendelson, SH.G. 2008 | A supplementary education session | 49 in IG 51 in CG |
GDM women referred by their obstetric provider to a hospital-based Perinatology clinic- Los Angeles, USA | 12–32 |
|
| Petkova, V. 2011 | An education program | 15 in each group | GDM women attending antenatal clinic - Sofia- Bulgaria | From 28 in diagnose |
|
| Kaveh, M. 2012 | Instruct education | 31 in IG 30 in CG |
GDM women, referred to hospitals of Shiraz University of Medical Sciences-IRAN | 21–34 |
|
| Life Style Interventions | |||||
| Cao, XP. 2012 | Individualized diabetes education, dietary and exercise advice, and instructions to SMBG* | 127 in IG 148 in CG |
GDM women from the outpatient clinic at the First Affiliated Hospital of Sun Yat-sen University (Guangzhou, China) | IG from 30.04± 4.46 CG from 30.82 ± 4.91 |
Lower instances of:
|
| Youngwanichsetha S. 2014 | Training of Yoga exercise & mindfulness eating | 87 in IG 90 in CG |
GDM women referred to a tertiary hospital in southern Thailand (the referral center for diabetes care) | 24–30 |
|
| Abirami. P. 2014 | Multi Model Intervention: counseling about diet, exercise, SMBG, insulin therapy and yoga | 104 in IG 108 in CG |
GDM women attended the antenatal outpatient department at government hospital, Tambaram- INDIA | 24–28 |
|
| Ferrara, A. 2011 | Diet, Exercise and Breast feeding Intervention (DEBI) | 96 in IG 101 in CG |
GDM women attending to the Kaiser Permanente Medical Care Program of Northern California- USA | After diagnosis in IG 31.8 (5.6) & in CG 31.0 (6.1) |
|
| Yang, X. 2014 | Life style intervention | 343 in IG 362 in CG |
Women with plasma glucose (PG) at GCT ≥7.8 mmol/L were referred to TWCHC GDM Clinic-Tiangin, CHINA | After screening in 24–28 |
|
| Bo, S. 2014 | Exercise and behavioral recommendations and counseling | 200 participants (Undetermine in each group) | GDM women attending the Sant’Anna Hospital-Turin, ITALY | After diagnosis in 24–26 |
|
| Exercise Training Interventions | |||||
| Hasle, RH.E. 2015 | Exercise training with stationary ergometer | 20 in each group | GDM women were recruited from the Diabetes Service at King Edward Memorial Hospital, Perth, Western Australia | 26–30 |
|
| De Barros, M.C. 2010 | Training of resistance exercise program | 32 in each group | GDM women who were under prenatal follow-up at the Obstetric Clinic of the University Hospital, University of Sao Paulo School of Medicine – Brazil | 24–34 |
|
| Brankston, G.N. 2004 | Circuit-type resistance training | 16 in each group | GDM women cared for at one of two perinatal units in Edmonton, Alberta, Canada | 26–32 |
|
| Avery, M.D. 1997 | Home based aerobic exercise training with cycle Ergometer and walking | 15 in IG 14 in CG |
GDM women referred to a large Midwestern health maintenance organization- Minnesota university-USA | ≥32 |
|
| Nutritional education Interventions | |||||
| Valipur. GH. 2014 | DASH* Diet education | 16 in each group | GDM women attending in fertility clinics of medical university of Kashan-IRAN | 24–28 |
|
| Reader, D. 2006 | Nutrition practice guidelines education | 85 in routine dietetic care & 130 in new guideline | GDM women attending in clinics (diabetes clinics, obstetric and other clinic types)- USA | After diagnosis of GDM |
|
| Mental Health Interventions | |||||
| Kaviani, M. 2014 | Benson’s relaxation technique | 29 in each group | GDM women referred to Hafez medical university of Shiraz- IRAN | 24–30 |
|
| Khadivzadeh, T. 2015 | Self-care education | 30 in each group | GDM women referred to Omolbanin hospital-Mashhad- IRAN | 24–30 |
|
| Educational Interventions of Blood glucose self-Monitoring | |||||
| Homko, C.A. 2002 | Self-monitoring of Blood glucose | 31 in IG 27 in CG | GDM women participate in the Diabetes-in-Pregnancy Program at Temple University Hospital and/or 1 of its satellite hospitals- USA | ≥33 |
|
Self-care education
Only one study was found to have complete educational content about self-care education (15). The effects of this intervention on self-efficacy and self-care behaviors were observed in these studies (15,16). Assessment of the impact of self-care training, a significant difference was found in the total score of self-care and its domains consist of adher to diet, drug use, physical activity, and blood glucose self-monitoring (15). Moreover, an increased score showed for self-care and its three dimensions (16).
Knowledge development
Although most of the interventions presented a kind of education in different domains of self-care, few studies had been done to enhance the participant’s knowledge (17–20). Several interventions were found to have improved the knowledge level (17,19, 20) or health promotion behaviors (18). Interventions were performed over one (17,18) or three training sessions (19,20). The maternal or neonatal outcomes, except for preterm birth (17), showed no significant difference between groups (17,18).
Lifestyle education
The maximum number of articles obtained was related to lifestyle interventions, a total of 7 articles being included in the study (21–26). Nutritional education and sports training were the basis of these articles. Glycemic control with a significant reduction of fast blood sugar (FBS) (22,23), blood glucose two hours postprandial (22–25) and hemoglobin A1c (HbA1c) (22,26) was seen in these interventions. In a study, lack of significant difference of FBS (26) and abnormal HbA1c was reported (25). Lack of difference in maternal and neonatal outcomes (21,25, 26) were some of the findings of these studies.
Exercise interventions
In this study, the exercise interventions with educational/training approach were included (27–30). In exercise interventions, aerobic fitness improvement, exercise attitude, exercise intention and cardiovascular fitness (27,30), as well as contradictory results, were observed with regard to the effect of resistance exercise on the number of patients requiring insulin and prescribed insulin dose (28,29). These interventions did not have a significant impact on glycemic control (28,29).
Nutritional interventions
The majority of interventional studies in this domain compared various diets in GDM, and only three studies were found to have educational approach (18,31, 32). The nutrition education intervention with dietary approaches to stop hypertension (DASH) performed significantly reduced FBS and serum insulin level of blood (31). However, teaching the practical guidelines of nutrition, compared with conventional nutrition training and diets, showed no significant difference in glycemic control or other maternal or neonatal outcomes (32).
Mental health interventions
No study was found with exactly this title in the searches. Relaxation training through Benson method in the study improved glycemic control and systolic blood pressure (33). The self-care education intervention carried out significantly reduced perceived stress by proposing problem troubleshooting, using problem-solving skills and group discussion strategies and presenting the experiences of other mothers in coping with their disease and problems (15).
Blood glucose self-monitoring
The studies on blood glucose measurement mostly concentrated on three domains of measurement times, comparison of self-monitoring with regular blood glucose monitoring system and use of telemedicine. The only educational/training intervention assessing the effect of blood glucose self-monitoring on self-efficacy and outcomes of pregnancy in GDM was conducted (34), revealing no significant difference between groups in blood glucose control.
Discussion
Numerous studies have been carried out around the world on self-care in type I and II diabetes, but the position of this approach is still not recognized in the management of GDM. Improvement of the self-care behaviors reported in a limited number of studies (15,16, 35) is indicative of the efficacy of and necessity of these interventions. The importance of self-care education and training in GDM not only helps the management of disease and reduction of maternal and neonatal complications but also will reduce the risk of maternal and neonatal type II diabetes in the upcoming years in the case of persistent changes in the lifestyle of people.
Increasing the knowledge level is one of the basic foundations of every self-care educational/training program. Evidently, this stage should be more taken into account in less developed societies.
In lifestyle studies, the interventions compatible with national cultures such as use of yoga or approaches like mindfulness eating (22,23, 25) in Asian countries. This approach recommended by international organization (36,37).
In exercise interventions, common characteristics, and to some extent different from other interventions, were seen, including low number of participants, considering fetal health approval in addition to maternal health in inclusion criteria, considering all known principles of exercise in pregnancy, supervised sessions and necessity of blood glucose measurement before starting exercise (27–30). The insignificant difference in obstetric results or glycemic control in these studies (38–41) might be due to small sample size. The mechanism of exercise effect on GDM was similar to type II diabetes and stated that exercise probably increased sensitivity to insulin (42). There was more tendency to use physical activities and exercise simultaneously to manage GDM over the past few years.
As for the educational interventions studied, a significant increase in nutritional knowledge, improved FBS, serum insulin level, glycemic control and quality of life were observed (19,25). Most of the available nutritional guidelines were on types I and II diabetes, and no specific instructions were designed for GDM (32). Studies on different diets in GDM are being conducted, and no definite results have been obtained so far.
In fact, reducing stress and improving the psychological status of individuals can be the incidental effects of every education and training. The results of the limited existing studies (15,20) were the same as those of other studies (35,43). Reducing stress and promoting the mental health were the positive effects of these interventions, which could favorably enhance glycemic control by decreasing the stress hormones and promoting the sense of self-efficacy ( 15,20,35,43). Mental health care is necessary for the mothers diagnosed with GDM.
In spite to result of another study (34), if we accept the blood glucose self-monitoring includes two sections of test performance and blood glucose model management, its position and role in the management of disease will be established.
Conclusion
There are few articles with educational/training or counseling approach to self-care in GDM than in type I and II diabetes. The existing studies have been carried out on various populations around the world, with different approaches, at various centers with limited number of samples. Despite these limitations and difficulty of interventional studies on pregnancy, their common findings can be acceptably generalized considering the homogeneity of participants, including gender, age (reproductive age), gestational diabetes, lack of other important diseases and referral to diabetes clinics of university centers. Thus, based on the homogeneity of participants and effective results of self-care interventions, especially lifestyle ones, self-care guide and guidelines can be developed for GDM. Although low number of studies or samples in some self-care domains were some limitations of this study, this study was the first to assess the need for self-care education in GDM.
Ethical considerations
Ethical issues (Including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Acknowledgements
The authors would like to acknowledge all the authors and participants of studies used in this review. This study was derived from a Ph.D. dissertation in Reproductive Health at Shahroud University of Medical Sciences.
Footnotes
Conflict of interest
The authors declare that there is no conflict of interests.
References
- 1.Cunningham L, Bloom Spong, et al. Williams Obstetrics (2014). McGraw Hill Education; 24th Edition Pp: 1125–1145. [Google Scholar]
- 2.International Federation of Diabetes (2016). Gestational diabetes. http://www.idf.org/about-diabetes
- 3.Centers for Disease Control and Prevention National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States, 2011. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, 2011. https://www.cdc.gov/diabetes/pubs/pdf/ndfs_2011.pdf [Google Scholar]
- 4.Jafari-Shobeiri M, GHojazadeh M, Azami-Aghdash S, et al. (2015). Prevalence and risk factors of gestational diabetes in Iran: A systematic review and meta-analysis. Iran J Public Health, 44(8):1036–1044. [PMC free article] [PubMed] [Google Scholar]
- 5.Rahimi R, Dinari ZH, Najafi F. (2010). Prevalence of gestational diabetes and its risk factors in Kermanshah 2009. Behbood J, 14(3):244–250. [In Persian] [Google Scholar]
- 6.Sayehmiri F, Bakhtiari S, Darvishi P, et al. (2013). Assessment of prevalence of gestational diabetes in IRAN: systematic review and meta analysis. The Iranian Journal of Obstetrics, Gynecology and Infertility, 15(40):16–23. [In Persian] [Google Scholar]
- 7.Ferrara A. (2007). Increasing prevalence of gestational diabetes mellitus a public health perspective. Diabetes Care, 30 Suppl 2:S141–6. [DOI] [PubMed] [Google Scholar]
- 8.Greuter MJE, Van Emmerik NMA, Wouters MGAJ, et al. (2012). Quality of guidelines on the management of diabetes in pregnancy: A systematic review. BMC Pregnancy Childbirth, 12:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.American Diabetes Association (2012). Standards of medical care in diabetesd. Diabetes Care, 35 Suppl 1;S11–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Norris SL, Engelgau MM, Venka Narayan KM. (2001). Effectiveness of self-management training in type 2 diabetes. Diabetes Care, 24:561–587. [DOI] [PubMed] [Google Scholar]
- 11.Berger VW, Alperson SY. (2009). A general framework for the evaluation of clinical trial quality. Rev Recent Clin Trials, 4(2): 79–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jadad AR, Moore RA, Carrol D. (1996). Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control Clin Trials, 17(1):1–12. [DOI] [PubMed] [Google Scholar]
- 13.Halpern SH, Douglas MJ. (2005). Jadad scale for reporting randomized controlled trials. Blackwell Publishing Ltd. [Google Scholar]
- 14.Higgins JPT, Green S. (2011). Cochrane handbook for systematic reviews of interventions version 5.1.0. The Cochrane Collaboration. https://training.cochrane.org/handbook
- 15.Khadivzadeh T, Hoseinzadeh M, Azhari S, et al. (2015). Effects of self-care education on perceived stress in women with gestational diabetes under insulin treatment. Evidence Based Care Journal, 5(3): 7–18. [In Persian] [Google Scholar]
- 16.Viswanath L, Jose A. (2014). Self-care agency of women with gestational diabetes mellitus - effectiveness of a self-care enhancing intervention. Int J Nursing Care, 2(1):26–31. [Google Scholar]
- 17.Amason JS. (2013). The effect of an educational intervention in women with gestational diabetes: A pilot study. Dissertation, Georgia State University; http://scholarworks.gsu.edu/nursing_diss/34 [Google Scholar]
- 18.Mendelson SH.G, McNeese-Smith D, Koniak-Griffin D, et al. (2008). A community-based Parish nurse intervention program for Mexican American women with gestational diabetes. J Obstet Gynecol Neonatal Nurs, 37(4):415–25. [DOI] [PubMed] [Google Scholar]
- 19.Petkova V, Dimitrov M, Geourgiev S. (2011). Pilot project for education of gestational diabetes mellitus (GDM) patients – Can it be beneficial? Afr J Pharm Pharmacol, 5(10):1282–1286. [Google Scholar]
- 20.Kaveh M, Kiani A, Salehi M, Amouei, et al. (2012). Impact of education on nutrition and exercise on the level of knowledge and metabolic control indicators of gestational diabetes mellitus patients. Iran J Endocrinol Metab, 13(5):441–448. [In Persian] [Google Scholar]
- 21.Cao XP, Wang Z, Yang CH, et al. (2012). Comprehensive intensive therapy for chinese gestational diabetes benefits both newborns and mothers. Diabetes Technol Ther, 14(11):1002–1007. [DOI] [PubMed] [Google Scholar]
- 22.Youngwanichsetha S, Phumdoung S, Ingkathawornwong TH. (2014). The effects of mindfulness eating and yoga exercise on Blood sugar levels of pregnant women with gestational diabetes mellitus. Appl Nurs Res, 27(4):227–30. [DOI] [PubMed] [Google Scholar]
- 23.Abirami PAJ. (2014). Reduction of risk on newly detected gestational diabetes mellitus by multi model intervention- A hospital based study. Int J Pharmaceut Clin Res, 6(4): 370–374. [Google Scholar]
- 24.Ferrara A, Hedderson MM, Albright CHL, et al. (2011). A pregnancy and postpartum lifestyle intervention in women with gestational diabetes mellitus reduces diabetes risk factors. Diabetes Care, 34(7):1519–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yang X, Tian H, Zhang F, et al. (2014). A randomized translational trial of lifestyle intervention using a 3-tier shared care approach on pregnancy outcomes in Chinese women with gestational diabetes mellitus but without diabetes. J Transl Med, 12:290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bo S, Rosato R, Ciccone G, et al. (2014). Simple lifestyle recommendations and the outcomes of gestational diabetes. A 2×2 factorial randomized trial. Diabetes Obes Metab, 16(10):1032–5. [DOI] [PubMed] [Google Scholar]
- 27.Hasle RHE, Wallmman KE, Dimmock JA, et al. (2015). Home-based exercise improves fitness and exercise attitude and intention in women with GDM. Med Sci Sports Exerc, 47(8):1698–704. [DOI] [PubMed] [Google Scholar]
- 28.De Barros MC, Lopes MAB, Francisco RPV, et al. (2010). Resistance exercise and glycemic control in women with gestational diabetes mellitus. Am J Obstet Gynecol, 203(6):556, e1–6. [DOI] [PubMed] [Google Scholar]
- 29.Brankston GN, Itchell BF, Ryan EA, et al. (2004). Resistance exercise decreases the need for insulin in overweight women with gestational diabetes mellitus. Am J Obstet Gynecol, 190(1):188–93. [DOI] [PubMed] [Google Scholar]
- 30.Avery MD, Leon AS, Kopher RA. (1997). Effect of partially home based exercise program for women with gestational diabetes. Obstet Gynecol, 89(1):10–15. [DOI] [PubMed] [Google Scholar]
- 31.Valipur GH, Asemi z, Samimi M, et al. (2014). The effect of DASH diet on insulin resistance, inflammation, and oxidative stress in gestational diabetes: A randomized controlled clinical trial. Iran J Diabetes Metab, 13(4):352–361. [In Persian] [Google Scholar]
- 32.Reader D, Splett P, Gunderson EP. (2006). Impact of gestational diabetes mellitus nutrition practice guidelines implemented by registered dietitians on pregnancy outcomes. J Am Diet Assoc, 106(9):1426–33. [DOI] [PubMed] [Google Scholar]
- 33.Kaviani M, Bahoosh N, Azima S, et al. (2014). The effect of relaxation on blood sugar and blood pressure changes of women with gestational diabetes: A randomized control trial. Iran J Diabet Obes, 6(1):14–22. [Google Scholar]
- 34.Homko CA, Sivan E, Reece EA. (2002). The Impact of self-monitoring of blood glucose on self-efficacy and pregnancy outcomes in women with diet-controlled gestational diabetes. Diabetes Educ, 28(3):435–443. [DOI] [PubMed] [Google Scholar]
- 35.Ko JM, Lee JK. (2014). Effects of a coaching program on comprehensive lifestyle modification for women with gestational diabetes mellitus. J Korean Acad Nurs, 44(6):672–81. [DOI] [PubMed] [Google Scholar]
- 36.Hod M, Kapur A, Sacks DA, et al. (2015). The international federation of gynecology and obstetrics (FIGO) initiative on gestational diabetes mellitus: A pragmatic guide for diagnosis, management, and care. Int J Gynaecol Obstet, 131 Suppl 3:S173–211. [DOI] [PubMed] [Google Scholar]
- 37.International Diabetes Federation (2009). Global guideline. Pregnancy and Diabetes. © International Diabetes Federation. https://www.idf.org/e-library/guidelines/84-pregnancy-and-diabetes.html
- 38.Avery MD, Walker AJ. (2001). Acute effect of exercise on Blood glucose and insulin levels in women with gestational diabetes. J Matern Fetal Med, 10(1):52–58. [DOI] [PubMed] [Google Scholar]
- 39.Davenport M.H, Mottola M.F, McManus, et al. (2008). A walking intervention improve capillary glucose control in women with gestational diabetes mellitus: A pilot study. Appl Physiol Nutr Metab, 33(3):511–7. [DOI] [PubMed] [Google Scholar]
- 40.Simony L, Nascimento, Fernanda G, et al. (2012). Physical exercise during pregnancy: A systematic review. Curr Opin Obstet Gynecol, 24(6):387–94. [DOI] [PubMed] [Google Scholar]
- 41.Ceysens G, Rouiller D, Boulvain M. (2010). Exercise for diabetic pregnant women (Review). The Cochrane Collaboration. Published by John Wiley & Sons, Ltd; https://www.cochrane.org/CD004225/PREG_exercise-for-diabetic-pregnant-women [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Golbidi S, Laher I. (2013). Potential Mechanisms of Exercise in Gestational Diabetes. J Nutr Metab, 2013:285948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bea ES, Park HJ. (2013). Effects of a Case Management Program on Self-efficacy, Depression and Anxiety in Pregnant Women with Gestational Diabetes Mellitus. Korean J Women Health Nurs, 19(2):88–98. [DOI] [PubMed] [Google Scholar]