Abstract
Transitional diabetes self-management (DSM) for children and their families is complicated. This article was undertaken to provide an exemplar of DSM strategies used by one family that were based on developmental milestones from preschool through college age. Two brothers who were both diagnosed with type 1 diabetes before the age of 2 years reflected on how their parents began a DSM navigation process during their early preschool years. Personal strategies and recommendations successfully resulted in both youths transitioning to college. With the parents serving as DSM coaches to the boys, an interdependent relationship was built. Key recommendations include 1) starting early, 2) being consistent and flexible, 3) using “invisible actions” and “what ifs,” 4) incorporating technology and community resources into DSM, and 5) building confidence with shared problem-solving.
More young children are being diagnosed with type 1 diabetes than ever before (1). An annual 1.4% increase (P = 0.03) was recently reported; for example, in 2002–2003, there were 19.5 cases per 100,000 youths/year compared to 21.7 cases per 100,000 youths/year in 2011–2012. Although between 2002 and 2012, the 0- to 4-year-old age-group had a slightly decreased incidence of type 1 diabetes, the 5- to 9-year-old age-group had a significantly increased incidence.
The increase in numbers of younger children being diagnosed earlier suggests that children are living with type 1 diabetes longer, which heightens the need for effective disease management. Without good management, the risk for these children to develop long-term physical and mental health complications intensifies, as does the care burden for longer periods of time.
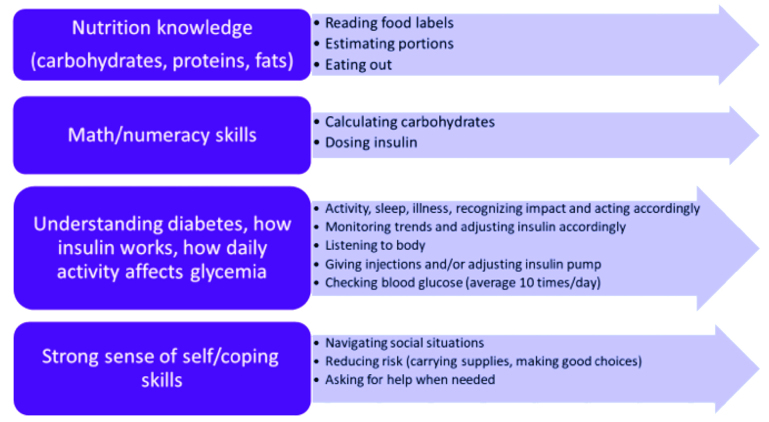
Successful management of type 1 diabetes is an active, daily, fluid, iterative process that varies with developmental stages. The management transition from parents to child takes place over years and, although the pre-teen years are appropriate to actively begin the self-management process, planning for this transition should be considered early on. Diabetes self-management (DSM) requires building family competency in nutrition knowledge, numeracy, and understanding of diabetes and how insulin works in relation to food and activity, as well as developing confidence and problem-solving skills (Figure 1) (2–5).
FIGURE 1.
Internal and external skills/tasks required for DSM.
Two of the co-authors (B.T., an adolescent with type 1 diabetes, and S.S.-B., a family nurse scientist) who have worked together on family-focused interventions for several years recently discussed how B.T. and his brother (C.T.) came to successfully manage their chronic condition. Both brothers (ages 19 and 18 years, respectively) had been diagnosed with type 1 diabetes before 2 years of age and are healthy and now attending college. Although still strongly connected to their parents, they are both successfully managing their type 1 diabetes fairly independently with parental and health care provider (HCP) guidance as needed, a scenario that has been referred to as “interdependence” (6). In our discussion, we were curious about how this process occurred. We decided that the brothers would journal and reminisce from their personal perspectives (with parental input) about the strategies their parents used to raise the boys to be able to proficiently manage their chronic condition by the time they went to college, a process that did not happen overnight.
The purpose of this article is to provide a rich description of the transition from preschool years to college from the perspective of the two brothers, focusing on building blood glucose management (BGM) skills, with exemplars to illustrate the process. The aims include 1) to describe the gradual shift of developmentally appropriate tasks and experiences over this time period from parental management to shared management to interdependent management; 2) to describe strategies used to handle BGM in partnership during active and weekend days, sick days, sports, and social activities; and 3) to offer suggestions and tips for clinicians to advise parents regarding gradual and consistent management strategies to prepare for their child’s eventual transition to college.
Design and Methods
Qualitative description was used to explore developmental experiences with learning DSM (7). This approach allowed for clearly representing the perspectives of the participants and was a good fit with the journaling technique.
Theoretical Underpinnings
We used the Family Management Style Framework (FMSF) (8) and the American Diabetes Association’s (ADA’s) position statement on developmental milestones for self-management (Table 1) (9) to undergird our analysis and findings. The FMSF is a perfect fit for exploring how families deal with and respond to management challenges. It considers how families define the chronic condition in relation to family life (i.e., as manageable vs. as a burden), the behaviors used to manage the condition on a daily basis, and the perceived consequences (i.e., future expectations) of the disease as it affects the child and family-related activities. Contextual influences must also be considered, including community and/or peer support, relationships with HCPs, school advocacy, and socialization resources within the family’s community. All of these factors can have either a positive or negative influence on the family’s response.
TABLE 1.
Developmental Milestones Related to Type 1 Diabetes Management
| Developmental Stage (Ages) | Normal Developmental Tasks | Type 1 Diabetes Management Priorities | Family Issues in Type 1 Diabetes Management |
|---|---|---|---|
| Preschool and early elementary school (3–7 years) | • Developing initiative in activities and confidence in self |
• Preventing hypoglycemia • Coping with unpredictable appetite and activity • Positively reinforcing cooperation with regimen • Trusting other caregivers’ management |
• Reassuring child that diabetes is no one’s fault • Educating other caregivers about management |
| Older elementary school (8–11 years) | • Developing skills in athletic, cognitive, artistic, and social areas • Consolidating self-esteem/peer group |
• Making diabetes regimen flexible • Child learning short- and long-term benefits of optimal control |
• Maintaining parental involvement in diabetes management while allowing for shared care for special occasions • Continuing to educate school and other caregivers |
| Early adolescence (12–15 years) | • Managing body changes • Developing a strong sense of self-identity |
• Increasing insulin requirements during puberty • Diabetes management and blood glucose control becoming more difficult • Weight and body image concerns |
Renegotiating parental and teenager’s roles in diabetes management Child learning coping skills to enhance ability to self-manage Preventing and intervening in diabetes-related family conflict Monitoring for signs of depression, eating disorders, and risky behaviors |
| Later adolescence (16–19 years) | • Establishing a sense of identity after high school (decisions about location, social issues, work, and education) |
• Starting an ongoing discussion about transition to a new diabetes team (discussion begins in earlier adolescent years) • Integrating diabetes into new lifestyle |
• Supporting the transition to independence • Learning self-management coping skills • Preventing family conflict • Monitoring for signs of depression, eating disorders, and risky behaviors |
Adapted from ref. 2.
Organization of Management Strategies
Authors M.L.P. and S.S.-B. compared their co-authors’ journaling perspectives and their family’s approach to transition from early life, to school age, to high school and college. Once the brothers had described their experiences with learning self-monitoring of blood glucose and other diabetes management strategies across the developmental milestones, the other two authors clustered the information into age-related strategies, highlighting key BGM points that facilitated the brothers’ eventual DSM activities and expectations. All authors reviewed, questioned, and discussed each management component, identifying illustrations that conveyed day-to-day experiences (10). Tables 2–5 are written from the brothers’ points of view and illustrate diabetes management across the developmental milestones, allowing readers to compare and contrast the family strategies that promoted the brothers’ eventual interdependence with their parents with regard to diabetes management.
TABLE 2.
Strategies for Gradually Performing BGM by Developmental Stage (According to B.T. and C.T.)
| Task | Preschool | Older Elementary School | Early Adolescence | Later Adolescence (Current) |
|---|---|---|---|---|
| General BGM | • Began helping with BGM by inserting strips into the glucose meter (∼2 years of age) • Performed glucose checks with supervision • Injections given by parents • Got first pump (∼7 years of age); code on it, so no accidental doses • Once in school, would go to the nurse with a buddy to check blood glucose twice daily • Focused on set times to check blood glucose at school, camp, and home • Checked blood glucose 8–10 times per day, parents checking or reminding (stop activity or leave during class to check) • Approached teachers to ask to go to the nurse • Worked on identifying low and high blood glucose levels and how they felt to us |
• Carried a “diabetes snack bag” with juices, meter, and snacks • Continued to carry pump in a fanny pack • Began checking blood glucose without supervision • Began programming pump independently at home; at school, the nurse would check pump settings • Went to nurse twice daily during class and another time at lunch for blood glucose checks • Understood the differences between feeling high and feeling low |
• Began going out more; would always carry a backpack with supplies • Began to play organized sports; talked to coaches about what we might need to do on the bench or in the locker room • Talked to teachers about what having diabetes meant and what we would need to do |
• Essentially complete independence with BGM • Still rely on parents to order supplies • Both carry a meter around in backpack at school or in the car • Check blood glucose before driving • When sleeping over at a friend’s house, text parents glucose result before going to bed |
TABLE 5.
Smooth Transition to College
| General | Considerations for Choosing a College | Choosing a Career | Considerations for College and Dorm Life | |
|---|---|---|---|---|
| BGM suggestions and thoughts from the boys (B.T. and C.T.) | • Had already gotten used to daily life with diabetes; very comfortable with blood glucose checks, infusion set changes, injections (if needed), carbohydrate counting, and so forth | • Distance from home Programs of study • Food services (allergies) |
• Still not sure but would like to be involved in the diabetes community in some way | • Assigned to a single room to better manage diabetes needs, able to appeal to Residence Life for privacy and security (with regard to insulin, pump, CGM supplies, and maintenance) • Prepare for potential emergencies (e.g., pump failure or running out of supplies) by assembling a folder with appropriate contacts (i.e., doctor, campus health resources, pharmacy, and insurance) • Address food situation (make sure to have allergy-friendly options and also always have snacks and juice in the dorm room • Peer support important |
| Suggestions and thoughts from the family | • Proactive early planning allowed the family to focus on the joy of sons growing up and following their passions at college • Use of technology for DSM support |
Results
BGM Strategies
We have summarized perspectives on key management strategies regarding BGM in general, as well as specific strategies related to sports and travel and sick-day management across the developmental milestones of preschool, older elementary, and early and late adolescence; we also addressed key considerations for the transition to college.
General strategies for BGM are shown in Table 2. DSM tasks were introduced early on, with gradual building on developmentally appropriate and individualized skills. For example, during the preschool milestone, “play to learn” was an important strategy used with the young brothers. They were allowed to play with the glucose meter by inserting a test strip into the machine. Their mother also had them guess if their blood glucose numbers were high or low, transforming the task of learning to recognize high and low blood glucose into a game. She incorporated sign language (hand up for high, hand down for low) into the game that was associated with how they felt (e.g., jittery or dizzy), which they both remembered as being fun.
Of course, being brothers close in age was helpful for both, allowing them to observe, model, support, and reinforce their sibling’s DSM as the boys often approached tasks a bit differently but with the same expectations of interdependence. By elementary school, both boys reported that they understood the difference between how their symptoms presented with high versus low blood glucose levels. Figure 2 is a drawing the boys made during elementary school illustrating their growing understanding.
FIGURE 2.

Drawing by the two co-authors during their elementary school years.
Another example of this gradual DSM education was strategic placement of glucose meters to remind the boys to check their blood glucose. For example, a glucose meter would be placed by the boys’ beds, another on the kitchen table, and another in the car when they began to drive. This strategy gave visual cues that BGM should occur before and after sleeping, around mealtimes, and before driving.
The boys’ parents were strong advocates of having the boys approach their school nurse from preschool age on if they felt that their blood glucose may be high or low, thus normalizing this action to avoid making the boys feeling embarrassed about their condition. This procedure also supported the boys’ continued gradual transfer to independent DSM. Both boys were always prepared with a backpack of diabetes-related supplies and knew what to do regarding daily management. For example, they had a permanent backpack in the trunk of the car with nonperishable snacks, juice, and extra pump supplies for emergencies.
As they grew into adolescence, they took charge of more management so that, by late adolescence with college on the horizon, they were both essentially independent in BGM, consulting with their parents as needed.
Continuous glucose monitoring (CGM) devices, introduced when the brothers were in high school, made life for the family more manageable, although it could be perceived as a double-edge sword. A CGM device that transmitted glucose readings automatically to the boys and their parents via smartphone reduced parental anxiety. However, the family shared stories about the parents receiving low readings on their smartphone over the years and experiencing anxiety if they were not able to reach their son. They described back-up safety strategies they developed such as their current practice of making sure the phone numbers of the boys’ college roommates are readily available to all concerned.
Sports and Travel
Table 3 illustrates gradual developmental strategies incorporated into day-to-day management associated with sports and other travel activities. Sports involvement for both boys has long been important to this family, which began early on using “invisible actions” to prevent the boys from feeling embarrassed or different from their peers. Starting in the early years after their sons were diagnosed, both parents became active participants in organized sports from preschool through the older elementary school years. For example, during the preschool years, if one of the parents observed one of their boys exhibiting signs of low blood glucose during a sports activity, the parent would discreetly call a time out and give all the children a break with popsicle treats and then resume the activity. In most sports-related activities, the parents would check their sons’ blood glucose during breaks between innings or periods rather than interrupting play, thus reducing the focus on diabetes management.
TABLE 3.
BGM Around Sports and Travel by Developmental Stage (According to B.T. and C.T.)
| Task | Preschool | Older Elementary School | Early Adolescence | Later Adolescence (Current) |
|---|---|---|---|---|
| BGM around sports and travel | • At younger part of this stage, playing in the yard with friends, routine stops to check blood glucose as suggested by parents • Parent(s) would ask everyone if they wanted a popsicle or something else with carbohydrate if play had gone on for a while; discreet about preventing lows • Stopped to check blood glucose during playtime breaks, or mom would step in (always sure to be discreet) • For travel, parents were always there and so were usually responsible for bringing supplies • Parents would check blood glucose at mealtimes and usually other set times (∼2 hours before or after meals) |
• Playing baseball and hockey, would have a “snack bag” on the bench • Would alter pump sites to try and have pump pack (fanny pack) face away from the pitcher so it would not get hit • Figured out a way to put pump pack under hockey pants, as with baseball • Checked blood glucose in locker room between periods or on bench between innings • Knew parents had talked to coaches about potential needs that could arise • Participated in social and school-related activities of interest versus placing restrictions on daily life |
• Responsible for checking glucose before and after activity, although often with reminders from parents • Responsible for packing bag with appropriate snacks and diabetes supplies (mom usually checked to make sure it was good; eventually though, entirely our responsibility) • For extended travel, mom would usually pack the diabetes supplies • “What ifs” discussed before travel: passing out, what to do |
• Keep a drawstring bag on the hockey bench during practice/games and in the gym locker • Fill a sports bottle with 50% juice/Gatorade and 50% water to sip throughout activity • Check blood glucose right before going out to activity; make sure glucose is ∼180mg/dL and steady (on CGM) • After intense activity, blood glucose can become high temporarily. Given this knowledge, do not take corrective insulin unless taking it simultaneously with a snack. If so, reduce the insulin dose because of the heightened effects of insulin after intense activity • Entirely responsible for packing supplies for trips; bag is packed a day in advance while mentally going through all the potential situations that could arise • Travel without fear, but with planning and communication |
That is not to say they were not transparent about their sons’ condition because they felt they needed to model acceptance and transparency for themselves and their sons. The parents informed coaches, so they, too, knew their sign language and could read the boys’ behavioral cues. This strategy has strengthened the boys’ friendships across time. Diabetes is just something the boys need to deal with, and their friends see diabetes management as a normal accommodation—an important life lesson for all. Over time, this parental modeling helped the boys transition to taking responsibility for talking to their coaches and other adults such as teachers and school nurses about their health care needs.
Technology played an important part in their overall developmental participation in DSM, especially around sports activities. Both boys used insulin pumps and eventually CGM devices. As B.T. stated, “This gave me the ability to explore, participate more with organized sports, and socialize with my friends, often outside of my parents’ supervision.” They also figured out pragmatic tricks such as padded clothing to protect their pump and CGM devices when playing baseball or hockey.
“What If” Strategy
One important strategy the boys’ father adopted was to review the “what ifs” that may occur when the boys were away from home. This provided opportunities for problem-solving through hypothetical situations, beginning in preschool with “What if you feel like you’re passing out?” and advancing as the boys matured into “What if you run out of supplies?” and “What if your infusion pump falls out?” This preparation allowed the boys to develop key DSM decision-making skills by the time they went to college, while still having the opportunity to seek advice from their parents who were only a phone call or a text away.
Sick-Day Management
BGM and sick-day management (Table 4) during the early years were completely managed by the parents with developmentally incremental sick-day management education for the boys. With the initiation of insulin pumps and CGM, sick-day management became easier (e.g., watching blood glucose trends and increasing insulin when trending high). As the boys became more independent, they were encouraged to not ignore symptoms and instead to acknowledge how they were feeling and act upon it appropriately (e.g., checking for ketones, using CGM data, and, if they could not eat, having a sugar-sweetened drink to correct low-trending blood glucose).
TABLE 4.
BGM and Sick-Day Management (According to B.T. and C.T.)
| Task | Preschool | Older Elementary School | Early Adolescence | Later Adolescence (Current) |
|---|---|---|---|---|
| BGM and sick-day management | • Parent(s) took care of everything • Parent(s) checked blood glucose, made sure we were drinking fluids, as well as getting insulin and carbohydrates Parent(s) checked ketones for blood glucose >200 mg/dL • If persistent highs/vomiting, parent(s) took us to doctor and stayed in contact with hospital Increased blood glucose checks • Used regular insulin for sick days • Because ketones act as good indicators for sickness, ketones and high blood glucose appeared before symptoms of illnesses • If very sick, doctor visit to get IV to prevent diabetic ketoacidosis |
• The pump made it easier to raise basal rate when blood glucose was consistently high (20–50% increase if ketones were high) • Checked blood glucose throughout the day • Checked ketones if high (if so, more insulin) • Lots of fluids (especially if ketones were high) Less contact with the doctor |
• Blood glucose checks throughout day • Lots of fluids • If blood glucose was >250 mg/dL, checked ketones • Boosted basal insulin to keep ketones away (figured out sick days from experience) • Better control of high blood glucose and symptoms of sickness due to better understanding of body • Checked ketones if blood glucose was high and gave even more insulin; prevention was focus |
• Check for ketones if blood glucose is >250 mg/dL for a couple of readings (rarely) or if feeling particularly terrible • Check blood glucose often (use CGM usually) • Increase basal if blood glucose is high • Lots of fluids • If unable to eat, take sugary drinks with insulin |
Transition to College
Table 5 summarizes the transition process that was the culmination of years of gradually shifting DSM responsibilities from the parents to their sons. The sons described this process as being fairly seamless because their parents had been preparing them bit by bit since their preschool years. Because they were already accustomed to performing daily DSM tasks, there were no surprises when it was time to move to their respective campuses. They were prepared for potential emergencies and knew whom to call at school. The family had developed strategies such as making sure the volume on the CGM device was turned high and attaching the device to a speaker at bedtime to alert a sleeping adolescent that his blood glucose was low. College roommates were informed of potential medical issues, and food was made readily available in the dorms. The end result of all of this planning and preparation is nicely illustrated in this statement by B.T.: “I found myself advocating for myself. My dad’s hypotheticals when living at home had become a sort of habit where I would give ‘what ifs’ to myself whenever I left the dorm.”
Discussion and Clinical Implications
Mapping the shift of DSM from the parents to the adolescent sons in this family via developmental milestones provides many pragmatic recommendations for nurses and other HCPs working with families. When we consider the internal and external skill requirements necessary to master DSM, we can see that the process is complex (3,5). Yet we found from our adolescent co-authors’ perspectives that there were some key strategies that led to their successful transition to interdependent DSM. These accomplishments can be framed by the strength-based FMSF components of having a positive perspective on DSM—that it is manageable without having it overtake family life, especially if contextual influences are accessed and used to provide additional support.
Nurses and HCPs working with families over time can facilitate and encourage this type of plan well ahead of the college transition (4). Recommendations that families can be encouraged to incorporate into their DSM transition plan are listed in Table 6.
TABLE 6.
Takeaway Messages for Preparing a Child for DSM Interdependence
|
• Start early • Be consistent but flexible • Gradually shift responsibilities from parent to child • Use problem-solving strategies and available technology • Make the transition family-focused (as opposed to condition-focused) • Address “invisible actions” (e.g., where/when to discreetly adjust insulin pump and CGM device and check blood glucose) • Locate community and health care provider resources • Build confidence • Have fun together! |
Starting early means keeping in mind children’s developmental level while gradually teaching them about their disease with the goal of interdependence by the time they are ready for college. Consistency and flexibility are essential to allow children to live and play normally as the main DSM goal is creatively incorporated into their daily activities. The shift of responsibilities is again developmentally purposeful and incremental as it moves from adult delivery of care and supervision (including delivery of insulin, BGM, and carbohydrate counting) to allowing teens to eventually be in charge of an increasing portion of their DSM needs until interdependence is achieved.
This approach includes problem-solving and the use of available technology. For example, as suggested earlier, developmental strategies can be used to develop game-like instruction to engage children in learning DSM. Uploading blood glucose data to a software program that allows school-aged children to view their personal glucose trends can be fun and educational at the same moment. Reviewing glucose data can also set the stage for older adolescents to regularly use CGM devices to see daily trends and correct short-term, spontaneous problems, as well as viewing trends over longer periods of time, which enables better understanding of recurring problems.
The family-focused management pattern of the FMSF, rather than a condition-focused management style, allowed our adolescent co-authors to grow up as normally as possible. The goal was to make sure they were healthy and maintaining good glycemic control without allowing the condition to take over their family life (11). How a family accomplishes this is partially through “invisible actions” such as those described earlier in the management behaviors around sports (e.g., checking blood glucose during natural breaks and providing snacks for all of the players).
Finally, a strong recommendation not only for parents, but also for HCPs is to focus on building DSM confidence in children with diabetes over time. When high or low blood glucose levels occurred, our adolescent co-authors’ parents never yelled, but instead initiated a problem-solving session or teachable moment. Asking “How can we solve this and make it less severe or eliminate the situation in the future?” goes much further than saying “You are going to end up blind or on dialysis!” (12). As our wise-beyond-their-years adolescent co-authors noted, they are very good at understanding DSM and predicting what may work in unique situations based on the confidence they developed over time through their parents’ nurturing, skill, and dedication. The parents’ ultimate goal of this long process was to ensure that their sons would be self-sufficient by the time they went to college.
Limitations
We recognize that this report includes only two adolescent perspectives (with concurrence from their parents) on strategies for gradually learning DSM over several developmental milestones. We also acknowledge that this family has abundant financial, social, educational, and environmental resources, resulting in a rich culture of health. Our goal as HCPs is to conduct family assessments through which we identify and acknowledge families’ unique needs and provide education, support, and resource referrals to better support those who are struggling with basic needs as well as with DSM. However, we maintain that there are no magic bullets other than parents systematically planning for transition of DSM from a developmental framework with the goal of interdependent self-sufficiency that fits their family. This same pragmatic goal, which includes consideration of each child’s developmental abilities, should be used when raising any child with special health care needs.
Conclusion
We have, through mapping and journaling, provided pragmatic examples across several developmental milestones of childhood of family strategies for incrementally transferring DSM from parents to adolescents. As Comeaux and Jaser (6) suggested, when focusing on metabolic control in adolescents, more attention should be paid to how families approach the whole transition of the DSM process. We have described here the history of an exemplar family who started early, worked gradually, and are now at the college phase of their children’s lives having met the long-term goal of facilitating the boys’ performance of DSM with parental coaching as needed.
Acknowledgments
Duality of Interest
No conflicts of interest relevant to this article were reported.
Author Contributions
B.T. and C.T. wrote the diabetes management strategies and edited the manuscript. M.L.P. contributed to discussion and edited the manuscript. S.S.-B. developed the concept and wrote and edited the manuscript. S.S.-B. is the guarantor of this work and, as such, had full access to the developed strategy in the article and takes responsibility for the integrity of the data shared and its accuracy.
References
- 1.Mayer-Davis EJ, Lawrence JM, Dabelea D, et al. Incidence trends of type 1 and type 2 diabetes among youths, 2002–2012. N Engl J Med 2017;376:1419–1429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chiang JL, Kirkman MS, Laffel LM, Peters AL. Type 1 diabetes through the life span: a position statement of the American Diabetes Association. Diabetes Care 2014;37:2034–2054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Babler E, Strickland CJ. Normalizing: adolescent experiences living with type 1 diabetes. Diabetes Educ 2015;41:351–360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Babler E, Strickland CJ. Helping adolescents with type 1 diabetes “figure it out.” J Pediatr Nurs 2016;31:123–131 [DOI] [PubMed] [Google Scholar]
- 5.Babler EK, Strickland CJ. Moving the journey towards independence: adolescents transitioning to successful diabetes self-management. J Pediatr Nurs 2015;30:648–660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Comeaux SJ, Jaser SS. Autonomy and insulin in adolescents with type 1 diabetes. Pediatr Diabetes 2010;11:498–504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Willis DG, Sullivan-Bolyai S, Knafl K, Cohen MZ. Distinguishing features and similarities between descriptive phenomenological and qualitative description research. West J Nurs Res 2016;38:1185–1204 [DOI] [PubMed] [Google Scholar]
- 8.Knafl KA, Deatrick J, Havill NL. Continued development of the family management style framework. J Fam Nurs 2012:11–34 [DOI] [PubMed] [Google Scholar]
- 9.Haas L, Maryniuk M, Beck J, et al. National standards for diabetes self-management education and support. Diabetes Care 2014;37:S144–S153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77–101 [Google Scholar]
- 11.Knafl KA, Deatrick J, Knafl G, Gallo A, Grey M, Dixon J. Patterns of family management of childhood chronic conditions and their relationship to child and family functioning. J Pediatr Nurs 2013;28:523–535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dickinson JK, Guzman SJ, Maryniuk MD, et al. The use of language in diabetes care and education. Diabetes Educ 2017;43:551–564 [DOI] [PubMed] [Google Scholar]