Abstract
Background
The permissible extent of pretransplant dialysis for patient and allograft survival is unclear. We assumed that a short period of dialysis before living donor kidney transplantation (LDKT) will show the similar results as preemptive kidney transplantation (PKT).
Material/Methods
We retrospectively evaluated the outcomes of LDKT according to pretransplant dialysis duration in both unmatched cohorts (n=1984) and propensity-score-matched cohorts (n=986) cohorts. The primary study endpoint was post-transplantation patient survival and death-censored graft survival (DCGS) according to the duration of pretransplant dialysis by 19 months which was the best cutoff value to differentiate clinical outcomes with the use of the time-dependent area under the curve.
Results
Of 1984 patients with LDKT at our center between January 2005 and September 2016, PKT was performed in 429 patients. The durations of pretransplant dialysis were <19 months in 962 recipients and ≥19 months in 593 recipients. There was no significant difference in mortality and DCGS between PKT and non-PKT recipients with pretransplant dialysis of <19 months. Patient survival (P=0.024) and DCGS (P=0.001) were worse in non-PKT recipients with pretransplant dialysis of ≥19 months. In the matched cohort, DCGS was significantly lower in non-PKT recipients with pretransplant dialysis of ≥19 months (P=0.037). It is likely that the incidence of biopsy-proven acute rejection was higher in this group (P=0.083).
Conclusions
Patient survival and DCGS were worse when the pretransplant dialysis duration was ≥19 months in a propensity-score-matched LDKT cohort.
MeSH Keywords: Dialysis, Kidney Transplantation, Propensity Score
Background
Preemptive kidney transplantation (PKT) is defined as kidney transplantation (KT) before the initiation of chronic maintenance dialysis. PKT provides better improvement in clinical outcomes than KT after a period of maintenance dialysis therapy. Thus far, it has been reported that PKT has better outcomes than non-PKT in both living-donor KT (LDKT) and deceased-donor KT (DDKT) [1–6]. However, although PKT has several advantages, not all recipients can be matched with a proper living donor in time. Therefore, pretransplant dialysis is inevitable in many patients.
In Asia, the mean waiting time for DDKT is rather longer than that in Western countries [7]. Evidently, prolonged waiting periods for DDKT may cause physical, psychological, and economic problems and can lead to poor clinical outcomes [8].
The dialysis duration before KT is one of the strong, independent risk factors for patient and graft survival after KT. Recent studies have suggested that the duration of dialysis before KT is an important factor determining clinical outcomes, with each additional year of dialysis treatment associated with an approximately 6% increase in the risk of death [9–11] Our hypothesis, however, is that short-term dialysis before KT may be permissible in terms of patient survival and graft survival, as much as PKT.
The purpose of this study was to validate the cutoff value of pretransplant dialysis duration to differentiate clinical outcomes, and to analyze whether patients with a longer duration of pretransplant dialysis had worse clinical outcomes.
Material and Methods
Study design and population
We conducted a retrospective cohort study of recipients who underwent KT at our center between January 2005 and September 2016. This study was performed after receiving approval from the Institutional Review Board of our center (S2017-2390-0001). Variables associated with recipients and donors were extensively reviewed. The clinical and research activities being reported are consistent with the Principles of the Declaration of Istanbul as outlined in the Declaration of Istanbul on Organ Trafficking and Transplant Tourism.
Immunosuppressants
The main immunosuppressive regimen consisted of basiliximab as an induction agent, and maintenance immunosuppressants consisted of a combination of a calcineurin inhibitor (tacrolimus or cyclosporine), mycophenolic acid, and prednisolone. As another option, recipients (n=112) with immunologic risk factors (highly sensitized patients or re-transplant recipients) and those with complications due to long-term use of steroids received rabbit anti-thymocyte globulin (Thymoglobulin®; Genzyme, Cambridge, MA, USA) as an induction regimen, and maintenance immunosuppression included tacrolimus, mycophenolic acid, and early steroid withdrawal in a week. In a case of ABO-incompatible KT, rituximab was used for desensitization 2 weeks before transplantation. The maintenance immunosuppression regimen was not different from those in ABO-compatible KT.
Outcome measures
We hypothesized that a short period of dialysis before KT will show similar results to those of PKT. The primary endpoint was the differences in patient and graft survival according to the duration of dialysis before transplantation: preemptive group, short-term dialysis group, and relatively long-term dialysis group. The secondary endpoint is biopsy-proven acute rejection (BPAR).
Statistical analysis
All data were presented as percentages, means with standard deviations, or medians with interquartile ranges (25–75%). Differences in continuous variables between 2 groups were compared using Student’s t test or Mann-Whitney test according to the distribution of the variables.
The Kaplan-Meier method was used to estimate the survival distributions, and differences between 2 groups were compared using the log-rank test. The global c-index, which represents the discrimination ability for patient survival and graft survival, was computed to determine a cutoff value of pretransplant dialysis duration.
Propensity score matching was performed to eliminate biases that might affect the results. Propensity scores for the estimated probability of each patient who underwent PKT were calculated using a multiple logistic regression model. A matching procedure was performed with the caliper of 0.1 score, and the model had a c-statistics of 0.68.
All statistical analyses were performed using SPSS version 19.0 for Windows (SPSS Inc., Chicago, IL, USA) and R software version 2.13 (R Foundation for Statistical Computing, Vienna, Austria). P values of <0.05 were considered statistically significant.
Results
Cutoff value of pretransplant dialysis duration for discrimination of patient survival and graft survival
A total of 2898 patients who underwent KT between January 2005 and September 2016 were included in this study. Among them, 1984 patients were analyzed after 914 patients were excluded owing to DDKT (n=667), multiorgan transplantation (n=207), and HLA-incompatible transplant including complement-dependent cytotoxicity-positive or flow-cytometry-positive cases (n=40) (Figure 1).
Figure 1.
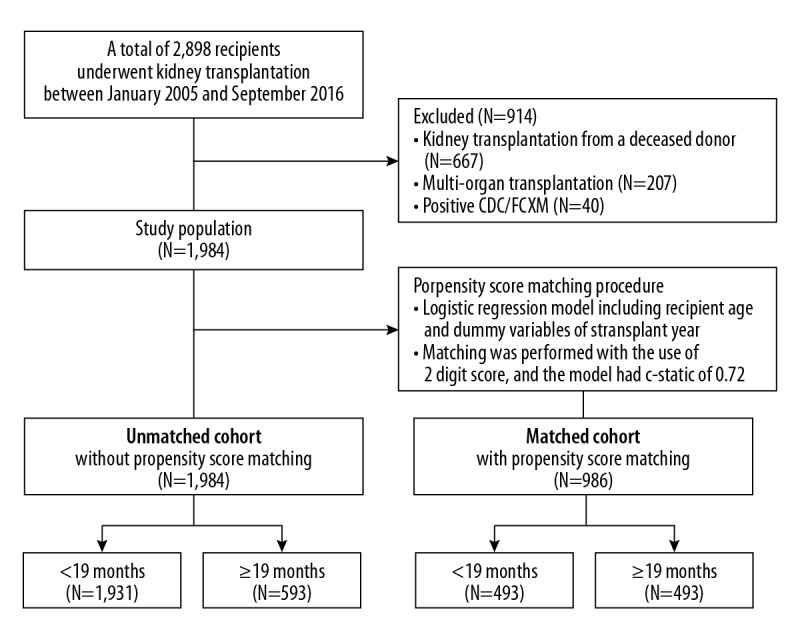
Flow diagram of the study. CDC – complement-dependent cytotoxicity; FCXM – flow cytometry crossmatch.
As described, we computed the global c-index, which represents the discrimination ability for patient survival and graft survival, to determine a cutoff value of pretransplant dialysis duration. The most appropriate cutoff value of pretransplant dialysis duration to differentiate clinical outcomes was 19 months. The receiver operating characteristic curve showed that this cutoff value yielded an area under the curve of 0.617 (95% confidence interval (CI), 0.508–0.726; P<0.001) (Figure 2). This cutoff value of 19 months has 57.6% sensitivity and 70.6% specificity for discriminating clinical outcomes. There were 429 recipients who underwent KT before the initiation of dialysis; 962 patients had pretransplant dialysis for <19 months; and 593 patients had pretransplant dialysis for >19 months. In the matched cohort, a total of 986 patients were included: 493 patients were assigned to a group with pretransplant dialysis duration < 19 months including PKT recipients (short pretransplant dialysis group), whereas the other 493 were assigned to another group with pretransplant dialysis duration ≥19 months (long pretransplant dialysis group).
Figure 2.
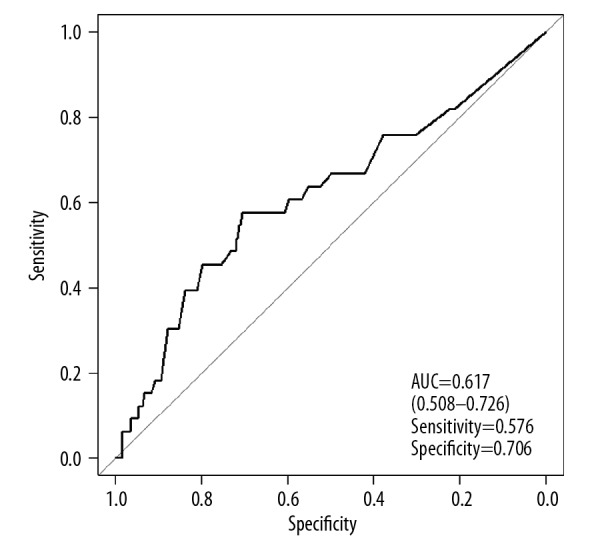
Receiver operating characteristic curve of pretransplant dialysis duration, predicting patient survival and graft survival. AUC – area under curve.
Demographics and baseline characteristics
Table 1 shows the clinical characteristics of patients enrolled in this study. In the unmatched cohort, the mean age of the recipients was 45±12 years, and 754 recipients (38%) were women. ABO-incompatible KT was performed in 319 recipients (16.1%). The mean follow-up period was 68.9±40.3 months. The mean age of the donors was 42±11 years, and 1023 donors (51.6%) were women. A total of 1269 recipients (64%) received a kidney from a related donor. In the unmatched cohort, those in the short pretransplant dialysis group were less likely to have a history of malignancy, tuberculosis, chronic hepatitis, and congestive heart failure. In addition, anticoagulants and anti-platelet agents were more frequently used in the short pretransplant dialysis group.
Table 1.
Characteristics of the study population before and after matching.
| Variables | Unmatched cohort | P value | Matched cohort | P value | ||
|---|---|---|---|---|---|---|
| <19 months (n=1391) | ≥19 months (n=593) | <19 months (n=493) | ≥19 months (n=493) | |||
| Recipient | ||||||
| Duration of dialysis (mo) | ||||||
| Median [interquartile range] | 2.0 [3–48] | 48.0 [19–288] | 3.0 [0–18] | 48.0 [19–288] | ||
| Mean (SD) | 4.2 (4.9) | 61.3 (42.4) | <0.001 | 4.4 (4.90) | 59.6 (40.44) | |
| Mean age, y (SD) | 45.3 (12.2) | 44.9 (12.1) | 0.570 | 46.0 (12.2) | 45.2 (11.9) | 0.327 |
| Female sex, n (%) | 544 (39.1) | 210 (35.4) | 170 (34.5) | 179 (36.3) | ||
| Body mass index, kg/m2 (SD) | 24.7 (69.9) | 23.1 (8.2) | 0.408 | 22.8 (3.4) | 23.3 (8.8) | 0.246 |
| Primary cause of ESRD, n (%) | <0.001 | 0.969 | ||||
| Glomerulonephritis | 217 (15.6) | 86 (14.5) | 65 (13.2) | 73 (14.8) | ||
| IgA nephropathy | 169 (12.1) | 36 (6.1) | 30 (6.1) | 32 (6.5) | ||
| Diabetes | 283 (20.4) | 115 (19.4) | 109 (22.1) | 98 (19.9) | ||
| Hypertension | 163 (11.7) | 95 (16.0) | 78 (15.8) | 76 (15.4) | ||
| FSGS | 32 (2.3) | 11 (1.9) | 9 (1.8) | 8 (1.6) | ||
| Polycystic kidney disease | 45 (3.2) | 24 (4.0) | 17 (3.4) | 18 (3.7) | ||
| Other/unknown | 482 (34.6) | 226 (38.1) | 185 (37.5) | 188 (38.1) | ||
| Hypertension, n (%) | 1201 (86.3) | 502 (84.7) | 0.360 | 426 (86.4) | 416 (84.4) | 0.417 |
| Diabetes mellitus, n (%) | 309 (22.2) | 120 (20.2) | 0.357 | 109 (22.1) | 101 (20.5) | 0.586 |
| Chronic hepatitis, n (%) | 63 (4.5) | 52 (8.8) | 0.021 | 35 (7.1) | 34 (6.9) | 1.000 |
| History of tuberculosis, n (%) | 50 (3.6) | 41 (6.9) | 0.002 | 26 (5.3) | 30 (6.1) | 0.680 |
| History of malignancy, n (%) | 31 (2.2) | 24 (4.0) | 0.035 | 16 (3.2) | 16 (3.2) | 1.000 |
| Cerebrovascular accident, n (%) | 34 (2.4) | 12 (2.0) | 0.682 | 8 (1.6) | 9 (1.8) | 1.000 |
| Congestive heart failure, n (%) | 4 (0.4) | 15 (2.5) | <0.001 | 4 (0.8) | 3 (0.6) | 1.000 |
| Coronary artery disease, n (%) | 72 (5.2) | 34 (5.7) | 0.692 | 30 (6.1) | 32 (6.5) | 0.896 |
| Arrhythmias, n (%) | 15 (1.1) | 14 (2.4) | 0.048 | 8 (1.6) | 8 (1.6) | 1.000 |
| Anticoagulant use, n (%) | <0.001 | 0.999 | ||||
| Antiplatelet | 144 (10.3) | 108 (18.2) | 79 (16.0) | 81 (16.4) | ||
| Warfarin | 5 (0.4) | 9 (1.5) | 5 (1.0) | 5 (1.0) | ||
| None | 1242 (89.3) | 476 (80.3) | 409 (83.0) | 407 (82.6) | ||
| Number of HLA mismatch (ABDR), (SD) | 3.1 (1.6) | 3.1 (1.6) | 0.948 | 3.1 (1.6) | 3.1 (1.5) | 0.617 |
| Number of HLA mismatch (DR), (SD) | 1.1 (0.6) | 1.1 (0.7) | 0.912 | 1.1 (0.7) | 1.0 (0.7) | 0.769 |
| PRA >20%, n (%) | 246 (17.7) | 110 (18.5) | 0.646 | 79 (16.0) | 94 (19.1) | 0.209 |
| Pre-DSA, n (%) | 80 (8.5) | 32 (9.2) | 0.683 | 83 (16.8) | 78 (15.8) | 0.667 |
| ABO incompatible, n (%) | 218 (15.8) | 101 (17.1) | 0.482 | 83 (16.8) | 78 (15.8) | 0.730 |
| Induction, n (%) | 0.586 | 0.888 | ||||
| Basiliximab | 1137 (81.7) | 490 (82.6) | 404 (81.9) | 404 (81.9) | ||
| Thymoglobulin | 76 (5.5) | 36 (6.1) | 26 (5.3) | 29 (5.9) | ||
| None | 178 (12.8) | 67 (11.3) | 63 (12.8) | 60 (12.2) | ||
| Calcineurin inhibitor, n (%) | 0.499 | 0.821 | ||||
| Cyclosporine | 505 (37.8) | 205 (35.8) | 177 (35.9) | 184 (37.3) | ||
| Tacrolimus | 832 (62.3) | 365 (63.8) | 314 (64.4) | 309 (62.7) | ||
| Antimetabolite, n (%) | 0.118 | 0.897 | ||||
| Mycophenolate mofetil | 679 (50.8) | 284 (49.7) | 250 (50.7) | 243 (49.3) | ||
| Myfortic acid | 389 (29.1) | 157 (27.4) | 146 (29.6) | 144 (29.2) | ||
| Azathioprine | 125 (9.3) | 67 (11.7) | 48 (9.7) | 58 (11.8) | ||
| CYT | 67 (5.0) | 40 (7.0) | 28 (5.7) | 28 (5.7) | ||
| None | 77 (5.8) | 24 (4.2) | 21 (4.3) | 20 (4.1) | ||
| Steroid, n (%) | 0.876 | 1.000 | ||||
| Maintenance | 1279 (95.5) | 548 (95.8) | 472 (95.7) | 473 (95.9) | ||
| Steroid withdrawal | 60 (4.5) | 24 (4.2) | 21 (4.3) | 20 (4.1) | ||
| Delayed graft function, n (%) | 21 (1.5) | 17 (2.9) | 0.066 | 12 (2.4) | 12. (2.4) | 1.000 |
| Donor | ||||||
| Mean age, y (SD) | 42.5 (11.1) | 41.8 (11.4) | 0.217 | 41.6 (11.3) | 41.8 (11.3) | 0.817 |
| Female sex, n (%) | 721 (51.8) | 302 (50.9) | 249 (49.5) | 247 (50.1) | ||
| Body mass index, kg/m2 (SD) | 24.4 (3.3) | 24.2 (3.2) | 0.451 | 24.3 (3.2) | 24.2 (3.3) | 0.778 |
| Current smoker, n (%) | 472 (33.9) | 180 (30.4) | 0.133 | 148 (30.0) | 156 (31.6) | 0.629 |
| Hypertension, n (%) | 58 (4.2) | 23 (3.9) | 0.860 | 24 (4.9) | 18 (3.7) | 0.430 |
| Diabetes mellitus, n (%) | 9 (0.6) | 1 (0.2) | 0.302 | 1 (0.2) | 1 (0.2) | 1.000 |
| Chronic hepatitis, n (%) | 8 (0.6) | 6 (1.0) | 0.326 | 3 (0.6) | 5 (1.0) | 0.723 |
| History of tuberculosis, n (%) | 28 (2.8) | 13 (2.2) | 0.589 | 8 (1.6) | 10 (2.0) | 0.812 |
| History of malignancy, n (%) | 10 (0.7) | 4 (0.7) | 1.000 | 1 (0.2) | 4 (0.8) | 0.370 |
| Relationship with recipient | 0.011 | 1.000 | ||||
| Related, n (%) | 915 (65.8) | 354 (59.7) | 299 (60.6) | 300 (60.9) | ||
| Unrelated, n (%) | 476 (34.2) | 239 (40.3) | 323 (65.5) | 314 (63.7) | ||
| 24-h creatinine clearance, mL/min (SD) | 117.4 (38.5) | 116.8 (26.9) | 0.704 | 117.5 (31.7) | 117.1 (27.4) | 0.814 |
| 24-h urine protein, mg/day (SD) | 90.4 (51.4) | 96.2 (90.8) | 0.143 | 93.8 (74.1) | 94.0 (32.8) | 0.960 |
| Kidney graft weight, g (SD) | 189.7 (51.8) | 192.3 (100.3) | 0.446 | 192.7 (68.9) | 88.2 (36.2) | 0.199 |
| eGFR (CKD-EPI),% (SD) | 103.9 (14.5) | 104.6 (14.5) | 0.290 | 105.3 (14.4) | 104.4 (14.7) | 0.321 |
SD – standard deviation; ESRD – end-stage renal disease; FSGS – focal segmental glomerulosclerosis; HLA – human leukocyte antigen; PRA – panel reactive antibody; DSA – donor-specific antibody; CYT – cyclophosphamide; eGFR – estimated glomerular filtration rate; CKD-EPI – Chronic Kidney Disease Epidemiology Collaboration.
Meanwhile, in the matched cohort, the 2 groups were well balanced with respect to all potential relevant clinical confounders (Table 1).
Impact of pretransplant dialysis duration on long-term mortality, graft failure, and BPAR
To verify the difference in clinical outcomes according to the duration of pretransplant dialysis, the cohort was classified into 3 groups: PKT, pretransplant dialysis <19 months, and pretransplant dialysis ≥19 months.
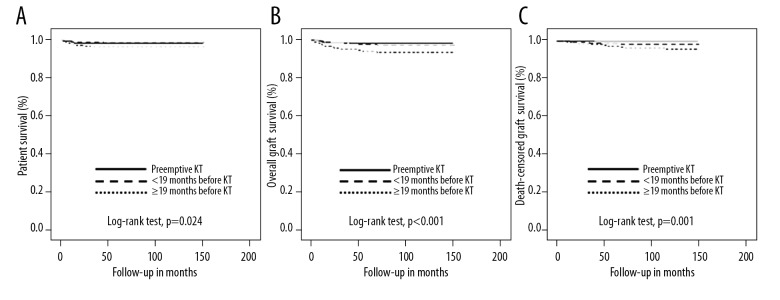
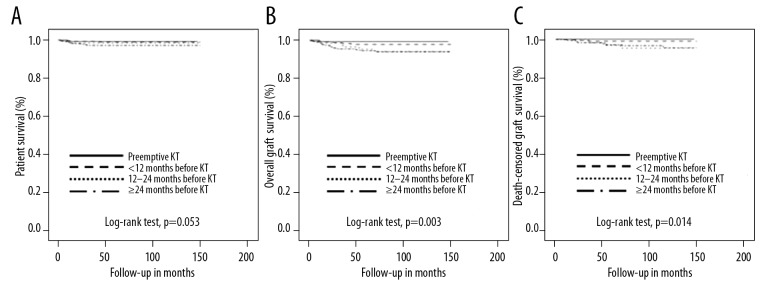
In the unmatched cohort, patient survival (P=0.024), overall graft survival (P<0.001), and death-censored graft survival (DCGS) (P=0.001) were significantly lower in recipients with pretransplant dialysis ≥19 months than in the other groups (Figure 3).
Figure 3.
Kaplan-Meier curves of unmatched cohorts for 11-year overall patient survival (A), overall graft survival (B), and death-censored graft survival (C) according to the duration of dialysis before kidney transplantation.
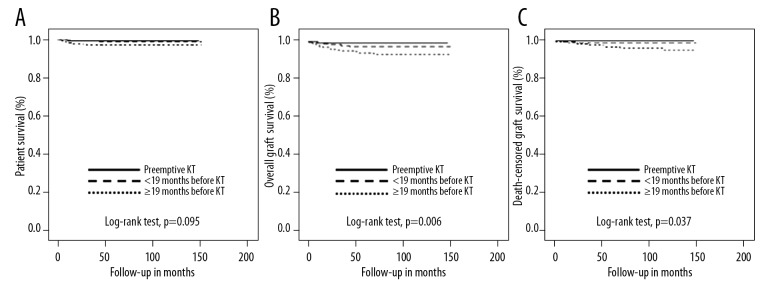
In the matched cohort, it is likely that patient survival was lower in those with pretransplant dialysis ≥19 months; however, the difference had marginal significance (P=0.095) (Figure 4A). However, overall graft survival (P=0.006) and DCGS (P=0.037) were significantly lower in those with pretransplant dialysis ≥19 months than in the other groups (Figure 4B, 4C).
Figure 4.
Kaplan-Meier curves of matched cohorts for 11-year overall patient survival (A), overall graft survival (B), and death-censored graft survival (C) according to the duration of dialysis before kidney transplantation.
In the unmatched cohort, a total of 32 of the 1984 recipients had died during the follow-up period. Infections (50%, n=16), cardiovascular events (21.9%, n=7), and malignancy (9.4%, n=3) were the 3 major causes of death after LDKT. Other causes of death were suicide, bowel perforation, and adrenal insufficiency. On the other hand, there were 17 mortality cases (1.7%) in the matched cohort. Of these, 1 case of PKT, 3 cases of pretransplant dialysis <3 months, and 13 cases pretransplant dialysis ≥19 months. Infection (52.9%) and cardiovascular accidents (23.5%) were the most common causes of mortality. Of the 19 cases of death-censored graft failure (1.9%), there were 4 recipients from the pretransplant dialysis <19 months and 15 recipients from the ≥19 months group. There was no death-censored graft failure in the PKT group during the follow-up period.
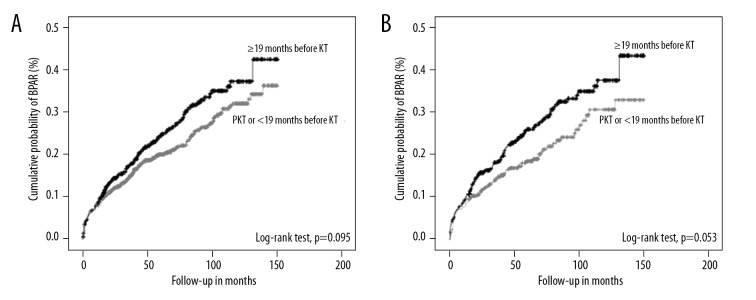
It seems that the BPAR rate was higher in those who had pretransplant dialysis ≥19 months than in those who had PKT or had pretransplant dialysis <19 months, not only in the unmatched cohort (P=0.083) (Figure 5A) but also in the matched cohort (P=0.053) (Figure 5B).
Figure 5.
Kaplan-Meier curves of unmatched (A) and matched (B) cohorts for 11-year biopsy-proven acute rejection (BPAR) according to the duration of dialysis before kidney transplantation.
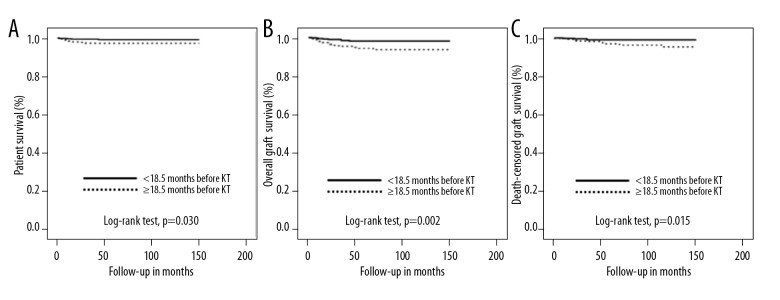
In addition, to support the reliability of the cutoff value, we compared clinical outcomes according to the median value of pretransplant dialysis duration. The median duration was 18.5 months in the matched cohort. In the matched cohort, 493 patients had pretransplant dialysis for equal to or less than 18.5 months whereas the other 493 had pretransplant dialysis for more than 18.5 months. Patient survival (P=0.03), overall graft survival (P=0.002), and DCGS (P=0.015) were significantly lower in those with the pretransplant dialysis for more than 18.5 months in the unmatched cohort as well as in the matched cohort (Figure 6).
Figure 6.
Kaplan-Meier curves of the matched cohort for 11-year overall patient survival (A), overall graft survival (B), and death-censored graft survival (C) according to duration of dialysis before kidney transplantation, classified by the median value (18.5 months) of pre-transplant dialysis duration.
On the other hand, clinical outcomes were compared according to pretransplant dialysis duration on a year-to-year basis. In the matched cohort, 140 patients had PKT whereas 308, 125 patients, and 413 patients had pretransplant dialysis for less than 12 months, 12 to 24 months, and equal to or longer than 24 months, respectively. It is likely that the patient survival was getting lower as the duration of pretransplant dialysis got longer with marginal significance (P=0.053). Meanwhile, overall graft survival (P=0.003) and DCGS (P=0.014) were getting lower as the duration of pretransplant dialysis got longer (Figure 7).
Figure 7.
Kaplan-Meier curves of the matched cohort for 11-year overall patient survival (A), overall graft survival (B) and death-censored graft survival (C) according to pre-transplant dialysis duration on a year-to-year basis.
Discussion
This study revealed that recipients who underwent LDKT after a short period of pretransplant dialysis had similar long-term outcomes to recipients who underwent PKT in terms of patient survival and allograft survival. In addition, the better allograft survival in the short pretransplant dialysis group than in the long pretransplant dialysis group is attributed, in part, to a lower incidence of BPAR.
The long-term outcomes of PKT in this study are consistent with those in previous reports. Mange et al. demonstrated that LDKT without long-term dialysis was associated with a 52%, 82%, and 86% reduction in the risk of allograft failure during the first, second, and subsequent years after transplantation, respectively, as compared with transplantation after dialysis [12]. A study in a Japanese cohort revealed that PKT could be beneficial for reducing mortality, graft failure, and post-transplant cardiovascular disease [1]. Kasiske et al. demonstrated that PKT was associated with improved patient and graft survival in both DDKT and LDKT [3]. On the other hand, this study differs from previous reports in that the long-term outcomes of LDKT recipients were assessed, whereas most of the previous studies dealt with outcomes of DDKT recipients according to a pretransplant dialysis duration [8,13–15].
Although the waiting time while on dialysis is a significant risk factor for mortality and graft failure, it is not well known how long a patient can maintain dialysis before KT to minimize the deleterious effects of long-term dialysis on patient and graft survival. This study suggests that recipients with a pretransplant dialysis time of ≥19 months have worse patient survival and graft survival. Furthermore, it is likely that the incidence of BPAR is higher in recipients who had maintained pretransplant dialysis for ≥19 months. Although this cutoff value of pretransplant dialysis duration needs to be further validated, the duration is much shorter than that in previous reports. Recently, it was reported that recipients with a pretransplant dialysis time of ≥10 years had worse outcomes than those who were preemptively transplanted or those who were transplanted with a shorter dialysis time, according to the analysis of the United Network for Organ Sharing registry data [13]. Goto et al. [1] also demonstrated that PKT could be beneficial for reducing the rate of clinical events including mortality, graft failure, and post-transplant cardiovascular disease (3.3%), whereas the rate of clinical events for those with a pretransplant dialysis time of <1 year is significantly increased (10.8%). On the contrary, the present study verifies that recipients with a short period of dialysis (<19 months) had favorable long-term outcomes similar to those of PKT recipients. Unlike in Western countries, candidates for DDKT in South Korea have a low chance for PKT unless they are undergoing dialysis according to the regulations established by the Korean Network for Organ Sharing (KONOS). Furthermore, the average waiting time for DDKT exceeds 5 years in South Korea, according to the 2016 KONOS annual report (data not shown). Therefore, a physician has to be able to recommend an optimal time of transplantation when a patient with end-stage renal disease considers LDKT in order to minimize the length of dialysis duration for favorable long-term outcomes. Although Okumi et al. [2] compared the clinical outcomes of PKT with those of non-PKT in a propensity-score-matched cohort, they only revealed that PKT was not associated with either improvement of post-transplant renal function or with a lower rate of common post-transplant complications compared with non-PTK. In the propensity-score-matched cohort of this study, however, it was evident that recipients with a short pretransplant dialysis duration had similar long-term outcomes to those who had PKT, whereas they had superior results to those with a long pretransplant dialysis duration in terms of mortality, graft survival, and BPAR.
This study has some limitations. First, the cutoff value of pretransplant dialysis duration to differentiate clinical outcomes was retrospectively determined from the data of a single center, although we used propensity score matching to remove potential confounding variables. For general application, therefore, it is necessary to validate our findings in a larger, multicenter cohort. Second, assessment of pretransplant donor-specific antibody was available since January 2009 when a single-antigen bead assay by Luminex was introduced at our center. Therefore, it is difficult to confirm a positive correlation between the duration of pretransplant dialysis and the presence of pretransplant donor-specific antibody. Third, ABO-incompatible KT was performed in about 16% of recipients who had desensitization treatments, including rituximab and total plasma exchange. Although there was no significant difference in the incidence of ABO-incompatible KT between the short and long pretransplant dialysis groups, it is possible that desensitization might have influenced the clinical outcomes. Nevertheless, to our knowledge, this study is the first to suggest the optimal duration of pretransplant dialysis for obtaining long-term clinical outcomes comparable to those of PKT.
Conclusions
Compared with a pretransplant dialysis time of ≥19 months, a pretransplant dialysis time of <19 months was associated with superior clinical outcomes that are similar to those of PKT in a propensity-score-matched cohort. It is necessary to set an appropriate cutoff value of pretransplant dialysis duration by using a national or international database to improve long-term patient survival and graft survival in LDKT.
Footnotes
Source of support: Departmental sources
Conflict of interets
None.
References
- 1.Goto N, Okada M, Yamamoto T, et al. Association of dialysis duration with outcomes after transplantation in a Japanese cohort. Clin J Am Soc Nephrol. 2016;11:497–504. doi: 10.2215/CJN.08670815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Okumi M, Sato Y, Unagami K, et al. Preemptive kidney transplantation: A propensity score matched cohort study. Clin Exp Nephrol. 2017;21:1105–12. doi: 10.1007/s10157-016-1345-x. [DOI] [PubMed] [Google Scholar]
- 3.Kasiske BL, Snyder JJ, Matas AJ, et al. Preemptive kidney transplantation: The advantage and the advantaged. J Am Soc Nephrol. 2002;13:1358–64. doi: 10.1097/01.asn.0000013295.11876.c9. [DOI] [PubMed] [Google Scholar]
- 4.Arze Aimaretti L, Arze S. Preemptive renal transplantation-The best treatment option for terminal chronic renal failure. Transplant Proc. 2016;48:609–11. doi: 10.1016/j.transproceed.2016.02.047. [DOI] [PubMed] [Google Scholar]
- 5.Fissell RB, Srinivas T, Fatica R, et al. Preemptive renal transplant candidate survival, access to care, and renal function at listing. Nephrol Dial Transplant. 2012;27:3321–29. doi: 10.1093/ndt/gfs012. [DOI] [PubMed] [Google Scholar]
- 6.Yoo SW, Kwon OJ, Kang CM. Preemptive living-donor renal transplantation: Outcome and clinical advantages. Transplant Proc. 2009;41:117–20. doi: 10.1016/j.transproceed.2008.09.063. [DOI] [PubMed] [Google Scholar]
- 7.Ahn C, Koo TY, Jeong JC, et al. Korean Organ Transplantation Registry Study Group. Initial report of the Korean Organ Transplant Registry: The first report of national kidney transplantation data. Transplant Proc. 2014;46:425–30. doi: 10.1016/j.transproceed.2013.11.083. [DOI] [PubMed] [Google Scholar]
- 8.Rose C, Gill J, Gill JS. Association of kidney transplantation with survival in patients with long dialysis exposure. Clin J Am Soc Nephrol. 2017;12:2024–31. doi: 10.2215/CJN.06100617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liem Y, Weimar W. Early living-donor kidney transplantation: A review of the associated survival benefit. Transplantation. 2009;87:317–18. doi: 10.1097/TP.0b013e3181952710. [DOI] [PubMed] [Google Scholar]
- 10.Meier-Kriesche HU, Kaplan B. Waiting time on dialysis as the strongest modifiable risk factor for renal transplant outcomes a paired donor kidney analysis. Transplantation. 2002;74:1377–81. doi: 10.1097/00007890-200211270-00005. [DOI] [PubMed] [Google Scholar]
- 11.Meier-Kriesche HU, Port FK, Ojo AO, et al. Effect of waiting time on renal transplant outcome. Kidney Int. 2000;58:1311–17. doi: 10.1046/j.1523-1755.2000.00287.x. [DOI] [PubMed] [Google Scholar]
- 12.Mange KC, Joffe MM, Feldman HI. Effect of the use or nonuse of long-term dialysis on the subsequent survival of renal transplants from living donors. N Engl J Med. 2001;344:726–31. doi: 10.1056/NEJM200103083441004. [DOI] [PubMed] [Google Scholar]
- 13.Aufhauser DD, Jr, Peng AW, Murken DR, et al. Impact of prolonged dialysis prior to renal transplantation. Clin Transplant. 2018;15:e13260. doi: 10.1111/ctr.13260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Keith DS. Preemptive deceased donor kidney transplant not associated with patient survival benefit in minority kidney transplant recipients. Clin Transplant. 2012;26:82–86. doi: 10.1111/j.1399-0012.2011.01398.x. [DOI] [PubMed] [Google Scholar]
- 15.Grams ME, Chen BP, Coresh J, Segev DL. Preemptive deceased donor kidney transplantation: considerations of equity and utility. Clin J Am Soc Nephrol. 2013;8:575–58. doi: 10.2215/CJN.05310512. [DOI] [PMC free article] [PubMed] [Google Scholar]