Abstract
Introduction:
Operative duration is an important but under-studied predictor of mortality in emergency laparotomies.
Aims and Objectives:
The primary objective of this study was to quantify the effect of duration of emergency laparotomy in children on mortality; and to identify a rough cut-off duration of laparotomy to serve as a guide so that a laparotomy can be planned to optimize pediatric surgical patient outcome.
Materials and Methods:
This is a prospective study conducted in a government tertiary teaching institution over a period of 24 months. All children in the age group of 5–10 years presenting in the emergency department with Pediatric Risk of Mortality III score ≤8, undergoing emergency laparotomy in emergency operation theater, were included.
Observations and Results:
In all, 213 children were included in the study. The mean time from presentation to shifting to the operating room was 3.7 h. The mean operative duration was 108 min. The mean operative time in survived patients was 102 min as compared to 135 min in expired patients (P < 0.05). The 30-day in-hospital mortality rate was 17.4%. After application of binary logistic regression analysis, it was found that time to laparotomy and operative duration were significant risk factors (<0.05) predicting post-operative mortality. Kaplan–Meier survival curve showed a decrease at a mean weighted operative duration of approximately 100 min. Receiver operating characteristic curve analysis yielded operative duration of 123.5 min at which Youden's index maximized.
Conclusion:
This 100-min duration of laparotomy might appear a long duration but in casualty setup of a government hospital with limited resources, there are so many hurdles for optimal working that completion of an emergency laparotomy in children in 100 min can be considered a realistic target for improving post-operative outcome. At an operative duration of <123.50 min, mortality rates within acceptable limits can be achieved.
KEY WORDS: Emergency laparotomy, Kaplan–Meier analysis, mortality rate, operative duration, ROC curve analysis, survival
Introduction
Operative duration has been found to affect post-operative mortality rates.[1,2] Operative duration has been studied in various studies as a risk factor for predicting morbidity[3] and several other post-operative complications such as pneumonia.[4] However, the direct effect of operative duration on mortality has been studied sparingly and that too mainly in elective setting as studied by Yamashita et al.[2] and other authors. Thus, operative duration is an under-studied risk factor in predicting mortality in emergency laparotomies. No study was found during our literature review which predicted mortality as a function of operative duration in emergency laparotomies. Most studies focused on pre-operative factors and post-operative management for predicting laparotomy outcomes such as the use of Physiological and Operative Severity Score for the enumeration of Mortality and morbidity (POSSUM) score.[5] Thus, no clear-cut recommendation exists regarding the optimal time duration for an emergency laparotomy in pediatric population beyond which a laparotomy must not proceed as that would significantly increase the mortality rate.
Aims and objectives
The primary objectives of our study were to quantify the effect of duration of emergency laparotomy in children on mortality; and to identify a rough cut-off duration of laparotomy to serve as a guide so that a laparotomy can be planned to optimize pediatric surgical patient outcome in terms of decreased mortality. The secondary objectives included identifying factors that increase the time of emergency laparotomy and identifying measures that could be applied to reduce the time of laparotomy significantly, thus improving outcome.
Materials and Methods
This is a prospective study which was conducted at a government teaching institution over a period of 24 months (January 2015–December 2016). Ethical approval was provided by the Ethical Committee of the University and was conducted in accordance with guidelines of Good Clinical Practice and the Declaration of Helsinki. Written informed consent was taken from all patients.
Inclusion criteria
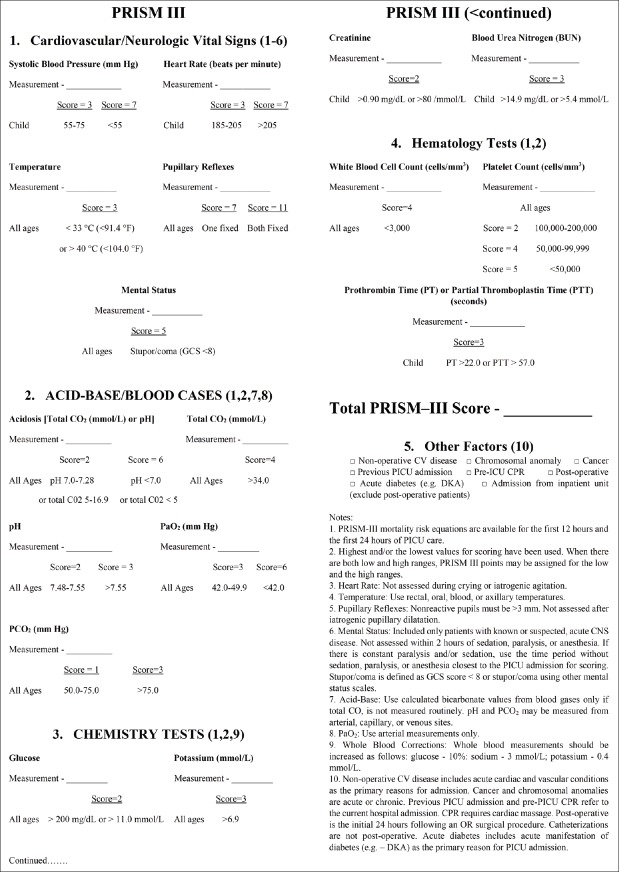
All pediatric patients in the age group of 5–10 years presenting with acute abdomen, diagnosed clinically and radiologically to be having a diagnosis of secondary peritonitis or obstruction, who were adequately resuscitated (with a minimum resuscitation period of at least 1 h) pre-operatively and underwent definitive surgery by a single surgeon (pediatric surgery senior resident) in the emergency operation theater (EOT) were included in the study. This age group was chosen because we had full follow-of up these patients in our intensive care unit (ICU) and ward. We had the facilities of managing patients only in the age group of >5 years in our high-dependency unit (HDU)-cum-ICU. Children under the age of 5 years were managed in pediatric ICU in collaboration with pediatricians. At our center, patients up to 14 years of age are categorized in pediatric age group. For managing patients above 10 years of age, we had collaborated with general surgical units in their ICU. Hence, the age group of 5–10 years was exclusively managed by us in our ICU. In addition, only those patients who had a Pediatric Risk of Mortality III (PRISM-III) score [Figure 1][6] of ≤8 at presentation were included to avoid the confounding effect of pre-operative variables that might affect mortality. All patients were adequately resuscitated in terms of temperature, central nervous system (Glasgow Coma Scale, pupillary reflexes), cardiovascular system (systolic blood pressure, heart rate), and respiratory system (oxygen saturation >95%, pCO2, pH, PaO2) parameters so that they were brought within 0 score range of PRISM-III score at the end of resuscitation and before shifting to operation theater. Furthermore, for inclusion only those pediatric patients were considered who presented within 72 h of initial onset of symptoms, operated within 24 h of initial presentation and who died in index hospital admission within 30 days.
Figure 1.
PRISM-III scoring chart (modified from Pollack et al.[6]) used in the study
Exclusion criteria
Patients who underwent damage control surgery, whose PRISM-III score was >9 at any point of time before undergoing laparotomy or inability to achieve adequate resuscitation (PRISM-III score >0 before shifting to operation theater), and/or requirement of resuscitation beyond 4 h of presentation were excluded from the study.
Postoperative care
All patients were shifted to pediatric ICU (PICU) after operation where dedicated staff and pediatrician were available for monitoring of patients and standard care of treatment. Poor patients who had limited purchasing power of buying expensive drugs were helped by obtaining drugs from our hospital's efficient Drug Society (which ran on funds provided by resident doctors voluntarily), procuring medicines from hospital's indent system, medical representatives, and non-government organizations (NGOs) working in collaboration with our hospital; exemption of dues of EOT and PICU was generously granted by courtesy of our respectful chief medical officers, head of the department, and chief medical superintendent. Thus, weak economic status of a patient was taken care of so it did not pose a problem in providing optimal post-operative management for such patients.
Statistical analysis
Data recording and follow-up progress were done with SURGILOG® android application. Data analysis was done with IBM SPSS Statistics® (Statistical Package for Social Sciences) software version 24 (IBM Corp., Armonk, NY, USA). Mean and standard deviation were observed for continuous forms of data such as age and operative duration. Such data were further evaluated for significance by Student's t-test (for comparing two groups), analysis of variance (ANOVA) (for comparing more than two groups), and post hoc analysis in the form of Tukey's honest significance difference (HSD) test. For categorical data, significance testing was done by Fisher's exact test (FET). A P value of less than 0.05 was considered statistically significant for all practical applications.
Results
A total of 247 patients were eligible for inclusion. However, 14 patients did not give consent for inclusion in this study. Nine patients had to be sent for ventilatory support outside the hospital, so the quality of post-operative care could not be standardized in these patients hence they were excluded from analysis. Further six patients took discharge on personal request and five patients left against medical advice. Thus, only 213 patients were included in the study for final analysis. Patients were divided into two study groups – survived (n = 176) and expired (n = 37) patients. The 30-day in-hospital mortality rate in our study was 17.4%. About 154 (72%) of them were males and the remaining 59 (28%) females giving a male-to-female ratio of 2.6:1.
Descriptive variables analyzed
The following descriptive variables of patients were analyzed – sex distribution, age distribution, time to presentation in emergency from initial symptoms (in hours), PRISM-III score at presentation and then before shifting inside EOT, duration to laparotomy after initial presentation in emergency (that is time duration from initial presentation to shifting inside EOT measured in hours), skin-to-skin operative duration (in hours), and outcome during index admission up to a maximum of 30-day hospital stay.
Normality testing
First, we performed a test of normality on our data to see whether it was normally distributed or not using SPSS software. This was important as we needed to know whether to use parametric or non-parametric tests to examine significance of data. Table 1 shows the result of normality testing. As can be seen from Table 1, for most of the data variables, P value is <0.05 thereby indicating that data distribution was not following normal distribution. So we decided to use non-parametric testing in the form of Mann–Whitney U test as the test of significance.
Table 1.
Results of tests of normality on the descriptive variable data
| Outcome | Kolmogorov-Smirnov | Shapiro-Wilk | ||||
|---|---|---|---|---|---|---|
| Statistic | df | Sig. | Statistic | df | Sig. | |
| Age (years) | ||||||
| Survived | 0.074 | 176 | 0.021 (S) | 0.980 | 176 | 0.011 (S) |
| Expired | 0.104 | 37 | 0.200 (NS) | 0.959 | 37 | 0.187 (NS) |
| Time to presentation (h) | ||||||
| Survived | 0.060 | 176 | 0.200 (NS) | 0.976 | 176 | 0.004 (S) |
| Expired | 0.156 | 37 | 0.023 (S) | 0.949 | 37 | 0.088 (NS) |
| PRISM-III score | ||||||
| Survived | 0.152 | 176 | 0.000 (S) | 0.955 | 176 | 0.000 (S) |
| Expired | 0.168 | 37 | 0.010 (S) | 0.924 | 37 | 0.015 (S) |
| Duration to laparotomy (h) | ||||||
| Survived | 0.212 | 176 | 0.000 (S) | 0.573 | 176 | 0.000 (S) |
| Expired | 0.265 | 37 | 0.000 (S) | 0.713 | 37 | 0.000 (S) |
| Operative duration (min) | ||||||
| Survived | 0.069 | 176 | 0.038 (S) | 0.987 | 176 | 0.094 (NS) |
| Expired | 0.098 | 37 | 0.200 (NS) | 0.974 | 37 | 0.531 (NS) |
df, degree of freedom; NS, not significant; S, significant; PRISM-III, Pediatric Risk of Mortality III
Analysis of descriptive variables with respect to gender
All the descriptive variable parameters have been tabulated with respect to gender in Table 2. It can be seen that the P value obtained from Mann–Whitney U test is >0.05 indicating there is no sex predilection for any of these confounding parameters. The mean age of presentation of patients was 7.9 ± 0.9 years. The mean time of presentation from initial onset of symptoms was 42.6 h. The mean time from presentation to shifting in the operating room was 3.7 h. The mean operative duration among all patients was 108 min.
Table 2.
Descriptive variables with respect to gender of patients
| Sex | No. of patients | Mean with standard deviation (range) | P (Mann-Whitney U test) |
|---|---|---|---|
| Age (years) | |||
| Male | 154 | 7.8±0.9 | 0.403 (NS) |
| Female | 59 | 7.9±0.9 | |
| Time to presentation (h) | |||
| Male | 154 | 42.0±14.8 (3-68) | 0.362 (NS) |
| Female | 59 | 44.1±15.5 (4-70) | |
| PRISM-III score | |||
| Male | 154 | 4.7±2.0 | 0.706 (NS) |
| Female | 59 | 4.6±1.9 | |
| Duration to laparotomy (h) | |||
| Male | 154 | 3.6±2.0 (1.7-16.4) | 0.316 (NS) |
| Female | 59 | 3.9±3.0 (2-21.5) | |
| Operative duration (min) | |||
| Male | 154 | 108.1±25.0 (54-197) | 0.773 (NS) |
| Female | 59 | 109.2±23.7 (65-174) |
NS, not significant; PRISM-III, Pediatric Risk of Mortality III
Analysis of descriptive variables by gender in study groups
Tables 3 and 4 show the descriptive parameters by gender in survived and expired patients, respectively, which again show that gender was not a confounding variable in the two study groups (P > 0.05). Figure 2 shows the final outcome of patients by gender. Males had a 30-day in-hospital mortality rate of 15.6% as against 22.0% among females. The data obtained from Figure 2 yielded a two-tailed P value of 0.313 (from FET) and P value of 0.266 (from Pearson's Chi-square test) implying that there was no significant difference between the mortality rates of males and females.
Table 3.
Descriptive variables in survived patients by gender
| Sex | No. of patients | Mean | Standard deviation | P |
|---|---|---|---|---|
| Age (years) | ||||
| Male | 130 | 7.842 | 0.9729 | 0.779 (NS) |
| Female | 46 | 7.889 | 0.9748 | |
| Time to presentation (h) | ||||
| Male | 130 | 42.00 | 14.973 | 0.816 (NS) |
| Female | 46 | 42.61 | 16.033 | |
| PRISM-III score | ||||
| Male | 130 | 4.75 | 1.996 | 0.718 (NS) |
| Female | 46 | 4.63 | 1.970 | |
| Duration to laparotomy (h) | ||||
| Male | 130 | 3.526 | 1.8780 | 0.581 (NS) |
| Female | 46 | 3.733 | 2.8637 | |
| Operative duration (min) | ||||
| Male | 130 | 103.11 | 21.726 | 0.626 (NS) |
| Female | 46 | 101.37 | 17.714 |
NS, not significant; PRISM-III, Pediatric Risk of Mortality III
Table 4.
Descriptive variables in expired patients by gender
| Sex | No. of patients | Mean | Standard deviation | P |
|---|---|---|---|---|
| Age (years) | ||||
| Male | 24 | 7.717 | 0.7961 | 0.104 (NS) |
| Female | 13 | 8.131 | 0.5483 | |
| Time to presentation (h) | ||||
| Male | 24 | 42.38 | 14.114 | 0.128 (NS) |
| Female | 13 | 49.62 | 12.197 | |
| PRISM-III score | ||||
| Male | 24 | 4.58 | 2.358 | 0.954 (NS) |
| Female | 13 | 4.54 | 1.941 | |
| Duration to laparotomy (h) | ||||
| Male | 24 | 4.225 | 2.5178 | 0.495 (NS) |
| Female | 13 | 4.915 | 3.5400 | |
| Operative duration (min) | ||||
| Male | 24 | 134.79 | 24.970 | 0.827 (NS) |
| Female | 13 | 136.62 | 22.273 |
NS, not significant; PRISM-III, Pediatric Risk of Mortality III
Figure 2.
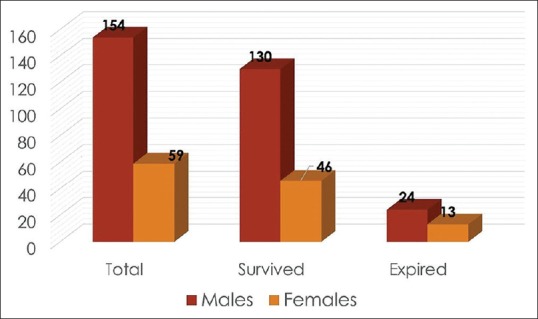
Final outcome of patients by gender
Relationship of descriptive variables with final outcome
Table 5 shows the relationship of descriptive variables with outcome. It can be seen that age, time to presentation, and PRISM-III score are not significantly different (P > 0.05) between the survived and expired groups of patients neither by Mann–Whitney U test nor by binary logistic regression analysis. This can also be explained by the fact that a capping was done in inclusion criteria for these parameters, for example, for age group it was 5–10 years, for time to presentation it was ≤72 h from initial onset of symptoms, and for PRISM-III score it was ≤8. Time duration to laparotomy was also capped by including only those patients who were operated within 24 h of presentation, but binary logistic regression analysis revealed a significant difference between the survived and expired patients (P = 0.049) though Mann–Whitney U test failed to reveal this relationship (P = 0.084). This means that expired patients were taken to operation theater significantly later as compared to survived patients. Thus, we can say that time to laparotomy is a relative risk factor in predicting operative mortality as this relationship was only elicited on regression analysis. Operative duration was significantly different in the two groups of outcomes in both statistical analyses, that is, Mann–Whitney U test and binary logistic regression analysis. The mean operative duration in survived patients was 102 min as against 135 min in expired group of patients (P = 0.000).
Table 5.
Relationship of descriptive variables with outcome
| Outcome | No. of patients | Mean with SD | P (Mann-Whitney U test) | Binary logistic regression significance |
|---|---|---|---|---|
| Age (years) | ||||
| Survived | 176 | 7.9±1.0 | 0.964 (NS) | 0.716 (NS) |
| Expired | 37 | 7.9±0.7 | ||
| Time to presentation (h) | ||||
| Survived | 176 | 42.16±15.2 | 0.309 (NS) | 0.308 (NS) |
| Expired | 37 | 44.92±13.8 | ||
| PRISM-III score | ||||
| Survived | 176 | 4.72±2.0 | 0.674 (NS) | 0.681 (NS) |
| Expired | 37 | 4.57±2.2 | ||
| Duration to laparotomy (h) | ||||
| Survived | 176 | 3.580±2.12 | 0.084 (NS) | 0.049 (S) |
| Expired | 37 | 4.468±2.9 | ||
| Operative duration (min) | ||||
| Survived | 176 | 102.65±20.7 | 0.000 (S) | 0.000 (S) |
| Expired | 37 | 135.43±23.8 |
SD, standard deviation; NS, not significant; S, significant; PRISM-III, Pediatric Risk of Mortality III
Kaplan–Meier survival curve
A Kaplan–Meier (K-M) curve was plotted using the data obtained in our study as shown in Figure 3. Survival function starts decreasing at around 99 min for females and 106 min for males. For males, 95% survival function corresponds to operative duration of 110 min, whereas for females it is 102 min. The K-M survival probability estimates at 125 min are about 0.90 for males and 0.85 for females. So here the survival in males starts outnumbering females as against the initial reverse difference. The K-M survival probability estimates are 75% at 132 min for males and 136 min for females, that is, again a reversal with females surviving longer operative durations. Around 50% survival corresponds to 146 min for males and 138 min for females implying that here the males are tolerating longer operative durations better than females. Thus, survival function suddenly decreases beyond approximately 135 min for both males and females. Mean-weighted decrease in survival function was defined around 100 min. Thus, we have taken 100 min operative duration as the cut-off duration beyond which survival function starts decreasing and this should ideally be the duration at which a laparotomy should be completed. A log-rank (Mantel–Cox) analysis was applied to compare the survival function of males and females which yielded a P value of 0.394 (P > 0.05), again indicating that there was no significant difference in survival function (mortality rates) between the two genders.
Figure 3.
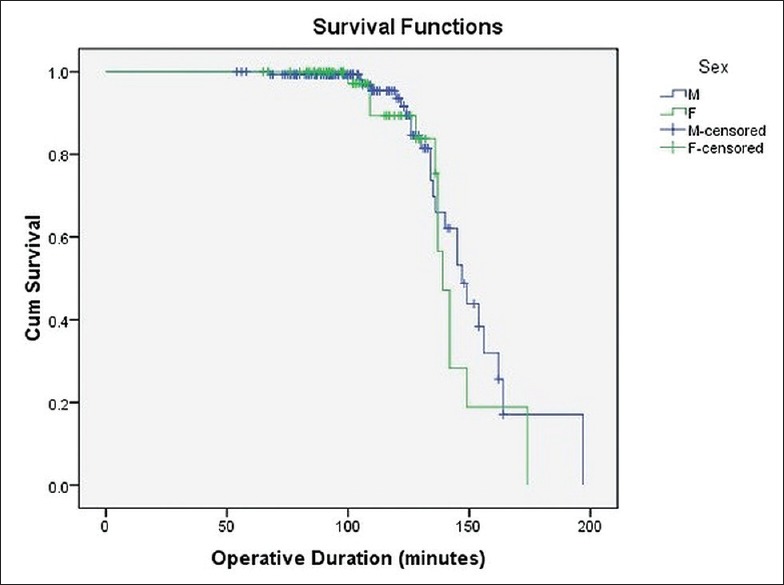
Kaplan–Meier survival curve
About 4% females with operative duration ≤100 min expired when compared with 35% females with operative duration >100 min (P < 0.05). Similarly, 1.2% males with operative duration of ≤100 min expired as against 26% males with operative duration >100 min (P < 0.05). Figure 4 shows the data of patients divided by cut-off laparotomy duration of 100 min against the final outcome. Around 2.2% patients expired in whom operative duration was ≤100 min when compared with a mortality rate of 28.7% in patients undergoing laparotomy >100 min (P < 0.05).
Figure 4.
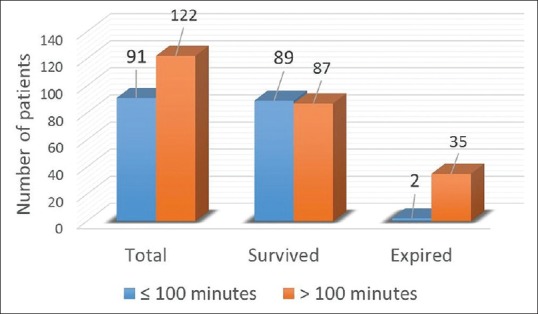
Final outcome as function of operative duration of 100 min
Receiver operating characteristic curve analysis
Receiver operating characteristic (ROC) curve was plotted for all descriptive variables, that is, age, time to presentation, PRISM-III score, time to laparotomy, and operative duration. The area under curve (AUC) for age was 0.501, for time to presentation 0.552, for PRISM-III score 0.529, for time to laparotomy 0.596, and for operative duration 0.864. An area between 0.9% and 0.99% is considered “very good,” between 0.8 and 0.89% is “good” and between 0.7 and 0.79% is “acceptable“ and finally, if the area is 0.5, the model is “bad.“[7] Thus, out of the five descriptives only operative duration (AUC = 0.864) showed good discriminative ability between survivors and non-survivors, and 86% variability in mortality could be attributed to operative duration. Other four descriptive variables showed poor overall accuracy (AUC between 0.5 and 0.6). ROC curve for operative duration is shown in Figure 5. Youden's index maximized at 123.50 min giving a sensitivity of 75.7%, specificity of 82.4%, positive predictive value of 94.2%, and negative predictive value of 47.5%. A P value of <0.05 was obtained on applying Chi-square test, indicating that at cut-off operative duration of 123.50 min, there were significantly more number of patients expiring in >123.50 min operative duration group and significantly more patients survived in <123.50 min operative duration group. Mortality rate in <123.50 min group was 5.8% as against 47.5% mortality in the other group.
Figure 5.
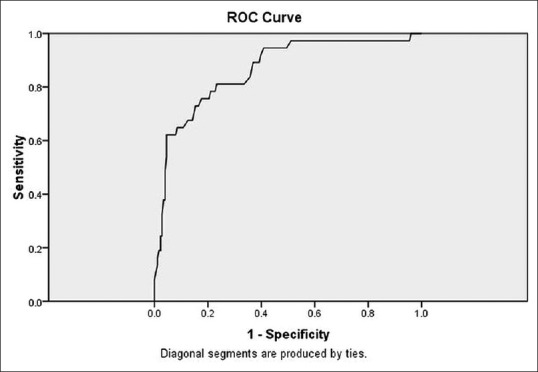
ROC curve for operative duration
Discussion
As familiarized earlier, there is scarce data in understanding the effects of operative duration alone as a function of postoperative mortality.
Interpretations from our study
From our study, we can chalk out several important interpretations.First, sex/gender does not affect post-operative 30-day in-hospital mortality. We also deduced that time to laparotomy is a relative risk factor for forecasting mortality in pediatric emergency laparotomies. Furthermore, operative duration was found to be an important risk factor in prognosticating probability of death following surgery in emergency setting. We conclude that in resource-limited setting like ours, an emergency pediatric laparotomy should ideally be completed within 100 min taking into account all intra-operative factors up to senior resident level in the EOT. At this cut-off value of 100 min operation time, mortality rates are minimal (1%–2%). If for some unforeseen circumstances the laparotomy duration is increasing, mortality rates in acceptable limits (≈5%) could be obtained at a cut-off operative duration of 123.5 min. Finally, an emergency pediatric laparotomy must not exceed 135 min in any situation as survival function decreases rapidly beyond this point.
Factors leading to increased time in shifting patient to emergency operation theater for laparotomy
Our study identified increased time to laparotomy as a relative risk factor for predicting mortality even after capping of 24 h that we applied in inclusion criteria. Time to surgery has been validated as a risk factor predicting post-operative mortality in some studies.[3] Now it is important to identify the factors which lead to increased duration in shifting the patient inside EOT as curbing these determinants will help in improving the survival of patients. We identified several factors that need to be addressed and can be used to optimize final outcome.
First and foremost is the nil per oral (NPO) status of children particularly from anesthetist's point of view. American Society of Anesthesiologist recommends a minimum fasting period of 2 h for clear fluids for all age groups; 4-h fasting period for human milk; 6-h fasting period for infant formulas, non-human milk or light meal; and 8-h fasting for fried foods, fatty foods, or meat.[8] Non-adherence to these guidelines can lead to increased risk of peri-operative aspiration thus putting the life of child at risk. Many a times this so happened that anesthetists had to deliberately postpone the patient for taking up for general anesthesia due to their recent oral intake status. Furthermore, sometimes we had so many patients in our emergency department who required operative intervention that deciding priority among those patients was difficult as we had only two EOTs, one of which was primarily for orthopedicians, vascular, and plastic surgeons but could be availed on request; and the other one was for surgical specialities including pediatric surgery cases. Pediatric cases were always taken up on priority basis except for adult cases of blunt and penetrating injuries. But this was a factor which delayed posting our cases sometimes. Presence of a dedicated pediatric EOT could have taken care of this aspect.
Then, we had only a single pediatric instrument operative tray which held us from posting back-to-back pediatric cases and also sometimes pediatric instruments were used by other surgical specialities particularly vascular surgery. This contributed to deferral of our cases. Round-the-clock availability of OT dresses and draping sheets was also a minor factor which held us from posting cases at times of high operative volume, rainy weather, and in winters.
It is a common understanding that pediatric cases require special attention with regard to anesthesia so the presence of at least a senior resident was a pre-requisite for taking up our cases. Now, since the senior resident in anesthesia did not remain in emergency all the time and was available on-call only, this sometimes lead to minor delays in taking up the patient specially at night time. Pre-operative resuscitation time, though, has been capped to maximum of 4 h for inclusion criteria in our study; but at times patients required longer time for resuscitation so that 0 value on PRISM-III score could be achieved before shifting for operation consequently leading to additional delays. However these cases have been excluded from final analysis for the sake of uniformity.
It is difficult to arrange medicines, resources, money, transport facilities, and blood by patient's attendants at odd timings, especially night time. Also, the residents, hospital staff, and OT staff are less efficient at odd hours. This effect of odd operative timing as a risk factor of post-operative morbidity and mortality has been validated in previous studies.[9] The same was true for us as well and this also contributed to delay in shifting patients inside EOT. Then there were problems in obtaining informed consent after explaining the procedures and its complications to patient's attendants. Several times, the procedure and its associated complications had to be explained to multiple family members. Patient's family members often resorted to calling and waiting for arrival of other elderly or educated or presumed knowledgeable relatives and sometimes their known doctors. They gave consent for laparotomy only after discussing the whole matter with them. This occasionally led to delays of several hours and was quite tiresome from operating teams’ point of view. Finally, availability of bed in PICU needed to be ensured, particularly if patient was anticipated to be requiring post-operative ventilatory support, again contributing to delays in operation.
Factors contributing to increased duration of laparotomy
Strictly speaking, this 100-min duration of laparotomy might appear a long duration from a senior consultant's perspective, but this operative duration has been measured from giving skin incision to the final stitch for abdominal closure; and all the operations were performed by a single senior resident with the help of junior residents posted in emergency. There were several factors which increased our overall operative duration. A review of all these factors might help us reduce the operative duration further thus improving survival even more.
Intra-operative hypothermia was one of the major factors especially in winters as our EOT had no spontaneous temperature regulatory mechanism and the only means of prevention was cotton wrapping and using warmers/blowers to actively warm-up the patient. Due to this hypothermia, operation had to be halted mid-way at many occasions so as to allow warming the patient by switching off fans and using hot air blowers. Intra-operative development of shock or hypotension was another mechanism which contributed to increased laparotomy duration as the anesthetists frequently asked for time to optimize the patient and/or requirement of insertion of central venous catheter, if it was not previously inserted. One more thing which contributed to increased duration was informing patients’ per-operative findings to senior consultants (as it was a norm at our hospital to do so) or asking for advice from a senior regarding operative decision-making intra-operatively. Non-availability of warm normal saline for intraperitoneal lavage also led to increased operation time sometimes. We also felt the need to inform the per-operative findings to patients’ relatives intra-operatively when some major operative findings were found. For example, we operated a female child of strangulated inguinal hernia in whom ovary of that side was found to be a part of hernial sac and was of questionable viability due to prolonged torsion. We had to inform this finding to patient's father and he made a decision to go with oophorectomy to avoid any chances of second exploration. Similarly, we had a policy to inform about requirement of major bowel resections or hemicolectomy to patients’ parents. There were a few occasions, when parents were not giving consent, and we had to bring them inside the EOT to show them per-operative finding to obtain consent for definitive procedure. This all added up to operative time.
Furthermore, the operating surgeon was initially less experienced and gradually learned over the course of time. Assisting residents kept on changing due to different duty days and compulsory rotation of postings. Moreover, OT assistant and other OT staff worked in shifts so they used to exchange duties at the time of shift change thus posing further difficulties. Night shift usually had relatively new and in-experienced OT staff. In-experience of anesthetists, again, due to junior residents working on shift basis led to temporary halting of procedures. All these factors led to minor increase in operative time but cumulatively it could amount to becoming significant. Here, we would specially like to mention that availability of dedicated pediatric surgery EOT, OT staff and anesthetists would definitely have cut short a lot of usual difficulties that we faced in our emergency setup. On occasions, it happened that suitable pediatric instruments were not available as we had only one pediatric emergency OT instrument set which was sometimes used by vascular surgery, plastic surgery, otorhinolaryngology, orthopaedics, and general surgery residents as well thereby contributing to inevitable delay and addition to operation duration. We had only single electrocautery set which sporadically malfunctioned. Non-availability of cautery pencil, suction set in the EOT led to delays. Finally, non-availability of specific pediatric sutures especially due to closed shops at night and poor non-affording patients also led to increased operative time. Thus, we saw that working in emergency setup in a teaching tertiary hospital has some unique problems which might lead to significantly increased operative time. Anticipating these problems prior-hand and proper planning of operation can reduce this wastage of time and we can reduce operative duration by as much as 20–30 min which will greatly improve patient survival.
Limitations of our study
As is the case, our study is not perfect after all and has some pitfalls which we would like to acknowledge so that if any other similar study is taken up in future, these limitations can be circumvented and more optimal results can be obtained. First, our study is not a case–control randomized study. Sample size can be further increased in future studies to account for any error which might have crept in due to the limited sample size of 213 patients. Although we have ruled out the confounding effect of gender in our study, still the number of females in our study was less than half of males. As is the common saying that female sex is more resilient to adversities especially in the pediatric population, our study might have overlooked the effect of gender on mortality. Patients with PRISM-III scores of 6–8 might skew the result due to their higher predictive mortality rates. Furthermore, secondary peritonitis and obstruction have different pathophysiology so there might be different mortality rates for these two disease processes but we have overlooked this fact in favor of PRISM-III score which can be used to predict mortality in all emergency situations.
Operating surgeons’ learning and skill would have improved over the course of time leading to decreased operative duration and improved overall survival. Since this study has been conducted in a teaching institution, operating surgeon might have given some operative steps to his juniors leading to increased operative time which might have affected the final outcome. The type of operative procedure performed, amount of intra-operative blood loss, and cause of mortality have not been discussed in our study. These might have a confounding effect on post-operative outcome which we have attributed to operative duration. Then, only mortality has been the focus of discussion in our study. Morbidity and other post-operative management characteristics have not been studied in this study. Further studies are required to study about the outcome in damage control procedures. Finally, the socioeconomic and educational status of patient's family also has a huge impact on their receptiveness to treatment, and faith in the health system and treating doctors.
Importance of our study and future directions
Our study is unique in the sense that it is the first study which has quantified the effect and impact of operative duration alone as a function of mortality by taking into account other pre-operative and post-operative confounding variables. We have also identified time taken to shift the patient to operation theater after initial presentation as a risk factor predicting postoperative mortality. Furthermore, we identified factors which led to increased time in shifting the patient to EOT and increased operative duration. Although the discussed factors which might reduce the operative duration are not new and at times might sound silly and lame, these elements have not been acknowledged in any previous studies. By taking into account the identified determinants for reducing operative duration and the deficiencies in our study listed above, a more comprehensive study can be taken up which may highlight additional risk factors of operative mortality which we might have missed. This study can also be roughly applied to adult population for optimizing outcome. Additionally, our study can provide a base for conducting a similar research in adults for quantifying a cut-off operative duration beyond which mortality is significantly increased.
Conclusion
In government hospitals’ casualty setup in developing countries, there are many hurdles that surgery residents have to face to strive for optimal working conditions. In such scenarios, completion of an emergency laparotomy in children in 100 min is a realistic target for improving postoperative outcome. We recommend pre- and per-operative planning so that ideally a pediatric emergency laparotomy is completed within 100-min time-frame in most circumstances to improve survival and minimize mortality. An operative duration <123.50 min is desirable if laparotomy time is increasing for some unforeseen circumstances as up to this duration, mortality rates within acceptable limits can be achieved. Finally, no pediatric laparotomy should go for >135 min because survival function decreases exponentially beyond this cut-off duration.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Cook TM, Day CJ. Hospital mortality after urgent and emergency laparotomy in patients aged 65 yr and over. Risk and prediction of risk using multiple logistic regression analysis. Br J Anaesth. 1998;80:776–81. doi: 10.1093/bja/80.6.776. [DOI] [PubMed] [Google Scholar]
- 2.Yamashita S, Haga Y, Nemoto E, Imanishi N, Ohta M, Kawahara K. E-PASS (The Estimation of Physiologic Ability and Surgical Stress) scoring system helps the prediction of postoperative morbidity and mortality in thoracic surgery. Eur Surg Res. 2004;36:249–55. doi: 10.1159/000078860. [DOI] [PubMed] [Google Scholar]
- 3.McGillicuddy EA, Schuster KM, Davis KA, Longo WE. Factors predicting morbidity and mortality in emergency colorectal procedures in elderly patients. Arch Surg. 2009;144:1157–62. doi: 10.1001/archsurg.2009.203. [DOI] [PubMed] [Google Scholar]
- 4.Liu R, Li W, Li Y, Han Y, Ma M, Zhu W, et al. Total time of operation is a risk factor of stroke-associated pneumonia in acute ischemic stroke patients with intra-arterial treatment. Medicine. 2016;95:e3958. doi: 10.1097/MD.0000000000003958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stonelake S, Thomson P, Suggett N. Identification of the high risk emergency surgical patient: Which risk prediction model should be used? Ann Med Surg. 2015;4:240–7. doi: 10.1016/j.amsu.2015.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pollack MM, Patel KM, Ruttimann UE. PRISM III: an updated Pediatric Risk of Mortality score. Crit Care Med. 1996;24:743–52. doi: 10.1097/00003246-199605000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Shann F. Are we doing a good job: PRISM, PIM and all that. Intensive Care Med. 2002;28:105–7. doi: 10.1007/s00134-001-1186-1. [DOI] [PubMed] [Google Scholar]
- 8.Practice Guidelines for Preoperative Fasting and the Use of Pharmacologic Agents to Reduce the Risk of Pulmonary Aspiration: Application to Healthy Patients Undergoing Elective Procedures: An Updated Report by the American Society of Anesthesiologists Task Force on Preoperative Fasting and the Use of Pharmacologic Agents to Reduce the Risk of Pulmonary Aspiration. Anesthesiology. 2017;126:376–93. doi: 10.1097/ALN.0000000000001452. [DOI] [PubMed] [Google Scholar]
- 9.Desai V, Gonda D, Ryan SL, Briceño V, Lam SK, Luerssen TG, et al. The effect of weekend and after-hours surgery on morbidity and mortality rates in pediatric neurosurgery patients. J Neurosurg Pediatr. 2015;16:726–31. doi: 10.3171/2015.6.PEDS15184. [DOI] [PubMed] [Google Scholar]