Abstract
Context
Interventions are required that address patients’ medically related financial needs.
Objective
To evaluate a Financial Navigator pilot addressing patients’ concerns/needs regarding medical care costs in an integrated health care system.
Methods
Adults (aged ≥ 18 years) enrolled at Kaiser Permanente Northwest, who had a concern/need about medical care costs and received care in 1 of 3 clinical departments at the intervention or comparison clinic were recruited between August 1, 2016, and October 31, 2016. Baseline and 30-day follow-up participant surveys were administered to assess medical and nonmedical socioeconomic needs, satisfaction with medical care, and satisfaction with assistance with cost concerns. Physicians at both clinics were invited to complete a survey on medical care costs. We assessed participant characteristics and survey responses using descriptive statistics and 30-day change in satisfaction measures using multivariable linear regression models.
Results
Eighty-five intervention and 51 comparison participants completed the baseline survey. At baseline, intervention participants reported transportation (52.9%), housing (38.2%), and social isolation (32.4%) needs; comparison participants identified employment (33.3%), food (33.3%), and housing (33.3%) needs. Intervention participants reported higher satisfaction with care (p = 0.01) and higher satisfaction with cost concerns assistance (p = 0.01) vs comparison participants at 30-day follow-up, controlling for baseline responses. Although most physicians (80%) reported discussing medical care costs with their patients, only 18% reported knowing about their patients’ financial well-being.
Conclusion
We demonstrated the promise of a novel Financial Navigator pilot intervention to address medical care cost concerns and needs, and underscored the prevalence of nonmedical social needs in an economically vulnerable population.
Keywords: financial hardship, financial navigator, medical costs, patient-reported outcomes, physician beliefs, social needs
INTRODUCTION
The US is experiencing rising health care prices and shifting health care policies. Along with these changes, the out-of-pocket costs that individuals and families must pay for health care have far outpaced wage growth.1,2 In 2017, for example, US workers with employer-based health insurance paid average annual premium contributions of $1213 for single coverage and $5714 for family coverage.3 This is in addition to annual deductibles of $1505 for single coverage and $2645 for family coverage.3 During the same period, approximately one-third of American adults with health insurance reported they had trouble affording their health insurance premiums and other out-of-pocket costs, 40% had difficulty affording their deductible, and nearly 25% worried about not being able to afford health care.4 Faced with difficulties paying for health care, many Americans are deciding to delay or skip recommended medical treatment or prescription medications because of costs.4,5
Financial issues associated with medical costs can also have other major consequences for individuals and their families. Many families struggle with financial pressures arising from balancing their health needs with their basic social and economic needs. More than 70% of Americans, for example, report having to cut back on spending for basic necessities such as food, clothing, and transportation. Similarly, about 60% of Americans need to use up all or most of their savings to pay their medical bills.4 Nevertheless, basic needs such as financial hardship, food insecurity, and housing instability greatly influence health and may account for up to 40% of negative health outcomes.6–9 This recognition has led to increased efforts to develop interventions that reduce medically related financial hardship10–12 as well as address social and economic needs within the health care delivery system.13,14
Importantly, there is a need for interventions that address medically related financial needs and reduce financial hardship from medical care.15 A growing body of evidence suggests that social and economic needs interventions may help identify patients most in need. This can lead to interventions to reduce the burden of basic social and economic needs by increasing connections with community resources (eg, food banks).14,16–18 Among these studies, however, none have reported findings on the impact of the interventions on medically related financial needs. To fill this gap, we report findings from a novel Financial Navigator (FN) pilot designed to address the medical care cost needs and concerns of patients receiving primary and specialty care in an integrated health care delivery system.
METHODS
Intervention Setting
Kaiser Permanente Northwest (KPNW) is an integrated health care system that provides health insurance coverage and medical services to approximately 580,000 members in Oregon and Southwest Washington. KPNW operates 34 medical offices and 2 hospitals. At KPNW, patient navigators are an important part of the health care team, supporting members by identifying, prioritizing, and addressing their nonmedical social and economic needs. Patient navigators engage with KPNW members through phone, email, or in-person appointments when possible. Standard patient navigation support includes interacting with patients to understand and identify their nonmedical social or economic needs, educating patients about KPNW-specific resources (eg, KPNW Medical Financial Assistance Program) and community resources available to meet the identified needs, and care coordination to help members obtain resources.
Financial Navigator Intervention
The FN pilot was developed to enhance patient navigators’ ability to address patients’ needs and concerns surrounding medical care costs. This pilot entailed a 2-pronged approach: 1) providing enhanced training to 1 patient navigator (to become the FN), including 40 hours of specialized training in financial assistance resources to assist with medical care costs, cost estimation tools, health insurance benefits, and meetings with operational and clinical staff and leadership; and 2) building new capabilities in the electronic health record (EHR) to enable health care staff to make referrals to the FN. After completing this training, the FN provided services at a single KPNW medical campus, which became the pilot intervention clinic.
The FN pilot was conducted in 3 clinical departments (ie, Primary Care, Rheumatology, Ophthalmology) located in 2 separate medical offices (hereafter referred to as the intervention clinic and comparison clinic). The intervention and comparison clinics were selected because they had all 3 clinical departments operating in the same medical campus. This quality improvement intervention was deemed exempt from the need for institutional review board approval.
Participants
Inclusion Criteria
We developed and implemented the following criteria to identify eligible participants: Be aged 18 years or older at the time of the pilot; be an enrolled member at KPNW; have received medical care in 1 of the 3 participating departments at the intervention or comparison clinics; and have a medical care cost concern/need (eg, unable to afford prescription medication). Comparison clinic participants also were required to have a valid email address documented in the EHR.
Intervention Participants
Patients who received care at the intervention clinic and reported a concern/need about medical care costs to a health care team member (eg, physician, nurse, or other frontline health care staff) were referred by health care staff (eg, physician, nurse, medical assistant) to the FN via a message in the EHR. The FN then attempted to contact the patient and invite him/her to participate (a proactive, system-driven approach). Patients who agreed to participate completed the baseline survey. Approximately 213 patients were referred to the FN pilot between August 1, 2016, and October 31, 2016, and 97 completed the baseline survey (45.5% response rate). Twelve patients were excluded from analysis because of ineligibility (eg, not a KPNW member at the time of the pilot or did not receive care at the intervention clinic). This resulted in a final sample of 85 intervention clinic participants.
Comparison Participants
We used the EHR to identify comparable patients with a visit to 1 of the 3 participating clinical departments (ie, Primary Care, Rheumatology, Ophthalmology) at the comparison clinic within the 6 months before the FN pilot (N = 6324). These patients were then sent a secure email message by project staff, inviting them to participate in the baseline survey. Among the approximately 374 patients who completed the baseline survey (6% response rate), patients were defined as having a medical care cost concern/need if they reported any of the following financial or economic needs on the baseline survey: Medical bills, treatment costs, or utility/bill pay. Fifty-one patients were identified as having a medical care cost concern/need and were included in the comparison clinic cohort.
Comparison clinic participants were eligible for standard patient navigation services only. To maintain the integrity of the intervention, patients who received care at the comparison clinic and who reported a social or economic need to a health care team member were given a phone number to contact a patient navigator (a patient-driven approach). We could not assess whether patients reported their cost concerns/needs during their medical visits or whether they were referred to a patient navigator because of these cost concerns/needs.
Data Collection and Measures
Baseline and 30-day follow-up participant surveys were administered to assess the following: 1) social and economic needs, 2) satisfaction with medical care, and 3) satisfaction with assistance with cost concerns. Follow-up assessment included: 1) satisfaction with medical care, 2) satisfaction with cost concerns/needs assistance, and 3) satisfaction with navigation services (intervention only). For intervention participants, baseline survey administration was conducted either by phone or in-person (by the FN), and follow-up surveys were conducted by mail (with paid return envelope) or via REDCap (Research Electronic Data Capture) Survey software (REDCap Consortium, Vanderbilt University, Nashville, TN).19 For comparison participants, both baseline and follow-up surveys were conducted using REDCap Survey software.19 Participants who did not complete the follow-up survey after initial contact were sent reminder emails 1 week after the initial attempt.
For all participants who completed the baseline survey, we used EHR data to collect baseline patient sociodemographic and disease characteristics, including age at the time of intervention, sex, race, Hispanic ethnicity, Health Plan type; length of enrollment in the Health Plan, US Census-level household income, marital status, educational attainment, body mass index (BMI), Charlson Comorbidity Index, and tobacco use.
Physicians in the participating departments at both clinics (N = 70) were invited to complete a survey to assess: 1) perceptions about the costs of medical care and treatment, 2) patient financial well-being, and 3) satisfaction with the financial navigator (this last item available for physicians at intervention clinic only).
Statistical Analysis
We used descriptive statistics to evaluate participants’ demographic and clinical characteristics, as well as survey response rates. Other than the section on social and economic needs, all items on the patient survey were presented on a 5-point Likert scale: 0, “strongly disagree”; 1, “disagree”; 3, “neutral”; 4, “agree”; and 5, “strongly agree.” For final analyses, we dichotomized responses (1 = “agree” or “strongly agree”; 0 = “neutral,” “disagree,” or “strongly disagree”) and evaluated differences using χ2 tests. We used ordinary least squares regression to assess change in member-reported satisfaction from baseline to 30-day follow-up, controlling for baseline values. We conducted analyses and data management in SAS Version 9.4 (SAS Institute Inc, Cary, NC) and Stata Version 13.1 (StataCorp LLC, College Station, TX).
RESULTS
Table 1 shows participants’ baseline demographic and clinical characteristics. Most participants in both the intervention and comparison groups were women, non-Hispanic, and white. Approximately half of participants in both the intervention group (48%) and comparison group (52%) resided in an area with annual household incomes below $50,000. Intervention participants were older (mean age = 66.5 years) and had lower mean body mass index (30.3 kg/m2) than comparison participants (mean age = 58.7 years, mean body mass index = 34.6 kg/m2). A low percentage of both intervention (15%) and comparison (18%) participants were tobacco users.
Table 1.
Participant baseline demographic and clinical characteristicsa
| Characteristic | Intervention (n = 85) | Comparison (n = 51) | p value |
|---|---|---|---|
| Demographic | |||
| Age, years, mean (SD)b | 66.5 (17.3) | 58.7 (13.7) | 0.007 |
| Women, no. (%)b | 53 (63.9) | 35 (68.6) | 0.572 |
| White, no. (%)c | 72 (91.1) | 46 (90.2) | 0.856 |
| Hispanic ethnicity, no. (%)b | 7 (8.4) | 2 (3.9) | 0.311 |
| Health Plan type, no. (%)b | |||
| Commercial | 3 (3.6) | 5 (9.8) | 0.088 |
| Deductible | 13 (15.7) | 17 (33.3) | |
| Medicaid | 3 (3.6) | 2 (3.9) | |
| Medicare | 52 (62.7) | 22 (43.1) | |
| ACA marketplace/exchange | 5 (6.0) | 3 (5.9) | |
| Uninsured | 7 (8.4) | 2 (3.9) | |
| Annual out-of-pocket expenses, US dollars | |||
| Health Plan maximum out-of-pocket (individual), mean (SD)d | 3206 (1485) | 3688(1885) | 0.129 |
| Months of Health Plan enrollment, mean (SD) | 159.6 (168.6) | 122.0 (116.4) | 0.164 |
| Census-based socioeconomic measures, %e | |||
| Annual household income < $50,000 | 47.9 | 51.7 | 0.216 |
| Married | 49.8 | 57.1 | 0.003 |
| Did not complete high school | 10.4 | 12.4 | 0.182 |
| Clinical | |||
| BMI (kg/m2), mean (SD)f | 30.3 (8.4) | 34.6 (10.2) | 0.015 |
| Charlson Comorbidity Index, mean (SD)b | 1.52 (2.62) | 0.67 (1.44) | 0.070 |
| Tobacco user, no. (%)g | 12 (15.0) | 9 (17.6) | 0.687 |
All estimates are based on those participants who completed baseline surveys with valid nonmissing data.
Percentages are based on 83 responses in the intervention group
Percentages are based on 79 responses in the intervention group.
Mean Health Plan annual out-of-pocket maximum for an individual is based on 55 responses in the intervention group and 63 in the comparison group, who had cost-sharing requirements for each individual in their health plan.
Estimates for all Census-based measures represent the mean percentage of persons with the given characteristics in the census block groups across participants’ locations of residence.
Estimates are based on 76 responses in the intervention group and 45 in the comparison group.
Percentages are based on 80 responses in the intervention group.
ACA = Affordable Care Act; BMI = body mass index; SD = standard deviation.
Baseline Survey Results
Forty percent of intervention participants and 24% of comparison participants reported having 1 or more nonmedical social needs at baseline (p = 0.062; Table 2). Among those participants with 1 or more nonmedical social needs, the 3 most commonly reported needs among the intervention group were transportation (53%), housing (38%), and social activities (32%). For the comparison group, the most common needs were employment (33%), food (33%), and housing (33%).
Table 2.
Participant responses to baseline and follow-up survey items
| Item | Intervention (n = 85), no. (%) | Comparison (n = 51), no. (%) | p valuea |
|---|---|---|---|
| Baseline needs | |||
| ≥ 1 Nonmedical social/economic need | 34 (40.0) | 12 (24.0) | 0.062 |
| Type of nonmedical social/economic need reportedb | |||
| Clothing | 6 (17.7) | 2 (16.7) | > 0.999 |
| Employment | 6 (17.7) | 4 (33.3) | 0.416 |
| Food | 9 (26.5) | 4 (33.3) | 0.717 |
| Housing | 13 (38.2) | 4 (33.3) | 1.000 |
| Legal | 6 (17.7) | 3 (25.0) | 0.678 |
| Social activities/isolation | 11 (32.4) | 3 (25.0) | 0.729 |
| Transportation | 18 (52.9) | 2 (16.7) | 0.043 |
| Baseline survey responses | |||
| The costs of medical care are important to me when choosing which treatment I will get. | 34 (40.5) | 42 (84.0) | < 0.001 |
| I am comfortable asking questions about the costs of medical care with my doctor or KP staff member. | 34 (40.0) | 27 (52.9) | 0.212 |
| I know how much I will have to pay for my medical care at KP. | 25 (30.5) | 16 (32.0) | 0.849 |
| I know who to contact if I have a question or concern related to costs of my medical care. | 28 (34.2) | 22 (43.1) | 0.358 |
| In the last year, I have avoided or delayed getting medical care when I was sick because of cost. | 14 (17.1) | 22 (43.1) | 0.001 |
| I am satisfied with how KP assists me with my questions and concerns about costs related to my medical care. | 33 (40.2) | 23 (45.1) | 0.593 |
| I am very satisfied with the medical care I receive. | 40 (47.6) | 38 (74.5) | 0.002 |
| Follow-up survey responsesc | |||
| I feel comfortable asking questions and voicing concerns about my medical care. | 14 (100.0) | 9 (64.3) | 0.041 |
| I feel like my medical care team is good at listening carefully to what I have to say.d | 13 (92.9) | 9 (69.2) | 0.165 |
| My medical care team is good about explaining things in clear, understandable information.e | 12 (85.7) | 9 (64.3) | 0.385 |
| My medical care team helped me cope with any uncertainty or unknowns related to costs.f | 4 (30.8) | 3 (25.0) | > 0.999 |
| I got answers to my questions about costs.d | 8 (61.5) | 4 (30.8) | 0.238 |
| I know my share of the costs for medical care from KP that I am responsible for paying.g | 7 (58.3) | 4 (33.3) | 0.414 |
| I got the resources I needed to meet my cost concerns.g | 6 (50.0) | 5 (41.7) | > 0.999 |
| I got all of the medical care, tests, medications, or treatments that my doctor recommended.f | 9 (69.2) | 10 (83.3) | 0.645 |
| I am satisfied with how KP assists me with my questions and concerns about costs related to my medical care. | 8 (61.5) | 3 (25.0) | 0.111 |
| I am very satisfied with the medical care I receive.d | 14 (100.0) | 9 (69.2) | 0.041 |
p values are based on Fisher exact test, because of small expected cell size.
Percentages are based on those who reported having ≥ 1 nonmedical social need (34 intervention participants; 12 comparison participants) and categories not mutually exclusive.
Frequencies and percentages are based on those participants who completed both the baseline and follow-up surveys and who provided valid, nonmissing responses to each survey item and who responded “agree” or “strongly agree.”
Percentages are based on 13 responses in the comparison group.
Percentages are based on 14 responses in the comparison group.
Percentages are based on 13 responses in the intervention group and 12 responses in the comparison group.
Percentages are based on 12 responses in the intervention group and 12 responses in the comparison group.
KP = Kaiser Permanente.
Among the intervention participants, at baseline, 41% reported that costs of medical care were important when choosing treatment and 41% reported that they were comfortable asking questions about the costs of medical care. These results are compared with 84% (p < 0.001) and 53% (p = 0.212) of comparison participants, respectively (Table 2). Seventeen percent of intervention participants and 43% of comparison participants reported that they have avoided or delayed medical care when sick because of cost during the previous year (p = 0.001, Table 2).
Follow-up Survey Results
Fourteen intervention participants and 18 comparison participants completed the follow-up survey. This resulted in 30-day follow-up response rates of 16.5% for the intervention group and 35.2% for the comparison group. Among intervention participants, 93% reported that their medical care team was “good at listening carefully to what I have to say” and 31% reported that their medical care team “helped me cope with any uncertainty or unknowns related to costs,” compared with 69% and 25% of comparison participants, respectively. Sixty-one percent of intervention participants and 31% of comparison participants reported getting answers to their questions about medical care costs. A greater percentage of intervention (62%) than comparison (25%) participants reported satisfaction with assistance answering questions and concerns about costs related to their medical care.
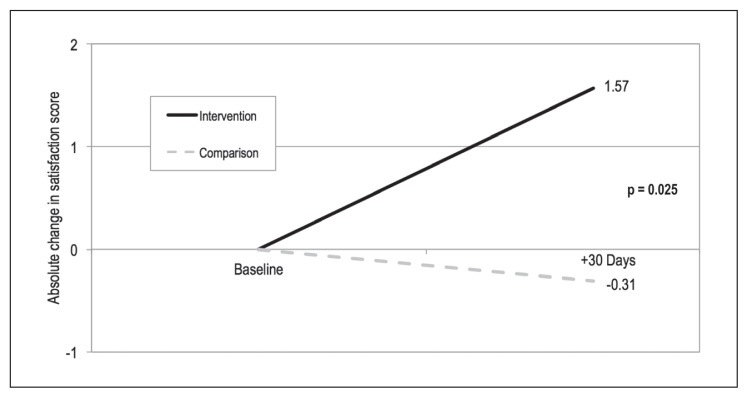
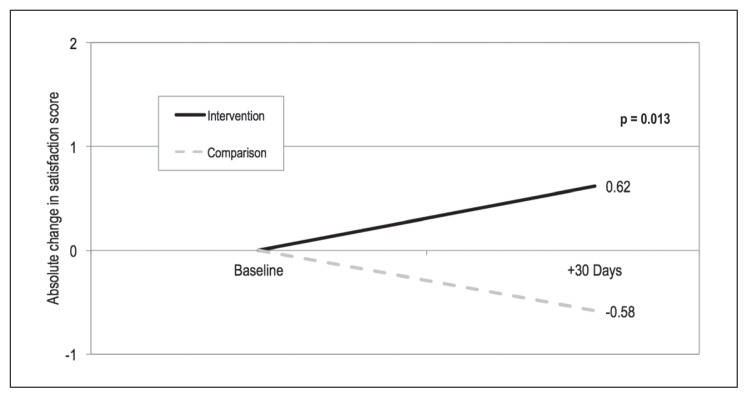
Intervention participants had significantly greater improvements in both satisfaction with their medical care (Figure 1, p = 0.025) and satisfaction with cost assistance (Figure 2, p = 0.013) at 30-day follow-up, compared with comparison participants, after we controlled for baseline responses (Table 3).
Figure 1.
Change in participant self-reported satisfaction with medical care between baseline and 30-day follow-up.a
a Estimates are based on participants with valid, nonmissing responses to the survey item, “I am very satisfied with the medical care I receive” on both the baseline and follow-up surveys, presented on a 5-point Likert scale: 1, “strongly disagree”; 2, “disagree”; 3, “neutral”; 4, “agree”; and 5, “strongly agree.” Ordinary least squares regression was used to measure change in member-reported satisfaction from baseline to 30-day follow-up, controlling for baseline values; p value is test of difference in change in satisfaction between groups.
Figure 2.
Change in participant self-reported satisfaction with assistance with cost concerns between baseline and 30-day follow-up.a
a Estimates are based on participants with valid, nonmissing responses to the survey item, “I am satisfied with how Kaiser Permanente assists me with my questions and concerns about costs related to my medical care” on both the baseline and follow-up surveys, presented on a 5-point Likert scale: 1, “strongly disagree”; 2, “disagree”; 3, “neutral”; 4, “agree”; and 5, “strongly agree.” Ordinary least squares regression was used to measure change in member-reported satisfaction from baseline to 30-day follow-up, controlling for baseline values; p value is test of difference in change in satisfaction between groups.
Table 3.
Baseline and follow-up satisfaction scores, by groupa
| Survey item | Intervention (n = 14) | Comparison (n = 13) | p valueb | ||||
|---|---|---|---|---|---|---|---|
| Baseline score | 30-day follow-up score | Change | Baseline score | 30-day follow-up score | Change | ||
| Satisfaction with medical carec | 2.93 (1.33) | 4.50 (0.52) | 1.57 (1.51) | 4.15 (1.07) | 3.85 (1.28) | −0.31 (0.63) | 0.025 |
| Satisfaction with cost assistanced | 3.15 (1.14) | 3.77 (0.93) | 0.62 (1.76) | 3.33 (1.23) | 2.75 (0.97) | −0.58 (0.90) | 0.013 |
Estimates are based on participants with valid, nonmissing data to each survey item on both the baseline and follow-up surveys, with all survey items presented on a 5-point Likert scale: 1, “strongly disagree”; 2, “disagree”; 3, “neutral”; 4, “agree”; and 5, “strongly agree.” Estimated are presented as mean satisfaction scores (standard deviation).
Ordinary least squares regression was used to measure change in member-reported satisfaction from baseline to 30-day follow-up, controlling for baseline values; p value is test of difference in change in satisfaction between groups.
Based on responses to survey item, “I am very satisfied with the medical care I receive.”
Based on responses to survey item, “I am satisfied with how KP assists me with my questions and concerns about costs related to my medical care.”
KP = Kaiser Permanente.
Physician Survey Results
Eleven of 70 physicians completed the survey (response rate of 16%). All 11 agreed that cost influences their patients’ decisions about medical care (Table 4). More than 80% of the physician respondents reported that they were comfortable discussing costs of medical care/treatment and that they engage in these cost-of-care discussions with their patients. Ninety-one percent of physician respondents reported that physicians have a responsibility to consider how medical care has an impact on their patients’ financial well-being, although only 18% of physicians reported having a sense of their patients’ financial well-being.
Table 4.
Results of physician surveya
| Survey Item | No. (%) |
|---|---|
| Medical care costs, no. of responsesb | 11 |
| Costs influence my patients’ decisions about medical care/treatment. | 11 (100.0) |
| I am comfortable discussing costs of medical care/treatment with patients. | 9 (81.8) |
| I discuss the costs of medical care/treatment with my patients. | 9 (81.8) |
| When patients ask about costs of medical care/treatment, I refer them to another staff member such as a financial counselor or billing representative. | 10 (90.9) |
| Patient financial well-being, no. of responsesb | 11 |
| It is important for my patients to understand the cost of their medical care/treatments. | 11 (100.0) |
| It is important to be explicit with patients about the financial consequences of their medical care/treatment options. | 11 (100.0) |
| Physicians have a responsibility to consider the impact that medical care/treatment decisions may have on their patients’ financial well-being. | 10 (90.9) |
| I have a sense of my patients’ financial well-being. | 2 (18.2) |
| Satisfaction with financial navigator, no. of responsesc | 4 |
| Satisfied with financial navigator’s overall responsivenessd | 3 (75) |
| Satisfied with financial navigator’s awareness of appropriate resourcesd | 2 (50) |
| Satisfied with financial navigator’s timeliness in coordination of cared | 3 (75) |
| The financial navigator was helpful providing information to meet the needs of my patient.b | 3 (75) |
| The financial navigator worked with me to address patient concerns.b | 3 (75) |
| I would recommend the financial navigator to other patients in our health care system.b | 3 (75) |
| I value financial navigation services as part of our health care system.b | 3 (75) |
Frequencies and percentages are based on those participants who provided valid, nonmissing responses to each survey item.
Responses are based on participants who reported to “agree” or “strongly agree” on survey item.
Survey items on “Satisfaction with financial navigator” were asked of physicians at the intervention clinic only. Among the 6 intervention clinic physicians who responded to the survey, 4 reported to have worked with the financial navigator; accordingly, the satisfaction with financial navigator items are based on the responses of these 4 physicians.
Responses are based on participants who reported being “satisfied” or “very satisfied” on survey item.
We asked about satisfaction with the FN only at the intervention clinic. Because the FN intervention was conducted at this clinic only, 6 of the 11 physicians who completed the survey were from the intervention clinic. Of these 6 physicians, 4 had worked with the FN during the intervention period. Among these 4 physicians, 75% were satisfied with both the FN’s overall responsiveness and timeliness in coordination of care. Fifty percent of respondents were satisfied with the FN’s awareness of appropriate resources. Additionally, physicians reported that the FN was helpful in providing information to meet the needs of their patients (75%), that the FN worked with them to address their patients’ concerns (75%), that they would recommend the FN to other patients in the health care system (75%), and that they value financial navigation services as part of the health care system (75%).
DISCUSSION
Our findings underscore the impact of a novel FN pilot intervention to address patients’ needs and concerns surrounding medical care costs in a real-world health care delivery setting. Participants who received the FN intervention had greater improvements in satisfaction with their medical care and satisfaction with cost assistance at 30-day follow-up than did comparison participants. Furthermore, although we found that most physicians agreed about the importance of discussing the costs of care and knowing the financial implications of medical care costs on their patients, very few knew about their patients’ financial well-being. Importantly, physicians valued financial navigation services as part of the health care system. This is important because as the number of Americans facing higher out-of-pocket health care costs and having troubles paying their medical expenses grows,19,20 the demand for health care systems to identify and address patients’ needs and concerns related to their medical care costs will rise.
Although health insurance is designed to protect individuals from high or unexpected medical care expenses, it is not a guaranteed shield from medical-related financial hardship. Among US households with medical bill problems, about 62% had health insurance and 34% were uninsured. For most of these individuals (66%), either a 1-time expense or short-term medical expense (eg, accident or hospital stay) led to financial hardship.21 Unexpected medical care expenses can present a substantial financial shock, because approximately 76% of Americans with medical bill problems owed amounts of $1000 or more, including 31% who owed in excess of $5000.21 This is especially troubling given that nearly half of Americans report that they would have difficulty paying an unexpected medical bill of $500.4 It is not surprising, then, that nearly 1 in every 4 US adults is paying off medical debt over time22 and worries about not being able to afford health care.4
The importance of addressing this phenomenon is 2-fold. First, individuals who experience medically related financial hardship may delay or forgo necessary medical care,5,23–28 which could lead to poor downstream health outcomes. Approximately 1 in every 10 US adults reports delaying or forgoing medical care because of cost.29 Prior research indicates that individuals may change their patterns of prescription drug use for financial reasons, such as skip medication doses, take less medication, or delay filling a prescription.5 Consequently, individuals who delay or forgo care are more likely to report worse health and may be at greater risk of disease progression24 and premature death.30 Second, given that decisions about medical care occur within the socioeconomic context alongside everyday household expenses and family obligations,31 individuals may be forced to make trade-offs between meeting basic social and economic needs and health needs.32 As shown in our findings, individuals with concerns about medical care costs also reported having other basic, nonmedical social and economic needs. These needs included food, housing, employment, and transportation. Accordingly, as families struggle to pay medical care costs, decisions between necessary care and care they can afford could lead to other unmet basic needs and exacerbate health disparities.
We found an apparent disconnect between physicians’ beliefs about the importance of medical care costs in the delivery of medical care and their understanding of individual patients’ financial well-being. This could be caused by many factors. First, the time available to discuss the complex topic of financial well-being during a routine office encounter is limited by the demands of immediate needs and meeting Health Plan priorities in terms of care delivery and performance metrics.33 Second, patients may not be willing to fully disclose financial hardship because of trust, pride, or embarrassment.34–37 Third, evaluating a person’s financial well-being may be difficult. It’s one thing to be able to balance a checkbook; it’s another to be able to absorb an unexpected $10,000 expense. Fourth, physicians may be uncomfortable asking about finances. Not only is it outside their formal training, the subject is still a little taboo if the patients don’t bring it up themselves.34 Fifth, the physician may have little idea of the patient burden of the service (complexity of plans/benefits and accumulated expenses contributing to maximum out-of-pocket expenses).33,34 Last, physicians may not believe that it is their responsibility to address financial hardship and other nonmedical social needs.38 Nevertheless, understanding patients’ financial well-being by engaging in costs-of-care conversations is critical to reducing patient financial hardship38 and may help reduce financial distress33 and improve medical decision making.39
The development of this delivery system pilot intervention was driven by the goals of mitigating medically related financial hardship and reducing cost barriers to access among patients in both primary and specialty care settings. The FN intervention focused on enhancing existing resources in the health care system. The FNs’ training included medical care cost assistance resources, cost estimation tools, and health insurance benefits. These trainings sought to improve the overall knowledge and skill set required to work with, educate, and address a patient’s medical care costs needs and concerns. This is in addition to the standard navigation support of interacting with patients to identify, understand, and meet their nonmedical social or economic needs. Building new referral capabilities in the EHR and having the FN connect with key clinical and operational staff led to novel operational workflows to connect with patients and coordinate care between health care staff. Indeed, intervention clinic physicians reported that they valued the FN as part of the health care system.
Other Financial Navigation Pilot Intervention Work
Shankaran and colleagues40 recently reported on an oncology-specific financial navigation pilot program designed to help improve patient knowledge about treatment costs, provide financial counseling, and help manage out-of-pocket expenses. They used an intervention-group-only design. Patients at a single institution who were within 6 months of completing treatment of nonmetastatic cancer were eligible to receive a financial education course, followed by monthly assistance from 2 external organizations: Consumer Education and Training Services (CENTS) and Patient Advocate Foundation (PAF). The researchers found that patients most often needed assistance with budgeting, retirement planning, and medical bill questions, as well as processing applications for appropriate insurance coverage, basic social and economic needs (eg, housing, transportation), and disability benefits.40 Approximately 83% of participants reported high satisfaction with the financial navigation program. Furthermore, they found no significant decreases in the proportion of participants who had debt accrual between baseline (55%) and follow-up (57%), or in self-reported financial burden (45% at baseline and 43% at follow-up).
Collectively, findings from Shankaran et al40 and those based on the KPNW FN pilot underscore the importance of interventions to address medically related financial hardship in the care setting. Efforts to reduce financial hardship and limit the impact on medical care may need to consider specific issues in the development of future interventions. First, a comprehensive understanding of medical care costs, health insurance benefits, and medical financial assistance programs is essential for educating patients about their out-of-pocket costs for impending medical care and coordinating the resources to manage the financial implications. Early education of patients about their out-of-pocket responsibilities for medical care may help them prepare for and take the steps necessary to manage their finances.23 Second, as noted by Shankaran et al,40 the intervention “must be provided in a manner that is acceptable, accessible, and minimally burdensome alongside clinical care.” Third, despite broad recognition about the importance of addressing social determinants of health such as financial hardship, physicians may have limited time to inquire about patient’s financial concerns, and others may not believe that this task is part of their responsibility.41 Accordingly, it is imperative to develop a health system culture that embraces the importance of identifying patients’ financial concerns and financial capability as part of routine care, as well as the commitment to addressing patients’ financial needs, by establishing workflows that incorporate a health care team-based approach (eg, physicians, nurses, navigators, medical assistants, social workers) to engage in cost conversations and help identify financial resources (eg, financial assistance programs or prescription copay assistance programs). Finally, interventions aimed at addressing medically related financial hardship may also need to incorporate strategies for addressing other unmet, nonmedical basic social needs. This is especially salient because participants in both pilots required assistance with both types of needs.
Strengths and Limitations
Despite the strengths of findings from a novel FN pilot, there are several limitations that should be acknowledged. First, the FN pilot was a delivery system intervention, which was developed and conducted at a single, large integrated health care system that serves a predominately white, insured population. Accordingly, findings may be most generalizable to similar delivery settings and patient populations. Second, we employed a nonequivalent comparison group design by recruiting an untreated control group of patients that was as similar to the intervention group as possible. This strategy included recruiting from a comparison clinic with similar structural factors (eg, the comparison clinic housed Primary Care, Rheumatology, and Ophthalmology Departments on the same campus, just as the intervention clinic did) during the same timeframe. Comparison group participants were younger, more likely to have a commercial Health Plan and a health plan with a higher out-of-pocket maximum, and less likely to have Medicare than were intervention group participants. Because many of these factors are associated with risk of financial hardship, these differences may partly account for observed differences between groups in concerns about cost of medical care, delaying care because of cost, and having certain other social needs (ie, transportation).4,42 Although the findings are subject to biases inherent to nonrandomized study designs, administration of a preintervention baseline survey to both groups enabled us to partly account for observed differences between groups in our analyses. Third, comparison participants were identified on the basis of having made a recent visit to the Primary Care, Rheumatology, or Ophthalmology Department and were recruited using email-based outreach and an online survey.
Given the meager response rates for both the baseline and follow-up surveys, our findings are subject to response bias. Our use of the EHR as the primary mode to recruit and administer evaluation surveys may have limited participation.43 Future efforts to collect patient-reported outcomes in a clinical setting may need to use multiple modes of contact to improve response rates.44 These are the first reported findings on the impact of a novel FN pilot intervention conducted in a real-world clinical setting. Pilot studies are not intended to provide a meaningful effect size estimate because of the imprecision inherent in the data from small sample size, although they are the critical initial step in exploring a novel intervention, to inform feasibility of an approach.45
Another limitation of our study was the relatively small sample size, which limited our statistical power to detect differences between intervention and comparison groups. Importantly, though, the pilot intervention was conducted over a 3-month timeframe, which limited the recruitment and follow-up attempts. As such, our study reflects the challenges evaluating delivery system interventions that are designed to occur within a short timeframe, have minimal interruption to clinical flow, use limited resources, and prevent unintended consequences to patients.46
CONCLUSION
Health systems, physicians, and patients agree that medical care costs are an important component of health care. Despite this importance, however, medical care costs are rarely addressed explicitly in the delivery setting. Our evaluation demonstrates the promise of a novel FN intervention designed to address concerns and needs about medical care costs and to inform how financial navigation may be systematically delivered to address cost needs, improve patient satisfaction, and ultimately improve health outcomes. As US health care costs increase along with cost sharing, patients may increasingly be at financial risk. Interventions that identify individuals who have the greatest need for assistance with financial aspects of medical care may reduce the likelihood of financial hardship and improve health equity.
Acknowledgment
Kathleen Louden, ELS, of Louden Health Communications provided editorial assistance.
Footnotes
Disclosure Statement
Dr Banegas has received a research grant from AstraZeneca (paid to the institution) for work outside of the scope of this project. The other author(s) have no conflicts of interest to disclose.
References
- 1.Cuckler GA, Sisko AM, Poisal JA, et al. National health expenditure projections, 2017–26: Despite uncertainty, fundamentals primarily drive spending growth. Health Aff (Millwood) 2018 Mar;37(3):482–92. doi: 10.1377/hlthaff.2017.1655. [DOI] [PubMed] [Google Scholar]
- 2.Claxton G, Levitt L, Long M, Blumenkranz E. Increases in cost-sharing payments have far outpaced wage growth [Internet] Menlo Park, CA: Henry J Kaiser Family Foundation; 2017. Oct 4, [cited 2018 Oct 22]. Available from: http://pnhp.org/blog/2017/10/10/cost-sharing-payments-have-far-outpaced-wage-growth/ [Google Scholar]
- 3.Claxton G, Rae M, Long M, Damico A, Foster G, Whitmore H. Employer health benefits: 2017 annual survey [Internet] Menlo Park, CA: Henry J Kaiser Family Foundation; 2017. Sep 19, [cited 2018 Oct 22]. Available from: http://files.kff.org/attachment/Report-Employer-Health-Benefits-Annual-Survey-2017. [Google Scholar]
- 4.DiJulio B, Kirzinger A, Wu B, Brodie M. Data note: Americans’ challenges with health care costs [Internet] Menlo Park, CA: Henry J Kaiser Family Foundation; 2017. Mar 2, [cited 2018 Oct 22]. Available from: www.kff.org/health-costs/poll-finding/data-note-americans-challenges-with-health-care-costs/ [Google Scholar]
- 5.Zheng Z, Han X, Guy GP, Jr, et al. Do cancer survivors change their prescription drug use for financial reasons? Findings from a nationally representative sample in the United States. Cancer. 2017 Apr 15;123(8):1453–63. doi: 10.1002/cncr.30560. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Booske BC, Athens JK, Kindig DA, Park H, Remington PL. Different perspectives for assigning weights to determinants of health [Internet] Madison, WI: University of Wisconsin, Population Health Institute; 2010. Feb, [cited 2018 Oct 23]. Available from: www.countyhealthrankings.org/sites/default/files/differentPerspectivesForAssigningWeightsToDeterminantsOfHealth.pdf. [Google Scholar]
- 7.Woolf SH, Braveman P. Where health disparities begin: The role of social and economic determinants—and why current policies may make matters worse. Health Aff (Millwood) 2011 Oct;30(10):1852–9. doi: 10.1377/hlthaff.2011.0685. . [DOI] [PubMed] [Google Scholar]
- 8.Krieger J, Higgins DL. Housing and health: Time again for public health action. Am J Public Health. 2002 May;92(5):758–68. doi: 10.2105/ajph.92.5.758. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mansfield C, Novick LF. Poverty and health: Focus on North Carolina. N C Med J. 2012 Sep-Oct;73(5):366–73. [PubMed] [Google Scholar]
- 10.American Society of Clinical Oncology. The state of cancer care in America, 2017: A report by the American Society of Clinical Oncology. J Oncol Pract. 2017 Apr;13(4):e353–94. doi: 10.1200/jop.2016.020743. . [DOI] [PubMed] [Google Scholar]
- 11.Altice CK, Banegas MP, Tucker-Seeley RD, Yabroff KR. Financial hardships experienced by cancer survivors: A systematic review. J Natl Cancer Inst. 2016 Oct 20;109(2):djw205. doi: 10.1093/jnci/djw205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zafar SY. Financial toxicity of cancer care: It’s time to intervene. J Natl Cancer Inst. 2015 Dec 11;108(5):djv370. doi: 10.1093/jnci/djv370. . [DOI] [PubMed] [Google Scholar]
- 13.Heiman HJ, Artiga S. Beyond health care: The role of social determinants in promoting health and health equity [Internet] Washington, DC: Henry J Kaiser Family Foundation; 2015. Nov, [cited 2018 Oct 23]. Available from: http://media.morehousetcc.org/RESEARCH_PROJECTS/HP/DELIVERABLES/KFF%20Brief%202015%20Beyond%20Health%20Care%20Role%20of%20Social%20Determinants.pdf. [Google Scholar]
- 14.Gottlieb L, Tobey R, Cantor J, Hessler D, Adler NE. Integrating social and medical data to improve population health: Opportunities and barriers. Health Aff (Millwood) 2016 Nov 1;35(11):2116–23. doi: 10.1377/hlthaff.2016.0723. . [DOI] [PubMed] [Google Scholar]
- 15.National Cancer Institute. Financial toxicity and cancer treatment (PDQ®)—health professional version [Internet] Bethesda, MD: National Institutes of Health; 2016. [cited 2016 Oct 24]. Available from: www.cancer.gov/about-cancer/managing-care/track-care-costs/financial-toxicity-hp-pdq. [Google Scholar]
- 16.Sarkar U, Piette JD, Gonzales R, et al. Preferences for self-management support: Findings from a survey of diabetes patients in safety-net health systems. Patient Educ Couns. 2008 Jan;70(1):102–10. doi: 10.1016/j.pec.2007.09.008. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Garg A, Toy S, Tripodis Y, Silverstein M, Freeman E. Addressing social determinants of health at well child care visits: A cluster RCT. Pediatrics. 2015 Feb;135(2):e296–304. doi: 10.1542/peds.2014-2888. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fiscella K, Tancredi D, Franks P. Adding socioeconomic status to Framingham scoring to reduce disparities in coronary risk assessment. Am Heart J. 2009 Jun;157(6):988–94. doi: 10.1016/j.ahj.2009.03.019. . [DOI] [PubMed] [Google Scholar]
- 19.Cohen RA, Martinez ME, Zammitti EP. Health insurance coverage: Early release of estimates from the National Health Interview Survey, January–March 2017 [Internet] Hyattsville, MD: National Center for Health Statistics; 2017. Aug, [cited 2018 Oct 23]. Available from: www.cdc.gov/nchs/data/nhis/earlyrelease/insur201708.pdf. [Google Scholar]
- 20.Claxton G, Rae M, Long M, Damico A, Whitmore H, Foster G. Health benefits in 2017: Stable coverage, workers faced considerable variation in costs. Health Aff (Millwood) 2017 Oct 1;36(10):1838–47. doi: 10.1377/hlthaff.2017.0919. . [DOI] [PubMed] [Google Scholar]
- 21.Hamel L, Norton M, Pollitz K, Levitt L, Claxton G, Brodie M. The burden of medical debt: Results from the Kaiser Family Foundation/New York Times Medical Bills Survey [Internet] Menlo Park, CA: Kaiser Family Foundation; 2016. Jan 5, [cited 2018 Oct 23]. Available from: www.kff.org/health-costs/report/the-burden-of-medical-debt-results-from-the-kaiser-family-foundationnew-york-times-medical-bills-survey/ [Google Scholar]
- 22.Collins SR, Gunja MZ, Doty MM, Beutel S. How the Affordable Care Act has improved Americans’ ability to buy health insurance on their own [Internet] New York, NY: The Commonwealth Fund; 2017. Feb 1, [cited 2018 Oct 23]. Available from: www.commonwealthfund.org/publications/issue-briefs/2017/feb/how-affordable-care-act-has-improved-americans-ability-buy. [PubMed] [Google Scholar]
- 23.Banegas MP, Dickerson JF, Kent EE, et al. Exploring barriers to the receipt of necessary medical care among cancer survivors under age 65 years. J Cancer Surviv. 2018 Feb;12(1):28–37. doi: 10.1007/s11764-017-0640-1. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dusetzina SB, Winn AN, Abel GA, Huskamp HA, Keating NL. Cost sharing and adherence to tyrosine kinase inhibitors for patients with chronic myeloid leukemia. J Clin Oncol. 2014 Feb 1;32(4):306–11. doi: 10.1200/jco.2013.52.9123. . [DOI] [PubMed] [Google Scholar]
- 25.Goldman DP, Jena AB, Lakdawalla DN, Malin JL, Malkin JD, Sun E. The value of specialty oncology drugs. Health Serv Res. 2010 Feb;45(1):115–32. doi: 10.1111/j.1475-6773.2009.01059.x. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kaisaeng N, Harpe SE, Carroll NV. Out-of-pocket costs and oral cancer medication discontinuation in the elderly. J Manag Care Spec Pharm. 2014 Jul;20(7):669–75. doi: 10.18553/jmcp.2014.20.7.669. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Streeter SB, Schwartzberg L, Husain N, Johnsrud M. Patient and plan characteristics affecting abandonment of oral oncolytic prescriptions. J Oncol Pract. 2011 May;7(3 Suppl):46s–51s. doi: 10.1200/jop.2011.000316. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Guy GP, Jr, Yabroff KR, Ekwueme DU, et al. Healthcare expenditure burden among non-elderly cancer survivors, 2008–2012. Am J Prev Med. 2015 Dec;49(6 Suppl 5):S489–97. doi: 10.1016/j.amepre.2015.09.002. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cox C, Sawyer B. Despite lower rates of access barriers for some groups, health costs remain a concern for many Americans [Internet] Washington, DC: Kaiser Family Foundation; 2016. Nov 30, [cited 2018 Oct 23]. Available from: www.healthsystemtracker.org/brief/despite-lower-rates-of-access-barriers-for-some-groups-health-costs-remain-a-concern-for-many-americans/ [Google Scholar]
- 30.Hsu J, Price M, Huang J, et al. Unintended consequences of caps on Medicare drug benefits. N Engl J Med. 2006 Jun 1;354(22):2349–59. doi: 10.1056/nejmsa054436. . [DOI] [PubMed] [Google Scholar]
- 31.Tucker-Seeley RD, Yabroff KR. Minimizing the “financial toxicity” associated with cancer care: Advancing the research agenda. J Natl Cancer Inst. 2016 Dec 11;108(5):djv410. doi: 10.1093/jnci/djv410. [DOI] [PubMed] [Google Scholar]
- 32.Artiga S, Tolbert J, Ubri P. Snapshots from Medicaid enrollees [Internet] Washington, DC: The Henry J Kaiser Family Foundation; 2017. Nov 9, How do health care costs fit into family budgets? [cited 2018 Oct 23]. Available from: www.kff.org/medicaid/issue-brief/how-do-health-care-costs-fit-into-family-budgets-snapshots-from-medicaid-enrollees/ [Google Scholar]
- 33.Ubel PA, Abernethy AP, Zafar SY. Full disclosure—out-of-pocket costs as side effects. N Engl J Med. 2013 Oct 17;369(16):1484–6. doi: 10.1056/nejmp1306826. . [DOI] [PubMed] [Google Scholar]
- 34.Hardee JT, Platt FW, Kasper IK. Discussing health care costs with patients: An opportunity for empathic communication. J Gen Intern Med. 2005 Jul;20(7):666–9. doi: 10.1111/j.1525-1497.2005.0125.x. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bestvina CM, Zullig LL, Rushing C, et al. Patient-oncologist cost communication, financial distress, and medication adherence. J Oncol Pract. 2014 May;10(3):162–7. doi: 10.1200/jop.2014.001406. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Irwin B, Kimmick G, Altomare I, et al. Patient experience and attitudes toward addressing the cost of breast cancer care [supplemental data available online] Oncologist. 2014 Nov;19(11):1135–40. doi: 10.1634/theoncologist.2014-0117. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zafar SY, Chino F, Ubel PA, et al. The utility of cost discussions between patients with cancer and oncologists. Am J Manag Care. 2015 Sep;21(9):607–15. [PubMed] [Google Scholar]
- 38.Henrikson NB, Chang E, Ulrich K, King D, Anderson ML. Communication with physicians about health care costs: Survey of an insured population. Perm J. 2017;21:16–070. doi: 10.7812/TPP/16.070. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bullock AJ, Hofstatter EW, Yushak ML, Buss MK. Understanding patients’ attitudes toward communication about the cost of cancer care. J Oncol Pract. 2012 Jul;8(4):e50–8. doi: 10.1200/jco.2011.29.15_suppl.6065. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shankaran V, Leahy T, Steelquist J, et al. Pilot feasibility study of an oncology financial navigation program. J Oncol Pract. 2018 Feb;14(2):e122–9. doi: 10.1200/jop.2017.024927. . [DOI] [PubMed] [Google Scholar]
- 41.Winfield L, DeSalvo K, Muhlestein D. 2017 Physician survey on social determinants of health [Internet] Salt Lake City, UT: Leavitt Partners LLC; 2018. May 9, Social determinants matter, but who is responsible? [cited 2018 Oct 24]. Available from: https://leavittpartners.com/press/leavitt-partners-releases-social-determinants-matter-but-who-is-responsible-2017-physician-survey-on-social-determinants-of-health-white-paper/ [Google Scholar]
- 42.Yabroff KR, Dowling EC, Guy GP, Jr, et al. Financial hardship associated with cancer in the United States: Findings from a population-based sample of adult cancer survivors. J Clin Oncol. 2016 Jan 20;34(3):259–67. doi: 10.1200/jco.2015.62.0468. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fraser D, Christiansen BA, Adsit R, Baker TB, Fiore MC. Electronic health records as a tool for recruitment of participants’ clinical effectiveness research: Lessons learned from tobacco cessation. Transl Behav Med. 2013 Sep;3(3):244–52. doi: 10.1007/s13142-012-0143-6. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Feigelson HS, McMullen CK, Madrid S, et al. Optimizing patient-reported outcome and risk factor reporting from cancer survivors: A randomized trial of four different survey methods among colorectal cancer survivors. J Cancer Surviv. 2017 Jun;11(3):393–400. doi: 10.1007/s11764-017-0596-1. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Leon AC, Davis LL, Kraemer HC. The role and interpretation of pilot studies in clinical research. J Psychiatr Res. 2011 May;45(5):626–9. doi: 10.1016/j.jpsychires.2010.10.008. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Garg A, Boynton-Jarrett R, Dworkin PH. Avoiding the unintended consequences of screening for social determinants of health. JAMA. 2016 Aug 23–30;316(8):813–4. doi: 10.1001/jama.2016.9282. [DOI] [PubMed] [Google Scholar]