Abstract
Health literacy is the degree to which individuals are able to access and process basic health information and services and thereby participate in health-related decisions. Limited health literacy is highly prevalent in the United States and is strongly associated with patient morbidity, mortality, healthcare use, and costs. The objectives of this American Heart Association scientific statement are (1) to summarize the relevance of health literacy to cardiovascular health; (2) to present the adverse associations of health literacy with cardiovascular risk factors, conditions, and treatments; (3) to suggest strategies that address barriers imposed by limited health literacy on the management and prevention of cardiovascular disease; (4) to demonstrate the contributions of health literacy to health disparities, given its association with social determinants of health; and (5) to propose future directions for how health literacy can be integrated into the American Heart Association’s mandate to advance cardiovascular treatment and research, thereby improving patient care and public health. Inadequate health literacy is a barrier to the American Heart Association meeting its 2020 Impact Goals, and this statement articulates the rationale to anticipate and address the adverse cardiovascular effects associated with health literacy.
Keywords: AHA Scientific Statements, cardiovascular diseases, health disparities, health literacy, prevention and control
Health literacy, the degree to which an individual can access, process, and comprehend basic health information and services in order to inform and participate in health decisions,1 has a pivotal, decisive role in healthcare delivery and outcomes. Limited health literacy is an invisible barrier to healthcare delivery that has profound costs for individual and public health. Health literacy has been associated with limited knowledge of health conditions2–4 and medications,5 poorer overall health status,6,7 higher healthcare costs,8,9 and increased likelihood of rehospitalization10 and mortality.11–13 Awareness of health literacy, its implications, and relevance to individual and public health is fundamental to achieving the American Heart Association (AHA) 2020 Impact Goals to improve cardiovascular health by 20% for all Americans.14 The rationale for this statement is to address the relevance of health literacy to cardiovascular disease (CVD) management, prevention, and public health.
The overall objective of this statement is to clarify the central relevance of health literacy to cardiovascular health. The Institute of Medicine’s landmark 2004 report Health Literacy: A Prescription to End Confusion emphasized that health literacy operates within the “health concept,” recognized as the broad social fabric in which institutional, public, and private health occurs.1 Over the course of the past 1 to 2 decades, the discourse has progressed: Abundant and consistent scholarship has shown that health literacy is a barrier to healthcare access, physician-patient communication, adherence, and effective healthcare use and that organizational factors have a major role in easing or complicating health for people with limited health literacy. Likewise, patient- and family-centered care and patient/family engagement have emerged as priorities for addressing health literacy. Limited health literacy prevents individuals and families from developing the knowledge, skills, and confidence necessary to engage in their care in an empowered fashion. The effects of limited health literacy extend beyond the individual health encounter, given that health literacy is a shared function of social, cultural, and individual factors. Therefore, it structures opportunities for health and mediates and exacerbates disparities in cardiovascular care and treatment. This statement affirms the commitment of the authors and the AHA to addressing these challenges.1,15
Programmatic initiatives from the American Medical Association, the American College of Physicians,16 and The Joint Commission17 have advocated for incorporating health literacy into healthcare delivery and services. The Agency for Health Research and Quality (AHRQ) has promoted the Universal Precautions Toolkit to improve communication and implementation of health care.18 The authors of this statement embrace the “universal precautions” approach, which advocates for standardized communication, accessible at any level of health literacy. Understanding health literacy is critical for delivering health care, developing prevention initiatives, and addressing public health. This statement appreciates health literacy as systematically permeating how patients interact with the medical system, including their self-care, activation, and participation in decision making. Limited health literacy prevents individuals and families from developing the knowledge, skills, and confidence necessary to engage or participate in their care. The summary objective of this statement is to clarify the central relevance of health literacy and its importance in cardiovascular health and the health of the individual, the family, and our society.
The commitment of the AHA to this statement stems from the recognition of the widespread prevalence of limited health literacy in US adults19; the associations of health literacy with increased patient morbidity, mortality, healthcare use, and costs7,8,20; and the increasing complexity of understanding and navigating healthcare material and documentation provided to patients, including the use of electronic patient portals and other Internet-based health tools.21
The objectives of this statement are 5-fold. The first objective is to inform healthcare professionals’ knowledge of the prevalence of limited health literacy as it relates to cardiovascular health within and across healthcare encounters. Second, the statement establishes the importance of health literacy to health care in general and CVD treatment and prevention specifically by summarizing the association of health literacy across a spectrum of cardiovascular risk factors, diseases, and treatments. Third, this statement describes established and promising strategies that mitigate barriers imposed by limited health literacy to CVD management and prevention. The fourth objective is to articulate the interface of health literacy with social determinants of health and thereby demonstrate how limited health literacy perpetuates health disparities. Finally, this statement suggests future directions for integrating health literacy in cardiovascular research and health with the goal of improving patient care and public health initiatives.
METHODS: COMMITTEE COMPOSITION AND APPROACH TO THE LITERATURE
This statement summarizes contemporary studies relevant to health literacy and CVD and situates health literacy as an essential concept for the community of AHA researchers, investigators, and practitioners. This statement is not a systematic review, given the expansive nature of the topics of health literacy and CVD, nor is it a guideline for clinical practice. Rather, the statement is a summary of the contemporary science of CVD and health literacy with the purpose of enhancing the knowledge and awareness of healthcare professionals. The studies presented are a synthesis of the existing literature, informed by existing systematic reviews and the diverse perspectives of the experts on the writing group.22 The 10-member writing group for this statement is diverse in its demographic composition, disciplinary perspectives, and context expertise. It consists of 4 women, includes 2 underrepresented minorities, and comprises clinicians (internal medicine, cardiovascular physicians, and nurses) and clinician scientists engaged in health services research, epidemiology, health education, and behavioral health interventions. The committee is further enhanced by individuals with expertise in social determinants of health (including health literacy) and cardiovascular health disparities affecting racial/ethnic minorities and rural populations and the development and evaluation of community-based interventions and strategies to promote health.
HEALTH LITERACY: DEFINITIONS AND DIMENSIONS
Measuring Literacy in the United States
In 1992, the US Department of Education initiated the first population-based, in-person assessment of adult literacy with the National Adult Literacy Survey.23 The survey characterized 46% to 51% of participants as being in the 2 lowest quintiles of literacy. From this study, as many as 90 million Americans ≥16 years old were estimated to have significantly limited reading and quantitative skills. In 2003, the US Department of Education conducted the National Assessment of Adult Literacy Survey,24 which specifically included health literacy, in contrast to the measurement of general literacy by the National Adult Literacy Survey. The National Assessment of Adult Literacy Survey determined that 36% of US adults had basic or below-basic health literacy and identified significant differences in health literacy across sex, age, and race/ethnicity categories.25 Twelve percent of women were classified in the lowest literacy category, below basic, compared with 16% of men. Older adults (categorized as ≥65 years of age) had worse health literacy than individuals in younger age categories in that 59% were measured at or below basic health literacy. There were substantive racial and ethnic differences: 9% of non-Hispanic whites had below-basic health literacy compared with 25% of American Indian/Alaskan Native, 24% of non-Hispanic black, and 41% of white Hispanic adults. Health literacy was positively correlated with educational attainment. Of individuals without a high school education, 49% were categorized as having below-basic health literacy compared with 3% to 5% of those with some college education.25
The more contemporary Programme for the International Assessment of Adult Competencies surveyed >160 000 adults 16 to 65 years of age in 24 countries and subnational regions to assess literacy and numeracy in a technology-rich environment. Literacy and numeracy levels were ranked from 1, the lowest level, to 5, the highest level, across participating countries.26 In the United States, 5010 adults participated in the administration of the survey in 2011 to 2012. The majority of US participants (54.3%) were categorized as having level 2 or lower literacy. In terms of numeracy proficiency, 65.6% of participants were classified as having level 2 or lower proficiency.27 These data indicate the ongoing challenge of adult literacy in contemporary US society.
Dimensions of Health Literacy
Continued scholarship in health literacy has broadened the definition and constituent components of the topic. The definition of health literacy has expanded to encompass skills requisite for successful functioning in an information-based, electronic society.28 There is a current appreciation that health literacy extends beyond proficiency in reading, writing, and numeracy and involves interpretation of images, oral communication, facility with technology, and social networking.29 Health literacy has further been considered fundamental to abstract skills such as evaluating and weighing treatment considerations and engaging in medical decision making; how patients navigate the electronic, geographic, and administrative components of health care; and how individuals implement health-related information and engage in self-care.30–32 The net result is an understanding of health literacy as spanning multiple cognitive and social domains that interface with the technological and community environments. A content analysis identified 11 fundamental, interrelated skills that make up and define health literacy.33 These skills and their definitions are summarized in Table 1.
Table 1.
Taxonomy of Health Literacy Skills and the Specific Domains of Their Competencies
| Skill | Constituent Competency and Ability |
|---|---|
| Literacy | Perform basic reading tasks |
| Interaction | Engage in communication about health |
| Comprehension | Understand varied sources of information |
| Numeracy | Engage in basic numerical and arithmetic tasks and operations |
| Information seeking | Seek and obtain health-related information |
| Application/function | Process and use current and evolving health-related information |
| Decision making/critical thinking | Engage in informed health-related decision making |
| Evaluation | Filter, interpret, and evaluate information |
| Responsibility | Take responsibility for health and health-related decision making |
| Confidence | Have sufficient confidence to improve personal and community health |
| Navigation | Navigate society and health systems for successful self-care |
Multiple and diverse measures have been implemented for quantifying and characterizing individuals’ health literacy. Table 2 summarizes select, widely used health literacy measures, their fundamental characteristics, and the health literacy dimensions assessed by the measures. The most recent comprehensive review of the dimensions and psychometric properties of the measures was published in 2014,34 which at that time identified 51 tools for health literacy measurement. The tools were characterized as general assessments (n=26), disease or condition specific (n=15), or targeted to a population (n=10). The Boston University Health Literacy Tool Shed maintains a database of health literacy measures.47 Items are categorized by health literacy domain, instrument context (such as condition or disease), number of items, instrument language, and administration time. The database also contains a psychometric evaluation for the various instruments that includes the sample size used for validation, cohort age, and the measure style as characterized by the predominant measurement tools for health literacy assessment. More than 125 such instruments are now cataloged by the Health Literacy Tool Shed.34,47
Table 2.
Health Literacy Measures and Descriptive Characteristics
| Measure | Constructs Measured | Year Published |
Available in Spanish |
Number of Items |
Time to Administer, min |
Remote Administration (Phone, E-Mail) |
|---|---|---|---|---|---|---|
| Rapid Estimate of Adult Literacy in Medicine35 | Recognition and pronunciation of medical terminology | 1991 (LV) 1993 (SV) | No | 66 (LV) 7 (SV) |
3–7 (LV) 1 (SV) |
No |
| Test of Functional Health Literacy in Adults36,37 | Reading comprehension, numeracy | 1995 (LV) 1999 (SV) | Yes | 67 (LV) 36 (SV) |
22 (LV) 7 (SV) |
No |
| Three-Item Health Literacy Screening,38 Brief Health Literacy Screening Tool39 | Reading and verbal comprehension, need for assistance, confidence | 2004, 2009 | Yes | 4 | 1–2 | Yes |
| Short Assessment of Health Literacy for Spanish-Speaking Adults40 | Recognition of medical terms | 2006 (LV)2010 (SV) | Yes | 50 18 |
3–6 (LV) 2–3 (SV) |
No |
| Newest Vital Sign41 | Reading, comprehension of a nutrition label | 2005 | Yes | 6 | 3–4 | No |
| Medical Term Recognition Test42 | Recognition of medical terms | 2010 | No | 70 | 2–3 | Yes |
| Functional Health Literacy Test43 | Reading comprehension | 2009 | No | 21 | 3 | No |
| Health Literacy Skills Instrument44,45 |
Prose, document, quantitative, oral and Internet information seeking | 2010 (LV) 2012 (SV) | No | 25 10 |
>10 (LV) 5–10 (SV) |
Yes |
| Health Literacy Assessment Using Talking Touchscreen Technology46 | Prose, document, quantitative | 2011 | Yes | 30 | 18 | Yes |
LV indicates long version; and SV, short version.
Adapted from Haun et al34 with permission. Copyright © 2014, Taylor and Francis, Ltd.
HEALTH LITERACY AND SOCIAL DETERMINANTS OF HEALTH
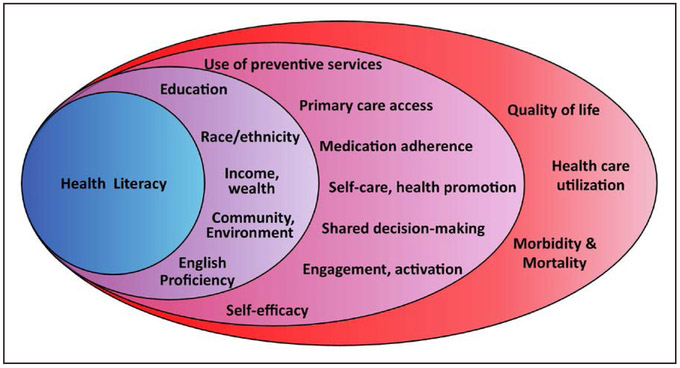
Health literacy extends beyond the clinic- or hospital-based environment where health care is delivered to encompass how individuals approach and navigate self-care and health-related experiences. Social determinants of health are defined by the World Health Organization as “the circumstances in which people are born, grow, live, work, and age, and the systems put in place to deal with illness.”48 Limited health literacy is more prevalent among racial and ethnic minorities, older adults, and individuals with less education.19,24 Likewise, health literacy is strongly related to socioeconomic position, English language proficiency, and the development of general literacy.49 The relationship between health literacy and social determinants of health is portrayed in Figure 1. This figure further indicates the shared associations among health literacy, social determinants, and intermediate and long-term health outcomes.
Figure 1.
Health literacy nested within social determinants of health (education, race/ethnicity, income and wealth, community and environment, and English proficiency), which in turn are associated with a range of intermediate- and long-term healthcare outcomes.
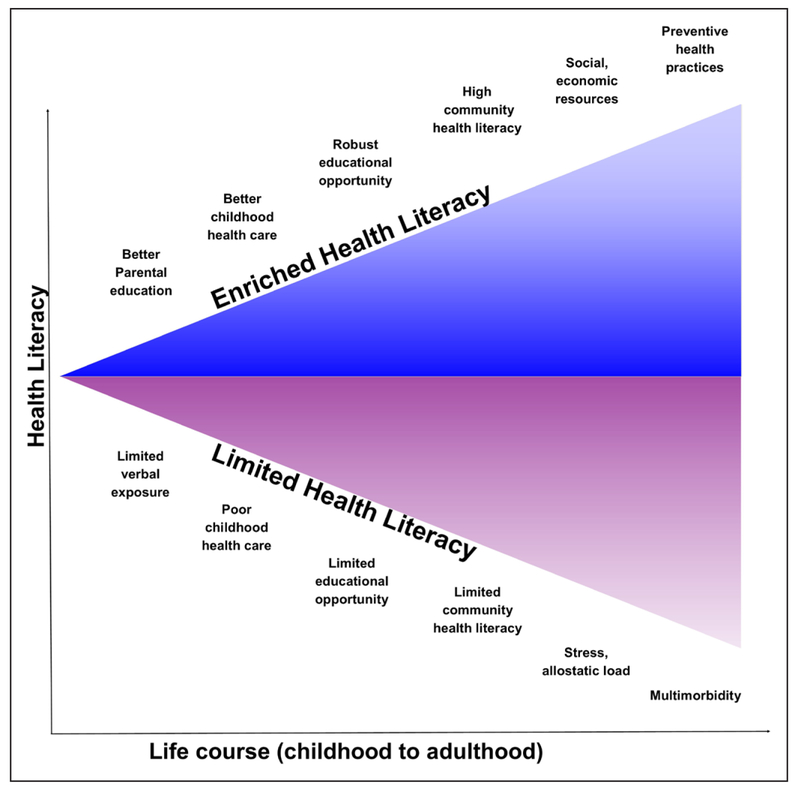
Health literacy may be contextualized in the context of the life course model of risk factors and disease.50–52 Language is critical for self-expression beginning in infancy and is shaped by early childhood exposure to verbal expression, diction, and linguistic content in the home and social arenas. Children of low-income families experience deficits in language exposure and acquisition (described as the “30-million-word gap”) from early infancy.53 In addition, parental health literacy directly affects the preventive care that children receive,54,55 having a direct impact on both childhood health and orientation toward preventive health care.56 Children of parents with limited literacy have been shown to have worse health out-comes. At least 1 in 3 adolescents and young adults has limited health literacy,54 and children with limited literacy tend to exhibit worse health behaviors.57 Older adults have increased risk for limited health literacy for multiple reasons that may include social norms and expectations about health or decline in cognitive function with aging. More important, limited generational opportunities for education may impair general literacy early and throughout life; older adults bear the effects of the absence of standardization in education and the historical racial segregation of the educational environment.52 Educational disenfranchisement in older adults similarly clusters with income and socioeconomic position, both correlated with health literacy. Thus, health literacy both is related to and perpetuates the disparities associated with social determinants of health. Figure 2 presents opportunities for challenges and gains in health literacy across the life course.
Figure 2. Health literacy presented as a life course trait.
Opportunities exist for the enfranchisement or impoverishment of health literacy beginning in infancy and spanning across the life course. Health literacy as encountered in adults reflects myriad familial, community and environmental, and educational influences. This statement emphasizes the overall goal as not correcting health literacy challenges in an individual but implementing approaches toward healthcare communication and delivery that are universally accessible.
The Challenge of Limited Health Literacy
Obstacles to optimal health care for people with limited health literacy occur at multiple levels in healthcare delivery.58 First, individuals with limited health literacy experience challenges in accessing healthcare services. Electronic or paper applications for insurance coverage are complex documents that are not designed for individuals with basic literacy skills. Successfully completing such documentation may be challenging. The details of insurance coverage and accompanying administrative bureaucracy demand a high level of literacy to grasp. The Affordable Care Act and its constituent mandates were critiqued as challenging for many to understand, which may have affected enrollment.59 Second, as consistently documented by an extensive body of literature, all manner of health-related materials exceeds the reading ability of the average US adult.1 Educational brochures and instructions routinely include technical language and complicated explanations of pathophysiology or do not include comprehensible illustrations, making them hard to understand. Despite hundreds of publications about the readability of informed consent documents and patient education materials, most patients cannot read documents intended to empower them. Individuals with limited health literacy may have less access to reliable Internet-based health education materials.60–65
A third challenge for individuals with limited health literacy stems from physician-patient communication. Physicians frequently use medical terminology in their written and oral communication that exceeds the understanding of even highly educated individuals.66,67 Overcoming patient-provider communication barriers remains challenging, particularly for patients with limited health literacy, despite the growing emphasis on improving communication skills in medical school and resident curricula.68 Furthermore, individuals with limited health literacy may not ask fundamental questions or seek to clarify ambiguity69,70; they may have had stigmatizing experiences resulting from limited literacy and have shame about their level of understanding.71,72 A universal precautions approach advocates screening for comprehension of the clinical plan and tailoring treatment to enhance and verify patient understanding.73,74 Such an approach mitigates shaming of individuals with limited literacy and improves healthcare communication by placing responsibility for successful communication with the provider.75
Fourth, patients with limited health literacy must use oral and written communication, integrate complex information, and use numeracy and quantitative skills. For example, medication adherence frequently requires understanding complex scheduling and dosing details, as well as information relating to dietary choices and timing, and appropriate vigilance about symptoms and side effects.
Finally, language and cultural barriers may interfere with healthcare delivery. There is extensive literature on health literacy challenges faced by refugees and immigrants, in addition to individuals with limited English proficiency.76,77 Such populations are vulnerable to poor communication about health-related services.78 Improved access to language-appropriate services is critical. It is also important to understand that overcoming language barriers is simply the first step; mitigating health literacy barriers in interpreted encounters is the next communication challenge to overcome for safe and effective care.
HEALTH LITERACY AND CARDIOVASCULAR RISK AND OUTCOMES
Health literacy has a prominent role in the primary and secondary prevention of CVD. Given the extensive literature, the writing group selected studies that emphasize health literacy in addressing CVD risk and outcomes. Table 3 provides details on studies selected for larger size (n>150, used to focus on larger studies), use of validated measurement of health literacy, and treatment of health literacy as an independent variable that were published from January 2004 through November 2016.
Table 3.
Summary of Selected Studies of Health Literacy and Cardiovascular Risk Factors and Outcomes
| Disease | Authors | Study Design, Setting | N | HL Assessment | Setting | Intervention and/or Main Outcomes |
Follow-Up | Essential Finding, Primary Outcome |
|---|---|---|---|---|---|---|---|---|
| Hypertension | Aboumatar et al70 | Observational, cross-sectional | 275 | REALM | Ambulatory | Involvement, communication, trust, satisfaction | NA | No difference in medical decision making by HL; communication behaviors differed by HL status in asking medical questions. |
| Willens et al79 | Observational, cross-sectional | 23 483* | BHLS | Ambulatory | BP control | NA | No difference in SBP control by HL; lower HL, median SBP, 130 (IQR 120–142) mm Hg; higher HL, SBP 131 (120–142) mm Hg. Difference in DBP by HL: lower HL, 70 (64–79) mm Hg; higher HL, 74 (67–82) mm Hg. | |
| McNaughton et al80 | Observational, cross-sectional | 423 | REALM | Ambulatory | BP control | NA | Limited HL associated with increased risk of uncontrolled BP (OR, 1.75; 95% CI, 1.06–2.87). | |
| McNaughton et al81 | Observational, cross-sectional | 46 263 | BHLS | Hospitalization | BP control | NA | Lower HL: OR, 1.06 (95% CI, 1.01–1.12) compared with higher HL. | |
| Halladay et al82 | RCT | 525 | S-TOFHLA | Ambulatory | BP control | 2 y | Mean SBP decrease at 12 mo: lower HL, 6.6 mm Hg; higher HL, 5.3 mm Hg. At 24 mo: lower HL, 8.1 mm Hg; higher HL, 4.6 mm Hg. Between-group difference not significant at 12 or 24 mo. | |
| Diabetes mellitus | Morris et al83 | Cross-sectional, observational | 1002 | S-TOFHLA | Ambulatory | HbA1c, cholesterol, BP | NA | HL not associated with glycemic control (β, 0.001; 95% CI, −0.01 to 0.01), systolic (β, 0.08; 95% CI, −0.10 to 0.26) or diastolic (β, −0.03; 95% CI, −0.12 to 0.07) BP, or low-density lipoprotein (β, 0.04; 95% CI, −0.27 to 0.36). |
| Cavanaugh et al84 | Observational, cross-sectional | 398 | DNT, REALM | Ambulatory | Glycemic control | NA | Limited HL, less diabetes mellitus knowledge (DNT: median, 40% vs adequate HL, 74%). DNT weakly associated with glycemic control. | |
| Mbaezue et al85 | Observational, cross-sectional | 189 | S-TOFHLA | Ambulatory | Blood glucose self-monitoring | NA | HL not associated with self-monitoring (OR, 1.50; 95% CI, 0.57–3.94). | |
| Sarkar et al86 | Observational, cross-sectional | 14 357 | 3-Item screener | HMO registry | Hypoglycemia | NA | Limited literacy associated with 1.3- to 1.4-fold (95% CI, 1.1–1.7) risk of hypoglycemia. | |
| Brega et al87 | Secondary analysis | 2594 | Print literacy, numeracy | Ambulatory | Mediation analysis, glycemic control | 1 y | Greater HL associated with glycemic control (standardized parameter estimate, −0.070; CI not provided), mediated by multiple factors. | |
| Bauer et al88 | Prospective | 1366 | 3-Item screener | HMO claims data | Adherence to antidepressant medications | 1 y | Inadequate HL increased early (<180 d) and later (≥180–365 d) adherence to antidepressant medications after index prescription date. | |
| McNaughton et al89 | Cross-sectional, Guyanese ED | 228 | SILS | ED presentation | HbA1c | NA | Limited HL: OR, 2.2 (95% CI, 1.2–3.8); HbA1c ≥48 mmol/mol, consistent with undiagnosed diabetes mellitus. | |
| Obesity | Geboers et al90 | Prospective cohort | 3241 | BHLS | Ambulatory | Obesity, health-related behaviors | 1 y | Limited HL, greater obesity risk (OR, 1.35; 95% CI, 1.11–1.63) vs higher HL; limited HL associated significantly with limited physical activity, diet, and alcohol. |
| Lassetter et al91 | Observational, cross-sectional | 364 | NVS | Enrolled at primary care visit | Obesity | NA | Lower NVS associated with increased BMI (r=−0.12). | |
| Lam and Yang92 | Observational, cross-sectional | 1035 | S-TOFHLA | Community-based adolescents | Obesity | NA | Low HL increased obesity risk (OR, 1.84; 95% CI, 1.13–2.99). | |
| Joshi et al93 | Observational, cross-sectional | 739 | HL Management Scale | Mail-based survey | Obesity | NA | Limited HL increased likelihood of self-reported obesity (OR, 1.86; 95% CI, 1.36–2.54) vs higher HL. | |
| Chari et al94 | Observational, cross-sectional | 239 | NVS | Ambulatory | Childhood obesity | NA | Higher parent NVS associated with decreased odds of obese child (OR, 0.75; 95% CI, 0.56–1.00). | |
| Coronary disease | Bailey et al95 | Retrospective | 696 | NVS, S-TOFHLA, REALM | Hospitalization | Readmission | 30 d | After adjustment for demographic and clinical characteristics, the risk of 30-d readmission was 12% lower (P=0.03) and the incidence rate was 16% lower (P<0.01) for patients with above-basic literacy. |
| Gazmararian et al96 | Prospective cohort | 1549 | S-TOFHLA | Ambulatory | Medication adherence | 1 y | Limited HL not related to low refill adherence (OR, 1.23; 95% CI, 0.92–1.64). | |
| Kripalani et al97 | Retrospective | 434 | REALM | Ambulatory | Medication adherence | 6 mo | Limited HL increased risk of low adherence (OR, 1.7; 95% CI, 1.0–3.1) defined by cumulative medication gap. | |
| McManus et al98 | Retrospective cohort | 804 | Single-item screen | Hospitalization, ACS registry | Readmission | 30 d | Limited HL increased readmission risk (OR, 1.75; 95% CI, 1.14–2.69). | |
| ACS and HF | Bell et al99 | RCT | 851 | S-TOFHLA | Hospitalization | ED, readmission | 30 d | Pharmacy intervention reduced event risk in low HL (HR, 0.41; 95% CI, 0.17–1.00). |
| HF | Laramee et al100 | Cross-sectional, observational | 998 | S-TOFHLA | Ambulatory | Association of HF to HL | NA | HF associated with limited HL (OR, 1.55; 95% CI, 1.00–2.41). |
| Murray et al101 | Prospective | 192 | S-TOFHLA | Ambulatory, inpatient | ED visit, hospitalization | 1 y | Adequate HL, lower risk of HF hospitalization (IRR, 0.34; 95% CI, 0.15–0.76). | |
| Macabasco-O’Connell et al102 | Cross-sectional, observational | 585 | S-TOFHLA | Multicenter, ambulatory | HF QOL | NA | Adequate and limited HL, significant differences in HF QOL, knowledge, self-care, and self-efficacy. | |
| Chaudhry et al103 | RCT, secondary analysis | 1464 | REALM-R | Ambulatory | Association of HF to HL by race | NA | Black race associated with worse HL (OR, 2.13; 95% CI, 1.46–3.10), 1.6- to 1.8-fold risk of barriers to care relative to white race. | |
| Peterson et al104 | Retrospective cohort | 1494 | BHLS | Outpatient survey | Hospitalization, mortality | Median, 1.2 (IQR, 0.25–1.25) y | Limited HL, hospitalization HR of 1.04 (95% CI, 0.79–1.37) and mortality HR of 1.61 (95% CI, 1.06–2.43). | |
| Noureldin et al105 | RCT, secondary analysis | 281 | S-TOFHLA | Hospitalization | Adherence intervention | 9 mo | Differences in adherence in usual care (15.2%; 95% CI, 6.04–24.3) and pharmacy intervention (12.0%; 95% CI, −0.3 to 24.4) by HL. | |
| Dewalt et al106 | Multisite RCT | 605 | S-TOFHLA | Ambulatory | Single session vs multisession patient support | 12 mo | Limited HL, trial participants had adjusted IRR of 0.73 (95% CI, 0.39–1.36) favoring multisession vs single-session group. | |
| HF (Continued) | Wu et al107 | Multisite RCT | 595 | S-TOFHLA | Ambulatory | Medication errors | NA | Higher HL (OR, 0.84; 95% CI, 0.74–0.95) and subjective numeracy (OR, 0.77; 95% CI, 0.63–0.95) reduced medication error. |
| Mixon et al108 | Prospective cohort | 471 | S-TOFHLA | Hospitalization | Medication errors | NA | Higher HL (OR, 0.84; 95% CI, 0.74–0.95) and subjective numeracy (OR, 0.77; 95% CI, 0.63–0.95) reduced medication error. | |
| McNaughton et al109 | Retrospective, hospital-based | 1379 | BHLS | Hospitalization | ED visit, hospitalization, mortality | 20.7 (12.8–29.6) mo | Limited HL, HR, 1.32 (95% CI, 1.05–1.66) for mortality vs higher HL; no association between HL and ED visit or hospitalization. | |
| Moser et al110 | Prospective cohort | 575 | S-TOFHLA | Hospitalization or ambulatory | HF hospitalization, mortality | 2 y | Inadequate HL, HR, 1.66 (95% CI, 1.16–2.39) combined outcome relative to adequate HL. | |
| Wu et al111 | Secondary analysis, RCT | 575 | S-TOFHLA | Hospitalization or ambulatory | Mediation by HL for age and hospitalization, cardiac death | 2 y | Older (≥65 y) individuals 3 times more likely to have limited HL; HL mediates age and outcomes in HF. |
Studies were selected for size (n>150), use of validated HL assessments, treatment of HL as an independent variable, and publication from January 2014 through November 2016. ACS indicates acute coronary syndrome; BHLS, Brief Health Literacy Survey; BMI, body mass index; BP, blood pressure; CI, confidence interval; CVD, cardiovascular disease; DBP, diastolic blood pressure; DNT, Diabetes Numeracy Test; ED, emergency department; HbA1c, glycated hemoglobin; HF, heart failure; HL, health literacy; HMO, health maintenance organization; HR, hazard ratio; IQR, interquartile range; IRR, incidence rate ratio; NA, not available; NLS, Nutritional Literacy Scale; NVS, Newest Vital Sign; OR, odds ratio; QOL, quality of life; r, correlation coefficient; RCT, randomized controlled trial; REALM, Rapid Estimate of Adult Literacy in Medicine; REALM-R, Rapid Estimate of Adult Literacy in Medicine–Revised; SBP, systolic blood pressure; SILS, Single-Item Literary Screener; and S-TOFHLA, Short Test of Functional Health Literacy in Adults.
Indicates 23 483 encounters in 10 644 individuals.
Hypertension and Health Literacy
Health literacy has had robust investigations in hyper-tension.79–81,112 Health literacy is related to recognition and knowledge of hypertension. A cross-sectional study of 402 patients from 2 racially diverse and geographically distinct public, urban healthcare facilities found that the majority (55%) of individuals with inadequate health literacy were not able to recognize a blood pressure of 160/100 mm Hg as abnormal.113 The finding is particularly relevant in that knowledge of blood pressure targets has been related to effective management of hypertension.114 In urban ambulatory care cohorts, individuals with limited health literacy had a 1.8 to 2.7 times increased risk of not achieving guideline-based blood pressure recommendations.80,115 Limited studies have examined the effect of patient-centered interventions integrating health literacy on blood pressure control. A multisite trial (the Heart Healthy Lenoir Study) conducted in 6 primary care practices over 24 months found that a multilevel intervention improved systolic blood pressure among patients across health literacy levels.82
Patient-centered interventions have addressed limited health literacy to improve medication adherence in hypertension. Adherence is a complex, multilevel concept; its constructs and the relevance of social determinants of health, including literacy, to medication adherence in patients with hypertension have been evaluated by a systematic review and meta-analysis.116,117 The aim of such interventions is to address patient misunderstanding of prescription instructions and unintentional misuse of medications to which individuals with limited health literacy are particularly vulnerable.118,119 A 2-arm multisite trial (n=845) used patient-centered drug labeling, recognized by the study team as an inexpensive and simple modification, to improve adherence to blood pressure and diabetes mellitus medications. The intervention improved adherence in study participants with inadequate literacy 4-fold, by self-report, and 5-fold, by pill count, compared with the standard care referent cohort.120 A small (n=68) study composed predominantly of participants with limited health literacy identified that aids, such as flashcards and smartphone-activated videos, improved medication adherence.121 These strategies indicate that simplified regimen administration, use of aids, and multilevel interventions can improve blood pressure control in individuals with limited health literacy.
There are continued gaps in the investigation of health literacy and hypertension. Few studies have measured health literacy as a covariate. Inclusion of health literacy as a measure in large, prospective, community-based cohort studies would facilitate exploring the prospective short- and long-term effect of health literacy on hypertension and blood pressure control. Inclusion of health literacy measurement in clinical trials may provide insight into how health literacy may modify adherence in a trial, as well as provide an assessment of generalizability to individuals with limited health literacy who are less likely to participate in clinical trials.
In addition, multidisciplinary and multilevel interventions are needed to improve blood pressure control in individuals with hypertension and limited health literacy. Healthcare providers and health systems should collaborate to provide patient materials and to use strategies that mitigate the effects of limited health literacy.122 For example, strategies that promote patient-provider communication82 and foster patient empowerment may improve medication adherence.123 Community-based interventions can leverage resources such as neighborhood pharmacies to promote blood pressure screening, monitoring, and adherence. Multifaceted interventions that incorporate patients, providers, and health systems are essential to address health literacy barriers and to promote patient empowerment and success with long-term hypertension management.
Diabetes Mellitus and Health Literacy
Success for the patient with diabetes mellitus requires an array of skills integral to health literacy: interactional, numeracy, information seeking, application/function, decision making, confidence, and navigation. Specific components of diabetes mellitus in which health literacy has been best evaluated are social and cognitive factors, including diabetes mellitus knowledge,124 self-efficacy125,126 or activation,127 and attitudes or beliefs,128 and self-care,84 spanning the range of activities that relate to diabetes mellitus management, including diet, physical activity, medication and treatment adherence, and problem solving. Health literacy has also been linked to outcomes relevant to diabetes mellitus such as glucose control and microvascular complications.129,130 The literature describing these associations between health literacy and diabetes mellitus was well evaluated and summarized in 2014 by Bailey et al.131 Limited health literacy has been related to decreased access to healthcare screening and basic services and therefore has been implicated in diabetes mellitus risk.132
Diabetes mellitus is a chronic disease that requires consistent health behaviors guided by specific knowledge of the condition and its treatment.128 A systematic review identified consistently strong evidence that health literacy is associated with diabetes mellitus knowledge.130 One study (n=2594) characterized Indians and Alaskan Natives as having limited social and economic resources and identified a strong relation between health literacy and diabetes mellitus knowledge that adversely affected dietary behaviors in this vulnerable cohort with significant social and economic challenges.87 The study authors concluded that diabetes mellitus knowledge is a central component of addressing diabetes mellitus care in individuals with inadequate health literacy. Conversely, decreased health literacy in a single-center cohort of individuals (n=280) with poorly controlled diabetes mellitus (hemoglobin A1c levels >8%) was related to poor knowledge; individuals in the lowest health literacy tertile were 4-fold more likely to assert that their diabetes mellitus was well controlled, despite a hemoglobin A1c >8.0%, than those in the referent tertile.133 The importance of health literacy as a parental trait is demonstrated by its impact on parents of children with type 1 diabetes mellitus; adults with limited health literacy face the challenge of knowledge gaps in providing care for their children.134,135
Observational studies have related health literacy to diverse and varied behaviors that make up diabetes mellitus self-care,131 including associations between health literacy and adherence to both diabetes mellitus and nondiabetes mellitus medication.84,88 Health literacy has been demonstrated to mediate the racial disparities in adherence to diabetes mellitus medications observed in a biracial (black and white; n=398) cohort.136
The electronic patient portal is increasingly used to augment self-care in diabetes mellitus and other chronic diseases. Analysis of a large health maintenance organization found that members with limited health literacy were 1.7 times less likely to use the electronic patient portal for communication and disease management than members with adequate or higher health literacy.137 Multiple studies have related health literacy to patient engagement, activation, and self-efficacy,3,138,139 with some demonstration that health literacy may facilitate or mediate patient activation and diabetes mellitus management.140,141 The range of studies indicates the types of health literacy skills (Table 1) that are needed for self-care among patients with diabetes mellitus.
Evidence about the relation of health literacy and glycemic control is mixed, which may be explained by variation in how potential confounders are handled in analysis. Similarly, health literacy has had varied associations with cardiovascular risk factors and clinical outcomes specific to diabetes mellitus. In a large cross-sectional study, health literacy was not associated with cardiovascular risk factors (systolic and diastolic blood pressures and low-density lipoprotein) or self-reported complications (retinopathy, nephropathy, CVD) in individuals with diabetes mellitus.83 However, in an urban patient cohort, individuals with inadequate health literacy had a 2-fold increased risk of retinopathy, as determined by self-report and confirmed by administrative data.129 The committee is not aware of studies examining the association of health literacy with adjudicated cardiovascular outcomes such as coronary or other cardiovascular events in individuals with diabetes mellitus. Understanding health literacy and prospective, long-term complications associated with diabetes mellitus would be enhanced by introducing health literacy assessments to established, well-characterized community-based cohort studies.
Health literacy has been incorporated into a range of interventions to improve outcomes in individuals with diabetes mellitus, particularly those with educational, social, and economic vulnerabilities.142–145 Strengths have been the outreach to economically and socially disadvantaged individuals, particularly Spanish-speaking adults, and 12-month follow-up to assess for sustained improvements in outcomes relevant to diabetes mellitus. Swavely et al143 reported improvement in diabetes mellitus knowledge and limited but statistically significant 12-month improvement in hemoglobin A1c (7.98±1.4% to 7.43±1.4%). A randomized trial used multidisciplinary care with enhanced, individualized communication targeting comprehension of diabetes mellitus knowledge and self-care.144 Of individuals with limited health literacy, those receiving the intervention had significant success in achieving diabetes mellitus control, defined as reaching a target hemoglobin A1c ≤7.0% (42% vs 15% of those receiving standard care). In contrast, individuals with higher health literacy receiving the intervention showed rates of success comparable to those receiving standard care. An educational intervention tailored for low-income Latinos with diabetes mellitus demonstrated a 4-month improvement in glycemic control.145 Of note, the improvement was not sustained at 12 months. These results suggest that multidisciplinary and culturally appropriate interventions that mitigate health literacy–related barriers are needed to achieve sustainable results.
Health literacy in individuals with limited English proficiency and immigrant cohorts has received increased focus.146 Selected studies have examined health literacy using qualitative and quantitative methods to investigate the relationship between health literacy and diabetes mellitus knowledge, acculturation, and access to care.147–150 However, interventions that improve access to language-appropriate services and health literacy support for patients with limited English proficiency are needed.151
Obesity, Diet, and Health Literacy
Health literacy informs health-related knowledge and self-efficacy, which are essential for the promotion of healthy behaviors such as physical activity and general health maintenance.152 The literature consistently demonstrates the association between health literacy and obesity, dietary choices, and exercise.153–155 In Spanish-speaking individuals in the United States with limited English proficiency, higher health literacy has been related to increased exercise and fruit and vegetable consumption.153 A study of rural, low-income, predominantly black, high school–educated adults identified a significant association between Healthy Eating Index scores and health literacy and an inverse correlation between health literacy and sugar-sweetened beverage intake.155
Educational programs aimed at dietary changes for individuals with limited health literacy have been demonstrated to affect caloric consumption significantly. A 6-month educational intervention used health literacy-focused strategies to decrease consumption of sugar-sweetened beverages (227 kcal/d) and show an improvement in body mass index in a medically underserved lower-income community.156 It remains unknown how mobile and electronic technologies can best support dietary and exercise interventions in individuals with limited health literacy.157
In elementary school–aged children, limited parental health literacy is associated with a 25% increased risk of obesity.94 Parents with limited health literacy are twice as likely to perceive their overweight child as being normal weight, and obesity in adolescents correlates with the adolescent’s health literacy.94 Health literacy may constitute a barrier to childhood physical activity.158 Community-based interventions such as the Greenlight program have been designed to address the role of health literacy in childhood obesity and nutrition.159
There are significant opportunities for developing programs to address health literacy challenges in relation to obesity and diet. Community- and school-based educational programs provide avenues for educating youth in communities vulnerable to limited health literacy. The life course impact of limited health literacy on obesity merits examination. Making weight loss, exercise, and diet education programs accessible and available to individuals with limited health literacy is essential. Interventions and programs that incorporate mobile health offer novel opportunities but must be developed so that health literacy is not a barrier for participation.
Tobacco Use and Health Literacy
The interrelation of health literacy, socioeconomic and demographic factors, and tobacco use and cessation is complex.160 In an urban, multiracial cohort (n=402), limited health literacy was related to increased risk of nicotine dependence and decreased knowledge deficits of smoking-related health risks.161 In the same cohort, researchers found that individuals with limited health literacy were 3.2 times more likely to suffer a relapse in smoking after a cessation program.162 The number of studies focusing specifically on health literacy and tobacco use is limited. However, the findings demonstrate the relevance of incorporating health literacy into tobacco treatment and cessation programming. These findings are consistent with the overall findings presented in this statement that health literacy is associated with health-related self-care and healthier lifestyle and behaviors.
Coronary Heart Disease and Health Literacy
The authors of this statement identified only a limited number of studies that examined health literacy as an independent variable in relation to cardiovascular risk, incident cardiovascular events, and strategies to improve or augment secondary prevention after cardiac events. Nevertheless, health literacy has been associated with poorer outcomes preceding and following coronary events. In a hospital-based registry of 1967 patients (1197 [60.9%] with acute coronary syndrome), limited health literacy and numeracy proficiency were associated with decreased adherence to medications preceding admission.163 Health literacy has likewise been associated with 30-day readmission after acute coronary syndromes.95 Medicare enrollees with literacy levels determined as above basic had a 12% reduced risk of readmission than those with basic or below-basic literacy.
To date, interventions addressing health literacy in individuals with CVD have focused primarily on medication adherence, including pharmacy-led interventions that prompt medication refills and graphic illustrations that promote accurate and timely medication taking.164,165 One systematic review166 found that the use of pictorial aids may enhance patients’ understanding of how to take medications, especially when combined with other patient education, either written or oral. However, results are mixed. The IMAGE-CHD study165 (Improving Medication Adherence Through Graphically Enhanced Interventions in Coronary Heart Disease) compared the effects of 2 low-literacy interventions (illustrated medication schedules and refill reminder postcards) on medication adherence in an underserved population with CVD (n=435; mean age, 63.7 years; 91% black; 78% reading below the ninth-grade level). Subjects were randomly assigned to refill reminder postcards, illustrated medication schedules, both interventions, or usual care for 1 year. Post hoc subgroup analyses suggested that illustrated medication schedules may be a useful approach among patients with low medication self-efficacy, polypharmacy, or baseline nonadherence. In the multisite PILL-CVD trial99 (Pharmacist Intervention for Low Literacy in Cardiovascular Disease), the effects of a pharmacist-assisted intervention focused on medication recon-ciliation, inpatient pharmacist counseling, low-literacy adherence aids, and tailored telephone follow-up after discharge from healthcare use were examined in a sample of 851 patients with acute coronary syndrome and decompensated heart failure. The intervention had benefit in individuals with inadequate health literacy, reducing 30-day risk of healthcare use by 59% in the intervention cohort (hazard ratio, 0.41; 95% confidence interval [CI], 0.17–1.00). The results suggest that a multifaceted approach targeting individuals with limited health literacy may be useful in improving healthcare outcomes.
Few studies have addressed the complexity of CVD treatment regimens for patients with limited health literacy; the authors of this statement found crucial gaps in the literature. Studies examining health literacy and CVD outcomes beyond 30-day readmission are essential. Multicenter trials with longer periods of follow-up are needed to clarify how interventions incorporating health literacy are associated with CVD events. Furthermore, studies in individuals of limited English proficiency are needed, given the multiple challenges of adherence, knowledge, self-care, and activation. Finally, health literacy can be evaluated as part of programs aiming to reduce CVD risk and to improve secondary prevention. For example, limited health literacy may be 1 factor that influences dropout rates in cardiac rehabilitation.166 Individuals with limited health literacy may experience barriers to referral to, engagement with, and participation in cardiac rehabilitation services and thus miss the physiological and nonphysiological benefits after coronary events.
Congestive Heart Failure and Health Literacy
Limited health literacy is highly prevalent in individuals with heart failure, and the relation of health literacy to heart failure outcomes has been confirmed in diverse studies. A systematic review of 20 unique studies of health literacy and heart failure identified the average prevalence of limited health literacy as 39% across all studies (range, 19%–61%).168 In individuals with heart failure, limited health literacy has been associated with 1.3- to 2-fold higher all-cause mortality in hospital and community-based cohorts.104,109 In individuals with heart failure presenting to the emergency room, limited numeracy has been related to 40% greater likelihood of returning to the hospital within 30 days.169 These data indicate that health literacy strongly contributes to adverse outcomes in heart failure.170
Health literacy has likewise been identified as a barrier to successful self-care in heart failure. Matsuoka et al171 identified “critical” health literacy (ie, health literacy challenges related to the cognitive ability to evaluate and process information172) as related to symptom monitoring and management for self-care in individuals with heart failure. Individuals with limited health literacy have less heart failure knowledge and decreased capacity for the self-care activities essential for heart failure.102 Health literacy is likewise an independent determinant of successful self-care behaviors used to assess treatment options and to make decisions.171
Interventions to improve health literacy in individuals with heart failure have been diverse and varied. Strategies have included use of low-literacy and standardized materials and implementation of clinician follow-up.173–175 One program used graphic illustrations to provide education and targeted symptom monitoring.176 Pictures included common avenues for patient engagement in heart failure self-assessment such as monitoring for weight gain and assessing for ankle edema. An intervention (n=123) using a self-management program designed for individuals with limited literacy reported a reduced rate of all-cause hospitalization; however, differences in hospitalization for heart failure and quality of life did not reach statistical significance when the intervention group was compared with control cohorts at the 12-month follow-up.177 A multisite comparative effectiveness trial (n=605) evaluated single-session versus multisession telephone-based intervention and found an effect by literacy status for the secondary outcome of all-cause hospitalization: Individuals with limited health literacy receiving the multisession intervention were less likely to require hospitalization (incidence rate ratio, 0.48; 95% CI, 0.24–0.92).106
A common theme is that education may improve behaviors such as adherence, dietary choices, and lifestyle modification; enhance monitoring for symptoms; and avoid clinical decompensation.178 Health literacy is integral to clinical education about patient monitoring and self-assessment. Interventions that incorporate health literacy as a risk factor for adverse outcomes and a barrier to dietary and medication adherence may benefit from multidisciplinary strategies.173,179 A critical next step is implementation research to learn how to bring the benefits of patient education and empowerment for self-care among patients with heart failure to broader populations.
Stroke and Health Literacy
Health literacy related to stroke includes knowledge of risk factors for stroke prevention and recognition of warning signs for acute stroke therapy. Stroke pre-paredness is the timely recognition of stroke symptoms and onset. Population-based studies have identified racial disparities in stroke preparedness,180 but how health literacy contributes to disparities in stroke recognition and knowledge has had limited examination. Because rapid intervention is essential for improved outcomes in stroke treatment, initiatives have focused on improving stroke literacy. Examples include the TLL Temple Foundation Stroke Project, a rural behavioral intervention181; the Cincinnati, OH, efforts, based in beauty parlors, to convey culturally meaningful stroke education182; Hip Hop Stroke, targeting black elementary school children by incorporating culturally relevant music183; and a community-based trial targeting Mexican American middle school-aged children in which students who received the intervention demonstrated greater stroke literacy than a referent cohort who did not.184
Health literacy related to stroke symptoms and signs remains poor, with low recognition of cardinal stroke symptoms and awareness of acute treatments.185–187 Interventions developed for individuals of limited health literacy have consistently shown improvement in knowledge and recognition of stroke signs and symptoms.182,188–190 A community-based intervention conducted in churches reported that stroke knowledge and behavioral response were improved with presentation of stroke vignettes.191 The studies cited here demonstrate the opportunities for enhanced stroke education that is delivered with culturally appropriate vehicles. The interventions target families and children to empower and prompt rapid action for stroke recognition. Moving forward, programs to prevent stroke and improve stroke preparedness should promote awareness that stroke is imminently preventable and treatable.
Atrial Fibrillation and Health Literacy
Treatment of the complex syndrome of atrial fibrillation (AF) involves education, decision making, and long-term adherence. Health literacy is correlated with education and socioeconomic position, and these factors may be associated with medication and behavioral adherence, communication about symptoms, health-related quality of life, access to and experience of care, and outcomes relevant to AF (hospitalization, stroke, heart failure, cognitive and physical decline).
Individuals with limited health literacy are particularly vulnerable to having a limited knowledge of AF and its treatments. In an international survey of physicians (11 countries, n=810), 46% described their patients as unable to explain what AF is and indicated that more than half of their patients needed more information about the condition.192 In a health maintenance organization, individuals with AF and inadequate health literacy, as assessed by a 3-item screening instrument, were shown to have decreased awareness of AF (prevalence ratio, 0.96; 95% CI, 0.94–0.98).193 Knowledge about AF was shown to be directly correlated with level of education in a single-center cohort.194 Only <10% of those receiving care (n=183) were able to report the indication for anticoagulation; those with inadequate health literacy had a 5-fold increased risk of not understanding the indication for warfarin.195
Unfortunately, one-off educational sessions as an intervention may have limited impact on patient knowledge, given that retention has been reported as poor.196,197 Cochrane analyses identified a small number of studies (n=8–11) evaluating the effect of educational and behavioral interventions on anticoagulation as measured by improvement in time in therapeutic range and did not identify sufficient evidence that such interventions affect time in therapeutic range in individuals with AF.198,199 However, a subsequent, limited-size (n=97) multimodality intervention demonstrated a 6-month improvement in time in therapeutic range that was not sustained to 12 months.200 A large clinical trial showed 12-month improvement in adherence to guidelines-based care and reduced hospitalization by implementing a nurse-led, multidisciplinary intervention.201 Consistent with other CVD risk factors and outcomes discussed here, multidisciplinary approaches may provide opportunities for continued reinforcement of educational programming to facilitate improved AF care. By necessity, to succeed, such interventions must adopt the universal precautions approach to be accessible across the health literacy spectrum.
Ongoing challenges in evaluating health literacy and AF are multiple. There has been limited investigation into how health literacy may influence evaluation and treatment in AF. For the individual, the AHA/American College of Cardiology/Heart Rhythm Society guideline on treatment of AF emphasizes the recognition and treatment of symptoms.202 The extent to which health literacy may influence how individuals report and monitor symptoms requires further examination. Shared decision making has relevance for AF because of the multiple decision points that may significantly influence the course of treatment,203 but tools and strategies need to be accessible across the spectrum of health literacy. Community- and institution-based cohorts can further our understanding of health literacy and its relation to adverse outcomes in AF. Individuals with limited health literacy and AF may experience worse outcomes and have decreased access to treatments and specialized care. Rather than seeking to tailor treatment by health literacy level, centers or hubs of AF care should adapt strategies that facilitate access to care and patient support regardless of health literacy level. The ongoing challenge for institutions is to develop as health-literate organizations in their care for those with AF and other cardiovascular conditions.204
INTEGRATING HEALTH LITERACY INTO CARDIOVASCULAR RISK TREATMENT AND PREVENTION PROGRAMS
Integrating the AHRQ Universal Precautions Toolkit into Cardiovascular Care
The AHRQ Universal Precautions Toolkit for Health Literacy,18 or Toolkit, is a publicly available document focused on improving quality of care. The Toolkit advocates an orientation to health literacy consistent with the universal precautions approach: best practices, instituted without exception, to provide a uniform, coherent standard of care.73–75 Consequently, the goal is not to tailor patient instructions, teaching, approach to care, or shared decision making according to individual patients’ level of health literacy. Rather, the objective is to develop and maintain a best practices approach—universal precautions—in written and oral encounters with patients. To emphasize, the objective of the Toolkit and health literacy advocacy is to provide practical approaches for clear oral and written communication to help patients better understand their health information.
The Toolkit includes a 21-step approach to implement a health literacy improvement plan that is scalable for healthcare delivery of any size and context. Fundamentally, healthcare providers who listen, speak slowly, use nonmedical language, encourage questions, apply teach-back methods, and integrate the use of graphics or models are creating a culture of patient care that is sensitive to health literacy. Table 4 presents the components of the AHRQ Toolkit with examples for their implementation in cardiovascular care, including primary and secondary prevention. The authors of this statement advocate the systematic adoption of the Toolkit as a resource for integrating health literacy in CVD prevention and management. Integrating Toolkit principles of being attentive to health literacy is practical and sensible. Cardiovascular centers can create health literacy-sensitive educational and consent materials; provide health literacy-appropriate education materials in waiting rooms and websites; and teach health literacy-attentive communication to practices.205
Table 4.
AHRQ Health Literacy Universal Precautions Toolkit18 Components and Modification for Integrating Health Literacy Into Cardiovascular Care
| Tool | Title | Applications for Cardiovascular Prevention and Management |
|---|---|---|
| 1 | Form a Team | Develop a team of multidisciplinary stakeholders (eg, primary care, geriatric, and cardiology representatives) to promote best practices for HL |
| 2 | Create a Health Literacy Improvement Plan | Construct a plan with explicit short-and long-term goals for addressing HL challenges in the care of CVD |
| 3 | Raise Awareness | Educate staff about HL and challenges of HL relevant to CVD |
| 4 | Communicate Clearly | Use plain language, avoiding jargon; review consents for reading level; adopt the patient’s words; integrate pictures to teach about testing, disease states |
| 5 | Use the Teach-Back Method | Document teach-back and use to demonstrate quality improvement in patient engagement and education |
| 6 | Follow-Up With Patients | Involve patient in monitoring (eg, symptoms and adherence tracking) |
| 7 | Improve Telephone Access | Implement universal precautions to facilitate patient-centered communications |
| 8 | Conduct Brown Bag Medicine Reviews | Review all medications as a standard for quality patient care; develop logs to assess adherence routinely with patients; implement pharmacist collaborators |
| 9 | Address Language Differences | Conduct education, assessments, and testing with a trained interpreter |
| 10 | Consider Culture, Customs, and Beliefs | Receive training in cultural competence; remember the patient’s expertise in the intersection of culture and beliefs with CVD and other medical care |
| 11 | Assess, Select, and Create Easy-to-Understand Materials | Evaluate forms, informed consents, procedural brochures for readability |
| 12 | Use Health Education Material Effectively | Create information order sets or collected materials on CVD treatment options |
| 13 | Welcome Patients: Helpful Attitude, Signs, and More | Use the environment to promote questions and medication review |
| 14 | Encourage Questions | Invite questions routinely on CVD, patients’ experience with disease and treatments |
| 15 | Make Action Plans | Have patients choose realizable goals (eg, medication adherence, or addressing risk factors for AF, such as smoking, physical activity, blood pressure control) |
| 16 | Help Patients Remember How and When to Take Their Medicine | Facilitate tools to support medication use; educate patients on systems for tracking medication; anticipate errors; provide tools such as pill boxes |
| 17 | Get Patient Feedback | Use patient expertise on being a patient through surveys and suggestions |
| 18 | Link Patients to Non-Medical Support | Use community-based resources |
| 19 | Direct Patients to Medicine Resources | Review insurance coverage and verify eligibility; integrate case management |
| 20 | Connect Patients With Literacy and Math Resources | Discern how HL affects patients’ lives and experience; identify and integrate community resources |
| 21 | Make Referrals Easy | Make sure the patient understands the referral rationale; provide timely and relevant feedback when consulting |
AF indicates atrial fibrillation; AHRQ, Agency for Healthcare Research and Quality; CVD, cardiovascular disease; and HL, health literacy.
Impact of Health Literacy on Cardiovascular Treatment and Care
Individuals with CVD are expected to adhere to complex medication and dietary regimens and to make decisions about how to respond to symptoms.206 The current literature has explored the association of health literacy and self-care of CVDs, which encompasses treatment adherence and symptom monitoring, and early response to symptoms when they occur.178 In general, adequate self-care has been shown to improve cardiovascular outcomes, including improved quality of life and symptom burden and reductions in hospitalizations and mortality.178,207–209 However, despite the availability of patient education, self-care remains especially challenging for those with limited health literacy.210
Health literacy in individuals with CVD includes the ability to understand medication instructions, discharge and appointment forms, and education materials (eg, dietary instructions), as well as the ability to negotiate complex healthcare systems.211 People with cardiovascular risk factors and CVD are aided by skills in reading, listening, analytical thinking, and decision making, as well as the ability to apply these skills to their specific health situation.1 Finding ways to support people who do not have advanced skills in these areas is the challenge posed by the field of health literacy because this literature shows the injustice of designing complex systems that work only for people with high levels of education and empowerment.212 Inattention to the unneeded complexities in our jargon-filled communications is not a safe or particularly effective approach to patient care and contributes to health disparities.
Adequate health literacy is associated with a higher level of understanding of medications and lifestyle modifications in populations with diabetes mellitus and congestive heart failure. This effect may be mediated by self-efficacy, which allows patients to take ownership of their treatment when they understand the rationale for each strategy. Adequate health literacy also allows patients to avoid medication errors and manage polypharmacy, to understand which symptoms may be caused by CVD and initiate timely response as instructed, and to report side effects that could affect outcomes. Furthermore, self-efficacy, patient engagement, and shared decision making have been increasingly promoted as approaches to enhance care. The writing group for this statement recognizes that work is needed to refine intervention models to attain sustained and generalizable results.
Health Literacy and Participation in Clinical Research
A basic tenet outlined in bioethics principles of clinical research and codified in the Belmont report is respect for individuals with the associated requirement that patients are adequately informed about the nature of research and the voluntary nature of participation.213 For multiple reasons, limited health literacy has been strongly associated with lower participation rates in clinical research.214 Limited health literacy may be associated with researchers not offering participation in studies because of a perception of lower understanding of the risks and benefits of research or a concern that follow-up or adherence could be compromised. The nature of the informed consent document may be such that the complexity of the language could be a barrier to participation, and distrust of the healthcare system may play an important role. Alternatively, when individuals with limited health literacy are informed about the nature of research in a culturally tailored manner and given the opportunity to participate, their enrollment rates may be similar to those of individuals with higher health literacy.
The study by Ownby et al215 evaluated the association between health literacy and understanding orally presented informed consent information in a sample of 334 English- or Spanish-speaking participants. Health literacy, numeracy, education, and the interaction of health literacy and education accounted for 29% of the variability in performance scores. This suggests that other demographics (eg, race, ethnicity, sex) may not be as important as health literacy and education.
The problem of health literacy and informed consent is highlighted by the cross-sectional study by Paasche-Orlow et al216 that examined the Institutional Review Board (IRB) readability standards and informed consent form templates of 114 US medical schools. Using documents accessed from the schools’ websites, the study reported that readability varied widely from the 5th to 10th grade (mean, 10.6; 95% CI, 10.3–10.8). The mean Flesch-Kincaid score, a commonly used measure of readability,217 for sample text provided by IRBs exceeded stated standards by 2.8 (95% CI, 2.4–3.2) grade levels, illustrating that typical informed consent material likely challenges those with limited health literacy. In 2013, Paasche-Orlow et al218 updated the analysis of informed consent form templates (sample n=109) and reported a mean readability level of 9.8 (95% CI, 9.4–10.2), representing a significant improvement from or lower mean readability level (P<0.0001) compared with the earlier study. Similarly, there was a slight improvement in consistency of the sample text with IRB standards (mean improvement, 2.2 grade levels; 95% CI, 1.7–2.8). However, most of the Health Insurance Portability and Accountability Act sample content did not reach IRB standards, exceeding the targeted standard by a mean of 4.2 (95% CI, 3.4–5.0) grade levels.
There are several recommendations to address the informed consent challenges faced by those with limited health literacy. First, informed consent documents should meet IRB readability standards, especially the most complex portions like the Health Insurance Portability and Accountability Act material. For many individuals, these standards may still be challenging, so tailoring the informed consent to participants’ health literacy level is recommended.215 Alternative strategies for ensuring confirmability of informed consent include the teach to goal approach219 and the Brief Informed Consent Evaluation Protocol, which uses a telephone interview after consent process.220 Results of the ePRISM study221 (Patient Risk Information Services Manager), which generated personalized consent forms that were based on a patient’s specific clinical risk, suggest that a personalized consent document can improve the patient’s understanding of the purpose and risks of procedures, engage patients in shared decision making, and thus improve process of informed consent.
Strategies and Future Directions for Incorporating Health Literacy for Vulnerable Populations
Improving health literacy among those at highest risk and with the lowest economic resources poses a unique challenge. The use of health information technology, including mobile apps to improve self-care behaviors in patients with CVD and to prevent CVD risk by promoting healthy behaviors, is on the rise222 and may be beneficial in individuals with limited health literacy. However, for individuals who cannot afford a smartphone or who have inconsistent Internet connections, those benefits are unlikely to permeate. Use of mobile health platforms may present an attractive option for patient-oriented education, text messages, and social networking to help with chronic disease management. However, a mobile health intervention study found that those least engaged with text messaging and automated calls were racial or ethnic minorities, older adults, and those with limited health literacy.223 This result suggests that reliance on mobile health solutions to mitigate health literacy concerns has the potential to exacerbate disparities in vulnerable populations; the “health literacy divide” may reinforce what has been described as the “digital divide.”21
Several investigators have explored novel mechanisms for improving CVD-related health literacy. An important component of these interventions is that an understanding of limited health literacy does not exist in isolation with poverty but that other barriers to communication exist, including language and culturally appropriate messaging.224 For example, promising avenues for improving knowledge of stroke signs and symptoms have involved the use of hairstylists to deliver health messages in predominantly black populations,182 houses of worship for Spanish-speaking patients,225 and hip-hop music to educate urban, school-aged children.189,226 The use of novel avenues of communication such as case vignettes of possible patients reflective of the community may also be an additional culturally tailored approach.191
Multidisciplinary interventions have incorporated nonmedical providers such as pharmacists and community health workers to address health literacy challenges in CVD, with successful improvement in outcomes.227–230 Common themes emerge in several of these interventions, which hold the potential for generalizability to other settings. First, such interventions are community centered and address barriers to care that are specific to individual communities. Such insight may provide a starting point for launching broader interventions that account for health literacy as a barrier to improved CVD screening, prevention, and management. Second, interventions that incorporate health literacy tend to be further enriched by accounting for other social determinants of health: the economic, cultural, language, and other social barriers that obstruct public health implementation.
Toward a Health-Literate Cardiovascular Organization and Program
This statement has articulated how limited health literacy may contribute to increased risk for a range of cardiovascular risk factors and conditions. Individuals with limited health literacy face challenges in accessing and navigating health care, and such obstacles may be exacerbated by family, community, and social factors. Health literacy is a ubiquitous challenge throughout any healthcare system, particularly because only 12% of US adults have the health literacy skills to navigate its complexity successfully.24 Health literacy interfaces with the electronic portal, the physical layout and use of signage for directions, patient instructions, informed consent, the discharge plan, and the complex multitude of communication with patients and their families. The systemic challenge is, therefore, to develop healthcare systems that are accessible and for which health literacy is not an obstacle.
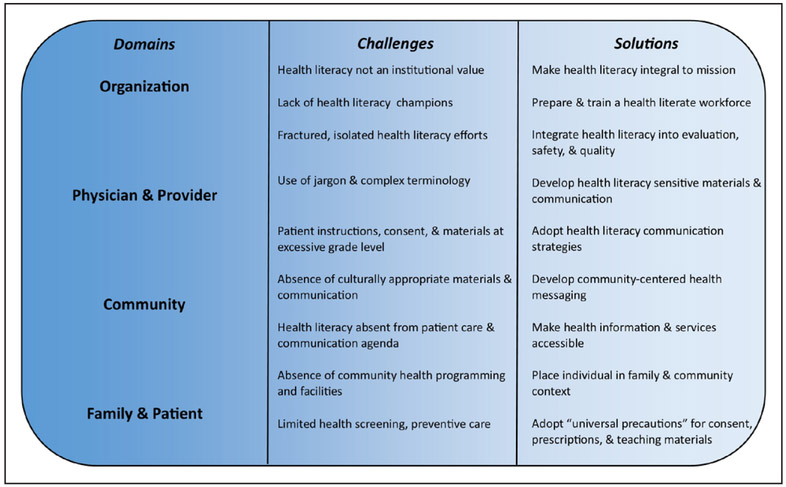
The concept of the health-literate organization has emerged in response to the challenges.231 The concept of the health-literate organization has a 3-fold intent. First, it asserts that health literacy as a problem belongs to the institution, not the individual patient, and declares health literacy as a basic condition and standard for health care. Patients cannot be expected, for instance, to adapt their literacy to meet the complex demands of medical care. As stated, “Being a health literate organization should not be seen as a luxury.…Rather, it is a necessary prerequisite to assuring patient safety, promoting adherence, enhancing self-efficacy, and improving patient outcomes.”204 Second, it provides a standard for development as a health-literate organization. Ten attributes of a health-literate organization231 have been articulated, and they provide substantive guidance for cardiovascular centers and organizations to make it easier for their constituencies and patients to seek and receive health care. The attributes of such an organization may be used to design road maps for institutional growth to become a health-literate organization. The 10 attributes span an attention to health literacy from healthcare institutional leadership, organization framework, and care delivery. Finally, the declaration of a health-literate organization emphasizes the need for a comprehensive program. Health literacy is not the bailiwick of a few individuals; the responsibility for pursuing a health-literate organization belongs to every individual who associates with patients, starting at the front desk and extending to the examination room, hospital ward, and executive boardroom. In Figure 3, we summarize critical domains and their relevant challenges and solutions for addressing health literacy.
Figure 3. Multilevel domains of health literacy and challenges and solutions for achieving a health-literate organization.
Health literacy is operative in the healthcare organization, physician and provider, family and community, and individual patient. The organization has the chief responsibility and capacity for implementing strategies for effective healthcare delivery that address health literacy challenges.
FUTURE DIRECTIONS FOR HEALTH LITERACY AND CVD
Health literacy has dynamic and important interfaces with CVD prevention, recognition, management, and treatment. The authors of this statement recognize that links between inadequate health literacy and cardiovascular outcomes can be confounded by substantial overlap with other social determinants of health, including social and economic position, educational attainment, access to care, and cultural affiliations. We conclude that the relations between health literacy and CVD risk and outcomes described in this statement are independent, valid, and significant. Inadequate health literacy is a barrier that will need to be overcome to fulfill the mission of cardiovascular health across the spectrum of prevention, screening, and treatment. The public health effectiveness of cardiovascular treatments that have demonstrated efficacy in clinical trials cannot be realized without managing the issue of health literacy. Further work on health literacy in patients with or at risk for CVD should therefore focus on effectively addressing the adverse health impact of limited health literacy. The authors of this statement note the following questions as priorities:
- How can healthcare organizations mitigate the effects of inadequate health literacy on CVD risk and outcomes? Addressing health literacy is an institutional mandate; decreasing health literacy barriers is the responsibility of healthcare organizations. Individuals, centers, departments, and institutions can collaborate for multilevel strategies that incorporate and address health literacy by removing unneeded complexity, thus advancing patient empowerment and education to improve healthcare delivery. Although many aspects of the AHRQQ Toolkit can be readily implemented by healthcare organizations, opportunities to further establish promote health-literate organizations are evident.
- In terms of preventive cardiology, interventions at the organizational level focused on hypertension, diabetes mellitus, diet, and exercise that are effective and scalable should be disseminated. Appropriate incentives for healthcare organizations to use such interventions should be considered.
- In terms of treatment of established CVDs such as acute coronary syndromes, heart failure, stroke, and AF, interventions that can be recommended with confidence are less widely available. Tools that support shared decision making for complex preference-sensitive procedures such as percutaneous coronary interventions and radiofrequency ablation need to be validated and disseminated.
- Any and all resources provided to patients should be usable and empowering for people across the spectrum of health literacy. Assessment of readability is paramount and may identify text that is obviously too complex. However, readability assessment is not sufficient as a mechanism to determine what material will be understood and effective.
How can individual physicians mitigate the effects of inadequate health literacy on CVD? Improving the skills of physicians in understanding the health literacy challenges of their patients and communicating complex health concepts requires continued attention. Mechanisms to inculcate an approach of universal precautions in which patient comprehension is proactively confirmed need to be further elaborated.
- How can the AHA as an organization address health literacy? For the AHA, it is imperative to develop a best practices approach to health literacy and to be a leader in promoting massive improvements in patient education and empowerment.
- Material developed by the AHA can be evaluated and tested by patient stakeholders and individuals with demonstrated content expertise in health literacy, with easily accessible online assessments to determine grade-level readability.
- The AHA can recognize and legitimize health literacy and its relevance for cardiovascular outcomes. The AHA can incorporate health literacy as part of the curricula of professional meetings, webinars, and professional learning opportunities, as well as in scientific statements. The AHA can include health literacy as a targeted factor in health services research-funding mechanisms. The AHA can encourage council leadership to recognize and address health literacy as an obstacle for optimal cardiovascular health. An integrated, multilevel, cross-disciplinary approach will likely be needed for the AHA to enhance an organizational approach to health literacy.
What is the impact of the rise in information technology on those with inadequate health literacy? The increasing reliance on health information via the Internet and social media threatens to exclude individuals with limited health literacy. People may lack access to such resources. However, information technology may emerge as an effective path to mitigating inadequate health literacy through such things as interactive text messaging and graphic or video communication. Technology alone, without adaptation for health literacy challenges, is likely to be inadequate to overcome health literacy challenges.
How should awareness of limited health literacy affect the design and conduct of clinical trials? Because of the complexity of informed consent for clinical trials and the lack of standardization across institutional review boards, individuals with inadequate health literacy may inadvertently be excluded from clinical trials. Consequently, the external validity of clinical trials may be limited by the lack of attention to health literacy. Similarly, without evaluation or measurement of health literacy, imbalances in effect by health literacy cannot be measured. Health literacy measurement should be explored as an important baseline variable in trials.
What is the role of communities in mitigating inadequate health literacy in CVD? Because inadequate health literacy often coexists with characteristics such as educational attainment and income, individuals with inadequate health literacy may be segregated by neighborhood and community. Involving community groups in efforts to address health literacy appears to be feasible on the basis of available research and deserves wider study. Community agencies and representatives can provide leadership and participate as stakeholders for programs and interventions.
What is the impact of an increasingly complex healthcare financing system on access for those with limited health literacy? Individual responsibility for enrollment in health insurance plans, frequent changes between different health insurance plans, and complex plans with high deductible levels are realities of American health care. Although the evaluation of the impact of health literacy on healthcare access and financing is beyond the scope of this statement, the impacts of health literacy on healthcare access and financing merit investigation. Advocacy for an equitable healthcare system must also incorporate health literacy obstacles in the access to and administration of health care.
What are the next steps in health literacy investigation and scholarship? Throughout this statement, the authors have identified knowledge gaps and opportunities for further research that integrates health literacy. Researchers conducting clinical, health services, and outcomes investigations and clinical trialists have multiple opportunities for incorporating health literacy into their studies. Priorities are to include health literacy assessments in cardiovascular studies and trials to assess generalizability and to determine effect modification by health literacy as part of either primary or secondary analyses. Second, study materials for patients should be reviewed with the objective of maintaining the universal precautions approach described in this statement. Third, multifaceted interventions should be developed that incorporate healthcare systems, providers, and patients. Researchers addressing health literacy should avoid being siloed, that is, developing interventions that are not integrated with the healthcare system, practice, and clinical interface that patients experience. Fourth, inclusion of patient stakeholders with limited health literacy in patient advisory committees and similar bodies is fundamental for patient-centered outcomes research because such individuals will enhance and legitimize the development of patient-centered research. The final and most pressing priority is the examination of the implementation of a universal precautions approach in clinical care. As identified by this statement, the evidence for the significant contribution of health literacy to disparities is well established. Steps forward must study how to improve the process of implementation of literacy sensitive strategies and interventions.
Appendix
Disclosures
Writing Group Disclosures
| Writing Group Member |
Employment | Research Grant | Other Research Support |
Speakers’ Bureau/ Honoraria |
Expert Witness |
Ownership Interest |
Consultant/ Advisory Board |
Other |
|---|---|---|---|---|---|---|---|---|
| Jared W. Magnani |
University of Pittsburgh | Doris Duke Charitable Foundation* | None | None | None | None | None | None |
| Herbert D. Aronow |
Warren Alpert Medical School of Brown University, Lifespan Cardiovascular Institute | None | None | None | None | None | None | None |
| Crystal W. Cené | University of North Carolina at Chapel Hill | None | None | None | None | None | None | None |
| Victoria Vaughan Dickson | New York University College of Nursing | None | None | None | None | None | None | None |
| Edward Havranek | Denver Health | AHA (investigator)*; AHRQ (principal investigator)*; NIH (investigator)*; PCORI (principal investigator)* | None | None | None | None | None | None |
| Lewis B. Morgenstern | University of Michigan Medical School | None | None | None | None | None | None | None |
| Mahasin S. Mujahid | University of California, Berkeley | NIH (co-investigator and investigator on 2 NIH grants)*; Robert Wood Johnson Foundation (co-investigator on a grant)* | None | None | None | None | None | None |
| Michael K. Paasche-Orlow | Boston University School of Medicine | None | None | None | None | None | None | None |
| Amy Pollak | Mayo Clinic | None | None | None | None | None | None | None |
| Joshua Z. Willey | Columbia University | None | None | None | None | None | None | None |
This table represents the relationships of writing group members that may be perceived as actual or reasonably perceived conflicts of interest as reported on the Disclosure Questionnaire, which all members of the writing group are required to complete and submit. A relationship is considered to be “significant” if (a) the person receives $10 000 or more during any 12-month period, or 5% or more of the person’s gross income; or (b) the person owns 5% or more of the voting stock or share of the entity, or owns $10 000 or more of the fair market value of the entity. A relationship is considered to be “modest” if it is less than “significant” under the preceding definition.
Significant.
Reviewer Disclosures
| Reviewer | Employment | Research Grant | Other Research Support |
Speakers’ Bureau/ Honoraria |
Expert Witness |
Ownership Interest |
Consultant/ Advisory Board |
Other |
|---|---|---|---|---|---|---|---|---|
| Pamela L. Lutsey | University of Minnesota | None | None | None | None | None | None | None |
| Kimberly S. Plake | Purdue University | Heart Failure Society of America (Cognitive Impairment and Depression as Mediators of the Relationship Between Health Literacy and Self-Care: A Proposed Model)* | None | Indiana Society of Cardiovascular and Pulmonary Rehabilitation (Health Literacy and its Influence on Education and Cardiovascular Outcomes, April 2017)* | None | None | None | None |
This table represents the relationships of reviewers that may be perceived as actual or reasonably perceived conflicts of interest as reported on the Disclosure Questionnaire, which all reviewers are required to complete and submit. A relationship is considered to be “significant” if (a) the person receives $10 000 or more during any 12-month period, or 5% or more of the person’s gross income; or (b) the person owns 5% or more of the voting stock or share of the entity, or owns $10 000 or more of the fair market value of the entity. A relationship is considered to be “modest” if it is less than “significant” under the preceding definition.
Modest.
REFERENCES
- 1.Nielson-Bohlman L, Panzer AM, Kindig DA. Health Literacy: A Prescription to End Confusion. Washington, DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- 2.Chen AM, Yehle KS, Albert NM, Ferraro KF, Mason HL, Murawski MM, Plake KS. Health literacy influences heart failure knowledge attainment but not self-efficacy for self-care or adherence to self-care over time. Nurs Res Pract. 2013;2013:353290. doi: 10.1155/2013/353290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McCleary-Jones V Health literacy and its association with diabetes knowledge, self-efficacy and disease self-management among African Americans with diabetes mellitus. ABNF J. 2011;22:25–32. [PubMed] [Google Scholar]
- 4.Gazmararian JA, Williams MV, Peel J, Baker DW. Health literacy and knowledge of chronic disease. Patient Educ Couns. 2003;51:267–275. [DOI] [PubMed] [Google Scholar]
- 5.Mosher HJ, Lund BC, Kripalani S, Kaboli PJ. Association of health literacy with medication knowledge, adherence, and adverse drug events among elderly veterans. J Health Commun. 2012;17(suppl 3):241–251. doi: 10.1080/10810730.2012.712611. [DOI] [PubMed] [Google Scholar]
- 6.Sentell T, Zhang W, Davis J, Baker KK, Braun KL The influence of community and individual health literacy on self-reported health status. J Gen Intern Med. 2014;29:298–304. doi: 10.1007/s11606-013-2638-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wolf MS, Gazmararian JA, Baker DW. Health literacy and functional health status among older adults. Arch Intern Med. 2005;165:1946–1952. doi: 10.1001/archinte.165.17.1946. [DOI] [PubMed] [Google Scholar]
- 8.Eichler K, Wieser S, Brügger U The costs of limited health literacy: a systematic review. Int J Public Health. 2009;54:313–324. doi: 10.1007/s00038-009-0058-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Howard DH, Gazmararian J, Parker RM. The impact of low health literacy on the medical costs of Medicare managed care enrollees. Am J Med. 2005;118:371–377. doi: 10.1016/j.amjmed.2005.01.010. [DOI] [PubMed] [Google Scholar]
- 10.Mitchell SE, Sadikova E, Jack BW, Paasche-Orlow MK. Health literacy and 30-day postdischarge hospital utilization. J Health Commun. 2012;17(suppl 3):325–338. doi: 10.1080/10810730.2012.715233. [DOI] [PubMed] [Google Scholar]
- 11.Bostock S, Steptoe A. Association between low functional health literacy and mortality in older adults: longitudinal cohort study. BMJ. 2012;344:e1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baker DW, Wolf MS, Feinglass J, Thompson JA, Gazmararian JA, Huang J. Health literacy and mortality among elderly persons. Arch Intern Med. 2007;167:1503–1509. doi: 10.1001/archinte.167.14.1503. [DOI] [PubMed] [Google Scholar]
- 13.Sudore RL, Yaffe K, Satterfield S, Harris TB, Mehta KM, Simonsick EM, Newman AB, Rosano C, Rooks R, Rubin SM, Ayonayon HN, Schillinger D. Limited literacy and mortality in the elderly: the Health, Aging, and Body Composition Study. J Gen Intern Med. 2006;21:806–812. doi: 10.1111/j.1525-1497.2006.00539.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, Arnett DK, Fonarow GC, Ho PM, Lauer MS, Masoudi FA, Robertson RM, Roger V, Schwamm LH, Sorlie P, Yancy CW, Rosamond WD; on behalf of the American Heart Association Strategic Planning Task Force and Statistics Committee. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 15.Health literacy: report of the Council on Scientific Affairs: Ad Hoc Committee on Health Literacy for the Council on Scientific Affairs, American Medical Association. JAMA. 1999;281:552–557. [PubMed] [Google Scholar]
- 16.ACP Foundation Promoting health literacy, https://www.acponline.org/. Accessed May 27, 2017.
- 17.The Joint Commission. "What did the doctor say?" Improving health literacy to protect patient safety. http://www.jointcommission.org/assets/1/18/improving_health_literacy.pdf. Accessed May 27, 2017. [Google Scholar]
- 18.Brega AG, Barnard J, Mabachi NM, Weiss BD, DeWalt DA, Brach C, Cifuentes M, Albright K, West DR AHRQ health literacy Universal Precautions Toolkit, 2nd edition. 2015. https://www.ahrq.gov/sites/default/files/publications/files/healthlittoolkit2_3.pdf. Accessed May 27, 2017. [Google Scholar]
- 19.Paasche-Orlow MK, Parker RM, Gazmararian JA, Nielsen-Bohlman LT, Rudd RR. The prevalence of limited health literacy. J Gen Intern Med. 2005;20:175–184. doi: 10.1111/j.1525-1497.2005.40245.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wolf MS, Gazmararian JA, Baker DW. Health literacy and health risk behaviors among older adults. Am J Prev Med. 2007;32:19–24. doi: 10.1016/j.amepre.2006.08.024. [DOI] [PubMed] [Google Scholar]
- 21.Levy H, Janke AT, Langa KM. Health literacy and the digital divide among older Americans. J Gen Intern Med. 2015;30:284–289. doi: 10.1007/s11606-014-3069-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Info Libr J. 2009;26:91–108. doi: 10.1111/j.1471-1842.2009.00848.x. [DOI] [PubMed] [Google Scholar]
- 23.Kirsch IS, Jungeblut A, Jenkins L, Kolstad A. Adult literacy in America: a first look at the results of the National Adult Literacy Survey. Washington, DC: Office of Educational Research and Improvement, US Department of Education; 1993. [Google Scholar]
- 24.Kunter M, Greenberg E, Jin Y, Paulsen C The health literacy of America's adults: results from the 2003 National Assessment of Adult Literacy (NECS 2006-483) Washington, DC: US Department of Education, National Center for Education Statistics; 2006. [Google Scholar]
- 25.The health literacy of America’s adults: results from the 2003 National Assessment of Adult Literacy. http://nces.ed.gov/pubsearch/pubsinfo.asp?pubid=2006483. Accessed May 27, 2017.
- 26.Skills Matter Further Results From the Survey of Adult Skills. Paris, France: OECD Publishing; 2016. [Google Scholar]
- 27.Time for the U.S. to reskill? What the Survey of Adult Skills says. https://www.nationalskillscoalition.org/resources/…/Survey_of_Adult_Skills_US.pdf. Accessed May 27, 2017.
- 28.Berkman ND, Davis TC, McCormack L. Health literacy: what is it? J Health Commun. 2010;15(suppl 2):9–19. doi: 10.1080/10810730.2010.499985. [DOI] [PubMed] [Google Scholar]
- 29.Nutbeam D The evolving concept of health literacy. Soc Sci Med. 2008;67:2072–2078. doi: 10.1016/j.socscimed.2008.09.050. [DOI] [PubMed] [Google Scholar]
- 30.Paasche-Orlow MK, Wolf MS. The causal pathways linking health literacy to health outcomes. Am J Health Behav. 2007;31(suppl 1):S19–S26. doi: 10.5555/ajhb.2007.31.supp.S19. [DOI] [PubMed] [Google Scholar]
- 31.Manganello J, Gerstner G, Pergolino K, Graham Y, Falisi A, Strogatz D. The relationship of health literacy with use of digital technology for health information: implications for public health practice. J Public Health Manag Pract. 2017;23:380–387. doi: 10.1097/PHH.0000000000000366. [DOI] [PubMed] [Google Scholar]
- 32.Koh HK, Rudd RE. The arc of health literacy. JAMA. 2015;314:1225–1226. doi: 10.1001/jama.2015.9978. [DOI] [PubMed] [Google Scholar]
- 33.Sørensen K, Van den Broucke S, Fullam J, Doyle G, Pelikan J, Slonska Z, Brand H; (HLS-EU) Consortium Health Literacy Project European. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health. 2012;12:80. doi: 10.1186/1471-2458-12-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Haun JN, Valerio MA, McCormack LA, Sørensen K, Paasche-Orlow MK Health literacy measurement: an inventory and descriptive summary of 51 instruments. J Health Commun. 2014;19(suppl 2):302–333. doi: 10.1080/10810730.2014.936571. [DOI] [PubMed] [Google Scholar]
- 35.Davis TC, Crouch MA, Long SW, Jackson RH, Bates P, George RB, Bairnsfather LE. Rapid assessment of literacy levels of adult primary care patients. Fam Med. 1991;23:433–435. [PubMed] [Google Scholar]
- 36.Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999;38:33–42. [DOI] [PubMed] [Google Scholar]
- 37.Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults: a new instrument for measuring patients’ literacy skills. J Gen Intern Med. 1995;10:537–541. [DOI] [PubMed] [Google Scholar]
- 38.Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004;36:588–594. [PubMed] [Google Scholar]
- 39.Haun J, Noland Dodd VJ, Graham-Pole J, Rienzo B, Donaldson P. Testing a health literacy screening tool: implications for utilization of a BRIEF Health Literacy Indicator. Fed Pract. 2009;26:24–31. [Google Scholar]
- 40.Lee SY, Bender DE, Ruiz RE, Cho YI. Development of an easy-to-use Spanish Health Literacy test. Health Serv Res. 2006;41(pt 1):1392–1412. doi: 10.1111/j.1475-6773.2006.00532.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Weiss BD, Mays MZ, Martz W, Castro KM, DeWalt DA, Pignone MP, Mockbee J, Hale FA. Quick assessment of literacy in primary care: the newest vital sign. Ann Fam Med. 2005;3:514–522. doi: 10.1370/afm.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rawson KA, Gunstad J, Hughes J, Spitznagel MB, Potter V, Waechter D, Rosneck J The METER: a brief, self-administered measure of health literacy. J Gen Intern Med. 2010;25:67–71. doi: 10.1007/s11606-009-1158-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhang XH, Thumboo J, Fong KY, Li SC Development and validation of a functional health literacy test. Patient. 2009;2:169–178. doi: 10.2165/11314850-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 44.McCormack L, Bann C, Squiers L, Berkman ND, Squire C, Schillinger D, Ohene-Frempong J, Hibbard J. Measuring health literacy: a pilot study of a new skills-based instrument. J Health Commun. 2010;15(suppl 2):51–71. doi: 10.1080/10810730.2010.499987. [DOI] [PubMed] [Google Scholar]
- 45.Bann CM, McCormack LA, Berkman ND, Squiers LB. The Health Literacy Skills Instrument: a 10-item short form. J Health Commun. 2012;17(suppl 3):191–202. doi: 10.1080/10810730.2012.718042. [DOI] [PubMed] [Google Scholar]
- 46.Hahn EA, Choi SW, Griffith JW, Yost KJ, Baker DW. Health literacy assessment using talking touchscreen technology (Health LiTT): a new item response theory-based measure of health literacy. J Health Commun. 2011;16(suppl 3):150–162. doi: 10.1080/10810730.2011.605434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Health Literacy Tool Shed. http://healthliteracy.bu.edu/all. Accessed November 6, 2016.
- 48.Marmot M, Friel S, Bell R, Houweling TA, Taylor S; Commission on Social Determinants of Health. Closing the gap in a generation: health equity through action on the social determinants of health. Lancet. 2008;372:1661–1669. doi: 10.1016/S0140-6736(08)61690-6. [DOI] [PubMed] [Google Scholar]
- 49.Havranek EP, Mujahid MS, Barr DA, Blair IV, Cohen MS, Cruz-Flores S, Davey-Smith G, Dennison-Himmelfarb CR, Lauer MS, Lockwood DW, Rosal M, Yancy CW; on behalf of the American Heart Association Council on Quality of Care and Outcomes Research, Council on Epidemiology and Prevention, Council on Cardiovascular and Stroke Nursing, Council on Lifestyle and Cardiometabolic Health, and Stroke Council. Social determinants of risk and outcomes for cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2015;132:873–898. doi: 10.1161/CIR.0000000000000228. [DOI] [PubMed] [Google Scholar]
- 50.Lynch J, Smith GD. A life course approach to chronic disease epidemiology. Annu Rev Public Health. 2005;26:1–35. doi: 10.1146/annurev.publhealth.26.021304.144505. [DOI] [PubMed] [Google Scholar]
- 51.Clouston SAP, Manganello JA, Richards M. A life course approach to health literacy: the role of gender, educational attainment and lifetime cognitive capability. Age Ageing. 2017;46:493–499. doi: 10.1093/ageing/afw229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Goodman MS, Gaskin DJ, Si X, Stafford JD, Lachance C, Kaphingst KA. Self-reported segregation experience throughout the life course and its association with adequate health literacy. Health Place. 2012;18:1115–1121. doi: 10.1016/j.healthplace.2012.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hirsh-Pasek K, Adamson LB, Bakeman R, Owen MT, Golinkoff RM, Pace A, Yust PK, Suma K. The contribution of early communication quality to low-income children’s language success. Psychol Sci. 2015;26:1071–1083. doi: 10.1177/0956797615581493. [DOI] [PubMed] [Google Scholar]
- 54.Sanders LM, Shaw JS, Guez G, Baur C, Rudd R. Health literacy and child health promotion: implications for research, clinical care, and public policy. Pediatrics. 2009;124(suppl 3):S306–S314. doi: 10.1542/peds.2009-1162G. [DOI] [PubMed] [Google Scholar]
- 55.Yin HS, Johnson M, Mendelsohn AL, Abrams MA, Sanders LM, Dreyer BP The health literacy of parents in the United States: a nationally representative study. Pediatrics. 2009;124(suppl 3):S289–S298. doi: 10.1542/peds.2009-1162E. [DOI] [PubMed] [Google Scholar]
- 56.Sanders LM, Federico S, Klass P, Abrams MA, Dreyer B. Literacy and child health: a systematic review. Arch Pediatr Adolesc Med. 2009;163:131–140. doi: 10.1001/archpediatrics.2008.539. [DOI] [PubMed] [Google Scholar]
- 57.DeWalt DA, Hink A Health literacy and child health outcomes: a systematic review of the literature. Pediatrics. 2009;124(suppl 3):S265–S274. doi: 10.1542/peds.2009-1162B. [DOI] [PubMed] [Google Scholar]
- 58.Paasche-Orlow MK, Parker RM. Improving the effectiveness of patient education: a focus on limited health literacy In: King TE, Wheeler MB, eds. Medical Management of Vulnerable and Underserved Patients. New York, NY: McGraw Hill; 2007:101–109. [Google Scholar]
- 59.Levitt L Why health insurance literacy matters. JAMA. 2015;313:555–556. doi: 10.1001/jama.2014.17419. [DOI] [PubMed] [Google Scholar]
- 60.Yom-Tov E, Marino B, Pai J, Harris D, Wolf M. The effect of limited health literacy on how Internet users learn about diabetes. J Health Commun. 2016;21:1107–1114. doi: 10.1080/10810730.2016.1222033. [DOI] [PubMed] [Google Scholar]
- 61.Meppelink CS, Smit EG, Diviani N, Van Weert JC Health literacy and online health information processing: unraveling the underlying mechanisms. J Health Commun. 2016;21(suppl 2):109–120. doi: 10.1080/10810730.2016.1193920. [DOI] [PubMed] [Google Scholar]
- 62.Mackert M, Mabry-Flynn A, Champlin S, Donovan EE, Pounders K Health literacy and health information technology adoption: the potential for a new digital divide. J Med Internet Res. 2016;18:e264. doi: 10.2196/jmir.6349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Joury AU, Alshathri M, Alkhunaizi M, Jaleesah N, Pines JM Internet websites for chest pain symptoms demonstrate highly variable content and quality. Acad Emerg Med. 2016;23:1146–1152. doi: 10.1111/acem.13039. [DOI] [PubMed] [Google Scholar]
- 64.Hutchinson N, Baird GL, Garg M. Examining the reading level of Internet medical information for common internal medicine diagnoses. Am J Med. 2016;129:637–639. doi: 10.1016/j.amjmed.2016.01.008. [DOI] [PubMed] [Google Scholar]
- 65.Cajita MI, Rodney T, Xu J, Hladek M, Han HR. Quality and health literacy demand of online heart failure information. J Cardiovasc Nurs. 2017;32:156–164. doi: 10.1097/JCN.0000000000000324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Castro CM, Wilson C, Wang F, Schillinger D. Babel babble: physicians’ use of unclarified medical jargon with patients. Am J Health Behav. 2007;31(suppl 1):S85–S95. doi: 10.5555/ajhb.2007.31.supp.S85. [DOI] [PubMed] [Google Scholar]
- 67.Hauptman PJ, Chibnall JT, Guild C, Armbrecht ES. Patient perceptions, physician communication, and the implantable cardioverter-defibrillator. JAMA Intern Med. 2013;173:571–577. doi: 10.1001/jamainternmed.2013.3171. [DOI] [PubMed] [Google Scholar]
- 68.Levinson W, Lesser CS, Epstein RM. Developing physician communication skills for patient-centered care. Health Aff (Millwood). 2010;29:1310–1318. doi: 10.1377/hlthaff.2009.0450. [DOI] [PubMed] [Google Scholar]
- 69.Katz MG, Jacobson TA, Veledar E, Kripalani S Patient literacy and question-asking behavior during the medical encounter: a mixed-methods analysis. J Gen Intern Med. 2007;22:782–786. doi: 10.1007/s11606-007-0184-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Aboumatar HJ, Carson KA, Beach MC, Roter DL, Cooper LA The impact of health literacy on desire for participation in healthcare, medical visit communication, and patient reported outcomes among patients with hypertension. J Gen Intern Med. 2013;28:1469–1476. doi: 10.1007/s11606-013-2466-5.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Baker DW, Parker RM, Williams MV, Pitkin K, Parikh NS, Coates W, Imara M. The health care experience of patients with low literacy. Arch Fam Med. 1996;5:329–334. [DOI] [PubMed] [Google Scholar]
- 72.Farrell TW, Chandran R, Gramling R. Understanding the role of shame in the clinical assessment of health literacy. Fam Med. 2008;40:235–236. [PubMed] [Google Scholar]
- 73.Paasche-Orlow M Caring for patients with limited health literacy: a 76-year-old man with multiple medical problems. JAMA. 2011;306:1122–1129. doi: 10.1001/jama.2011.1203. [DOI] [PubMed] [Google Scholar]
- 74.Killian L, Coletti M The role of universal health literacy precautions in minimizing “medspeak” and promoting shared decision making. AMA J Ethics. 2017;19:296–303. doi: 10.1001/journalofethics.2017.19.3.pfor1-1703. [DOI] [PubMed] [Google Scholar]
- 75.Mabachi NM, Cifuentes M, Barnard J, Brega AG, Albright K, Weiss BD, Brach C, West D Demonstration of the Health Literacy Universal Precautions Toolkit: lessons for quality improvement. J Ambul Care Manage. 2016;39:199–208. doi: 10.1097/JAC.0000000000000102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kreps GL, Sparks L. Meeting the health literacy needs of immigrant populations. Patient Educ Couns. 2008;71:328–332. doi: 10.1016/j.pec.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 77.Sudore RL, Landefeld CS, Pérez-Stable EJ, Bibbins-Domingo K, Williams BA, Schillinger D. Unraveling the relationship between literacy, language proficiency, and patient-physician communication. Patient Educ Couns. 2009;75:398–402. doi: 10.1016/j.pec.2009.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Prins E, Monnat S. Examining associations between self-rated health and proficiency in literacy and numeracy among immigrants and U.S.- born adults: evidence from the Program for the International Assessment of Adult Competencies (PIAAC). PLoS One. 2015;10:e0130257. doi: 10.1371/journal.pone.0130257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Willens DE, Kripalani S, Schildcrout JS, Cawthon C, Wallston K, Mion LC, Davis C, Danciu I, Rothman RL, Roumie CL. Association of brief health literacy screening and blood pressure in primary care. J Health Commun. 2013;18(suppl 1):129–142. doi: 10.1080/10810730.2013.825663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.McNaughton CD, Jacobson TA, Kripalani S Low literacy is associated with uncontrolled blood pressure in primary care patients with hypertension and heart disease. Patient Educ Couns. 2014;96:165–170. doi: 10.1016/j.pec.2014.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.McNaughton CD, Kripalani S, Cawthon C, Mion LC, Wallston KA, Roumie CL Association of health literacy with elevated blood pressure: a cohort study of hospitalized patients. Med Care. 2014;52:346–353. doi: 10.1097/MLR.0000000000000101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Halladay JR, Donahue KE, Cené CW, Li Q, Cummings DM, Hinderliter AL, Miller CL, Garcia BA, Little E, Rachide M, Tillman J, Ammerman AS, DeWalt D The association of health literacy and blood pressure reduction in a cohort of patients with hypertension: the Heart Healthy Lenoir Trial. Patient Educ Couns. 2017;100:542–549. doi: 10.1016/j.pec.2016.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Morris NS, MacLean CD, Littenberg B. Literacy and health outcomes: a cross-sectional study in 1002 adults with diabetes. BMC Fam Pract. 2006;7:49. doi: 10.1186/1471-2296-7-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Cavanaugh K, Huizinga MM, Wallston KA, Gebretsadik T, Shintani A, Davis D, Gregory RP, Fuchs L, Malone R, Cherrington A, Pignone M, DeWalt DA, Elasy TA, Rothman RL. Association of numeracy and diabetes control. Ann Intern Med. 2008;148:737–746. [DOI] [PubMed] [Google Scholar]
- 85.Mbaezue N, Mayberry R, Gazmararian J, Quarshie A, Ivonye C, Heisler M. The impact of health literacy on self-monitoring of blood glucose in patients with diabetes receiving care in an inner-city hospital. J Natl Med Assoc. 2010;102:5–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Sarkar U, Karter AJ, Liu JY, Moffet HH, Adler NE, Schillinger D Hypoglycemia is more common among type 2 diabetes patients with limited health literacy: the Diabetes Study of Northern California (DISTANCE). J Gen Intern Med. 2010;25:962–968. doi: 10.1007/s11606-010-1389-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Brega AG, Ang A, Vega W, Jiang L, Beals J, Mitchell CM, Moore K, Manson SM, Acton KJ, Roubideaux Y; Special Diabetes Program for Indians Healthy Heart Demonstration Project. Mechanisms underlying the relationship between health literacy and glycemic control in American Indians and Alaska Natives. Patient Educ Couns. 2012;88:61–68. doi: 10.1016/j.pec.2012.03.008. [DOI] [PubMed] [Google Scholar]
- 88.Bauer AM, Schillinger D, Parker MM, Katon W, Adler N, Adams AS, Moffet HH, Karter AJ Health literacy and antidepressant medication adherence among adults with diabetes: the Diabetes Study of Northern California (DISTANCE). J Gen Intern Med. 2013;28:1181–1187. doi: 10.1007/s11606-013-2402-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.McNaughton CD, Korman RR, Kabagambe EK, Wright SW. Health literacy and blood glucose among Guyanese emergency department patients without diagnosed diabetes: a cross-sectional study. Diabetol Metab Syndr. 2015;7:31. doi: 10.1186/s13098-015-0028-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Geboers B, Reijneveld SA, Jansen CJ, de Winter AF. Health literacy is associated with health behaviors and social factors among older adults: results from the LifeLines Cohort Study. J Health Commun. 2016;21(suppl 2):45–53. doi: 10.1080/10810730.2016.1201174. [DOI] [PubMed] [Google Scholar]
- 91.Lassetter JH, Clark L, Morgan SE, Brown LB, VanServellen G, Duncan K, Hopkins ES. Health literacy and obesity among native Hawaiian and Pacific Islanders in the United States. Public Health Nurs. 2015;32:15–23. doi: 10.1111/phn.12155. [DOI] [PubMed] [Google Scholar]
- 92.Lam LT, Yang L. Is low health literacy associated with overweight and obesity in adolescents: an epidemiology study in a 12-16 years old population, Nanning, China, 2012. Arch Public Health. 2014;72:11. doi: 10.1186/2049-3258-72-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Joshi C, Jayasinghe UW, Parker S, Del Mar C, Russell G, Lloyd J, Mazza D, Denney-Wilson E, van Driel M, Taylor R, Harris MF; Preventive Evidence Into Practice (PEP) Partnership Group. Does health literacy affect patients’ receipt of preventative primary care? A multilevel analysis. BMC Fam Pract. 2014;15:171. doi: 10.1186/s12875-014-0171-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Chari R, Warsh J, Ketterer T, Hossain J, Sharif I. Association between health literacy and child and adolescent obesity. Patient Educ Couns. 2014;94:61–66. doi: 10.1016/j.pec.2013.09.006. [DOI] [PubMed] [Google Scholar]
- 95.Bailey SC, Fang G, Annis IE, O’Conor R, Paasche-Orlow MK, Wolf MS. Health literacy and 30-day hospital readmission after acute myocardial infarction. BMJ Open. 2015;5:e006975. doi: 10.1136/bmjopen-2014-006975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Gazmararian JA, Kripalani S, Miller MJ, Echt KV, Ren J, Rask K Factors associated with medication refill adherence in cardiovascular-related diseases: a focus on health literacy. J Gen Intern Med. 2006;21:1215–1221. doi: 10.1111/j.1525-1497.2006.00591.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Kripalani S, Gatti ME, Jacobson TA. Association of age, health literacy, and medication management strategies with cardiovascular medication adherence. Patient Educ Couns. 2010;81:177–181. doi: 10.1016/j.pec.2010.04.030. [DOI] [PubMed] [Google Scholar]
- 98.McManus DD, Saczynski JS, Lessard D, Waring ME, Allison J, Parish DC, Goldberg RJ, Ash A, Kiefe CI; TRACE-CORE Investigators. Reliability of predicting early hospital readmission after discharge for an acute coronary syndrome using claims-based data. Am J Cardiol. 2016;117:501–507. doi: 10.1016/j.amjcard.2015.11.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Bell SP, Schnipper JL, Goggins K, Bian A, Shintani A, Roumie CL, Dalal AK, Jacobson TA, Rask KJ, Vaccarino V, Gandhi TK, Labonville SA, Johnson D, Neal EB, Kripalani S; Pharmacist Intervention for Low Literacy in Cardiovascular Disease (PILL-CVD) Study Group. Effect of pharmacist counseling intervention on health care utilization following hospital discharge: a randomized control trial. J Gen Intern Med. 2016;31:470–477. doi: 10.1007/s11606-016-3596-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Laramee AS, Morris N, Littenberg B. Relationship of literacy and heart failure in adults with diabetes. BMC Health Serv Res. 2007;7:98. doi: 10.1186/1472-6963-7-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Murray MD, Tu W, Wu J, Morrow D, Smith F, Brater DC. Factors associated with exacerbation of heart failure include treatment adherence and health literacy skills. Clin Pharmacol Ther. 2009;85:651–658. doi: 10.1038/clpt.2009.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Macabasco-O’Connell A, DeWalt DA, Broucksou KA, Hawk V, Baker DW, Schillinger D, Ruo B, Bibbins-Domingo K, Holmes GM, Erman B, Weinberger M, Pignone M Relationship between literacy, knowledge, self-care behaviors, and heart failure-related quality of life among patients with heart failure. J Gen Intern Med. 2011;26:979–986. doi: 10.1007/s11606-011-1668-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Chaudhry SI, Herrin J, Phillips C, Butler J, Mukerjhee S, Murillo J, Onwuanyi A, Seto TB, Spertus J, Krumholz HM. Racial disparities in health literacy and access to care among patients with heart failure. J Card Fail. 2011;17:122–127. doi: 10.1016/j.cardfail.2010.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Peterson PN, Shetterly SM, Clarke CL, Bekelman DB, Chan PS, Allen LA, Matlock DD, Magid DJ, Masoudi FA. Health literacy and outcomes among patients with heart failure. JAMA. 2011;305:1695–1701. doi: 10.1001/jama.2011.512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Noureldin M, Plake KS, Morrow DG, Tu W, Wu J, Murray MD. Effect of health literacy on drug adherence in patients with heart failure. Pharmacotherapy. 2012;32:819–826. doi: 10.1002/j.1875-9114.2012.01109.x. [DOI] [PubMed] [Google Scholar]
- 106.DeWalt DA, Schillinger D, Ruo B, Bibbins-Domingo K, Baker DW, Holmes GM, Weinberger M, Macabasco-O’Connell A, Broucksou K, Hawk V, Grady KL, Erman B, Sueta CA, Chang PP, Cene CW, Wu JR, Jones CD, Pignone M Multisite randomized trial of a single-session versus multisession literacy: sensitive self-care intervention for patients with heart failure. Circulation. 2012;125:2854–2862. doi: 10.1161/CIRCULATIONAHA.111.081745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Wu JR, Holmes GM, DeWalt DA, Macabasco-O’Connell A, Bibbins-Domingo K, Ruo B, Baker DW, Schillinger D, Weinberger M, Broucksou KA, Erman B, Jones CD, Cene CW, Pignone M Low literacy is associated with increased risk of hospitalization and death among individuals with heart failure. J Gen Intern Med. 2013;28:1174–1180. doi: 10.1007/s11606-013-2394-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Mixon AS, Myers AP, Leak CL, Lou Jacobsen JM, Cawthon C, Goggins KM, Nwosu S, Schildcrout JS, Schnelle JF, Speroff T, Kripalani S. Characteristics associated with postdischarge medication errors. Mayo Clin Proc. 2014;89:1042–1051. doi: 10.1016/j.mayocp.2014.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.McNaughton CD, Cawthon C, Kripalani S, Liu D, Storrow AB, Roumie CL. Health literacy and mortality: a cohort study of patients hospitalized for acute heart failure. J Am Heart Assoc. 2015;4:e001799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Moser DK, Robinson S, Biddle MJ, Pelter MM, Nesbitt TS, Southard J, Cooper L, Dracup K. Health literacy predicts morbidity and mortality in rural patients with heart failure. J Card Fail. 2015;21:612–618. doi: 10.1016/j.cardfail.2015.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Wu JR, Moser DK, DeWalt DA, Rayens MK, Dracup K Health literacy mediates the relationship between age and health outcomes in patients with heart failure. Circ Heart Fail. 2016;9:e002250. doi: 10.1161/CIRCHEARTFAILURE.115.002250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Powers BJ, Olsen MK, Oddone EZ, Thorpe CT, Bosworth HB Literacy and blood pressure: do healthcare systems influence this relationship? A cross-sectional study. BMC Health Serv Res. 2008;8:219. doi: 10.1186/1472-6963-8-219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Williams MV, Baker DW, Parker RM, Nurss JR Relationship of functional health literacy to patients’ knowledge of their chronic disease: a study of patients with hypertension and diabetes. Arch Intern Med. 1998;158:166–172. [DOI] [PubMed] [Google Scholar]
- 114.Wright-Nunes JA, Luther JM, Ikizler TA, Cavanaugh KL Patient knowledge of blood pressure target is associated with improved blood pressure control in chronic kidney disease. Patient Educ Couns. 2012;88:184–188. doi: 10.1016/j.pec.2012.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Pandit AU, Tang JW, Bailey SC, Davis TC, Bocchini MV, Persell SD, Federman AD, Wolf MS. Education, literacy, and health: mediating effects on hypertension knowledge and control. Patient Educ Couns. 2009;75:381–385. doi: 10.1016/j.pec.2009.04.006. [DOI] [PubMed] [Google Scholar]
- 116.AlGhurair SA, Hughes CA, Simpson SH, Guirguis LM A systematic review of patient self-reported barriers of adherence to antihypertensive medications using the World Health Organization Multidimensional Adherence Model. J Clin Hypertens (Greenwich). 2012;14:877–886. doi: 10.1111/j.1751-7176.2012.00699.x.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Miller TA. Health literacy and adherence to medical treatment in chronic and acute illness: a meta-analysis. Patient Educ Couns. 2016;99:1079–1086. doi: 10.1016/j.pec.2016.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Davis TC, Wolf MS, Bass PF 3rd, Thompson JA, Tilson HH, Neuberger M, Parker RM. Literacy and misunderstanding prescription drug labels. Ann Intern Med. 2006;145:887–894. [DOI] [PubMed] [Google Scholar]
- 119.Wolf MS, Davis TC, Tilson HH, Bass PF 3rd, Parker RM. Misunderstanding of prescription drug warning labels among patients with low literacy. Am J Health Syst Pharm. 2006;63:1048–1055. doi: 10.2146/ajhp050469. [DOI] [PubMed] [Google Scholar]
- 120.Wolf MS, Davis TC, Curtis LM, Bailey SC, Knox JP, Bergeron A, Abbet M, Shrank WH, Parker RM, Wood AJ. A patient-centered prescription drug label to promote appropriate medication use and adherence. J Gen Intern Med. 2016;31:1482–1489. doi: 10.1007/s11606-016-3816-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Yeung DL, Alvarez KS, Quinones ME, Clark CA, Oliver GH, Alvarez CA, Jaiyeola AO Low-health literacy flashcards & mobile video reinforcement to improve medication adherence in patients on oral diabetes, heart failure, and hypertension medications. J Am Pharm Assoc (2003). 2017;57:30–37. doi: 10.1016/j.japh.2016.08.012.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.DeWalt DA, Callahan LF, Hawk VH, Broucksou KA, Hink A, Rudd R, Brach C. Health Literacy Universal Precautions Toolkit Rockville, MD: Agency for Healthcare Research and Quality; 2010. [Google Scholar]
- 123.Náfrádi L, Galimberti E, Nakamoto K, Schulz PJ. Intentional and unintentional medication non-adherence in hypertension: the role of health literacy, empowerment and medication beliefs. J Public Health Res. 2016;5:762. doi: 10.4081/jphr.2016.762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Bains SS, Egede LE Associations between health literacy, diabetes knowledge, self-care behaviors, and glycemic control in a low income population with type 2 diabetes. Diabetes Technol Ther. 2011;13:335–341. doi: 10.1089/dia.2010.0160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.DeWalt DA, Boone RS, Pignone MP. Literacy and its relationship with self-efficacy, trust, and participation in medical decision making. Am J Health Behav. 2007;31(suppl 1):S27–S35. doi: 10.5555/ajhb.2007.31.supp.S27. [DOI] [PubMed] [Google Scholar]
- 126.Sarkar U, Fisher L, Schillinger D Is self-efficacy associated with diabetes self-management across race/ethnicity and health literacy? Diabetes Care. 2006;29:823–829. [DOI] [PubMed] [Google Scholar]
- 127.Powell CK, Hill EG, Clancy DE. The relationship between health literacy and diabetes knowledge and readiness to take health actions. Diabetes Educ. 2007;33:144–151. doi: 10.1177/0145721706297452. [DOI] [PubMed] [Google Scholar]
- 128.Fan JH, Lyons SA, Goodman MS, Blanchard MS, Kaphingst KA. Relationship between health literacy and unintentional and intentional medication nonadherence in medically underserved patients with type 2 diabetes. Diabetes Educ. 2016;42:199–208. doi: 10.1177/0145721715624969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Schillinger D, Grumbach K, Piette J, Wang F, Osmond D, Daher C, Palacios J, Sullivan GD, Bindman AB. Association of health literacy with diabetes outcomes. JAMA. 2002;288:475–482. [DOI] [PubMed] [Google Scholar]
- 130.Al Sayah F, Majumdar SR, Williams B, Robertson S, Johnson JA. Health literacy and health outcomes in diabetes: a systematic review. J Gen Intern Med. 2013;28:444–52. doi: 10.1007/s11606-012-2241-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Bailey SC, Brega AG, Crutchfield TM, Elasy T, Herr H, Kaphingst K, Karter AJ, Moreland-Russell S, Osborn CY, Pignone M, Rothman R, Schillinger D. Update on health literacy and diabetes. Diabetes Educ. 2014;40:581–604. doi: 10.1177/0145721714540220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Sudore RL, Mehta KM, Simonsick EM, Harris TB, Newman AB, Satterfield S, Rosano C, Rooks RN, Rubin SM, Ayonayon HN, Yaffe K. Limited literacy in older people and disparities in health and healthcare access. J Am Geriatr Soc. 2006;54:770–776. doi: 10.1111/j.1532-5415.2006.00691.x. [DOI] [PubMed] [Google Scholar]
- 133.Ferguson MO, Long JA, Zhu J, Small DS, Lawson B, Glick HA, Schapira MM. Low health literacy predicts misperceptions of diabetes control in patients with persistently elevated A1C. Diabetes Educ. 2015;41:309–319. doi: 10.1177/0145721715572446. [DOI] [PubMed] [Google Scholar]
- 134.Howe CJ, Cipher DJ, LeFlore J, Lipman TH. Parent health literacy and communication with diabetes educators in a pediatric diabetes clinic: a mixed methods approach. J Health Commun. 2015;20(suppl 2):50–59. doi: 10.1080/10810730.2015.1083636. [DOI] [PubMed] [Google Scholar]
- 135.Loucks EB, Gilman SE, Howe CJ, Kawachi I, Kubzansky LD, Rudd RE, Martin LT, Nandi A, Wilhelm A, Buka SL. Education and coronary heart disease risk: potential mechanisms such as literacy, perceived constraints, and depressive symptoms. Health Educ Behav. 2015;42:370–379. doi: 10.1177/1090198114560020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Osborn CY, Cavanaugh K, Wallston KA, Kripalani S, Elasy TA, Rothman RL, White RO Health literacy explains racial disparities in diabetes medication adherence. J Health Commun. 2011;16(suppl 3):268–278. doi: 10.1080/10810730.2011.604388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Sarkar U, Karter AJ, Liu JY, Adler NE, Nguyen R, Lopez A, Schillinger D. The literacy divide: health literacy and the use of an Internet-based patient portal in an integrated health system: results from the Diabetes Study of Northern California (DISTANCE). J Health Commun. 2010;15(suppl 2):183–196. doi: 10.1080/10810730.2010.499988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Bohanny W, Wu SF, Liu CY, Yeh SH, Tsay SL, Wang TJ. Health literacy, self-efficacy, and self-care behaviors in patients with type 2 diabetes mellitus. J Am Assoc Nurse Pract. 2013;25:495–502. doi: 10.1111/1745-7599.12017. [DOI] [PubMed] [Google Scholar]
- 139.White RO, Osborn CY, Gebretsadik T, Kripalani S, Rothman RL Health literacy, physician trust, and diabetes-related self-care activities in Hispanics with limited resources. J Health Care Poor Underserved. 2013;24:1756–1768. doi: 10.1353/hpu.2013.0177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Woodard LD, Landrum CR, Amspoker AB, Ramsey D, Naik AD. Interaction between functional health literacy, patient activation, and glycemic control. Patient Prefer Adherence. 2014;8:1019–1024. doi: 10.2147/PPA.S63954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Fransen MP, Beune EJ, Baim-Lance AM, Bruessing RC, Essink-Bot ML. Diabetes self-management support for patients with low health literacy: perceptions of patients and providers. J Diabetes. 2015;7:418–425. doi: 10.1111/1753-0407.12191. [DOI] [PubMed] [Google Scholar]
- 142.Schillinger D, Machtinger EL, Wang F, Palacios J, Rodriguez M, Bindman A. Language, literacy, and communication regarding medication in an anticoagulation clinic: a comparison of verbal vs. visual assessment. J Health Commun. 2006;11:651–664. doi: 10.1080/10810730600934500. [DOI] [PubMed] [Google Scholar]
- 143.Swavely D, Vorderstrasse A, Maldonado E, Eid S, Etchason J. Implementation and evaluation of a low health literacy and culturally sensitive diabetes education program. J Healthc Qual. 2014;36:16–23. doi: 10.1111/jhq.12021. [DOI] [PubMed] [Google Scholar]
- 144.Rothman RL, DeWalt DA, Malone R, Bryant B, Shintani A, Crigler B, Weinberger M, Pignone M Influence of patient literacy on the effectiveness of a primary care-based diabetes disease management program. JAMA. 2004;292:1711–1716. doi: 10.1001/jama.292.14.1711. [DOI] [PubMed] [Google Scholar]
- 145.Rosal MC, Ockene IS, Restrepo A, White MJ, Borg A, Olendzki B, Scavron J, Candib L, Welch G, Reed G Randomized trial of a literacy-sensitive, culturally tailored diabetes self-management intervention for low-income Latinos: Latinos en control. Diabetes Care. 2011;34:838–844. doi: 10.2337/dc10-1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Chaufan C, Karter AJ, Moffet HH, Quan J, Parker MM, Kruger J, Schillinger D, Fernandez A. Identifying Spanish language competent physicians: the Diabetes Study of Northern California (DISTANCE). Ethn Dis. 2016;26:537–544. doi: 10.18865/ed.26.4.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Aponte J General literacy and health literacy in Dominicans with diabetes. Hisp Health Care Int. 2013;11:167–172. doi: 10.1891/1540-4153.11.4.167. [DOI] [PubMed] [Google Scholar]
- 148.Choi SE, Rush E, Henry S. Health literacy in Korean immigrants at risk for type 2 diabetes. J Immigr Minor Health. 2013;15:553–559. doi: 10.1007/s10903-012-9672-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Leung AY, Bo A, Hsiao HY, Wang SS, Chi I. Health literacy issues in the care of Chinese American immigrants with diabetes: a qualitative study. BMJ Open. 2014;4:e005294. doi: 10.1136/bmjopen-2014-005294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Smith-Miller CA, Berry DC, DeWalt D, Miller CT. Type 2 diabetes selfmanagement among Spanish-speaking Hispanic immigrants. J Immigr Minor Health. 2016;18:1392–1403. doi: 10.1007/s10903-015-0271-4. [DOI] [PubMed] [Google Scholar]
- 151.Parker MM, Fernández A, Moffet HH, Grant RW, Torreblanca A, Karter AJ. Association of patient-physician language concordance and glycemic control for limited-English proficiency Latinos with type 2 diabetes. JAMA Intern Med. 2017;177:380–387. doi: 10.1001/jamainternmed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Osborn CY, Paasche-Orlow MK, Bailey SC, Wolf MS. The mechanisms linking health literacy to behavior and health status. Am J Health Behav. 2011;35:118–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Guntzviller LM, King AJ, Jensen JD, Davis LA. Self-efficacy, health literacy, and nutrition and exercise behaviors in a low-income, Hispanic population. J Immigr Minor Health. 2017;19:489–493. doi: 10.1007/s10903-016-0384-4. [DOI] [PubMed] [Google Scholar]
- 154.James DC, Harville C, Efunbumi O, Martin MY. Health literacy issues surrounding weight management among African American women: a mixed methods study. J Hum Nutr Diet. 2015;28(suppl 2):41–49. doi: 10.1111/jhn.12239. [DOI] [PubMed] [Google Scholar]
- 155.Zoellner J, You W, Connell C, Smith-Ray RL, Allen K, Tucker KL, Davy BM, Estabrooks P. Health literacy is associated with Healthy Eating Index scores and sugar-sweetened beverage intake: findings from the rural lower Mississippi Delta. J Am Diet Assoc. 2011;111:1012–1020. doi: 10.1016/j.jada.2011.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Zoellner JM, Hedrick VE, You W, Chen Y, Davy BM, Porter KJ, Bailey A, Lane H, Alexander R, Estabrooks PA. Effects of a behavioral and health literacy intervention to reduce sugar-sweetened beverages: a randomized-controlled trial. Int J Behav Nutr Phys Act. 2016;13:38. doi: 10.1186/s12966-016-0362-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Lee YJ, Boden-Albala B, Jia H, Wilcox A, Bakken S. The association between online health information-seeking behaviors and health behaviors among Hispanics in New York City: a community-based cross-sectional study. J Med Internet Res. 2015;17:e261. doi: 10.2196/jmir.4368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Charlton R, Gravenor MB, Rees A, Knox G, Hill R, Rahman MA, Jones K, Christian D, Baker JS, Stratton G, Brophy S. Factors associated with low fitness in adolescents: a mixed methods study. BMC Public Health. 2014;14:764. doi: 10.1186/1471-2458-14-764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Sanders LM, Perrin EM, Yin HS, Bronaugh A, Rothman RL; Greenlight Study Team. “Greenlight Study”: a controlled trial of low-literacy, early childhood obesity prevention. Pediatrics. 2014;133:e1724–e1737. doi: 10.1542/peds.2013-3867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Houston TK, Scarinci IC, Person SD, Greene PG Patient smoking cessation advice by health care providers: the role of ethnicity, socioeconomic status, and health. Am J Public Health. 2005;95:1056–1061. doi: 10.2105/AJPH.2004.039909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Stewart DW, Adams CE, Cano MA, Correa-Fernández V, Li Y, Waters AJ, Wetter DW, Vidrine JI. Associations between health literacy and established predictors of smoking cessation. Am J Public Health. 2013;103:e43–e49. doi: 10.2105/AJPH.2012.301062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Stewart DW, Cano MA, Correa-Fernández V, Spears CA, Li Y, Waters AJ, Wetter DW, Vidrine JI. Lower health literacy predicts smoking relapse among racially/ethnically diverse smokers with low socioeconomic status. BMC Public Health. 2014;14:716. doi: 10.1186/1471-2458-14-716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Kripalani S, Goggins K, Nwosu S, Schildcrout J, Mixon AS, McNaughton C, McDougald Scott AM, Wallston KA; Vanderbilt Inpatient Cohort Study. Medication nonadherence before hospitalization for acute cardiac events. J Health Commun. 2015;20(suppl 2):34–42. doi: 10.1080/10810730.2015.1080331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Schnipper JL, Roumie CL, Cawthon C, Businger A, Dalal AK, Mugalla I, Eden S, Jacobson TA, Rask KJ, Vaccarino V, Gandhi TK, Bates DW, Johnson DC, Labonville S, Gregory D, Kripalani S; for the PILL-CVD Study Group. Rationale and design of the Pharmacist Intervention for Low Literacy in Cardiovascular Disease (PILL-CVD) study. Circ Cardiovasc Qual Outcomes. 2010;3:212–219. doi: 10.1161/CIRCOUTCOMES.109.921833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Kripalani S, Schmotzer B, Jacobson TA. Improving Medication Adherence through Graphically Enhanced Interventions in Coronary Heart Disease (IMAGE-CHD): a randomized controlled trial. J Gen Intern Med. 2012;27:1609–1617. doi: 10.1007/s11606-012-2136-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Katz MG, Kripalani S, Weiss BD Use of pictorial aids in medication instructions: a review of the literature. Am J Health Syst Pharm. 2006;63:2391–2397. doi: 10.2146/ajhp060162. [DOI] [PubMed] [Google Scholar]
- 167.Heydarpour B, Saeidi M, Ezzati P, Soroush A, Komasi S. Sociodemographic predictors in failure to complete outpatient cardiac rehabilitation. Ann Rehabil Med. 2015;39:863–871. doi: 10.5535/arm.2015.39.6.863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Cajita MI, Cajita TR, Han HR Health literacy and heart failure: a systematic review. J Cardiovasc Nurs. 2016;31:121–130. doi: 10.1097/JCN.0000000000000229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.McNaughton CD, Collins SP, Kripalani S, Rothman R, Self WH, Jenkins C, Miller K, Arbogast P, Naftilan A, Dittus RS, Storrow AB. Low numeracy is associated with increased odds of 30-day emergency department or hospital recidivism for patients with acute heart failure. Circ Heart Fail. 2013;6:40–46. doi: 10.1161/CIRCHEARTFAILURE.112.969477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Grif Alspach J Heart failure and low health literacy: mitigating this lethal combination. Crit Care Nurse. 2015;35:10–14. doi: 10.4037/ccn2015734. [DOI] [PubMed] [Google Scholar]
- 171.Matsuoka S, Tsuchihashi-Makaya M, Kayane T, Yamada M, Wakabayashi R, Kato NP, Yazawa M. Health literacy is independently associated with self-care behavior in patients with heart failure. Patient Educ Couns. 2016;99:1026–1032. doi: 10.1016/j.pec.2016.01.003. [DOI] [PubMed] [Google Scholar]
- 172.Nutbeam D Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promot Int. 2000;15:259–267. [Google Scholar]
- 173.Murray MD, Young J, Hoke S, Tu W, Weiner M, Morrow D, Stroupe KT, Wu J, Clark D, Smith F, Gradus-Pizlo I, Weinberger M, Brater DC. Pharmacist intervention to improve medication adherence in heart failure: a randomized trial. Ann Intern Med. 2007;146:714–725. [DOI] [PubMed] [Google Scholar]
- 174.DeWalt DA, Pignone M, Malone R, Rawls C, Kosnar MC, George G, Bryant B, Rothman RL, Angel B Development and pilot testing of a disease management program for low literacy patients with heart failure. Patient Educ Couns. 2004;55:78–86. doi: 10.1016/j.pec.2003.06.002. [DOI] [PubMed] [Google Scholar]
- 175.Smith B, Forkner E, Krasuski RA, Galbreath AD, Freeman GL. Educational attainment has a limited impact on disease management outcomes in heart failure. Dis Manag. 2006;9:157–166. doi: 10.1089/dis.2006.9.157. [DOI] [PubMed] [Google Scholar]
- 176.Dickson V, Chyun D, Caridi C, Gregory J, Katz S. Low literacy self-care management patient education for a multi-lingual heart failure population: results of a pilot study. Appl Nurs Res. 2016;29:122–124. doi: 10.1016/j.apnr.2015.06.002. [DOI] [PubMed] [Google Scholar]
- 177.DeWalt DA, Malone RM, Bryant ME, Kosnar MC, Corr KE, Rothman RL, Sueta CA, Pignone MP A heart failure self-management program for patients of all literacy levels: a randomized, controlled trial [ISRCTN11535170]. BMC Health Serv Res. 2006;6:30. doi: 10.1186/1472-6963-6-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Riegel B, Moser DK, Anker SD, Appel LJ, Dunbar SB, Grady KL, Gurvitz MZ, Havranek EP, Lee CS, Lindenfeld J, Peterson PN, Pressler SJ, Schocken DD, Whellan DJ; on behalf of the American Heart Association Council on Cardiovascular Nursing; American Heart Association Council on Cardiovascular Nursing; American Heart Association Council on Clinical Cardiology; American Heart Association Council on Nutrition, Physical Activity, and Metabolism; American Heart Association Interdisciplinary Council on Quality of Care and Outcomes Research. State of the science: promoting self-care in persons with heart failure: a scientific statement from the American Heart Association. Circulation. 2009;120:1141–1163. doi: 10.1161/CIRCULATIONAHA.109.192628. [DOI] [PubMed] [Google Scholar]
- 179.Feltner C, Jones CD, Cené CW, Zheng ZJ, Sueta CA, Coker-Schwimmer EJ, Arvanitis M, Lohr KN, Middleton JC, Jonas DE Transitional care interventions to prevent readmissions for persons with heart failure: a systematic review and meta-analysis. Ann Intern Med. 2014;160:774–784. doi: 10.7326/M14-0083. [DOI] [PubMed] [Google Scholar]
- 180.Ojike N, Ravenell J, Seixas A, Masters-Israilov A, Rogers A, Jean-Louis G, Ogedegbe G, McFarlane SI. Racial disparity in stroke awareness in the US: an analysis of the 2014 National Health Interview Survey. J Neurol Neurophysiol. 2016;7:365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Morgenstern LB, Bartholomew LK, Grotta JC, Staub L, King M, Chan W. Sustained benefit of a community and professional intervention to increase acute stroke therapy. Arch Intern Med. 2003;163:2198–2202. doi: 10.1001/archinte.163.18.2198. [DOI] [PubMed] [Google Scholar]
- 182.Kleindorfer D, Miller R, Sailor-Smith S, Moomaw CJ, Khoury J, Frankel M. The challenges of community-based research: the Beauty Shop Stroke Education Project. Stroke. 2008;39:2331–2335. doi: 10.1161/STROKEAHA.107.508812. [DOI] [PubMed] [Google Scholar]
- 183.Williams O, Leighton-Herrmann E, DeSorbo A, Hecht M, Hedmann M, Huq S, Gerin W, Chinchilli V, Ogedegbe G, Noble J. Hip Hop Stroke: study protocol for a randomized controlled trial to address stroke literacy. J Clin Trials. 2015;5:242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Morgenstern LB, Gonzales NR, Maddox KE, Brown DL, Karim AP, Espinosa N, Moyé LA, Pary JK, Grotta JC, Lisabeth LD, Conley KM. A randomized, controlled trial to teach middle school children to recognize stroke and call 911: the Kids Identifying and Defeating Stroke Project. Stroke. 2007;38:2972–2978. doi: 10.1161/STROKEAHA.107.490078. [DOI] [PubMed] [Google Scholar]
- 185.Hawkes MA, Ameriso SF, Willey JZ. Stroke knowledge in Spanish-speaking populations. Neuroepidemiology. 2015;44:121–129. doi: 186.1159/000381100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Miyamatsu N, Okamura T, Nakayama H, Toyoda K, Suzuki K, Toyota A, Hata T, Hozawa A, Nishikawa T, Morimoto A, Ogita M, Morino A, Yamaguchi T Public awareness of early symptoms of stroke and information sources about stroke among the general Japanese population: the Acquisition of Stroke Knowledge Study. Cerebrovasc Dis. 2013;35:241–249. doi: 10.1159/000347066. [DOI] [PubMed] [Google Scholar]
- 187.Centers for Disease Control and Prevention. Awareness of stroke warning symptoms: 13 states and the District of Columbia, 2005. MMWR Morb Mortal Wkly Rep. 2008;57:481–485. [PubMed] [Google Scholar]
- 188.Gutiérrez-Jiménez E, Góngora-Rivera F, Martínez HR, Escamilla-Garza JM, Villarreal HJ; GECEN Investigators. Knowledge of ischemic stroke risk factors and warning signs after a health education program by medical students. Stroke. 2011;42:897–901. doi: 10.1161/STROKEAHA.110.597062. [DOI] [PubMed] [Google Scholar]
- 189.Williams O, DeSorbo A, Noble J, Gerin W. Child-mediated stroke communication: findings from Hip Hop Stroke. Stroke. 2012;43:163–169. doi: 10.1161/STROKEAHA.111.621029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Williams O, DeSorbo A, Noble J, Shaffer M, Gerin W. Long-term learning of stroke knowledge among children in a high-risk community. Neurology. 2012;79:802–806. doi: 10.1212/WNL.0b013e3182661f08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Skolarus LE, Zimmerman MA, Murphy J, Brown DL, Kerber KA, Bailey S, Fowlkes S, Morgenstern LB. Community-based participatory research: a new approach to engaging community members to rapidly call 911 for stroke. Stroke. 2011;42:1862–1866. doi: 10.1161/STROKEAHA.110.609495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Aliot E, Breithardt G, Brugada J, Camm J, Lip GY, Vardas PE, Wagner M; Atrial Fibrillation Awareness and Risk Education Group; Atrial Fibrillation Association; European Heart Rhythm Association; Stroke Alliance for Europe; World Heart Federation. An international survey of physician and patient understanding, perception, and attitudes to atrial fibrillation and its contribution to cardiovascular disease morbidity and mortality. Europace. 2010;12:626–633. doi: 10.1093/europace/euq109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Reading SR, Go AS, Fang MC, Singer DE, Liu IA, Black MH, Udaltsova N, Reynolds K; Anticoagulation, Risk Factors in Atrial Fibrillation-Cardiovascular Research Network Investigators. Health literacy and awareness of atrial fibrillation. J Am Heart Assoc. 2017;6:e005128. doi: 10.1161/JAHA.116.005128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Xu W, Sun G, Lin Z, Chen M, Yang B, Chen H, Cao K Knowledge, attitude, and behavior in patients with atrial fibrillation undergoing radiofrequency catheter ablation. J Interv Card Electrophysiol. 2010;28:199–207. doi: 10.1007/s10840-010-9496-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Fang MC, Panguluri P, Machtinger EL, Schillinger D. Language, literacy, and characterization of stroke among patients taking warfarin for stroke prevention: implications for health communication. Patient Educ Couns. 2009;75:403–10. doi: 10.1016/j.pec.2008.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.McCabe PJ, Schad S, Hampton A, Holland DE Knowledge and self-management behaviors of patients with recently detected atrial fibrillation. Heart Lung. 2008;37:79–90. doi: 10.1016/j.hrtlng.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 197.Lane DA, Ponsford J, Shelley A, Sirpal A, Lip GY Patient knowledge and perceptions of atrial fibrillation and anticoagulant therapy: effects of an educational intervention programme: the West Birmingham Atrial Fibrillation Project. Int J Cardiol. 2006;110:354–358. doi: 10.1016/j.ijcard.2005.07.031. [DOI] [PubMed] [Google Scholar]
- 198.Clarkesmith DE, Pattison HM, Lane DA. Educational and behavioural interventions for anticoagulant therapy in patients with atrial fibrillation. Cochrane Database Syst Rev. 2013;6:CD008600. [DOI] [PubMed] [Google Scholar]
- 199.Clarkesmith DE, Pattison HM, Khaing PH, Lane DA. Educational and behavioural interventions for anticoagulant therapy in patients with atrial fibrillation. Cochrane Database Syst Rev. 2017;4:CD008600. doi: 10.1002/14651858.CD008600.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Clarkesmith DE, Pattison HM, Lip GY, Lane DA Educational intervention improves anticoagulation control in atrial fibrillation patients: the TREAT randomised trial. PLoS One. 2013;8:e74037. doi: 10.1371/journal.pone.0074037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Hendriks JM, de Wit R, Crijns HJ, Vrijhoef HJ, Prins MH, Pisters R, Pison LA, Blaauw Y, Tieleman RG. Nurse-led care vs. usual care for patients with atrial fibrillation: results of a randomized trial of integrated chronic care vs. routine clinical care in ambulatory patients with atrial fibrillation. Eur Heart J. 2012;33:2692–2699. doi: 10.1093/eurheartj/ehs071. [DOI] [PubMed] [Google Scholar]
- 202.January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC Jr, Conti JB, Ellinor PT, Ezekowitz MD, Field ME, Murray KT, Sacco RL, Stevenson WG, Tchou PJ, Tracy CM, Yancy CW. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society [published correction appears in Circulation 2014; 130:e270-e271]. Circulation. 2014;130:2071–2104. doi: 10.1161/CIR.0000000000000040. [DOI] [PubMed] [Google Scholar]
- 203.Seaburg L, Hess EP, Coylewright M, Ting HH, McLeod CJ, Montori VM Shared decision making in atrial fibrillation: where we are and where we should be going. Circulation. 2014;129:704–710. doi: 10.1161/CIRCULATIONAHA.113.004498. [DOI] [PubMed] [Google Scholar]
- 204.Brach C, Dreyer BP, Schillinger D Physicians’ roles in creating health literate organizations: a call to action. J Gen Intern Med. 2014;29:273–275. doi: 10.1007/s11606-013-2619-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Beckwith N, Jean-Baptiste ML, Katz A Waiting room education in a community health system: provider perceptions and suggestions. J Community Health. 2016;41:1196–1203. doi: 10.1007/s10900-016-0201-y. [DOI] [PubMed] [Google Scholar]
- 206.Fraker TD Jr, Fihn SD, Gibbons RJ, Abrams J, Chatterjee K, Daley J, Deedwania PC, Douglas JS, Ferguson TB Jr, Fihn SD, Fraker TD Jr, Gardin JM, O’Rourke RA, Pasternak RC, Williams SV, Smith SC Jr, Jacobs AK, Adams CD, Anderson JL, Buller CE, Creager MA, Ettinger SM, Halperin JL, Hunt SA, Krumholz HM, Kushner FG, Lytle BW, Nishimura R, Page RL, Riegel B, Tarkington LG, Yancy CW; on behalf of the 2002 Chronic Stable Angina Writing Committee. 2007 Chronic angina focused update of the ACC/AHA 2002 guidelines for the management of patients with chronic stable angina: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines Writing Group to develop the focused update of the 2002 guidelines for the management of patients with chronic stable angina [published correction appears in Circulation 2007;116:e558]. Circulation. 2007;116:2762–2772. doi: 10.1161/CIRCULATIONAHA.107.187930. [DOI] [PubMed] [Google Scholar]
- 207.Moser DK, Kimble LP, Alberts MJ, Alonzo A, Croft JB, Dracup K, Evenson KR, Go AS, Hand MM, Kothari RU, Mensah GA, Morris DL, Pancioli AM, Riegel B, Zerwic JJ Reducing delay in seeking treatment by patients with acute coronary syndrome and stroke: a scientific statement from the American Heart Association Council on Cardiovascular Nursing and Stroke Council. Circulation. 2006;114:168–182. doi: 10.1161/CIRCULATI0NAHA.106.176040. [DOI] [PubMed] [Google Scholar]
- 208.Lee CS, Moser DK, Lennie TA, Tkacs NC, Margulies KB, Riegel B Biomarkers of myocardial stress and systemic inflammation in patients who engage in heart failure self-care management. J Cardiovasc Nurs. 2011;26:321–328. doi: 10.1097/JCN.0b013e31820344be. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Lee CS, Suwanno J, Riegel B. The relationship between self-care and health status domains in Thai patients with heart failure. Eur J Cardiovasc Nurs. 2009;8:259–266. doi: 10.1016/j.ejcnurse.2009.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Chen AM, Yehle KS, Plake KS, Murawski MM, Mason HL. Health literacy and self-care of patients with heart failure. J Cardiovasc Nurs. 2011;26:446–451. doi: 10.1097/JCN.0b013e31820598d4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Evangelista LS, Rasmusson KD, Laramee AS, Barr J, Ammon SE, Dunbar S, Ziesche S, Patterson JH, Yancy CW. Health literacy and the patient with heart failure: implications for patient care and research: a consensus statement of the Heart Failure Society of America. J Card Fail. 2010;16:9–16. doi: 10.1016/j.cardfail.2009.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Volandes AE, Paasche-Orlow MK Health literacy, health inequality and a just healthcare system. Am J Bioeth. 2007;7:5–10. doi: 10.1080/15265160701638520. [DOI] [PubMed] [Google Scholar]
- 213.Protection of human subjects; Belmont report: notice of report for public comment. Fed Regist. 1979;44:23191–23197. [PubMed] [Google Scholar]
- 214.Livaudais-Toman J, Burke NJ, Napoles A, Kaplan CP. Health literate organizations: are clinical trial sites equipped to recruit minority and limited health literacy patients? J Health Dispar Res Pract. 2014;7:1–13. [PMC free article] [PubMed] [Google Scholar]
- 215.Ownby RL, Acevedo A, Goodman K, Caballero J, Waldrop-Valverde D. Health literacy predicts participant understanding of orally-presented informed consent information. Clin Res Trials. 2015;1:15–19. doi: 10.15761/CRT.1000105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Paasche-Orlow MK, Taylor HA, Brancati FL. Readability standards for informed-consent forms as compared with actual readability. N Engl J Med. 2003;348:721–726. doi: 10.1056/NEJMsa021212. [DOI] [PubMed] [Google Scholar]
- 217.Flesch R A new readability yardstick. J Appl Psychol. 1948;32:221–233. [DOI] [PubMed] [Google Scholar]
- 218.Paasche-Orlow MK, Brancati FL, Taylor HA, Jain S, Pandit A, Wolf MS. Readability of consent form templates: a second look. IRB. 2013;35:12–19. [PubMed] [Google Scholar]
- 219.Sudore RL, Landefeld CS, Williams BA, Barnes DE, Lindquist K, Schillinger D Use of a modified informed consent process among vulnerable patients: a descriptive study. J Gen Intern Med. 2006;21:867–873. doi: 10.1111/j.1525-1497.2006.00535.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Sugarman J, Lavori PW, Boeger M, Cain C, Edsond R, Morrison V, Yeh SS. Evaluating the quality of informed consent. Clin Trials. 2005;2:34–41. doi: 10.1191/1740774505cn066oa. [DOI] [PubMed] [Google Scholar]
- 221.Spertus JA, Bach R, Bethea C, Chhatriwalla A, Curtis JP, Gialde E, Guerrero M, Gosch K, Jones PG, Kugelmass A, Leonard BM, McNulty EJ, Shelton M, Ting HH, Decker C. Improving the process of informed consent for percutaneous coronary intervention: patient outcomes from the Patient Risk Information Services Manager (ePRISM) study. Am Heart J. 2015;169:234–241.e1. doi: 10.1016/j.ahj.2014.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Burke LE, Ma J, Azar KM, Bennett GG, Peterson ED, Zheng Y, Riley W, Stephens J, Shah SH, Suffoletto B, Turan TN, Spring B, Steinberger J, Quinn CC, American Heart Association Publications Committee of the Council on Epidemiology and Prevention, Behavior Change Committee of the Council on Cardiometabolic Health, Council on Cardiovascular and Stroke Nursing, Council on Translational Biology, Council on Quality of Care and Outcomes Research, and Stroke Council. Current science on consumer use of mobile health for cardiovascular disease prevention: a scientific statement from the American Heart Association [published correction appears in Circulation 2015;132:e233]. Circulation. 2015;132:1157–1213. doi: 10.1161/CIR.0000000000000232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Nelson LA, Mulvaney SA, Gebretsadik T, Ho YX, Johnson KB, Osborn CY Disparities in the use of a mHealth medication adherence promotion intervention for low-income adults with type 2 diabetes. J Am Med Inform Assoc. 2016;23:12–18. doi: 10.1093/jamia/ocv082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Kim KB, Han HR, Huh B, Nguyen T, Lee H, Kim MT. The effect of a community-based self-help multimodal behavioral intervention in Korean American seniors with high blood pressure. Am J Hypertens. 2014;27:1199–1208. doi: 10.1093/ajh/hpu041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Ravenell J, Leighton-Herrmann E, Abel-Bey A, DeSorbo A, Teresi J, Valdez L, Gordillo M, Gerin W, Hecht M, Ramirez M, Noble J, Cohn E, Jean-Louis G, Spruill T, Waddy S, Ogedegbe G, Williams O. Tailored Approaches to Stroke Health Education (TASHE): study protocol for a randomized controlled trial. Trials. 2015;16:176. doi: 10.1186/s13063-015-0703-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Williams O, Hecht MF, DeSorbo AL, Huq S, Noble JM. Effect of a novel video game on stroke knowledge of 9- to 10-year-old, low-income children. Stroke. 2014;45:889–892. doi: 10.1161/STROKEAHA.113.002906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Plescia M, Groblewski M, Chavis L A lay health advisor program to promote community capacity and change among change agents. Health Promot Pract. 2008;9:434–439. doi: 10.1177/1524839906289670. [DOI] [PubMed] [Google Scholar]
- 228.Plescia M, Herrick H, Chavis L. Improving health behaviors in an African American community: the Charlotte Racial and Ethnic Approaches to Community Health project. Am J Public Health. 2008;98:1678–1684. doi: 10.2105/AJPH.2007.125062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Allen JK, Dennison-Himmelfarb CR, Szanton SL, Bone L, Hill MN, Levine DM, West M, Barlow A, Lewis-Boyer L, Donnelly-Strozzo M, Curtis C, Anderson K. Community Outreach and Cardiovascular Health (COACH) trial: a randomized, controlled trial of nurse practitioner/community health worker cardiovascular disease risk reduction in urban community health centers. Circ Cardiovasc Qual Outcomes. 2011;4:595–602. doi: 10.1161/CIRCOUTCOMES.111.961573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Brownstein JN, Bone LR, Dennison CR, Hill MN, Kim MT, Levine DM. Community health workers as interventionists in the prevention and control of heart disease and stroke. Am J Prev Med. 2005;29(suppl 1):128–133. doi: 10.1016/j.amepre.2005.07.024. [DOI] [PubMed] [Google Scholar]
- 231.Brach C, Keller D, Hernandez LM, Baur C, Parker R, Dreyer B, Schyve P, Lemerise AJ, Schillinger D. Ten attributes of health literate health care organizations. Institute of Medicine; 2012. https://nam.edu/wp-content/uploads/2015/06/BPH_Ten_HLit_Attributes.pdf. Accessed April 18, 2016. [Google Scholar]