Abstract
Background:
The Religious Orders Study and Rush Memory and Aging Project are both ongoing longitudinal clinical-pathologic cohort studies of aging and Alzheimer’s disease (AD).
Objectives:
To summarize progress over the past five years and its implications for understanding neurodegenerative diseases.
Methods:
Participants in both studies are older adults who enroll without dementia and agree to detailed longitudinal clinical evaluations and organ donation. The last review summarized findings through the end of 2011. Here we summarize progress and study findings over the past five years, and discuss new directions for how these studies can inform on aging and AD in the future.
Results:
We summarize 1) findings on the relation of neurobiology to clinical AD; 2) neurobiologic pathways linking risk factors to clinical AD; 3) non-cognitive AD phenotypes including motor function and decision making; 4) the development of a novel drug discovery platform.
Conclusion:
Complexity at multiple levels needs to be understood and overcome to develop effective treatments and preventions for cognitive decline and AD dementia.
Keywords: Religious Orders Study, Rush Memory and Aging Project, Dementia, Alzheimer’s Disease, Cognitive Function, Epidemiology, Clinical-pathologic Study, cognitive decline, motor function, decision making, neuropathology, omics, drug discovery
INTRODUCTION
For more than a century, careful clinical characterization followed by examination of neural tissues after death has been an important approach for identifying the neuropathologic determinants of dementia [1, 2]. The vast majority of older adults studied in clinical-pathologic studies are recruited at tertiary care dementia centers [3, 4]. In the early 1990s, community-based cohort studies of aging and dementia started obtaining autopsies. This is important as autopsies from community participants differ from autopsies of individuals evaluated at dementia centers [5]. The first community-based studies were the Nun Study, the Honolulu Asia Aging Study (HAAS), and the Hisayama Study [6–8]. Participants in the Nun Study were over age 75 at entry, and all agreed to organ donation; however, it was not explicitly designed as a study of risk factors for incident AD dementia. Both HAAS and the Hisayama Study were population based studies of risk factors for AD dementia. Both added organ donation for the relatively small number that agreed. Later, other community-based studies in the USA and Europe started to obtain autopsies [9].
The Religious Orders Study (ROS) and Rush Memory and Aging Project (MAP) began in 1994 and 1997 respectively (together referred to as ROSMAP). They are both cohort studies of risk factors for cognitive decline and incident AD dementia, and other health outcomes. They share all essential attributes of analytic cohort studies, and both require an agreement for organ donation as a condition of study entry. The last review of these studies summarized findings through the end of 2011 [10, 11]. Here, we describe the current datasets, summarize progress and study findings with emphasis on results from 2012 through 2017, and contextualize the findings with the other advances in the field. As ROSMAP serves as a resource for the aging and dementia research community, we hope the review will orient potential users of the resource to the wealth of data and findings which can be leveraged for future studies.
MATERIALS
Participants
ROS started in 1994 and enrolls nuns priests and brothers from across the United States. MAP started in 1997 and enrolls lay persons from across northeastern Illinois. Evaluations are annual and all participants in both cohorts are organ donors. This includes brain, spinal cord, nerve and muscle for those autopsied at Rush (Illinois, southeastern Wisconsin, and northwestern Indiana), and brain only for those autopsied elsewhere (California, central Illinois, central Indiana, Iowa, Kentucky, Louisiana, Maryland, Minnesota, Missouri, New York, Ohio, Pennsylvania, Tennessee, Texas, Washington DC, central and western Wisconsin). All MAP and a few hundred ROS donate blood annually. A large common core of data is shared by both studies allowing efficient merging of data. The two studies support additional sub-studies that address a wide range of other aspects of aging. Many sub-studies are restricted to MAP as nearly all participants are within driving distance of Rush and it is easier for staff to assess them more frequently. The parent studies and sub-studies were all approved by an Institutional Review Board of Rush University Medical Center and all participants signed an informed consent, Anatomical Gift Act, and a repository consent to share data and biospecimens.
Through December 31, 2017, the studies enrolled 3,414 persons of whom 72.6% are female, 88.2% are non-Latino White, 6.3% are African American, 5.5% are Latino (including African American Latinos), and the remainder are other racial groups. Their mean age was 78.3 years and education 16.9 years, and blood was collected from 94.3%. There have been 1,232 cases of incident mild cognitive impairment (MCI) and 764 cases of incident dementia, and only 7.8% have withdrawn. There have been 1,717 deaths and 1,506 (87.7%) brain autopsies and 834 spinal cord, nerve, and muscle autopsies. Of those autopsied, 67.2% are female, 94.8% are non-Latino White, and the remainder were members of other racial groups. Their mean age was 89.1 years and mean education is 16.9 years. Of those autopsied, 31.0% were without cognitive impairment, 23.0% had MCI, 41.4% had AD dementia with or without another condition, and the remainder had another cause of dementia.
The layers of data now available (or currently being generated) in one or both cohorts are illustrated in Fig 1. These are documented in the Rush Alzheimer’s Disease Center Resource Sharing Hub (www.radc.rush.edu). The Hub also includes all information and links required to request data and biospecimens, including downloadable data use and material transfer agreements. The Hub automatically updates with on-going data collection and is actively expanded when new data is available for sharing.
Fig 1.
Multi-layered omics, neuropathologic, and clinical data in ROSMAP.
Potential risk factors
Both studies collect a wide range of exposure data that includes genomic, experiential, psychological, and medical risk factors [12–46]. This includes continuous daily recordings of physical activity with an omnidirectional accelerometer [47]. From these recordings quantitative metrics of physical activity, sleep and circadian rhythms are extracted [48]. We administer the Food Frequency Questionnaire [49]. Genome-wide data has been generated [50], and we recently generated whole genome sequencing.
Multi-level omics
Several additional layers of brain and blood molecular genomics were generated. Data generated from the dorsolateral prefrontal cortex, include DNA methylation, H3K9Ac, miRNA, and RNAseq. We are currently generating 5hC methylation, another histone mark, proteomics and metabolomics from the same region, plus RNAseq and DNA methylation from other brain regions. Proteomic and metabolomic data is also being generated on blood, DNA methylation from CD4+ lymphocytes, and RNAseq from monocytes. Finally, we are in the process of establishing 50 iPSC lines from participants.
Neuropathologic and neurobiologic traits
A wide range of neuropathologic traits are generated. These include quantitative measures of AD pathology by histochemistry and immunohistochemistry, and Braak Stage, NIA-Reagan, and NIA-AA pathologic criteria for AD [51–55]. Other measures include macro- and microscopic infarcts, athero- and arteriolar-sclerosis, amyloid angiopathy, Lewy bodies, TDP-43, hippocampal sclerosis, and (on subsets) activated microglia and white matter pallor. Arteriolar sclerosis as well as AD pathology and Lewy bodies are also recorded in the spinal cord [56–61]. This is complemented by measures of resilience including presynaptic proteins and neuron density [62]. We also are generating data on targeted proteomics.
Structural and functional neuroimaging
Ante-mortem 3D MPRAGE, diffusion weighted imaging, 2D fast spin echo, 2D FLAIR, QSM, and resting state functional MRI is done on a subset of participants [63]. We also perform ex vivo imaging in many cases both fresh and fixed [64, 65].
Quantitative clinical phenotypes
Twenty-one cognitive performance tests with 19 in common, 17 of which are summarized as measures of global cognition, and scores of episodic memory, semantic memory, working memory, perceptual speed, and visuospatial ability [15, 66–68]. Parkinsonian signs summarized as a continuous measure of parkinsonism, and domains of gait, bradykinesia, rigidity, and resting and/or postural tremor, and a categorical measure of parkinsonism [69–72]. Other motor performance tests include quantitative measures of upper and lower limb performance [42, 43, 73–77]. Since 2012, annual gait testing now includes a body sensor with a triaxial accelerometer with three gyroscopes [78–82].
We also have studies of behavioral economics, decision making, and related behaviors in MAP. This includes measures of risk aversion and temporal discounting, health and financial decision making, health and financial literacy, and susceptibility to scams and fraud victimization, and related psychological measures (e.g., purpose in life) [40, 83–86].
Syndromic clinical phenotypes
Clinical diagnosis of dementia, especially AD dementia, and MCI are documented [87, 88]. We also make diagnoses of stroke and vascular cognitive impairment, Parkinson’s disease, and depression [89–91]. Other diagnoses are made by history and examination of medications. Diagnoses are rendered annually and a final diagnosis prior to death is generated after review of all data blinded to neuropathology. For some participants, we have linkages to Medicare data.
RESULTS
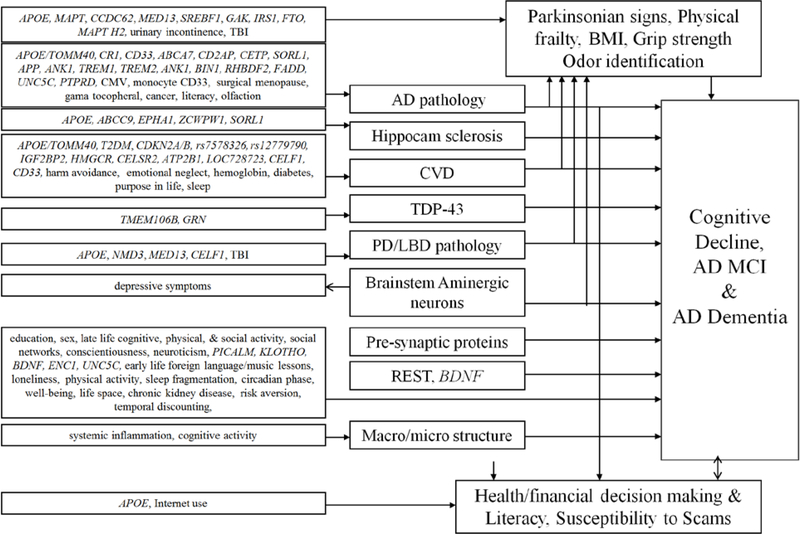
Several themes have dominated our work over the past six years. One is the relation of neuropathologic and resilience indices to cognitive decline, MCI, and AD dementia. Second are the neurobiologic pathways linking risk factors to cognitive decline, MCI and AD dementia. A summary of these associations are illustrated in Fig 2. Third is a comparable portfolio centering on motor structure and function including parkinsonism, and a fourth on behavioral- neuro-economics and decision making. Finally, we describe our emerging novel drug discovery pipeline.
Fig 2.
Neurobiologic pathways linking risk factors to AD clinical phenotypes.
Due to the large number of annual assessments over so many years, we calculated the attributable risk of death due to incident AD dementia [92]. Time from incident AD dementia to death was less than 4 years with a hazard ratio of more than 4. Upweighted to the US population resulted in an estimated 500,000 deaths attributable to incident AD dementia in 2010 putting it on par with cancer and heart disease.
Relation of neuropathology and resilience indices to cognitive decline, MCI, and AD dementia
We demonstrated that mixed pathologies were the most common cause of AD dementia with AD pathology including amyloid angiopathy, several indices of cerebrovascular disease, including macro- and micro-infarcts, atherosclerosis, arteriolarsclerosis, Lewy body disease, TDP-43 and hippocampal sclerosis all having additive effects on the odds of AD dementia [93–102]. Some pathologies, such as atrophy and white matter changes, were assessed with in vivo or ex vivo imaging and were also separately related to dementia [103–110].
A dozen years ago we first reported that pathologic AD was present in about a third of older persons without dementia or MCI and that it was related to episodic memory [55]. In a follow-up we showed that neocortical β-amyloid, mesial temporal PHFtau tangles, and macroscopic infarctions were all related to episodic memory and β-amyloid related to working memory in persons without cognitive impairment [111]. We recently extended this work showing that TDP and hippocampal sclerosis are associated with cognitive impairment in persons without pathologic AD, similar to earlier findings with AD pathology, Lewy bodies, and infarcts [101].
An important feature of the study design, the repeated measures of cognition, permits one to examine the relation of pathologies to the trajectory of cognitive decline over up to a quarter century prior to death. Using several approaches including latent variable models, change point models, Markov chain models, and sigmoidal models we find that the effects of neuropathology on cognitive decline emerge many years prior to death [112–123]. These data further illustrate the continuum of the clinical AD phenotype that seamlessly evolves from normality, to minimal then mild cognitive impairment, and eventually to dementia. Further, they show that effects of pathology, including hippocampal volume, measured at death are related to cognitive changes many years prior to death, including in persons who died without dementia [120, 124 ].
Using a Markov chain model we illustrated the effects of multiple pathologies on the “horserace” between dementia and death [121]. Without any pathology there is nearly a 20% likelihood of cognitive impairment prior to death. By contrast, with AD, infarcts, and Lewy body disease, the risk triples to nearly 60%. We recently reported nearly 250 different unique combinations of pathologies accounting for cognitive decline in just over 1000 persons [122]. The most common, pathologic AD alone was less than 10%. Nearly 100 people had a combination that was not present in any other person. Further, the magnitude of the effect of each pathology on cognitive decline varied widely depending on the specific combination present.
Interestingly, we found that when we link common neuropathologies to cognitive decline, we explain less than half of the person specific differences in slopes [124, 125]. This is likely results from several factors. First, neuropathologies are neither measured perfectly nor completely, and downstream effects of measured pathologies are only captured on a subset of participants [105–108]. In addition, we are not measuring all of the brain pathologies known to be associated with the named diseases. For example we only have soluble pathologies on a small subset of participants [126–131]. Further, it is likely that new associated pathologies will be discovered in the future.
However, another important factor is neural reserve or resilience. We define resilience as a continuous [latent] variable defined as cognitive decline not explained by extant pathologies, i.e., residual cognitive decline [132]. When viewed in this way, every person has some resilience. However, one can be more or less resilient relative to the average person and therefor have a slower or faster rate of residual cognitive decline. We found several genomic and neurobiologic indices of resilience were associated with a slower rate of decline including presynaptic proteins, neuron density, and BDNF expression [122, 132–137]. We are also finding genes associated with a faster rate of cognitive decline [138].
Neurobiologic pathways linking risk factor to cognitive decline, MCI and AD dementia
We first examine change in cognition and show that cognitive decline in African Americans and Latinos in our cohorts was similar to whites [139–141]. We also conducted a series of change point models in persons who developed AD dementia and showed that change in cognition began years prior to onset of AD dementia, and among persons who developed MCI, change in cognition began long before diagnosis [142]. Next, we summarize four sets of risk factor associations.
Genomic risk factors
We examined the effects of the TOMM40 haplotypes to cognitive decline, incident AD, and neuropathology [143–146]. Due to its strong linkage disequilibrium with APOE we restricted one analysis of Caucasians to persons with APOE ε3/3 genotype and found that both ‘523-L and ‘523-S/S S/S poly-T genotype were related to faster cognitive decline, especially episodic memory, a finding similar to APOE4 [146]. In another study we examined racial differences and found that among Caucasians nearly all APOE4 carriers had ‘523-L whereas less than half of the African Americans had this haplotype [144]. In African Americans, the ε4-’523-L haplotype had stronger effect on risk of AD dementia than other APOE4-’523 haplotypes. This contrasts with the effects of APOE4 among African Americans which is much weaker than in Caucasians [147]. Interestingly, the effect of the ‘523-L poly-T genotype was attenuated and no-longer significant controlling for AD and other neuropathologies, again similar to what we found for APOE4 [148–151]. By contrast, ‘523-S/S S/S association with unchanged in analyses with neuropathologies suggesting that the two haplotypes work via different pathologic mechanisms.
We also examined in more detail are several single nucleotide polymorphisms (SNP) that emerged from prior genome wide association studies (GWAS) [152]. We found that CR1, SORL1, and CD33 were all associated with cognitive decline, AD pathology and amyloid angiopathy [153–159]. CD33 also modulated TREM2 in monocytes [156]. When examining all genomic variants from prior GWAS we found some were associated with AD pathology but as a result of mixed pathologies and resilience, others were associated with co-morbid pathologies (i.e., ZCWPW, SORL1, and APOE with hippocampal sclerosis, CELF1 with Lewy bodies and microinfarcts, and ABCA7 with macroinfarcts), and some were not associated with any pathology [160]. We used DNA methylation to delve further into the known genomic variants and found associations between DNA methylation in several AD genes [161–163].
We found other genomic variants associated with cognitive decline and AD, and some associated with other pathologies or with no pathologies [164–172]. We also used GWAS to identify genomic variants associated with resilience and found two genes, ENC1 and UNCSC, that also showed evidence with DNA methylation and expression [162]. Interestingly, we also found that UNCSC was associated with amyloid angiopathy [173]. We did not find evidence of an association of the fragile X permutation expansion with cognition [174]. We also conducted GWAS for neuropathologic traits [175, 176]. Finally, we identified a variant in TMEM106B and expression of GRN associated with TDP-43 [177].
Experiential risk factors
Using change-point models we found that education was associated with better cognition, a slower rate of cognitive decline and a delayed change point but a more rapid rate of decline after the change point[142]. Further, life-time cognitive activities as well as foreign language and music instruction were associated with a slower rate of cognitive decline including among Latinos [178, 179 ]. To address the potential for reverse causality, we used a cross-lagged model to show that cognitive activities initially predicts cognitive decline but as cognition becomes poor, cognition predicts decline in late-life activity [180]. Further, late-life cognitive activity was not related to common neuropathologies [181]. However, it was related to brain microstructure by neuroimaging, which partially mediated the association of cognitive activity with level of cognition [182]. We also found that total daily physical activity measured by actigraphy was associated with risk of AD dementia [183] and negative social interactions were associated with incident cognitive impairment [184].
We also found that both the DASH and Mediterranean diets were associated with a slower rate of cognitive decline [185]. We created the MIND diet which combines elements of the other two diets and found a stronger association with cognitive decline and AD dementia risk [186, 187]. Green leafy vegetables and seafood were indiviudally associated with cognitive decline, the latter driven by consumption of foods high in long-chain omega-3 fatty acids [188–190]. Interestingly, in matched plasma and brain samples, we found lower levels of oleic acid isomers and omega-3 and omega-6 fatty acids as well as oleic acid in AD plasma [191]. By contrast, we only found lower docosahexaenoic acid (DHA) in brain. Interestingly, we found that fish consumption was associated with measures of AD pathology [192]. This is one of very few non-genomic factors that we found directly associated with measures of AD pathology. The finding was restricted to those with APOE4, but that could result from greater power. Higher α-linolenic acid (18:3 n-3) was associated with fewer cerebral macroinfarctions. Finally, we found that γ-Tocopherol concentrations were associated with less AD pathology [193].
Psychological risk factors
We previously showed that depressive symptoms were associated with risk of AD dementia and did not change as AD dementia developed suggesting that the association is not reverse causality [13, 35]. Recently, we controlled for neuropathology and showed that it did not influence the association, nor were depressive symptoms a consequence of typical pathologies that cause dementia [194, 195]. Interestingly, lower density of dopamine neurons in the ventral tegmental area was associated with more depressive symptoms [196]. We previously found that rate of cognitive decline increases several fold about four years prior to death, a concept referred to as terminal decline [197, 198]. We found that conscientiousness was related to a slower rate of terminal decline and that this trait attenuated the association of Lewy bodies with terminal decline [199].
We found that cognitive decline was associated with several aspects of reduced well-being, or eudaimonic happiness [200]. One aspect of well-being, purpose in life, was associated with risk of AD dementia and modified the relation, of pathology to cognitive decline [201]. It was also associated with reduced odds of cerebral infarctions [202], as well as with reduced hospitalization [203]. By contrast, childhood emotional neglect and harm avoidance were both associated with increased odds of cerebral infarction [204, 205]. Further, neuroticism modified the association of vision with cognition [206]. Finally, loneliness was associated with AD risk and cognitive decline, but not with neuropathologies [30]; and we identified numerous genes in the amygdala and the dorsolateral prefrontal cortex related to loneliness [207, 208].
Medical factors
We first examined cerebrovascular disease factors. Lower body mass index (BMI) was related to cognitive decline in both African Americans and whites [209]. Also, lower hemoglobin was related to macroscopic infarcts [210]. We did not find associations of antiphospholipid antibodies to any measure of cerebrovascular disease or of genetic variants associated with homocysteine to be associated with any pathology [211, 212]. Diabetes was associated with subcortical macroscopic infarcts [213]. Interestingly, we found that insulin resistance in brain was related to measures of AD pathology [214]. We found that initiation of anticholinergic medicine had a negative impact on the slope of cognitive decline [215]. Also, antibodies to cytomegalovirus were related to cognitive decline and AD dementia in both African Americans and whites, and was associated with measures of AD pathology [216, 217]. Better odor identification on a smell test was positively associated with cognition, and worse scores were associated with loneliness and depressive symptoms [218]. When we examine the anterior olfactory nucleus, we find co-localization of β-amyloid, PHF-1 and Caspase-6, and the level of PHF-1 and Caspase-6 were positively correlated [219]. In two other papers we found that surgical menopause was related to cognitive decline and neurofibrillary tangles, and history of cancer was associated with a lower likelihood of AD dementia and PHFtau tangles [220, 221]. Finally, in an in-vivo imaging study restricted to persons without dementia, we found that c-reactive protein and tumor necrosis factor-alpha were associated with cognition and brain microstructure [222]
Using data generated with the accelerometer, we developed a metric of rest-activity fragmentation as a proxy for sleep fragmentation [48, 223]. This measure was related to cognition and incident AD dementia, as well as lower cortical gray matter volume in the inferior frontal gyrus pars orbitalis and lateral orbitofrontal cortex [224, 225]. It modified the relation of APOE4 to measures of AD pathology and was directly associated with measures of cerebrovascular disease [226, 227]. The same data was used to generate circadian rhythms. We found inter-daily variability associated with the metabolic syndrome [228]. Further, we investigated the influence of several clock genes, using genomic, epigenomic, and transcriptomic data on circadian and seasonal rhythms [229–233]. Separately, we found that sleep fragmentation and circadian rhythm disruption were related to neuron counts in the ventrolateral preoptic/intermediate nucleus of the hypothalamus, and the suprachiasmatic nucleus [229].
Risk factors, neuropathology, and motor structure and function
Parkinsonism was progressive and associated with adverse health outcomes [183, 230–233]. Changes in motor structure and function were strongly correlated with changes in cognition and both related to the same neuropathologies. Parkinsonism was associated with risk of death, MCI, and AD dementia, and common brain pathologies were related to parkinsonian signs, and progression of physical frailty, respiratory function, and cognitive decline [234–239]. Further, neurons in the locus coeruleus were related to parkinsonian signs and to cognition [134, 240]. Thus, it was not surprising that many risk factors for cognitive decline and AD dementia are also risk factors for motor outcomes including physical and social activity, social isolation, neuroticism, harm avoidance, extraversion, and antihypertensive medications [232, 233, 241–244]. By contrast, traumatic brain injury was related to progression of parkinsonism and PD pathology but not change in cognition or AD pathology [245]. Sleep, was also associated with motor outcomes in both African Americans and Caucasians, and with PD pathology [246–248]. We also conducted a candidate SNP analysis examining PD risk alleles with a variety of motor clinical and pathologic phenotypes [249]. We are just beginning to explore the spinal cord examining the distribution of α-synuclein, atherosclerosis, white matter pallor, and their association with brain pathology and motor function [259–261]. Recently, we added a body sensor, a triaxial accelerometer with 3 gyroscopes, which participant’s wear on a belt, which continuously records 3 acceleration and 3 angular velocity signals during annual gait testing. We examined the metrics derived from these recording during several gait and balance tests and their relation to IADL, parkinsonism, and physical activity [78–82]. Finally, using resting state fMRI we interrogated connectivity in relation to chronic musculoskeletal pain [250]. In a separate study we found that physical activity modified the relation of white matter hyperintensities (WMH) with motor function [251].
Behavioral- and neuro-economics and decision making
We first examined health and financial decision making. We found both associated with risk of death, incident MCI and AD and cognitive decline among persons without dementia. Further, several factors help maintain decision making, including literacy and access to resources (e.g. internet use) [252–257]. Next, we examined health and financial literacy. These also are associated with cognition, MCI, functional status, mental health, health promoting behaviors, and APOE4 [258–260]. Literacy is both a consequence of cognitive decline and a predictor of future cognitive decline and incident AD dementia [261–264]. Interestingly, AD pathology was associated with literacy controlling for cognition [264]. Among persons without dementia, we found that higher diffusion anisotropy was associated with better financial literacy, especially tracts connecting right hemisphere temporal-parietal brain regions [265]. Financial literacy was also associated with greater functional connectivity between the posterior cingulate cortex and the right ventromedial prefrontal cortex, the left postcentral gyrus, and the right precuneus, and negatively associated with functional connectivity with left caudate [266]. Greater temporal discounting was associated with increased risk of death, cognition, and cognitive decline [267–269]. Discounting also was positively associated with functional connectivity to the right middle temporal regions and ventromedial prefrontal cortex, and negatively associated with parahippocampal and right cerebellar regions [270]. Risk aversion was associated with decision making and cognitive decline [269, 271]. Using a seed in the anterior cingulate, we found that risk averse persons had greater connectivity to clusters within multiple brain regions (e.g., insula, inferior and orbital, frontal, parahippocampal), and those low in risk aversion had greater connectivity to numerous clusters (e.g., inferior temporal, superior, middle, and medial frontal regions) [272]. We also reported that susceptibility to scams was negatively associated with cognition, well-being, and literacy, MCI, and cognitive decline [85, 273, 274]. There was also an inverse association between overall grey matter and susceptibility to scams [275]. Finally, cognitive decline and over-confidence in one’s financial knowledge was associated with fraud victimization [85].
Novel drug and biomarker discovery pipeline
The multilayer omics data are now being used to support a novel drug and biomarker discovery pipeline as part of the Accelerating Medicines Partnership-AD (Fig 3) [276, 277]. We are still at the early stage of generating omics data, performing the quality control, and developing a basic understanding of relationships with AD quantitative endophenotypes with epigenomic and transcriptomic data [278–286]. We are just beginning to examine relations of omic between brain and blood and brain and neuroimaging as part of our nascent biomarker discovery protocol [287, 288]. This will be complemented in the future with multiple layers of blood omics that can be related to ante-mortem imaging and brain omics. Further, we are still refining our ex vivo validation approaches [289, 290]. A forward looking framework has been developed and we will focus on neural reserve or resilience as a high value target [291, 292]. We identified one high value module that nominates genes/proteins that drive resilience and others that drive amyloid-β [293]. The latter have been validated in an ex vivo model system. Finally, as we look forward to better clinical trial designs we have been refining our cognitive phenotype that would best serve as a clinical trial outcome [294–296].
Fig. 3.
Cohort studies generating ante- and post-mortem biospecimens which are used to generate multi-layered omics data. These data feed a systems biology computation pipeline for therapeutic target nomination. There are two stages of functional validation, one with targeted proteomics using brain tissue from the same cases and the other with a variety of high throughput ex vivo models. High value targets will then move to small molecule drug screen and eventual drug selection.
Resource sharing
The ROSMAP investigators are committed to timely data sharing of raw or processed data which can be found on our Resource Sharing Hub with relevant links to the AMP-AD Knowledge Portal [297, 298]. A sample of work done with ROSMAP data including as part of translational studies and consortia is provided to give the community a better sense of the range of work that could be done leveraging the resource [299–350].
DISCUSSION
Ongoing for nearly a quarter of a century, ROSMAP has generated a wealth of data across a range of age-related phenotypes from the same individuals. It has served as a research resource for investigators around the globe who have generated about 400 publications over the past 6 years. The data support some general conclusions. Perhaps the over-arching theme running through the work is complexity. Complexity at multiple levels: 1) continuum of AD, 2) mixed and newly recognized pathologies, 3) neural reserve or resilience, and 4) non-cognitive phenotypes. Complexity has important implications for drug discovery.
Continuum of AD
Findings illustrate that cognitive decline as part of the AD dementia syndrome begins years or decades prior to AD dementia onset and MCI onset. We found that AD and other pathologies are common in persons without dementia and without MCI. Further, AD pathology is associated with change in cognition a decade or more prior to death, and that these associations occur long before dementia onset. These data complement data from other clinical-pathologic studies illustrating that AD pathology is present in persons without dementia [351–353]. However, there is much less information from other studies linking pathology to trajectories of cognitive change [354–357]. These data are complemented by clinical-imaging studies with amyloid and subsequently tau PET data [358–362]. More recently, amyloid and tau PET done on younger cohorts are finding that these pathologies appear to accumulate years prior to onset of overt cognitive impairment [363–366]. Together these data provide strong support for a new framework being proposed to capture the continuum of AD that allows a diagnosis of AD to be made in the absence of cognitive symptoms [367]. The framework is based largely on a recently proposed A/T/N classification scheme [368].
Mixed and newly recognized pathologies
We find that the clinical syndrome AD dementia cognitive impairment and dementia is a complex process that results from the additive and interactive effects of numerous pathologies. This is consistent with the results of several prior clinical-pathologic studies that have examined this issue [4, 369–377]. Similar data are emerging from neuroimaging studies as well [378–380] ]. At this point we have documented 9 pathologies on more than 1000 brains and find nearly 250 combinations. Besides AD pathology, this includes TDP-43/hippocampal sclerosis, several measures of macro- and micro-vascular disease. We also have other pathologies on a subset of participants, including some measured with ex vivo imaging, which will further increase the number of combinations.
Neural reserve or resilience
There are several approaches to the concept of neural reserve or resilience [381–384]. Many researchers limit the concept of reserve or resilience to having a unidirectional beneficial effect. We take a complementary approach that assumes all cognitive systems have some reserve; however, some have more reserve and others less [385]. Persons with more reserve have a slower rate of cognitive decline and lower AD dementia risk, and those with less reserve have a faster rate of cognitive decline and higher AD dementia risk. We have found many risk factors associated with more (e.g., cognitive activity, purpose in life) or less (e.g., neuroticism, loneliness) reserve, and some biologic factors associated with more reserve (e.g., BDNF expression, neuron density, presynaptic proteins), and network modules with genes associated with more and others with less reserve [292]. Several other groups have reported on the ability of factors to buffer or augment the impact of pathology on cognition [386–392]. Similar finding have been reported with neuroimaging and CSF biomarkers of AD pathology [361, 392–398]. Functional imaging approaches are also being employed to explore the neural basis of reserve [399, 400]. Finally, similar to our findings of neurons and presynaptic proteins, several groups have reported other structural indices that underlie reserve [401–404].
Non-cognitive phenotypes: motor function and decision making
Our work is congruent with work by other groups that a wide range of motor phenotypes are related to cognitive decline and to AD [405–410]. In addition, like others we find that cognitive function and many risk factors for AD are also related to change in motor structure and function [411, 412]. Our work extends these findings by showing that simultaneous change in cognitive and motor decline is highly correlated [239]. Few studies address whether cognitive or motor decline begins earlier [413]. The idea that both late-life cognitive and motor impairment may share a common neurobiology is supported by our postmortem results and work by others [404, 414–418]. Our studies extend these findings by showing that AD and other pathologies are related to level as well as progressive decline of several motor phenotypes [234, 236, 238, 239]. Together the clinical and postmortem findings are consistent with accumulating evidence that both cognition and motor function may rely on similar underlying neural systems essential for planning and monitoring goal – directed behavior and both may be affected by AD and other common brain pathologies [367, 419–422].
We also showed that cognition, AD and other pathologies negatively impact health and financial decision making [254–258, 269, 270]. This work is consistent with prior studies that have reported impaired decision making among persons with overt cognitive syndromes [423–427] and some small studies of non-demented persons [428–432] but extends prior work by showing that impaired decision making among cognitively intact persons is in fact a consequence of preclinical cognitive decline. Few studies have examined the association of decision making and related behaviors with subsequent cognitive or other health outcomes [423, 428, 431]. Our work suggests that decision making and related behaviors predict several adverse health outcomes including incident AD, incident mild cognitive impairment and mortality [252, 262–265, 268]. Moreover, whereas some prior studies have examined the neural underpinnings of select aspects decision making in older persons using neuroimaging approaches [433–439], we expanded this work by examining multiple aspects of decision making using a variety of imaging approaches [265–274] Finally, we found that age-related changes in decision making are associated with common neuropathologies such as AD pathology [264, 265]. Together, findings suggest that impaired decision making is an early manifestation of AD and other neuropathologies and a harbinger of adverse cognitive and other health outcomes.
Implications of complexity for drug discovery
It has been a bleak 15 years in the AD drug discovery space. Other than re-formulations, no new drug has been approved by the Food and Drug Administration (FDA) since 2003. The string of failed studies is long despite the investment of billions of dollars from the public and private sectors, the participation of many tens of thousands of people in clinical trials, and the efforts of thousands of researchers and study staff [440]. There are many reasons for these failures. A recent analysis pointed to complexity, low signal-to-noise, and recruitment/retention [441]. As many people have and others will develop AD dementia, more robust symptomatic treatment is urgently needed. However, symptomatic therapies will not reduce the overall human and economic toll of AD [442]. This can only be accomplished by prevention.
There are currently about 100 drugs in the AD pipeline in the USA with an additional 100 in development in the European Union with participants ranging from those with moderate to severe AD dementia to asymptomatic persons [443, 444]. The therapies are relatively evenly divided into three buckets. The first is small molecules for therapeutic treatment. The other two are disease modifying agents, one of which is small molecules and the other immuno-therapies.
The majority of the disease modifying agents target amyloid and tau. It has been argued that reducing complexity and creating more homogenous populations for clinical trials will improve the signal to noise ratio improving the likelihood of success. Thus, many trials now enrich studies by enrolling those at genetic risk or with a positive amyloid PET [445–447]. Perhaps this will be a successful approach. However, failure will only inform on subpopulations. A drug that fails to slow cognitive decline among persons at genetic risk or those who have amyloid might still work on those not at genetic risk of those who have not yet developed amyloid. Estimates suggest that studies to slow cognitive decline in asymptomatic persons may need to be much longer than is currently being done [448]. Further, requiring multiple spinal taps and/or PET scans likely increases the healthy volunteer effect by excluding people with non-cognitive factors that predict cognitive decline and are associated with AD pathology such as gait disturbance and frailty [235, 237, 239, 449]. We also found that β-amyloid does not predict cognitive decline after controlling for tangles and that β-amyloid and tangles together only account for about 25% of the variance of cognitive decline [118, 125, 450]. Are anti-amyloid studies adequately powered to impact such a small component of the trajectory? In addition, we found that the impact of nine common pathologies, e.g., pathologic AD, on cognitive decline varies widely depending on the presence of other pathologies, many of which are beyond the resolving power of extant biomarkers. Finally, is developing a biomarker for each pathology and a cocktail to treat each pathology really scalable? This could result in multiple cocktails over a long period of time in older persons with aged livers and kidneys, at a cost that is likely beyond what can be paid.
An alternate therapeutic strategy would be to target resilience itself. All physiologic systems have reserve or resilience. In some cases it is simply an extra organ, e.g., lung, kidney. However, with the brain it is plasticity that allows it to tolerate and/or recover from injury and disease. There is no evolutionary pressure to develop these systems from age related disease. Thus, there are likely few such systems and they are, as we have found, relatively agnostic to specific age related disease. We are currently using our drug discovery pipeline to find novel targets for reserve. To determine if they are druggable, the field needs to develop and validate an ex-vivo model for high throughput drug screens. In other words, we will need to model cognitive decline in a dish.
ACKNOWLEDGMENTS
This work is dedicated to the participants in the Religious Orders Study and Rush Memory and Aging Project. We thank the faculty and staff of the Rush Alzheimer’s Disease Center, and our collaborators around the world. Work was supported by grants from the National Institutes of Health: P30AG10161, RF1AG15819, R01AG17917, RF1AG22018, R01AG33678, R01AG34374, R01AG36042, R01AG40039, R01AG042210, U01AG46152, R01AG47976, R01AG43379, RF1AG54057, R01AG56352, R01NS78009, and UH2NS100599, and the Illinois Department of Public Health.
REFERENCES
- [1].Maurer K, Volk S, Gerbaldo H (1997) Auguste D and Alzheimer’s disease. Lancet 349, 1546–1549. [DOI] [PubMed] [Google Scholar]
- [2].Amaducci LA, Rocca WA, Schoenberg BS (1986) Origin of the distinction between Alzheimer’s disease and senile dementia: how history can clarify nosology. Neurology 36, 1497–1499. [DOI] [PubMed] [Google Scholar]
- [3].Cairns NJ, Perrin RJ, Franklin EE, Carter D, Vincent B, Xie M, Bateman RJ, Benzinger T, Friedrichsen K, Brooks WS, Halliday GM, McLean C, Ghetti B, Morris JC (2015) Neuropathologic assessment of participants in two multi-center longitudinal observational studies: the Alzheimer Disease Neuroimaging Initiative (ADNI) and the Dominantly Inherited Alzheimer Network (DIAN). Neuropathology 35, 390–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Toledo JB, Arnold SE, Raible K, Brettschneider J, Xie SX, Grossman M, Monsell SE, Kukull WA, Trojanowski JQ (2013) Contribution of cerebrovascular disease in autopsy confirmed neurodegenerative disease cases in the National Alzheimer’s Coordinating Centre. Brain 136, 2697–2706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Schneider JA, Aggarwal NT, Barnes L, Boyle P, Bennett DA (2009) The neuropathology of older persons with and without dementia from community versus clinic cohorts. J Alzheimers Dis 18, 691–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Snowdon DA (1997) Aging and Alzheimer’s disease: lessons from the Nun Study. Gerontologist 37, 150–156. [DOI] [PubMed] [Google Scholar]
- [7].White L, Launer L (2006) Relevance of cardiovascular risk factors and ischemic cerebrovascular disease to the pathogenesis of Alzheimer disease: a review of accrued findings from the Honolulu-Asia Aging Study. Alzheimer Dis Assoc Disord 20, S79–83. [DOI] [PubMed] [Google Scholar]
- [8].Shinkawa A, Ueda K, Kiyohara Y, Kato I, Sueishi K, Tsuneyoshi M, Fujishima M (1995) Silent cerebral infarction in a community-based autopsy series in Japan. The Hisayama Study. Stroke 26, 380–385. [DOI] [PubMed] [Google Scholar]
- [9].Zaccai J, Ince P, Brayne C (2006) Population-based neuropathological studies of dementia: design, methods and areas of investigation--a systematic review. BMC Neurol 6, 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Bennett DA, Schneider JA, Buchman AS, Barnes LL, Boyle PA, Wilson RS (2012) Overview and Findings From the Rush Memory and Aging Project. Curr Alzheimer Res 9, 646–663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Bennett DA, Schneider JA, Arvanitakis Z, Wilson RS (2012) Overview and findings from the religious orders study. Curr Alzheimer Res 9, 628–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Wilson RS, Mendes De Leon CF, Barnes LL, Schneider JA, Bienias JL, Evans DA, Bennett DA (2002) Participation in cognitively stimulating activities and risk of incident Alzheimer disease. Jama 287, 742–748. [DOI] [PubMed] [Google Scholar]
- [13].Wilson RS, Barnes LL, Mendes de Leon CF, Aggarwal NT, Schneider JS, Bach J, Pilat J, Beckett LA, Arnold SE, Evans DA, Bennett DA (2002) Depressive symptoms, cognitive decline, and risk of AD in older persons. Neurology 59, 364–370. [DOI] [PubMed] [Google Scholar]
- [14].Barnes LL, Wilson RS, Schneider JA, Bienias JL, Evans DA, Bennett DA (2003) Gender, cognitive decline, and risk of AD in older persons. Neurology 60, 1777–1781. [DOI] [PubMed] [Google Scholar]
- [15].Wilson R, Barnes L, Bennett D (2003) Assessment of lifetime participation in cognitively stimulating activities. J Clin Exp Neuropsychol 25, 634–642. [DOI] [PubMed] [Google Scholar]
- [16].Wilson RS, Bienias JL, Mendes de Leon CF, Evans DA, Bennett DA (2003) Negative affect and mortality in older persons. Am J Epidemiol 158, 827–835. [DOI] [PubMed] [Google Scholar]
- [17].Wilson RS, Evans DA, Bienias JL, Mendes de Leon CF, Schneider JA, Bennett DA (2003) Proneness to psychological distress is associated with risk of Alzheimer’s disease. Neurology 61, 1479–1485. [DOI] [PubMed] [Google Scholar]
- [18].Arvanitakis Z, Wilson RS, Bienias JL, Evans DA, Bennett DA (2004) Diabetes mellitus and risk of Alzheimer disease and decline in cognitive function. Arch Neurol 61, 661–666. [DOI] [PubMed] [Google Scholar]
- [19].Wilson RS, Mendes de Leon CF, Bienias JL, Evans DA, Bennett DA (2004) Personality and mortality in old age. J Gerontol B Psychol Sci Soc Sci 59, P110–116. [DOI] [PubMed] [Google Scholar]
- [20].Wilson RS, Scherr PA, Hoganson G, Bienias JL, Evans DA, Bennett DA (2005) Early life socioeconomic status and late life risk of Alzheimer’s disease. Neuroepidemiology 25, 8–14. [DOI] [PubMed] [Google Scholar]
- [21].Wilson RS, Barnes LL, Krueger KR, Hoganson G, Bienias JL, Bennett DA (2005) Early and late life cognitive activity and cognitive systems in old age. J Int Neuropsychol Soc 11, 400–407. [PubMed] [Google Scholar]
- [22].Buchman AS, Wilson RS, Bienias JL, Shah RC, Evans DA, Bennett DA (2005) Change in body mass index and risk of incident Alzheimer disease. Neurology 65, 892–897. [DOI] [PubMed] [Google Scholar]
- [23].Shah RC, Wilson RS, Bienias JL, Arvanitakis Z, Evans DA, Bennett DA (2006) Relation of blood pressure to risk of incident Alzheimer’s disease and change in global cognitive function in older persons. Neuroepidemiology 26, 30–36. [DOI] [PubMed] [Google Scholar]
- [24].Wilson RS, Krueger KR, Arnold SE, Barnes LL, Mendes de Leon CF, Bienias JL, Bennett DA (2006) Childhood adversity and psychosocial adjustment in old age. Am J Geriatr Psychiatry 14, 307–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Wilson RS, Buchman AS, Arnold SE, Shah RC, Tang Y, Bennett DA (2006) Harm avoidance and disability in old age. Exp Aging Res 32, 243–261. [DOI] [PubMed] [Google Scholar]
- [26].Krueger KR, Wilson RS, Shah RC, Tang Y, Bennett DA (2006) Personality and incident disability in older persons. Age Ageing 35, 428–433. [DOI] [PubMed] [Google Scholar]
- [27].Park M, Comella CL, Leurgans SE, Fan W, Wilson RS, Bennett DA (2006) Association of daytime napping and Parkinsonian signs in Alzheimer’s disease. Sleep Med 7, 614–618. [DOI] [PubMed] [Google Scholar]
- [28].Wilson RS, Arnold SE, Schneider JA, Kelly JF, Tang Y, Bennett DA (2006) Chronic psychological distress and risk of Alzheimer’s disease in old age. Neuroepidemiology 27, 143–153. [DOI] [PubMed] [Google Scholar]
- [29].Barnes LL, Schneider JA, Boyle PA, Bienias JL, Bennett DA (2006) Memory complaints are related to Alzheimer disease pathology in older persons. Neurology 67, 1581–1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Wilson RS, Krueger KR, Arnold SE, Schneider JA, Kelly JF, Barnes LL, Tang Y, Bennett DA (2007) Loneliness and risk of Alzheimer disease. Arch Gen Psychiatry 64, 234–240. [DOI] [PubMed] [Google Scholar]
- [31].Buchman AS, Boyle PA, Wilson RS, Bienias JL, Bennett DA (2007) Physical activity and motor decline in older persons. Muscle Nerve 35, 354–362. [DOI] [PubMed] [Google Scholar]
- [32].Wilson RS, Schneider JA, Arnold SE, Tang Y, Boyle PA, Bennett DA (2007) Olfactory identification and incidence of mild cognitive impairment in older age. Arch Gen Psychiatry 64, 802–808. [DOI] [PubMed] [Google Scholar]
- [33].Wilson RS, Scherr PA, Schneider JA, Tang Y, Bennett DA (2007) Relation of cognitive activity to risk of developing Alzheimer disease. Neurology 69, 1911–1920. [DOI] [PubMed] [Google Scholar]
- [34].Wilson RS, Schneider JA, Arnold SE, Bienias JL, Bennett DA (2007) Conscientiousness and the incidence of Alzheimer disease and mild cognitive impairment. Arch Gen Psychiatry 64, 1204–1212. [DOI] [PubMed] [Google Scholar]
- [35].Wilson RS, Arnold SE, Beck TL, Bienias JL, Bennett DA (2008) Change in depressive symptoms during the prodromal phase of Alzheimer disease. Arch Gen Psychiatry 65, 439–445. [DOI] [PubMed] [Google Scholar]
- [36].Buchman AS, Boyle PA, Wilson RS, Gu L, Bienias JL, Bennett DA (2008) Pulmonary function, muscle strength and mortality in old age. Mech Ageing Dev 129, 625–631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Buchman AS, Boyle PA, Wilson RS, Leurgans S, Shah RC, Bennett DA (2008) Respiratory muscle strength predicts decline in mobility in older persons. Neuroepidemiology 31, 174–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Buchman AS, Boyle PA, Wilson RS, Fleischman DA, Leurgans S, Bennett DA (2009) Association between late-life social activity and motor decline in older adults. Arch Intern Med 169, 1139–1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Buchman AS, Tanne D, Boyle PA, Shah RC, Leurgans SE, Bennett DA (2009) Kidney function is associated with the rate of cognitive decline in the elderly. Neurology 73, 920–927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Boyle PA, Buchman AS, Barnes LL, Bennett DA (2010) Effect of a purpose in life on risk of incident Alzheimer disease and mild cognitive impairment in community-dwelling older persons. Arch Gen Psychiatry 67, 304–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Boyle PA, Buchman AS, Barnes LL, James BD, Bennett DA (2010) Association between life space and risk of mortality in advanced age. J Am Geriatr Soc 58, 1925–1930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Shah RC, Buchman AS, Boyle PA, Leurgans SE, Wilson RS, Andersson GB, Bennett DA (2011) Musculoskeletal pain is associated with incident mobility disability in community-dwelling elders. J Gerontol A Biol Sci Med Sci 66, 82–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Buchman AS, Shah RC, Leurgans SE, Boyle PA, Wilson RS, Bennett DA (2010) Musculoskeletal pain and incident disability in community-dwelling older adults. Arthritis Care Res (Hoboken) 62, 1287–1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Wilson RS, Begeny CT, Boyle PA, Schneider JA, Bennett DA (2011) Vulnerability to stress, anxiety, and development of dementia in old age. Am J Geriatr Psychiatry 19, 327–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Shah RC, Buchman AS, Wilson RS, Leurgans SE, Bennett DA (2011) Hemoglobin level in older persons and incident Alzheimer disease: prospective cohort analysis. Neurology 77, 219–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Wilson RS, Boyle PA, Buchman AS, Yu L, Arnold SE, Bennett DA (2011) Harm avoidance and risk of Alzheimer’s disease. Psychosom Med 73, 690–696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Buchman AS, Wilson RS, Bennett DA (2008) Total daily activity is associated with cognition in older persons. Am J Geriatr Psychiatry 16, 697–701. [DOI] [PubMed] [Google Scholar]
- [48].Lim AS, Yu L, Costa MD, Buchman AS, Bennett DA, Leurgans SE, Saper CB (2011) Quantification of the fragmentation of rest-activity patterns in elderly individuals using a state transition analysis. Sleep 34, 1569–1581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Morris MC, Evans DA, Bienias JL, Tangney CC, Bennett DA, Aggarwal N, Schneider J, Wilson RS (2003) Dietary fats and the risk of incident Alzheimer disease. Arch Neurol 60, 194–200. [DOI] [PubMed] [Google Scholar]
- [50].De Jager PL, Shulman JM, Chibnik LB, Keenan BT, Raj T, Wilson RS, Yu L, Leurgans SE, Tran D, Aubin C, Anderson CD, Biffi A, Corneveaux JJ, Huentelman MJ, Rosand J, Daly MJ, Myers AJ, Reiman EM, Bennett DA, Evans DA (2012) A genome-wide scan for common variants affecting the rate of age-related cognitive decline. Neurobiol Aging 33, 1017.e1011–1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Bennett DA, Wilson RS, Schneider JA, Evans DA, Aggarwal NT, Arnold SE, Cochran EJ, Berry-Kravis E, Bienias JL (2003) Apolipoprotein E epsilon4 allele, AD pathology, and the clinical expression of Alzheimer’s disease. Neurology 60, 246–252. [DOI] [PubMed] [Google Scholar]
- [52].Bennett DA, Schneider JA, Wilson RS, Bienias JL, Arnold SE (2004) Neurofibrillary tangles mediate the association of amyloid load with clinical Alzheimer disease and level of cognitive function. Arch Neurol 61, 378–384. [DOI] [PubMed] [Google Scholar]
- [53].Bennett DA, Schneider JA, Bienias JL, Evans DA, Wilson RS (2005) Mild cognitive impairment is related to Alzheimer disease pathology and cerebral infarctions. Neurology 64, 834–841. [DOI] [PubMed] [Google Scholar]
- [54].Bennett DA, Schneider JA, Tang Y, Arnold SE, Wilson RS (2006) The effect of social networks on the relation between Alzheimer’s disease pathology and level of cognitive function in old people: a longitudinal cohort study. Lancet Neurol 5, 406–412. [DOI] [PubMed] [Google Scholar]
- [55].Bennett DA, Schneider JA, Arvanitakis Z, Kelly JF, Aggarwal NT, Shah RC, Wilson RS (2006) Neuropathology of older persons without cognitive impairment from two community-based studies. Neurology 66, 1837–1844. [DOI] [PubMed] [Google Scholar]
- [56].Schneider JA, Wilson RS, Bienias JL, Evans DA, Bennett DA (2004) Cerebral infarctions and the likelihood of dementia from Alzheimer disease pathology. Neurology 62, 1148–1155. [DOI] [PubMed] [Google Scholar]
- [57].Schneider JA, Li JL, Li Y, Wilson RS, Kordower JH, Bennett DA (2006) Substantia nigra tangles are related to gait impairment in older persons. Ann Neurol 59, 166–173. [DOI] [PubMed] [Google Scholar]
- [58].Schneider JA, Arvanitakis Z, Bang W, Bennett DA (2007) Mixed brain pathologies account for most dementia cases in community-dwelling older persons. Neurology 69, 2197–2204. [DOI] [PubMed] [Google Scholar]
- [59].Schneider JA, Arvanitakis Z, Leurgans SE, Bennett DA (2009) The neuropathology of probable Alzheimer disease and mild cognitive impairment. Ann Neurol 66, 200–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Arvanitakis Z, Leurgans SE, Wang Z, Wilson RS, Bennett DA, Schneider JA (2011) Cerebral amyloid angiopathy pathology and cognitive domains in older persons. Ann Neurol 69, 320–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Wilson RS, Yu L, Trojanowski JQ, Chen EY, Boyle PA, Bennett DA, Schneider JA (2013) TDP-43 pathology, cognitive decline, and dementia in old age. JAMA Neurol 70, 1418–1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Honer WG, Barr AM, Sawada K, Thornton AE, Morris MC, Leurgans SE, Schneider JA, Bennett DA (2012) Cognitive reserve, presynaptic proteins and dementia in the elderly. Transl Psychiatry 2, e114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Fleischman DA, Arfanakis K, Kelly JF, Rajendran N, Buchman AS, Morris MC, Barnes LL, Bennett DA (2010) Regional brain cortical thinning and systemic inflammation in older persons without dementia. J Am Geriatr Soc 58, 1823–1825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Dawe RJ, Bennett DA, Schneider JA, Vasireddi SK, Arfanakis K (2009) Postmortem MRI of human brain hemispheres: T2 relaxation times during formaldehyde fixation. Magn Reson Med 61, 810–818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Dawe RJ, Bennett DA, Schneider JA, Arfanakis K (2011) Neuropathologic correlates of hippocampal atrophy in the elderly: a clinical, pathologic, postmortem MRI study. PLoS One 6, e26286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Wilson RS, Beckett LA, Barnes LL, Schneider JA, Bach J, Evans DA, Bennett DA (2002) Individual differences in rates of change in cognitive abilities of older persons. Psychol Aging 17, 179–193. [PubMed] [Google Scholar]
- [67].Wilson RS, Bennett DA (2005) Assessment of cognitive decline in old age with brief tests amenable to telephone administration. Neuroepidemiology 25, 19–25. [DOI] [PubMed] [Google Scholar]
- [68].Wilson RS, Arnold SE, Tang Y, Bennett DA (2006) Odor identification and decline in different cognitive domains in old age. Neuroepidemiology 26, 61–67. [DOI] [PubMed] [Google Scholar]
- [69].Bennett DA, Shannon KM, Beckett LA, Goetz CG, Wilson RS (1997) Metric properties of nurses’ ratings of parkinsonian signs with a modified Unified Parkinson’s Disease Rating Scale. Neurology 49, 1580–1587. [DOI] [PubMed] [Google Scholar]
- [70].Bennett DA, Shannon KM, Beckett LA, Wilson RS (1999) Dimensionality of parkinsonian signs in aging and Alzheimer’s disease. J Gerontol A Biol Sci Med Sci 54, M191–196. [DOI] [PubMed] [Google Scholar]
- [71].Wilson RS, Schneider JA, Beckett LA, Evans DA, Bennett DA (2002) Progression of gait disorder and rigidity and risk of death in older persons. Neurology 58, 1815–1819. [DOI] [PubMed] [Google Scholar]
- [72].Boyle PA, Wilson RS, Aggarwal NT, Arvanitakis Z, Kelly J, Bienias JL, Bennett DA (2005) Parkinsonian signs in subjects with mild cognitive impairment. Neurology 65, 1901–1906. [DOI] [PubMed] [Google Scholar]
- [73].Buchman AS, Wilson RS, Boyle PA, Bienias JL, Bennett DA (2007) Change in motor function and risk of mortality in older persons. J Am Geriatr Soc 55, 11–19. [DOI] [PubMed] [Google Scholar]
- [74].Buchman AS, Wilson RS, Boyle PA, Bienias JL, Bennett DA (2007) Grip strength and the risk of incident Alzheimer’s disease. Neuroepidemiology 29, 66–73. [DOI] [PubMed] [Google Scholar]
- [75].Buchman AS, Wilson RS, Boyle PA, Tang Y, Fleischman DA, Bennett DA (2007) Physical activity and leg strength predict decline in mobility performance in older persons. J Am Geriatr Soc 55, 1618–1623. [DOI] [PubMed] [Google Scholar]
- [76].Boyle PA, Buchman AS, Wilson RS, Leurgans SE, Bennett DA (2009) Association of muscle strength with the risk of Alzheimer disease and the rate of cognitive decline in community-dwelling older persons. Arch Neurol 66, 1339–1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [77].Buchman AS, Wilson RS, Bienias JL, Bennett DA (2005) Gender differences in motor performance of older persons. Geriatrics Gerontology International 5, 59–65. [DOI] [PubMed] [Google Scholar]
- [78].Dawe RJ, Leurgans SE, Yang J, Bennett JM, Hausdorff JM, Lim AS, Gaiteri C, Bennett DA, Buchman AS (2017) Association between Quantitative Gait and Balance Measures and Total Daily Physical Activity in Community-Dwelling Older Adults. J Gerontol A Biol Sci Med Sci. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [79].Weiss A, Mirelman A, Giladi N, Barnes LL, Bennett DA, Buchman AS, Hausdorff JM (2016) Transition Between the Timed up and Go Turn to Sit Subtasks: Is Timing Everything? J Am Med Dir Assoc 17, 864.e869–864.e815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [80].Mirelman A, Weiss A, Buchman AS, Bennett DA, Giladi N, Hausdorff JM (2014) Association between performance on Timed Up and Go sub-tasks and Mild Cognitive Impairment: Further insights into the cognitive aspects of the TUG. Journal of the American Geriatrics Society 62, 673–678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [81].Buchman AS, Leurgans SE, Weiss A, VanderHorst V, Mirelman A, Dawe R, Barnes LL, Wilson RS, Hausdorff JM, Bennett DA (2014) Associations between Quantitative Mobility Measures Derived from Components of Conventional Mobility Testing and Parkinsonian Gait in Older Adults. PLoS ONE 9, e86262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [82].Weiss A, Mirelman A, Buchman AS, Bennett DA, Hausdorff JM (2013) Using a body-fixed sensor to identify subclinical gait difficulties in older adults with IADL disability: maximizing the output of the timed up and go. PLoS One 8, e68885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [83].Boyle PA, Buchman AS, Bennett DA (2010) Purpose in life is associated with a reduced risk of incident disability among community-dwelling older persons. Am J Geriatr Psychiatry 18, 1093–1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [84].James BD, Boyle PA, Bennett JS, Bennett DA (2012) The impact of health and financial literacy on decision making in community-based older adults. Gerontology 58, 531–539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [85].Gamble K, Boyle PA, Yu L, Bennett DA, The causes and consequences of financial fraud among older Americans.,Center for Retirement Research, Boston College; http://crr.bc.edu/wp-content/uploads/2014/11/wp_2014-13.pdf, [Google Scholar]
- [86].Gamble K, Boyle P, Yu L, Bennett D (2015) Aging and Financial Decision Making. Manage Sci 61, 2603–2610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [87].Bennett DA, Schneider JA, Aggarwal NT, Arvanitakis Z, Shah RC, Kelly JF, Fox JH, Cochran EJ, Arends D, Treinkman AD, Wilson RS (2006) Decision rules guiding the clinical diagnosis of Alzheimer’s disease in two community-based cohort studies compared to standard practice in a clinic-based cohort study. Neuroepidemiology 27, 169–176. [DOI] [PubMed] [Google Scholar]
- [88].Bennett DA, Wilson RS, Schneider JA, Evans DA, Beckett LA, Aggarwal NT, Barnes LL, Fox JH, Bach J (2002) Natural history of mild cognitive impairment in older persons. Neurology 59, 198–205. [DOI] [PubMed] [Google Scholar]
- [89].Schneider JA, Bienias JL, Wilson RS, Berry-Kravis E, Evans DA, Bennett DA (2005) The apolipoprotein E epsilon4 allele increases the odds of chronic cerebral infarction [corrected] detected at autopsy in older persons. Stroke 36, 954–959. [DOI] [PubMed] [Google Scholar]
- [90].Wilson RS, Schneider JA, Bienias JL, Arnold SE, Evans DA, Bennett DA (2003) Depressive symptoms, clinical AD, and cortical plaques and tangles in older persons. Neurology 61, 1102–1107. [DOI] [PubMed] [Google Scholar]
- [91].Buracchio T, Arvanitakis Z, Leurgans S, Bennett DA (2010) Parkinsonian signs and incident falls in older persons without Parkinson’s disease. J Am Geriatr Soc 58, 205–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [92].James BD, Leurgans SE, Hebert LE, Scherr PA, Yaffe K, Bennett DA (2014) Contribution of Alzheimer disease to mortality in the United States. Neurology 82, 1045–1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [93].Mungas D, Tractenberg R, Schneider JA, Crane PK, Bennett DA (2014) A 2-process model for neuropathology of Alzheimer’s disease. Neurobiol Aging 35, 301–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [94].Crystal HA, Schneider JA, Bennett DA, Leurgans S, Levine SR (2014) Associations of cerebrovascular and Alzheimer’s disease pathology with brain atrophy. Curr Alzheimer Res 11, 309–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [95].Wilson RS, Segawa E, Boyle PA, Anagnos SE, Hizel LP, Bennett DA (2012) The natural history of cognitive decline in Alzheimer’s disease. Psychol Aging 27, 1008–1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [96].Nag S, Yu L, Capuano AW, Wilson RS, Leurgans SE, Bennett DA, Schneider JA (2015) Hippocampal sclerosis and TDP-43 pathology in aging and Alzheimer disease. Ann Neurol 77, 942–952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [97].Boyle PA, Yu L, Nag S, Leurgans S, Wilson RS, Bennett DA, Schneider JA (2015) Cerebral amyloid angiopathy and cognitive outcomes in community-based older persons. Neurology 85, 1930–1936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [98].Arvanitakis Z, Capuano AW, Leurgans SE, Buchman AS, Bennett DA, Schneider JA (2017) The Relationship of Cerebral Vessel Pathology to Brain Microinfarcts. Brain Pathol 27, 77–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [99].Arvanitakis Z, Capuano AW, Leurgans SE, Bennett DA, Schneider JA (2016) Relation of cerebral vessel disease to Alzheimer’s disease dementia and cognitive function in elderly people: a cross-sectional study. Lancet Neurol 15, 934–943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [100].James BD, Wilson RS, Boyle PA, Trojanowski JQ, Bennett DA, Schneider JA (2016) TDP-43 stage, mixed pathologies, and clinical Alzheimer’s-type dementia. Brain 139, 2983–2993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [101].Nag S, Yu L, Wilson RS, Chen EY, Bennett DA, Schneider JA (2017) TDP-43 pathology and memory impairment in elders without pathologic diagnoses of AD or FTLD. Neurology 88, 653–660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [102].James BD, Bennett DA, Boyle PA, Leurgans S, Schneider JA (2012) Dementia from Alzheimer disease and mixed pathologies in the oldest old. Jama 307, 1798–1800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [103].Fleischman DA, Leurgans S, Arfanakis K, Arvanitakis Z, Barnes LL, Boyle PA, Han SD, Bennett DA (2014) Gray-matter macrostructure in cognitively healthy older persons: associations with age and cognition. Brain Struct Funct 219, 2029–2049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [104].Arvanitakis Z, Fleischman DA, Arfanakis K, Leurgans SE, Barnes LL, Bennett DA (2016) Association of white matter hyperintensities and gray matter volume with cognition in older individuals without cognitive impairment. Brain Struct Funct 221, 2135–2146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [105].Dawe RJ, Yu L, Leurgans SE, Schneider JA, Buchman AS, Arfanakis K, Bennett DA, Boyle PA (2016) Postmortem MRI: a novel window into the neurobiology of late life cognitive decline. Neurobiol Aging 45, 169–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [106].Yu L, Dawe RJ, Buchman AS, Boyle PA, Schneider JA, Arfanakis K, Bennett DA (2017) Ex vivo MRI transverse relaxation in community based older persons with and without Alzheimer’s dementia. Behav Brain Res 322, 233–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [107].Dawe RJ, Bennett DA, Schneider JA, Leurgans SE, Kotrotsou A, Boyle PA, Arfanakis K (2014) Ex vivo T2 relaxation: associations with age-related neuropathology and cognition. Neurobiol Aging 35, 1549–1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [108].Kotrotsou A, Schneider JA, Bennett DA, Leurgans SE, Dawe RJ, Boyle PA, Golak T, Arfanakis K (2015) Neuropathologic correlates of regional brain volumes in a community cohort of older adults. Neurobiol Aging 36, 2798–2805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [109].Kotrotsou A, Bennett DA, Schneider JA, Dawe RJ, Golak T, Leurgans SE, Yu L, Arfanakis K (2014) Ex vivo MR volumetry of human brain hemispheres. Magn Reson Med 71, 364–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [110].Evia AM, Kotrotsou A, Tamhane AA, Dawe RJ, Kapasi A, Leurgans SE, Schneider JA, Bennett DA, Arfanakis K (2017) Ex-vivo quantitative susceptibility mapping of human brain hemispheres. PLoS One 12, e0188395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [111].Bennett DA, Wilson RS, Boyle PA, Buchman AS, Schneider JA (2012) Relation of neuropathology to cognition in persons without cognitive impairment. Ann Neurol 72, 599–609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [112].Yang FM, Grigorenko A, Tommet D, Farias ST, Mungas D, Bennett DA, Jones RN, Crane PK (2013) AD pathology and cerebral infarctions are associated with memory and executive functioning one and five years before death. J Clin Exp Neuropsychol 35, 24–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [113].Schneider JA, Arvanitakis Z, Yu L, Boyle PA, Leurgans SE, Bennett DA (2012) Cognitive impairment, decline and fluctuations in older community-dwelling subjects with Lewy bodies. Brain 135, 3005–3014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [114].Wilson RS, Boyle PA, Yu L, Barnes LL, Sytsma J, Buchman AS, Bennett DA, Schneider JA (2015) Temporal course and pathologic basis of unawareness of memory loss in dementia. Neurology 85, 984–991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [115].Wilson RS, Capuano AW, Bennett DA, Schneider JA, Boyle PA (2016) Temporal course of neurodegenerative effects on cognition in old age. Neuropsychology 30, 591–599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [116].Capuano AW, Wilson RS, Leurgans SE, Dawson JD, Bennett DA, Hedeker D (2016) Sigmoidal mixed models for longitudinal data. Stat Methods Med Res. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [117].Boyle PA, Yu L, Fleischman DA, Leurgans S, Yang J, Wilson RS, Schneider JA, Arvanitakis Z, Arfanakis K, Bennett DA (2016) White matter hyperintensities, incident mild cognitive impairment, and cognitive decline in old age. Ann Clin Transl Neurol 3, 791–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [118].Boyle PA, Yang J, Yu L, Leurgans SE, Capuano AW, Schneider JA, Wilson RS, Bennett DA (2017) Varied effects of age-related neuropathologies on the trajectory of late life cognitive decline. Brain 140, 804–812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [119].Jansen WJ, Wilson RS, Visser PJ, Nag S, Schneider JA, James BD, Leurgans SE, Capuano AW, Bennett DA, Boyle PA (2018) Age and the association of dementia-related pathology with trajectories of cognitive decline. Neurobiol Aging 61, 138–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [120].Fleischman DA, Yu L, Arfanakis K, Han SD, Barnes LL, Arvanitakis Z, Boyle PA, Bennett DA (2013) Faster cognitive decline in the years prior to MR imaging is associated with smaller hippocampal volumes in cognitively healthy older persons. Front Aging Neurosci 5, 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [121].Yu L, Boyle PA, Leurgans S, Schneider JA, Kryscio RJ, Wilson RS, Bennett DA (2015) Effect of common neuropathologies on progression of late life cognitive impairment. Neurobiol Aging 36, 2225–2231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [122].Boyle PA, Yu L, Wilson RS, Leurgans SE, Schneider JA, Bennett DA (2017) Person-specific contribution of neuropathologies to cognitive loss in old age. Ann Neurol. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [123].Wang D, Schultz T, Novak GP, Baker S, Bennett DA, Narayan VA (in press). Longitudinal Modeling of Functional Decline associated with pathologic Alzheimer’s disease in older persons without cognitive impairment. JAD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [124].Boyle PA, Yu L, Wilson RS, Schneider JA, Bennett DA (2013) Relation of neuropathology with cognitive decline among older persons without dementia. Front Aging Neurosci 5, 50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [125].Boyle PA, Wilson RS, Yu L, Barr AM, Honer WG, Schneider JA, Bennett DA (2013) Much of late life cognitive decline is not due to common neurodegenerative pathologies. Ann Neurol 74, 478–489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [126].Sadleir KR, Bennett DA, Schneider JA, Vassar R (2013) Elevated Abeta42 in aged, non-demented individuals with cerebral atherosclerosis. Curr Alzheimer Res 10, 785–789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [127].Tremblay C, Francois A, Delay C, Freland L, Vandal M, Bennett DA, Calon F (2017) Association of Neuropathological Markers in the Parietal Cortex With Antemortem Cognitive Function in Persons With Mild Cognitive Impairment and Alzheimer Disease. J Neuropathol Exp Neurol. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [128].Larson ME, Sherman MA, Greimel S, Kuskowski M, Schneider JA, Bennett DA, Lesne SE (2012) Soluble alpha-synuclein is a novel modulator of Alzheimer’s disease pathophysiology. J Neurosci 32, 10253–10266. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- [129].Larson M, Sherman MA, Amar F, Nuvolone M, Schneider JA, Bennett DA, Aguzzi A, Lesne SE (2012) The complex PrP(c)-Fyn couples human oligomeric Abeta with pathological tau changes in Alzheimer’s disease. J Neurosci 32, 16857–16871a. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- [130].Lesne SE, Sherman MA, Grant M, Kuskowski M, Schneider JA, Bennett DA, Ashe KH (2013) Brain amyloid-beta oligomers in ageing and Alzheimer’s disease. Brain 136, 1383–1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [131].Sherman MA, LaCroix M, Amar F, Larson ME, Forster C, Aguzzi A, Bennett DA, Ramsden M, Lesne SE (2016) Soluble Conformers of Abeta and Tau Alter Selective Proteins Governing Axonal Transport. J Neurosci 36, 9647–9658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [132].Yu L, Boyle PA, Segawa E, Leurgans S, Schneider JA, Wilson RS, Bennett DA (2015) Residual decline in cognition after adjustment for common neuropathologic conditions. Neuropsychology 29, 335–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [133].Arnold SE, Louneva N, Cao K, Wang LS, Han LY, Wolk DA, Negash S, Leurgans SE, Schneider JA, Buchman AS, Wilson RS, Bennett DA (2013) Cellular, synaptic, and biochemical features of resilient cognition in Alzheimer’s disease. Neurobiol Aging 34, 157–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [134].Wilson RS, Nag S, Boyle PA, Hizel LP, Yu L, Buchman AS, Schneider JA, Bennett DA (2013) Neural reserve, neuronal density in the locus ceruleus, and cognitive decline. Neurology 80, 1202–1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [135].Ramos-Miguel A, Hercher C, Beasley CL, Barr AM, Bayer TA, Falkai P, Leurgans SE, Schneider JA, Bennett DA, Honer WG (2015) Loss of Munc18–1 long splice variant in GABAergic terminals is associated with cognitive decline and increased risk of dementia in a community sample. Mol Neurodegener 10, 65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [136].Buchman AS, Yu L, Boyle PA, Schneider JA, De Jager PL, Bennett DA (2016) Higher brain BDNF gene expression is associated with slower cognitive decline in older adults. Neurology 86, 735–741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [137].Ramos-Miguel A, Sawada K, Jones AA, Thornton AE, Barr AM, Leurgans SE, Schneider JA, Bennett DA, Honer WG (2017) Presynaptic proteins complexin-I and complexin-II differentially influence cognitive function in early and late stages of Alzheimer’s disease. Acta Neuropathol 133, 395–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [138].Mostafavi S, Gaiteri C, Sullivan S, White C, Takasi S, Xu J, Taga M, Klein H, Patrick E, Komashko V, McCable C, Smith R, Bradshaw E, Root D, Yu L, Regev A, Chibnik L, Schneider J, Young-Pearse T, Bennett D, De Jager P, A molecular network of the aging brain implicates INPPL1 and PLXNB1 in Alzheimer’s disease, https://www.biorxiv.org/content/early/2017/10/19/205807,
- [139].Wilson RS, Capuano AW, Sytsma J, Bennett DA, Barnes LL (2015) Cognitive aging in older Black and White persons. Psychol Aging 30, 279–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [140].Wilson RS, Capuano AW, Marquez DX, Amofa P, Barnes LL, Bennett DA (2016) Change in Cognitive Abilities in Older Latinos. J Int Neuropsychol Soc 22, 58–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [141].Barnes LL, Yumoto F, Capuano A, Wilson RS, Bennett DA, Tractenberg RE (2016) Examination of the Factor Structure of a Global Cognitive Function Battery across Race and Time. J Int Neuropsychol Soc 22, 66–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [142].Yu L, Boyle P, Wilson RS, Segawa E, Leurgans S, De Jager PL, Bennett DA (2012) A random change point model for cognitive decline in Alzheimer’s disease and mild cognitive impairment. Neuroepidemiology 39, 73–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [143].Valant V, Keenan BT, Anderson CD, Shulman JM, Devan WJ, Ayres AM, Schwab K, Goldstein JN, Viswanathan A, Greenberg SM, Bennett DA, De Jager PL, Rosand J, Biffi A (2012) TOMM40 in Cerebral Amyloid Angiopathy Related Intracerebral Hemorrhage: Comparative Genetic Analysis with Alzheimer’s Disease. Transl Stroke Res 3, 102–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [144].Yu L, Lutz MW, Wilson RS, Burns DK, Roses AD, Saunders AM, Yang J, Gaiteri C, De Jager PL, Barnes LL, Bennett DA (2017) APOE epsilon4-TOMM40 ‘523 haplotypes and the risk of Alzheimer’s disease in older Caucasian and African Americans. PLoS One 12, e0180356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [145].Yu L, Lutz MW, Wilson RS, Burns DK, Roses AD, Saunders AM, Gaiteri C, De Jager PL, Barnes LL, Bennett DA (2017) TOMM40’523 variant and cognitive decline in older persons with APOE epsilon3/3 genotype. Neurology 88, 661–668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [146].Yu L, Lutz MW, Farfel JM, Wilson RS, Burns DK, Saunders AM, De Jager PL, Barnes LL, Schneider JA, Bennett DA (2017) Neuropathologic features of TOMM40 ‘523 variant on late-life cognitive decline. Alzheimers Dement 13, 1380–1388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [147].Barnes LL, Arvanitakis Z, Yu L, Kelly J, De Jager PL, Bennett DA (2013) Apolipoprotein E and change in episodic memory in blacks and whites. Neuroepidemiology 40, 211–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [148].Yu L, Boyle P, Schneider JA, Segawa E, Wilson RS, Leurgans S, Bennett DA (2013) APOE epsilon4, Alzheimer’s disease pathology, cerebrovascular disease, and cognitive change over the years prior to death. Psychol Aging 28, 1015–1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [149].Yu L, Boyle PA, Nag S, Leurgans S, Buchman AS, Wilson RS, Arvanitakis Z, Farfel JM, De Jager PL, Bennett DA, Schneider JA (2015) APOE and cerebral amyloid angiopathy in community-dwelling older persons. Neurobiol Aging 36, 2946–2953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [150].Yu L, Boyle PA, Leurgans S, Schneider JA, Bennett DA (2014) Disentangling the effects of age and APOE on neuropathology and late life cognitive decline. Neurobiol Aging 35, 819–826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [151].Farfel JM, Yu L, De Jager PL, Schneider JA, Bennett DA (2016) Association of APOE with tau-tangle pathology with and without beta-amyloid. Neurobiol Aging 37, 19–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [152].Lambert JC, Ibrahim-Verbaas CA, Harold D, Naj AC, Sims R, Bellenguez C, DeStafano AL, Bis JC, Beecham GW, Grenier-Boley B, Russo G, Thorton-Wells TA, Jones N, Smith AV, Chouraki V, Thomas C, Ikram MA, Zelenika D, Vardarajan BN, Kamatani Y, Lin CF, Gerrish A, Schmidt H, Kunkle B, Dunstan ML, Ruiz A, Bihoreau MT, Choi SH, Reitz C, Pasquier F, Cruchaga C, Craig D, Amin N, Berr C, Lopez OL, De Jager PL, Deramecourt V, Johnston JA, Evans D, Lovestone S, Letenneur L, Moron FJ, Rubinsztein DC, Eiriksdottir G, Sleegers K, Goate AM, Fievet N, Huentelman MW, Gill M, Brown K, Kamboh MI, Keller L, Barberger-Gateau P, McGuiness B, Larson EB, Green R, Myers AJ, Dufouil C, Todd S, Wallon D, Love S, Rogaeva E, Gallacher J, St George-Hyslop P, Clarimon J, Lleo A, Bayer A, Tsuang DW, Yu L, Tsolaki M, Bossu P, Spalletta G, Proitsi P, Collinge J, Sorbi S, Sanchez-Garcia F, Fox NC, Hardy J, Deniz Naranjo MC, Bosco P, Clarke R, Brayne C, Galimberti D, Mancuso M, Matthews F, Moebus S, Mecocci P, Del Zompo M, Maier W, Hampel H, Pilotto A, Bullido M, Panza F, Caffarra P, Nacmias B, Gilbert JR, Mayhaus M, Lannefelt L, Hakonarson H, Pichler S, Carrasquillo MM, Ingelsson M, Beekly D, Alvarez V, Zou F, Valladares O, Younkin SG, Coto E, Hamilton-Nelson KL, Gu W, Razquin C, Pastor P, Mateo I, Owen MJ, Faber KM, Jonsson PV, Combarros O, O’Donovan MC, Cantwell LB, Soininen H, Blacker D, Mead S, Mosley TH Jr., Bennett DA, Harris TB, Fratiglioni L, Holmes C, de Bruijn RF, Passmore P, Montine TJ, Bettens K, Rotter JI, Brice A, Morgan K, Foroud TM, Kukull WA, Hannequin D, Powell JF, Nalls MA, Ritchie K, Lunetta KL, Kauwe JS, Boerwinkle E, Riemenschneider M, Boada M, Hiltuenen M, Martin ER, Schmidt R, Rujescu D, Wang LS, Dartigues JF, Mayeux R, Tzourio C, Hofman A, Nothen MM, Graff C, Psaty BM, Jones L, Haines JL, Holmans PA, Lathrop M, Pericak-Vance MA, Launer LJ, Farrer LA, van Duijn CM, Van Broeckhoven C, Moskvina V, Seshadri S, Williams J, Schellenberg GD, Amouyel P (2013) Meta-analysis of 74,046 individuals identifies 11 new susceptibility loci for Alzheimer’s disease. Nat Genet 45, 1452–1458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [153].Keenan BT, Shulman JM, Chibnik LB, Raj T, Tran D, Sabuncu MR, Allen AN, Corneveaux JJ, Hardy JA, Huentelman MJ, Lemere CA, Myers AJ, Nicholson-Weller A, Reiman EM, Evans DA, Bennett DA, De Jager PL (2012) A coding variant in CR1 interacts with APOE-epsilon4 to influence cognitive decline. Hum Mol Genet 21, 2377–2388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [154].Biffi A, Shulman JM, Jagiella JM, Cortellini L, Ayres AM, Schwab K, Brown DL, Silliman SL, Selim M, Worrall BB, Meschia JF, Slowik A, De Jager PL, Greenberg SM, Schneider JA, Bennett DA, Rosand J (2012) Genetic variation at CR1 increases risk of cerebral amyloid angiopathy. Neurology 78, 334–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [155].Felsky D, Szeszko P, Yu L, Honer WG, De Jager PL, Schneider JA, Malhotra AK, Lencz T, Ikuta T, Pipitone J, Chakravarty MM, Lobaugh NJ, Mulsant BH, Pollock BG, Kennedy JL, Bennett DA, Voineskos AN (2014) The SORL1 gene and convergent neural risk for Alzheimer’s disease across the human lifespan. Mol Psychiatry 19, 1125–1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [156].Bradshaw EM, Chibnik LB, Keenan BT, Ottoboni L, Raj T, Tang A, Rosenkrantz LL, Imboywa S, Lee M, Von Korff A, Morris MC, Evans DA, Johnson K, Sperling RA, Schneider JA, Bennett DA, De Jager PL (2013) CD33 Alzheimer’s disease locus: altered monocyte function and amyloid biology. Nat Neurosci 16, 848–850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [157].Raj T, Ryan KJ, Replogle JM, Chibnik LB, Rosenkrantz L, Tang A, Rothamel K, Stranger BE, Bennett DA, Evans DA, De Jager PL, Bradshaw EM (2014) CD33: increased inclusion of exon 2 implicates the Ig V-set domain in Alzheimer’s disease susceptibility. Hum Mol Genet 23, 2729–2736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [158].Chan G, White CC, Winn PA, Cimpean M, Replogle JM, Glick LR, Cuerdon NE, Ryan KJ, Johnson KA, Schneider JA, Bennett DA, Chibnik LB, Sperling RA, Bradshaw EM, De Jager PL (2015) CD33 modulates TREM2: convergence of Alzheimer loci. Nat Neurosci 18, 1556–1558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [159].Raj T, Shulman JM, Keenan BT, Chibnik LB, Evans DA, Bennett DA, Stranger BE, De Jager PL (2012) Alzheimer disease susceptibility loci: evidence for a protein network under natural selection. Am J Hum Genet 90, 720–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [160].Farfel JM, Yu L, Buchman AS, Schneider JA, De Jager PL, Bennett DA (2016) Relation of genomic variants for Alzheimer disease dementia to common neuropathologies. Neurology 87, 489–496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [161].Yu L, Chibnik LB, Srivastava GP, Pochet N, Yang J, Xu J, Kozubek J, Obholzer N, Leurgans SE, Schneider JA, Meissner A, De Jager PL, Bennett DA (2015) Association of Brain DNA methylation in SORL1, ABCA7, HLA-DRB5, SLC24A4, and BIN1 with pathological diagnosis of Alzheimer disease. JAMA Neurol 72, 15–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [162].Chibnik LB, Yu L, Eaton ML, Srivastava G, Schneider JA, Kellis M, Bennett DA, De Jager PL (2015) Alzheimer’s loci: epigenetic associations and interaction with genetic factors. Ann Clin Transl Neurol 2, 636–647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [163].Benedet AL, Yu L, Labbe A, Mathotaarachchi S, Pascoal TA, Shin M, Kang MS, Gauthier S, Rouleau GA, Poirier J, Bennett DA, Rosa-Neto P (2018) CYP2C19 variant mitigates Alzheimer s disease pathophysiology in vivo & post mortem. Neurology Genetics In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [164].Yu L, Shulman JM, Chibnik L, Leurgans S, Schneider JA, De Jager PL, Bennett DA (2012) The CETP I405V polymorphism is associated with an increased risk of Alzheimer’s disease. Aging Cell 11, 228–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [165].Replogle JM, Chan G, White CC, Raj T, Winn PA, Evans DA, Sperling RA, Chibnik LB, Bradshaw EM, Schneider JA, Bennett DA, De Jager PL (2015) A TREM1 variant alters the accumulation of Alzheimer-related amyloid pathology. Ann Neurol 77, 469–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [166].Hohman TJ, Chibnik L, Bush WS, Jefferson AL, De Jaeger PL, Thornton-Wells TA, Bennett DA, Schneider JA (2015) GSK3beta Interactions with Amyloid Genes: An Autopsy Verification and Extension. Neurotox Res 28, 232–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [167].Chou SY, Shulman JM, Keenan BT, Secor EA, Buchman AS, Schneider J, Bennett DA, De Jager PL (2013) Genetic susceptibility for ischemic infarction and arteriolosclerosis based on neuropathologic evaluations. Cerebrovasc Dis 36, 181–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [168].Barral S, Habeck C, Gazes E, De Jager PL, Bennett DA, Stern Y (2017) A Dopamine Receptor genetic variant enhances perceptual speed in cognitive healthy subjects. Alzheimers Dement (N Y) 3, 254–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [169].Chibnik LB, White CC, Mukherjee S, Raj T, Yu L, Larson EB, Montine TJ, Keene CD, Sonnen J, Schneider JA, Crane PK, Shulman JM, Bennett DA, De Jager PL (2017) Susceptibility to neurofibrillary tangles: role of the PTPRD locus and limited pleiotropy with other neuropathologies. Mol Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [170].Dubal DB, Yokoyama JS, Zhu L, Broestl L, Worden K, Wang D, Sturm VE, Kim D, Klein E, Yu GQ, Ho K, Eilertson KE, Yu L, Kuro-o M, De Jager PL, Coppola G, Small GW, Bennett DA, Kramer JH, Abraham CR, Miller BL, Mucke L (2014) Life extension factor klotho enhances cognition. Cell Rep 7, 1065–1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [171].Yokoyama JS, Sturm VE, Bonham LW, Klein E, Arfanakis K, Yu L, Coppola G, Kramer JH, Bennett DA, Miller BL, Dubal DB (2015) Variation in longevity gene KLOTHO is associated with greater cortical volumes. Ann Clin Transl Neurol 2, 215–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [172].White CC, Yang HS, Yu L, Chibnik LB, Dawe RJ, Yang J, Klein HU, Felsky D, Ramos-Miguel A, Arfanakis K, Honer WG, Sperling RA, Schneider JA, Bennett DA, De Jager PL (2017) Identification of genes associated with dissociation of cognitive performance and neuropathological burden: Multistep analysis of genetic, epigenetic, and transcriptional data. PLoS Med 14, e1002287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [173].Yang HS, White CC, Chibnik LB, Klein HU, Schneider JA, Bennett DA, De Jager PL (2017) UNC5C variants are associated with cerebral amyloid angiopathy. Neurol Genet 3, e176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [174].Hall DA, Bennett DA, Filley CM, Shah RC, Kluger B, Ouyang B, Berry-Kravis E (2014) Fragile X gene expansions are not associated with dementia. Neurobiol Aging 35, 2637–2638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [175].Shulman JM, Chen K, Keenan BT, Chibnik LB, Fleisher A, Thiyyagura P, Roontiva A, McCabe C, Patsopoulos NA, Corneveaux JJ, Yu L, Huentelman MJ, Evans DA, Schneider JA, Reiman EM, De Jager PL, Bennett DA (2013) Genetic susceptibility for Alzheimer disease neuritic plaque pathology. JAMA Neurol 70, 1150–1157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [176].Roostaei T, Nazeri A, Felsky D, De Jager PL, Schneider JA, Pollock BG, Bennett DA, Voineskos AN (2017) Genome-wide interaction study of brain beta-amyloid burden and cognitive impairment in Alzheimer’s disease. Mol Psychiatry 22, 287–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [177].Yu L, De Jager PL, Yang J, Trojanowski JQ, Bennett DA, Schneider JA (2015) The TMEM106B locus and TDP-43 pathology in older persons without FTLD. Neurology 84, 927–934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [178].Wilson RS, Boyle PA, Yang J, James BD, Bennett DA (2015) Early life instruction in foreign language and music and incidence of mild cognitive impairment. Neuropsychology 29, 292–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [179].Marquine MJ, Segawa E, Wilson RS, Bennett DA, Barnes LL (2012) Association between cognitive activity and cognitive function in older Hispanics. J Int Neuropsychol Soc 18, 1041–1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [180].Wilson RS, Segawa E, Boyle PA, Bennett DA (2012) Influence of late-life cognitive activity on cognitive health. Neurology 78, 1123–1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [181].Wilson RS, Boyle PA, Yu L, Barnes LL, Schneider JA, Bennett DA (2013) Life-span cognitive activity, neuropathologic burden, and cognitive aging. Neurology 81, 314–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [182].Arfanakis K, Wilson RS, Barth CM, Capuano AW, Vasireddi A, Zhang S, Fleischman DA, Bennett DA (2016) Cognitive activity, cognitive function, and brain diffusion characteristics in old age. Brain Imaging Behav 10, 455–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [183].Buchman AS, Boyle PA, Yu L, Shah RC, Wilson RS, Bennett DA (2012) Total daily physical activity and the risk of AD and cognitive decline in older adults. Neurology 78, 1323–1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [184].Wilson RS, Boyle PA, James BD, Leurgans SE, Buchman AS, Bennett DA (2015) Negative social interactions and risk of mild cognitive impairment in old age. Neuropsychology 29, 561–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [185].Tangney CC, Li H, Wang Y, Barnes L, Schneider JA, Bennett DA, Morris MC (2014) Relation of DASH- and Mediterranean-like dietary patterns to cognitive decline in older persons. Neurology 83, 1410–1416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [186].Morris MC, Tangney CC, Wang Y, Sacks FM, Bennett DA, Aggarwal NT (2015) MIND diet associated with reduced incidence of Alzheimer’s disease. Alzheimers Dement 11, 1007–1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [187].Morris MC, Tangney CC, Wang Y, Sacks FM, Barnes LL, Bennett DA, Aggarwal NT (2015) MIND diet slows cognitive decline with aging. Alzheimers Dement 11, 1015–1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [188].Morris MC, Wang Y, Barnes LL, Bennett DA, Dawson-Hughes B, Booth SL (2017) Nutrients and bioactives in green leafy vegetables and cognitive decline: Prospective study. Neurology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [189].van de Rest O, Wang Y, Barnes LL, Tangney C, Bennett DA, Morris MC (2016) APOE epsilon4 and the associations of seafood and long-chain omega-3 fatty acids with cognitive decline. Neurology 86, 2063–2070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [190].Samieri C, Morris MC, Bennett DA, Berr C, Amouyel P, Dartigues JF, Tzourio C, Chasman DI, Grodstein F (2017) Fish intake, genetic predisposition to alzheimer’s disease and decline in global cognition and memory in five cohorts of older persons. Am J Epidemiol. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [191].Cunnane SC, Schneider JA, Tangney C, Tremblay-Mercier J, Fortier M, Bennett DA, Morris MC (2012) Plasma and brain fatty acid profiles in mild cognitive impairment and Alzheimer’s disease. J Alzheimers Dis 29, 691–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [192].Morris MC, Brockman J, Schneider JA, Wang Y, Bennett DA, Tangney CC, van de Rest O (2016) Association of Seafood Consumption, Brain Mercury Level, and APOE epsilon4 Status With Brain Neuropathology in Older Adults. Jama 315, 489–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [193].Morris MC, Schneider JA, Li H, Tangney CC, Nag S, Bennett DA, Honer WG, Barnes LL (2015) Brain tocopherols related to Alzheimer’s disease neuropathology in humans. Alzheimers Dement 11, 32–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [194].Wilson RS, Capuano AW, Boyle PA, Hoganson GM, Hizel LP, Shah RC, Nag S, Schneider JA, Arnold SE, Bennett DA (2014) Clinical-pathologic study of depressive symptoms and cognitive decline in old age. Neurology 83, 702–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [195].Wilson RS, Boyle PA, Capuano AW, Shah RC, Hoganson GM, Nag S, Bennett DA (2016) Late-life depression is not associated with dementia-related pathology. Neuropsychology 30, 135–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [196].Wilson RS, Nag S, Boyle PA, Hizel LP, Yu L, Buchman AS, Shah RC, Schneider JA, Arnold SE, Bennett DA (2013) Brainstem aminergic nuclei and late-life depressive symptoms. JAMA Psychiatry 70, 1320–1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [197].Wilson RS, Beckett LA, Bienias JL, Evans DA, Bennett DA (2003) Terminal decline in cognitive function. Neurology 60, 1782–1787. [DOI] [PubMed] [Google Scholar]
- [198].Wilson RS, Beck TL, Bienias JL, Bennett DA (2007) Terminal cognitive decline: accelerated loss of cognition in the last years of life. Psychosom Med 69, 131–137. [DOI] [PubMed] [Google Scholar]
- [199].Wilson RS, Boyle PA, Yu L, Segawa E, Sytsma J, Bennett DA (2015) Conscientiousness, dementia related pathology, and trajectories of cognitive aging. Psychol Aging 30, 74–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [200].Wilson RS, Boyle PA, Segawa E, Yu L, Begeny CT, Anagnos SE, Bennett DA (2013) The influence of cognitive decline on well-being in old age. Psychol Aging 28, 304–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [201].Boyle PA, Buchman AS, Wilson RS, Yu L, Schneider JA, Bennett DA (2012) Effect of purpose in life on the relation between Alzheimer disease pathologic changes on cognitive function in advanced age. Arch Gen Psychiatry 69, 499–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [202].Yu L, Boyle PA, Wilson RS, Levine SR, Schneider JA, Bennett DA (2015) Purpose in life and cerebral infarcts in community-dwelling older people. Stroke 46, 1071–1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [203].Wilson RS, Capuano AW, James BD, Amofa P, Arvanitakis Z, Shah R, Bennett DA, Boyle PA (2017) Purpose in Life and Hospitalization for Ambulatory Care-Sensitive Conditions in Old Age. Am J Geriatr Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [204].Wilson RS, Boyle PA, Levine SR, Yu L, Anagnos SE, Buchman AS, Schneider JA, Bennett DA (2012) Emotional neglect in childhood and cerebral infarction in older age. Neurology 79, 1534–1539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [205].Wilson RS, Boyle PA, Levine SR, Yu L, Hoganson GM, Buchman AS, Schneider JA, Bennett DA (2014) Harm avoidance and cerebral infarction. Neuropsychology 28, 305–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [206].Gaynes BI, Shah R, Leurgans S, Bennett D (2013) Neuroticism modifies the association of vision impairment and cognition among community-dwelling older adults. Neuroepidemiology 40, 142–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [207].Canli T, Yu L, Yu X, Zhao H, Fleischman D, Wilson RS, De Jager PL, Bennett DA (2018) Loneliness five years ante-mortem is associated with disease-related differential gene expression in postmortem dorsolateral prefrontal cortex. Translational Psychiatry In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [208].Canli T, Wen R, Wang X, Mikhailik A, Yu L, Fleischman D, Wilson RS, Bennett DA (2017) Differential transcriptome expression in human nucleus accumbens as a function of loneliness. Mol Psychiatry 22, 1069–1078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [209].Arvanitakis Z, Capuano AW, Bennett DA, Barnes LL (2017) Body mass index and decline in cognitive function in older black and white persons. J Gerontol A Biol Sci Med Sci. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [210].Shah RC, Schneider JA, Leurgans S, Bennett DA (2012) Association of lower hemoglobin level and neuropathology in community-dwelling older persons. J Alzheimers Dis 32, 579–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [211].Arvanitakis Z, Brey RL, Rand JH, Schneider JA, Capuano AW, Yu L, Leurgans SE, Bennett DA, Levine SR (2015) Relation of antiphospholipid antibodies to postmortem brain infarcts in older people. Circulation 131, 182–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [212].Roostaei T, Felsky D, Nazeri A, De Jager PL, Schneider JA, Bennett DA, Voineskos AN (2018) Genetic influence of plasma homocysteine on Alzheimer’s disease. Neurobiol Aging 62, 243.e247–243.e214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [213].Pruzin JJ, Schneider JA, Capuano AW, Leurgans SE, Barnes LL, Ahima RS, Arnold SE, Bennett DA, Arvanitakis Z (2017) Diabetes, Hemoglobin A1C, and Regional Alzheimer Disease and Infarct Pathology. Alzheimer Dis Assoc Disord 31, 41–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [214].Talbot K, Wang HY, Kazi H, Han LY, Bakshi KP, Stucky A, Fuino RL, Kawaguchi KR, Samoyedny AJ, Wilson RS, Arvanitakis Z, Schneider JA, Wolf BA, Bennett DA, Trojanowski JQ, Arnold SE (2012) Demonstrated brain insulin resistance in Alzheimer’s disease patients is associated with IGF-1 resistance, IRS-1 dysregulation, and cognitive decline. J Clin Invest 122, 1316–1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [215].Shah RC, Janos AL, Kline JE, Yu L, Leurgans SE, Wilson RS, Wei P, Bennett DA, Heilman KM, Tsao JW (2013) Cognitive decline in older persons initiating anticholinergic medications. PLoS One 8, e64111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [216].Barnes LL, Capuano AW, Aiello AE, Turner AD, Yolken RH, Torrey EF, Bennett DA (2015) Cytomegalovirus infection and risk of Alzheimer disease in older black and white individuals. J Infect Dis 211, 230–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [217].Lurain NS, Hanson BA, Martinson J, Leurgans SE, Landay AL, Bennett DA, Schneider JA (2013) Virological and immunological characteristics of human cytomegalovirus infection associated with Alzheimer disease. J Infect Dis 208, 564–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [218].Sivam A, Wroblewski KE, Alkorta-Aranburu G, Barnes LL, Wilson RS, Bennett DA, Pinto JM (2016) Olfactory Dysfunction in Older Adults is Associated with Feelings of Depression and Loneliness. Chem Senses 41, 293–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [219].Foveau B, Albrecht S, Bennett DA, Correa JA, LeBlanc AC (2016) Increased Caspase-6 activity in the human anterior olfactory nuclei of the olfactory bulb is associated with cognitive impairment. Acta Neuropathol Commun 4, 127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [220].Bove R, Secor E, Chibnik LB, Barnes LL, Schneider JA, Bennett DA, De Jager PL (2014) Age at surgical menopause influences cognitive decline and Alzheimer pathology in older women. Neurology 82, 222–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [221].Yarchoan M, James BD, Shah RC, Arvanitakis Z, Wilson RS, Schneider J, Bennett DA, Arnold SE (2017) Association of Cancer History with Alzheimer’s Disease Dementia and Neuropathology. J Alzheimers Dis 56, 699–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [222].Arfanakis K, Fleischman DA, Grisot G, Barth CM, Varentsova A, Morris MC, Barnes LL, Bennett DA (2013) Systemic inflammation in non-demented elderly human subjects: brain microstructure and cognition. PLoS One 8, e73107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [223].Lim AS, Yu L, Costa MD, Leurgans SE, Buchman AS, Bennett DA, Saper CB (2012) Increased fragmentation of rest-activity patterns is associated with a characteristic pattern of cognitive impairment in older individuals. Sleep 35, 633–640b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [224].Lim AS, Kowgier M, Yu L, Buchman AS, Bennett DA (2013) Sleep Fragmentation and the Risk of Incident Alzheimer’s Disease and Cognitive Decline in Older Persons. Sleep 36, 1027–1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [225].Lim AS, Fleischman DA, Dawe RJ, Yu L, Arfanakis K, Buchman AS, Bennett DA (2016) Regional Neocortical Gray Matter Structure and Sleep Fragmentation in Older Adults. Sleep 39, 227–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [226].Lim AS, Yu L, Kowgier M, Schneider JA, Buchman AS, Bennett DA (2013) Modification of the relationship of the apolipoprotein E epsilon4 allele to the risk of Alzheimer disease and neurofibrillary tangle density by sleep. JAMA Neurol 70, 1544–1551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [227].Lim AS, Yu L, Schneider JA, Bennett DA, Buchman AS (2016) Sleep Fragmentation, Cerebral Arteriolosclerosis, and Brain Infarct Pathology in Community-Dwelling Older People. Stroke 47, 516–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [228].Sohail S, Yu L, Bennett DA, Buchman AS, Lim AS (2015) Irregular 24-hour activity rhythms and the metabolic syndrome in older adults. Chronobiol Int 32, 802–813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [229].Wang JL, Lim AS, Chiang WY, Hsieh WH, Lo MT, Schneider JA, Buchman AS, Bennett DA, Hu K, Saper CB (2015) Suprachiasmatic neuron numbers and rest-activity circadian rhythms in older humans. Ann Neurol 78, 317–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [230].Buchman AS, Yu L, Boyle PA, Shah RC, Bennett DA (2012) Total daily physical activity and longevity in old age. Arch Intern Med 172, 444–446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [231].Buchman AS, Wilson RS, Yu L, James BD, Boyle PA, Bennett DA (2014) Total daily activity declines more rapidly with increasing age in older adults. Arch Gerontol Geriatr 58, 74–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [232].James BD, Boyle PA, Bennett DA, Buchman AS (2012) Total daily activity measured with actigraphy and motor function in community-dwelling older persons with and without dementia. Alzheimer Dis Assoc Disord 26, 238–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [233].Shah RC, Buchman AS, Leurgans S, Boyle PA, Bennett DA (2012) Association of total daily physical activity with disability in community-dwelling older persons: a prospective cohort study. BMC Geriatr 12, 63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [234].Buchman AS, Wilson RS, Shulman JM, Leurgans SE, Schneider JA, Bennett DA (2016) Parkinsonism in Older Adults and Its Association With Adverse Health Outcomes and Neuropathology. J Gerontol A Biol Sci Med Sci 71, 549–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [235].Buchman AS, Shulman JM, Nag S, Leurgans SE, Arnold SE, Morris MC, Schneider JA, Bennett DA (2012) Nigral pathology and parkinsonian signs in elders without Parkinson disease. Ann Neurol 71, 258–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [236].Buchman AS, Yu L, Boyle PA, Levine SR, Nag S, Schneider JA, Bennett DA (2013) Microvascular brain pathology and late-life motor impairment. Neurology 80, 712–718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [237].Buchman AS, Yu L, Wilson RS, Schneider JA, Bennett DA (2013) Association of brain pathology with the progression of frailty in older adults. Neurology 80, 2055–2061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [238].Buchman AS, Yu L, Wilson RS, Dawe RJ, VanderHorst V, Schneider JA, Bennett DA (2015) Post-mortem brain pathology is related to declining respiratory function in community-dwelling older adults. Front Aging Neurosci 7, 197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [239].Buchman AS, Yu L, Wilson RS, Boyle PA, Schneider JA, Bennett DA (2014) Brain pathology contributes to simultaneous change in physical frailty and cognition in old age. J Gerontol A Biol Sci Med Sci 69, 1536–1544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [240].Buchman AS, Nag S, Shulman JM, Lim AS, VanderHorst VG, Leurgans SE, Schneider JA, Bennett DA (2012) Locus coeruleus neuron density and parkinsonism in older adults without Parkinson’s disease. Mov Disord 27, 1625–1631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [241].Shah RC, Maitra K, Barnes LL, James BD, Leurgans S, Bennett DA (2012) Relation of driving status to incident life space constriction in community-dwelling older persons: a prospective cohort study. J Gerontol A Biol Sci Med Sci 67, 984–989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [242].Buchman AS, Boyle PA, Wilson RS, Leurgans SE, Arnold SE, Bennett DA (2013) Neuroticism, extraversion, and motor function in community-dwelling older persons. Am J Geriatr Psychiatry 21, 145–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [243].Buchman AS, Yu L, Wilson RS, Shulman JM, Boyle PA, Bennett DA (2014) Harm avoidance is associated with progression of parkinsonism in community-dwelling older adults: a prospective cohort study. BMC Geriatr 14, 54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [244].Perlman A, Shah RC, Bennett DA, Buchman AS, Matok I (2016) Antihypertensive and Statin Medication Use and Motor Function in Community-Dwelling Older Adults. J Am Med Dir Assoc 17, 220–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [245].Crane PK, Gibbons LE, Dams-O’Connor K, Trittschuh E, Leverenz JB, Keene CD, Sonnen J, Montine TJ, Bennett DA, Leurgans S, Schneider JA, Larson EB (2016) Association of Traumatic Brain Injury With Late-Life Neurodegenerative Conditions and Neuropathologic Findings. JAMA Neurol 73, 1062–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [246].Park M, Buchman AS, Lim AS, Leurgans SE, Bennett DA (2014) Sleep complaints and incident disability in a community-based cohort study of older persons. Am J Geriatr Psychiatry 22, 718–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [247].Turner AD, Lim AS, Leurgans SE, Bennett DA, Buchman AS, Barnes LL (2016) Self-Reported Sleep in Older African Americans and White Americans. Ethn Dis 26, 521–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [248].Sohail S, Yu L, Schneider JA, Bennett DA, Buchman AS, Lim ASP (2017) Sleep fragmentation and Parkinson’s disease pathology in older adults without Parkinson’s disease. Mov Disord 32, 1729–1737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [249].Shulman JM, Yu L, Buchman AS, Evans DA, Schneider JA, Bennett DA, De Jager PL (2014) Association of Parkinson disease risk loci with mild parkinsonian signs in older persons. JAMA Neurol 71, 429–435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [250].Han SD, Buchman AS, Arfanakis K, Fleischman DA, Bennett DA (2013) Functional connectivity networks associated with chronic musculoskeletal pain in old age. Int J Geriatr Psychiatry 28, 858–867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [251].Fleischman DA, Yang J, Arfanakis K, Arvanitakis Z, Leurgans SE, Turner AD, Barnes LL, Bennett DA, Buchman AS (2015) Physical activity, motor function, and white matter hyperintensity burden in healthy older adults. Neurology 84, 1294–1300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [252].Boyle PA, Wilson RS, Yu L, Buchman AS, Bennett DA (2013) Poor decision making is associated with an increased risk of mortality among community-dwelling older persons without dementia. Neuroepidemiology 40, 247–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [253].Han SD, Boyle PA, James BD, Yu L, Barnes LL, Bennett DA (2016) Discrepancies between cognition and decision making in older adults. Aging Clin Exp Res 28, 99–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [254].Han SD, Boyle PA, James BD, Yu L, Bennett DA (2015) Mild cognitive impairment is associated with poorer decision-making in community-based older persons. J Am Geriatr Soc 63, 676–683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [255].Boyle PA, Yu L, Wilson RS, Gamble K, Buchman AS, Bennett DA (2012) Poor decision making is a consequence of cognitive decline among older persons without Alzheimer’s disease or mild cognitive impairment. PLoS One 7, e43647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [256].James BD, Boyle PA, Yu L, Bennett DA (2013) Internet use and decision making in community-based older adults. Front Psychol 4, 605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [257].Stewart CC, Yu C, Wilson RS, Bennett DA, Boyle PA (2018) Correlates of healthcare and financial decision making among older adults without dementia. Health Psychology in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [258].Bennett JS, Boyle PA, James BD, Bennett DA (2012) Correlates of health and financial literacy in older adults without dementia. BMC Geriatr 12, 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [259].Han SD, Boyle PA, James BD, Yu L, Bennett DA (2015) Poorer Financial and Health Literacy Among Community-Dwelling Older Adults With Mild Cognitive Impairment. J Aging Health 27, 1105–1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [260].Stewart CC, Boyle PA, James BD, Yu L, Han SD, Bennett DA (2016) Associations of APOE epsilon4 With Health and Financial Literacy Among Community-Based Older Adults Without Dementia. J Gerontol B Psychol Sci Soc Sci. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [261].Boyle PA, Yu L, Wilson RS, Segawa E, Buchman AS, Bennett DA (2013) Cognitive decline impairs financial and health literacy among community-based older persons without dementia. Psychol Aging 28, 614–624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [262].Wilson RS, Yu L, James BD, Bennett DA, Boyle PA (2017) Association of financial and health literacy with cognitive health in old age. Neuropsychol Dev Cogn B Aging Neuropsychol Cogn 24, 186–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [263].Yu L, Wilson RS, Han SD, Leurgans S, Bennett DA, Boyle PA (2017) Decline in Literacy and Incident AD Dementia Among Community-Dwelling Older Persons. J Aging Health, 898264317716361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [264].Yu L, Wilson RS, Schneider JA, Bennett DA, Boyle PA (2017) Financial and Health Literacy Predict Incident Alzheimer’s Disease Dementia and Pathology. J Alzheimers Dis 56, 1485–1493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [265].Han SD, Boyle PA, Arfanakis K, Fleischman D, Yu L, James BD, Bennett DA (2016) Financial literacy is associated with white matter integrity in old age. Neuroimage 130, 223–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [266].Han SD, Boyle PA, Yu L, Fleischman DA, Arfanakis K, Leurgans S, Bennett DA (2014) Financial literacy is associated with medial brain region functional connectivity in old age. Arch Gerontol Geriatr 59, 429–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [267].Boyle PA, Yu L, Gamble KJ, Bennett DA (2013) Temporal Discounting Is Associated with an Increased Risk of Mortality among Community-Based Older Persons without Dementia. PLoS One 8, e67376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [268].Boyle PA, Yu L, Segawa E, Wilson RS, Buchman AS, Laibson DI, Bennett DA (2012) Association of cognition with temporal discounting in community based older persons. BMC Geriatr 12, 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [269].James BD, Boyle PA, Yu L, Han SD, Bennett DA (2015) Cognitive decline is associated with risk aversion and temporal discounting in older adults without dementia. PLoS One 10, e0121900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [270].Han SD, Boyle PA, Yu L, Fleischman DA, Arfanakis K, Bennett DA (2013) Ventromedial PFC, parahippocampal, and cerebellar connectivity are associated with temporal discounting in old age. Exp Gerontol 48, 1489–1498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [271].Boyle PA, Yu L, Buchman AS, Bennett DA (2012) Risk Aversion is Associated with Decision Making among Community-Based Older Persons. Front Psychol 3, 205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [272].Han SD, Boyle PA, Arfanakis K, Fleischman DA, Yu L, Edmonds EC, Bennett DA (2012) Neural intrinsic connectivity networks associated with risk aversion in old age. Behav Brain Res 227, 233–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [273].James BD, Boyle PA, Bennett DA (2014) Correlates of susceptibility to scams in older adults without dementia. J Elder Abuse Negl 26, 107–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [274].Han SD, Boyle PA, James BD, Yu L, Bennett DA (2016) Mild Cognitive Impairment and Susceptibility to Scams in Old Age. J Alzheimers Dis 49, 845–851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [275].Han SD, Boyle PA, Yu L, Arfanakis K, James BD, Fleischman DA, Bennett DA (2016) Grey matter correlates of susceptibility to scams in community-dwelling older adults. Brain Imaging Behav 10, 524–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [276].Accelerating Medicines Partnership - Alzheimer’s Disease (AMP-AD), https://www.nia.nih.gov/research/amp-ad,
- [277].Bennett DA, Yu L, De Jager PL (2014) Building a pipeline to discover and validate novel therapeutic targets and lead compounds for Alzheimer’s disease. Biochem Pharmacol 88, 617–630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [278].De Jager PL, Bennett DA (2013) An inflection point in gene discovery efforts for neurodegenerative diseases: from syndromic diagnoses toward endophenotypes and the epigenome. JAMA Neurol 70, 719–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [279].De Jager PL, Srivastava G, Lunnon K, Burgess J, Schalkwyk LC, Yu L, Eaton ML, Keenan BT, Ernst J, McCabe C, Tang A, Raj T, Replogle J, Brodeur W, Gabriel S, Chai HS, Younkin C, Younkin SG, Zou F, Szyf M, Epstein CB, Schneider JA, Bernstein BE, Meissner A, Ertekin-Taner N, Chibnik LB, Kellis M, Mill J, Bennett DA (2014) Alzheimer’s disease: early alterations in brain DNA methylation at ANK1, BIN1, RHBDF2 and other loci. Nat Neurosci 17, 1156–1163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [280].Bennett DA, Yu L, Yang J, Srivastava GP, Aubin C, De Jager PL (2015) Epigenomics of Alzheimer’s disease. Transl Res 165, 200–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [281].Yang J, Yu L, Gaiteri C, Srivastava GP, Chibnik LB, Leurgans SE, Schneider JA, Meissner A, De Jager PL, Bennett DA (2015) Association of DNA methylation in the brain with age in older persons is confounded by common neuropathologies. Int J Biochem Cell Biol 67, 58–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [282].Klein HU, Bennett DA, De Jager PL (2016) The epigenome in Alzheimer’s disease: current state and approaches for a new path to gene discovery and understanding disease mechanism. Acta Neuropathol 132, 503–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [283].Ng B, White CC, Klein HU, Sieberts SK, McCabe C, Patrick E, Xu J, Yu L, Gaiteri C, Bennett DA, Mostafavi S, De Jager PL (2017) An xQTL map integrates the genetic architecture of the human brain’s transcriptome and epigenome. Nat Neurosci 20, 1418–1426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [284].Patrick E, Rajagopal S, Wong HA, McCabe C, Xu J, Tang A, Imboywa SH, Schneider JA, Pochet N, Krichevsky AM, Chibnik LB, Bennett DA, De Jager PL (2017) Dissecting the role of non-coding RNAs in the accumulation of amyloid and tau neuropathologies in Alzheimer’s disease. Mol Neurodegener 12, 51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [285].Zhao J, Zhu Y, Yang J, Li L, Wu H, De Jager PL, Jin P, Bennett DA (2017) A genome-wide profiling of brain DNA hydroxymethylation in Alzheimer’s disease. Alzheimers Dement 13, 674–688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [286].Olah M, Patrick E, Villani C, Xu J, White C, Ryan K, Piehowski P, Kapasi A, Nejad P, Cimpean M, Connor S, Yung C, Frangieh M, McHenry A, Elyaman W, Petyuk V, Shneider JA, Bennett DA, De Jager P, Bradshaw EM (2018) A transcriptomic atlas of aged human microglia. Nature Communications In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [287].Yu L, Chibnik LB, Yang J, McCabe C, Xu J, Schneider JA, De Jager PL, Bennett DA (2016) Methylation profiles in peripheral blood CD4+ lymphocytes versus brain: The relation to Alzheimer’s disease pathology. Alzheimers Dement 12, 942–951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [288].Yu L, Dawe RJ, Boyle PA, Gaiteri C, Yang J, Buchman AS, Schneider JA, Arfanakis K, De Jager PL, Bennett DA (2017) Association Between Brain Gene Expression, DNA Methylation, and Alteration of Ex Vivo Magnetic Resonance Imaging Transverse Relaxation in Late-Life Cognitive Decline. JAMA Neurol 74, 1473–1480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [289].Muratore CR, Zhou C, Liao M, Fernandez MA, Taylor WM, Lagomarsino VN, Pearse RV 2nd, Rice HC, Negri JM, He A, Srikanth P, Callahan DG, Shin T, Zhou M, Bennett DA, Noggle S, Love JC, Selkoe DJ, Young-Pearse TL (2017) Cell-type Dependent Alzheimer’s Disease Phenotypes: Probing the Biology of Selective Neuronal Vulnerability. Stem Cell Reports 9, 1868–1884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [290].Ryan KJ, White CC, Patel K, Xu J, Olah M, Replogle JM, Frangieh M, Cimpean M, Winn P, McHenry A, Kaskow BJ, Chan G, Cuerdon N, Bennett DA, Boyd JD, Imitola J, Elyaman W, De Jager PL, Bradshaw EM (2017) A human microglia-like cellular model for assessing the effects of neurodegenerative disease gene variants. Sci Transl Med 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [291].Gaiteri C, Mostafavi S, Honey CJ, De Jager PL, Bennett DA (2016) Genetic variants in Alzheimer disease - molecular and brain network approaches. Nat Rev Neurol 12, 413–427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [292].Bennett DA (2017) Mixed pathologies and neural reserve: Implications of complexity for Alzheimer disease drug discovery. PLoS Med 14, e1002256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [293].Mostafavi S, Gaiteri C, Sullivan S, White C, Takasi S, Xu J, Taga M, Klein H, Patrick E, Komashko V, McCable C, Smith R, Bradshaw E, Root D, Yu L, Regev A, Chibnik L, Schneider J, Young-Pearse T, Bennett DA, De Jager P (2017) A molecular network of the aging brain implicates INPPL1 and PLXNB1 in Alzheimer’s disease. bioRxiv
- [294].Xiong C, Weng H, Bennett DA, Boyle PA, Shah RC, Fague S, Hall CB, Lipton RB, Morris JC (2014) Subsets of a large cognitive battery better power clinical trials on early stage Alzheimer’s disease. Neuroepidemiology 43, 131–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [295].Langbaum JB, Hendrix SB, Ayutyanont N, Chen K, Fleisher AS, Shah RC, Barnes LL, Bennett DA, Tariot PN, Reiman EM (2014) An empirically derived composite cognitive test score with improved power to track and evaluate treatments for preclinical Alzheimer’s disease. Alzheimers Dement 10, 666–674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [296].Langbaum JB, Hendrix S, Ayutyanont N, Bennett DA, Shah RC, Barnes LL, Lopera F, Reiman EM, Tariot PN (2015) Establishing Composite Cognitive Endpoints for Use in Preclinical Alzheimer’s Disease Trials. J Prev Alzheimers Dis 2, 2–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [297].Rush Alzheimer’s Disease Center, http://www.radc.rush.edu,
- [298].AMPAD Knowledge Portal, https://www.synapse.org/#!Synapse:syn2580853/wiki/409840,
- [299].Zhang J, Wang S, Huang W, Bennett DA, Dickson DW, Wang D, Wang R (2016) Tissue Transglutaminase and Its Product Isopeptide Are Increased in Alzheimer’s Disease and APPswe/PS1dE9 Double Transgenic Mice Brains. Mol Neurobiol 53, 5066–5078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [300].Rangasamy SB, Corbett GT, Roy A, Modi KK, Bennett DA, Mufson EJ, Ghosh S, Pahan K (2015) Intranasal Delivery of NEMO-Binding Domain Peptide Prevents Memory Loss in a Mouse Model of Alzheimer’s Disease. J Alzheimers Dis 47, 385–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [301].Traversy MT, Vandal M, Tremblay C, Tournissac M, Giguere-Rancourt A, Bennett AD, Calon F (2017) Altered cerebral insulin response in transgenic mice expressing the epsilon-4 allele of the human apolipoprotein E gene. Psychoneuroendocrinology 77, 203–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [302].Ahmad F, Singh K, Das D, Gowaikar R, Shaw E, Ramachandran A, Rupanagudi KV, Kommaddi RP, Bennett DA, Ravindranath V (2017) Reactive Oxygen Species-Mediated Loss of Synaptic Akt1 Signaling Leads to Deficient Activity-Dependent Protein Translation Early in Alzheimer’s Disease. Antioxid Redox Signal 27, 1269–1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [303].Barbash S, Garfinkel BP, Maoz R, Simchovitz A, Nadorp B, Guffanti A, Bennett ER, Nadeau C, Turk A, Paul L, Reda T, Li Y, Buchman AS, Greenberg DS, Seitz A, Bennett DA, Giavalisco P, Soreq H (2017) Alzheimer’s brains show inter-related changes in RNA and lipid metabolism. Neurobiol Dis 106, 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [304].Klaver AC, Coffey MP, Bennett DA, Loeffler DA (2017) Specific serum antibody binding to phosphorylated and non-phosphorylated tau in non-cognitively impaired, mildly cognitively impaired, and Alzheimer’s disease subjects: an exploratory study. Transl Neurodegener 6, 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [305].Bis JC, DeCarli C, Smith AV, van der Lijn F, Crivello F, Fornage M, Debette S, Shulman JM, Schmidt H, Srikanth V, Schuur M, Yu L, Choi SH, Sigurdsson S, Verhaaren BF, DeStefano AL, Lambert JC, Jack CR Jr., Struchalin M, Stankovich J, Ibrahim-Verbaas CA, Fleischman D, Zijdenbos A, den Heijer T, Mazoyer B, Coker LH, Enzinger C, Danoy P, Amin N, Arfanakis K, van Buchem MA, de Bruijn RF, Beiser A, Dufouil C, Huang J, Cavalieri M, Thomson R, Niessen WJ, Chibnik LB, Gislason GK, Hofman A, Pikula A, Amouyel P, Freeman KB, Phan TG, Oostra BA, Stein JL, Medland SE, Vasquez AA, Hibar DP, Wright MJ, Franke B, Martin NG, Thompson PM, Nalls MA, Uitterlinden AG, Au R, Elbaz A, Beare RJ, van Swieten JC, Lopez OL, Harris TB, Chouraki V, Breteler MM, De Jager PL, Becker JT, Vernooij MW, Knopman D, Fazekas F, Wolf PA, van der Lugt A, Gudnason V, Longstreth WT Jr., Brown MA, Bennett DA, van Duijn CM, Mosley TH, Schmidt R, Tzourio C, Launer LJ, Ikram MA, Seshadri S (2012) Common variants at 12q14 and 12q24 are associated with hippocampal volume. Nat Genet 44, 545–551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [306].Tsuang D, Leverenz JB, Lopez OL, Hamilton RL, Bennett DA, Schneider JA, Buchman AS, Larson EB, Crane PK, Kaye JA, Kramer P, Woltjer R, Kukull W, Nelson PT, Jicha GA, Neltner JH, Galasko D, Masliah E, Trojanowski JQ, Schellenberg GD, Yearout D, Huston H, Fritts-Penniman A, Mata IF, Wan JY, Edwards KL, Montine TJ, Zabetian CP (2012) GBA mutations increase risk for Lewy body disease with and without Alzheimer disease pathology. Neurology 79, 1944–1950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [307].Zhang B, Gaiteri C, Bodea LG, Wang Z, McElwee J, Podtelezhnikov AA, Zhang C, Xie T, Tran L, Dobrin R, Fluder E, Clurman B, Melquist S, Narayanan M, Suver C, Shah H, Mahajan M, Gillis T, Mysore J, MacDonald ME, Lamb JR, Bennett DA, Molony C, Stone DJ, Gudnason V, Myers AJ, Schadt EE, Neumann H, Zhu J, Emilsson V (2013) Integrated systems approach identifies genetic nodes and networks in late-onset Alzheimer’s disease. Cell 153, 707–720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [308].Valenca GT, Srivastava GP, Oliveira-Filho J, White CC, Yu L, Schneider JA, Buchman AS, Shulman JM, Bennett DA, De Jager PL (2016) The Role of MAPT Haplotype H2 and Isoform 1N/4R in Parkinsonism of Older Adults. PLoS One 11, e0157452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [309].Felsky D, Xu J, Chibnik LB, Schneider JA, Knight J, Kennedy JL, Bennett DA, De Jager PL, Voineskos AN (2017) Genetic epistasis regulates amyloid deposition in resilient aging. Alzheimers Dement 13, 1107–1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [310].Levine ME, Lu AT, Bennett DA, Horvath S (2015) Epigenetic age of the pre-frontal cortex is associated with neuritic plaques, amyloid load, and Alzheimer’s disease related cognitive functioning. Aging (Albany NY) 7, 1198–1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [311].Abadir PM, Jain A, Powell LJ, Xue QL, Tian J, Hamilton RG, Bennett DA, Finucane T, Walston JD, Fedarko NS (2017) Discovery and Validation of Agonistic Angiotensin Receptor Autoantibodies as Biomarkers of Adverse Outcomes. Circulation 135, 449–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [312].Felsky D, De Jager PL, Schneider JA, Arfanakis K, Fleischman DA, Arvanitakis Z, Honer WG, Pouget JG, Mizrahi R, Pollock BG, Kennedy JL, Bennett DA, Voineskos AN (2016) Cerebrovascular and microglial states are not altered by functional neuroinflammatory gene variant. J Cereb Blood Flow Metab 36, 819–830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [313].Bartolotti N, Bennett DA, Lazarov O (2016) Reduced pCREB in Alzheimer’s disease prefrontal cortex is reflected in peripheral blood mononuclear cells. Mol Psychiatry 21, 1158–1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [314].Chan G, White CC, Winn PA, Cimpean M, Replogle JM, Glick LR, Cuerdon NE, Ryan KJ, Johnson KA, Schneider JA, Bennett DA, Chibnik LB, Sperling RA, De Jager PL, Bradshaw EM (2016) Trans-pQTL study identifies immune crosstalk between Parkinson and Alzheimer loci. Neurol Genet 2, e90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [315].Vardarajan BN, Tosto G, Lefort R, Yu L, Bennett DA, De Jager PL, Barral S, Reyes-Dumeyer D, Nagy PL, Lee JH, Cheng R, Medrano M, Lantigua R, Rogaeva E, St George-Hyslop P, Mayeux R (2017) Ultra-rare mutations in SRCAP segregate in Caribbean Hispanic families with Alzheimer disease. Neurol Genet 3, e178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [316].Huang JY, Hafez DM, James BD, Bennett DA, Marr RA (2012) Altered NEP2 expression and activity in mild cognitive impairment and Alzheimer’s disease. J Alzheimers Dis 28, 433–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [317].Wang H-Y, Stucky A, Hahn C-G, Wilson R, Bennett D, Arnold S (2011) in Translational Neuroscience, p. 91. [Google Scholar]
- [318].Ramcharitar J, Afonso VM, Albrecht S, Bennett DA, LeBlanc AC (2013) Caspase-6 activity predicts lower episodic memory ability in aged individuals. Neurobiol Aging 34, 1815–1824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [319].Ramcharitar J, Albrecht S, Afonso VM, Kaushal V, Bennett DA, Leblanc AC (2013) Cerebrospinal fluid tau cleaved by caspase-6 reflects brain levels and cognition in aging and Alzheimer disease. J Neuropathol Exp Neurol 72, 824–832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [320].Zhou L, Wei C, Huang W, Bennett DA, Dickson DW, Wang R, Wang D (2013) Distinct subcellular patterns of neprilysin protein and activity in the brains of Alzheimer’s disease patients, transgenic mice and cultured human neuronal cells. Am J Transl Res 5, 608–621. [PMC free article] [PubMed] [Google Scholar]
- [321].LeBlanc AC, Ramcharitar J, Afonso V, Hamel E, Bennett DA, Pakavathkumar P, Albrecht S (2014) Caspase-6 activity in the CA1 region of the hippocampus induces age-dependent memory impairment. Cell Death Differ 21, 696–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [322].Song W, Zukor H, Liberman A, Kaduri S, Arvanitakis Z, Bennett DA, Schipper HM (2014) Astroglial heme oxygenase-1 and the origin of corpora amylacea in aging and degenerating neural tissues. Exp Neurol 254, 78–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [323].Ohta Y, Tremblay C, Schneider JA, Bennett DA, Calon F, Julien JP (2014) Interaction of transactive response DNA binding protein 43 with nuclear factor kappaB in mild cognitive impairment with episodic memory deficits. Acta Neuropathol Commun 2, 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [324].Ramos-Miguel A, Garcia-Sevilla JA, Barr AM, Bayer TA, Falkai P, Leurgans SE, Schneider JA, Bennett DA, Honer WG, Garcia-Fuster MJ (2017) Decreased cortical FADD protein is associated with clinical dementia and cognitive decline in an elderly community sample. Mol Neurodegener 12, 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [325].Smith PY, Hernandez-Rapp J, Jolivette F, Lecours C, Bisht K, Goupil C, Dorval V, Parsi S, Morin F, Planel E, Bennett DA, Fernandez-Gomez FJ, Sergeant N, Buee L, Tremblay ME, Calon F, Hebert SS (2015) miR-132/212 deficiency impairs tau metabolism and promotes pathological aggregation in vivo. Hum Mol Genet 24, 6721–6735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [326].Lu T, Aron L, Zullo J, Pan Y, Kim H, Chen Y, Yang TH, Kim HM, Drake D, Liu XS, Bennett DA, Colaiacovo MP, Yankner BA (2014) REST and stress resistance in ageing and Alzheimer’s disease. Nature 507, 448–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [327].Hinrich AJ, Jodelka FM, Chang JL, Brutman D, Bruno AM, Briggs CA, James BD, Stutzmann GE, Bennett DA, Miller SA, Rigo F, Marr RA, Hastings ML (2016) Therapeutic correction of ApoER2 splicing in Alzheimer’s disease mice using antisense oligonucleotides. EMBO Mol Med 8, 328–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [328].Ali YO, Allen HM, Yu L, Li-Kroeger D, Bakhshizadehmahmoudi D, Hatcher A, McCabe C, Xu J, Bjorklund N, Taglialatela G, Bennett DA, De Jager PL, Shulman JM, Bellen HJ, Lu HC (2016) NMNAT2:HSP90 Complex Mediates Proteostasis in Proteinopathies. PLoS Biol 14, e1002472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [329].Do Carmo S, Hanzel CE, Jacobs ML, Machnes Z, Iulita MF, Yang J, Yu L, Ducatenzeiler A, Danik M, Breuillaud LS, Bennett DA, Szyf M, Cuello AC (2016) Rescue of Early bace-1 and Global DNA Demethylation by S-Adenosylmethionine Reduces Amyloid Pathology and Improves Cognition in an Alzheimer’s Model. Sci Rep 6, 34051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [330].Liu RX, Huang C, Bennett DA, Li H, Wang R (2016) The characteristics of astrocyte on Abeta clearance altered in Alzheimer’s disease were reversed by anti-inflammatory agent (+)-2-(1-hydroxyl-4-oxocyclohexyl) ethyl caffeate. Am J Transl Res 8, 4082–4094. [PMC free article] [PubMed] [Google Scholar]
- [331].Barbash S, Simchovitz A, Buchman AS, Bennett DA, Shifman S, Soreq H (2017) Neuronal-expressed microRNA-targeted pseudogenes compete with coding genes in the human brain. Transl Psychiatry 7, e1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [332].Kommaddi RP, Das D, Karunakaran S, Nanguneri S, Bapat D, Ray A, Shaw E, Bennett DA, Nair D, Ravindranath V (2017) Abeta mediates F-actin disassembly in dendritic spines leading to cognitive deficits in Alzheimer’s disease. J Neurosci. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [333].Arsenault D, Dal-Pan A, Tremblay C, Bennett DA, Guitton MJ, De Koninck Y, Tonegawa S, Calon F (2013) PAK inactivation impairs social recognition in 3xTg-AD Mice without increasing brain deposition of tau and Abeta. J Neurosci 33, 10729–10740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [334].Lu T, Aron L, Zullo J, Pan Y, Kim H, Chen Y, Yang TH, Kim HM, Drake D, Liu XS, Bennett DA, Colaiacovo MP, Yankner BA (2016) Addendum: REST and stress resistance in ageing and Alzheimer’s disease. Nature 540, 470. [DOI] [PubMed] [Google Scholar]
- [335].Larson ME, Greimel SJ, Amar F, LaCroix M, Boyle G, Sherman MA, Schley H, Miel C, Schneider JA, Kayed R, Benfenati F, Lee MK, Bennett DA, Lesne SE (2017) Selective lowering of synapsins induced by oligomeric alpha-synuclein exacerbates memory deficits. Proc Natl Acad Sci U S A 114, E4648–e4657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [336].Ziller MJ, Gu H, Muller F, Donaghey J, Tsai LT, Kohlbacher O, De Jager PL, Rosen ED, Bennett DA, Bernstein BE, Gnirke A, Meissner A (2013) Charting a dynamic DNA methylation landscape of the human genome. Nature 500, 477–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [337].Zhu J, Adli M, Zou JY, Verstappen G, Coyne M, Zhang X, Durham T, Miri M, Deshpande V, De Jager PL, Bennett DA, Houmard JA, Muoio DM, Onder TT, Camahort R, Cowan CA, Meissner A, Epstein CB, Shoresh N, Bernstein BE (2013) Genome-wide chromatin state transitions associated with developmental and environmental cues. Cell 152, 642–654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [338].Verghese J, Ayers E, Barzilai N, Bennett DA, Buchman AS, Holtzer R, Katz MJ, Lipton RB, Wang C (2014) Motoric cognitive risk syndrome: Multicenter incidence study. Neurology 83, 2278–2284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [339].Ramanan VK, Nho K, Shen L, Risacher SL, Kim S, McDonald BC, Farlow MR, Foroud TM, Gao S, Soininen H, Kloszewska I, Mecocci P, Tsolaki M, Vellas B, Lovestone S, Aisen PS, Petersen RC, Jack CR Jr., Shaw LM, Trojanowski JQ, Weiner MW, Green RC, Toga AW, De Jager PL, Yu L, Bennett DA, Saykin AJ (2015) FASTKD2 is associated with memory and hippocampal structure in older adults. Mol Psychiatry 20, 1197–1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [340].Ramanan VK, Risacher SL, Nho K, Kim S, Shen L, McDonald BC, Yoder KK, Hutchins GD, West JD, Tallman EF, Gao S, Foroud TM, Farlow MR, De Jager PL, Bennett DA, Aisen PS, Petersen RC, Jack CR Jr., Toga AW, Green RC, Jagust WJ, Weiner MW, Saykin AJ (2015) GWAS of longitudinal amyloid accumulation on 18F-florbetapir PET in Alzheimer’s disease implicates microglial activation gene IL1RAP. Brain 138, 3076–3088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [341].Cade BE, Gottlieb DJ, Lauderdale DS, Bennett DA, Buchman AS, Buxbaum SG, De Jager PL, Evans DS, Fulop T, Gharib SA, Johnson WC, Kim H, Larkin EK, Lee SK, Lim AS, Punjabi NM, Shin C, Stone KL, Tranah GJ, Weng J, Yaffe K, Zee PC, Patel SR, Zhu X, Redline S, Saxena R (2016) Common variants in DRD2 are associated with sleep duration: the CARe consortium. Hum Mol Genet 25, 167–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [342].Tosto G, Bird TD, Bennett DA, Boeve BF, Brickman AM, Cruchaga C, Faber K, Foroud TM, Farlow M, Goate AM, Graff-Radford NR, Lantigua R, Manly J, Ottman R, Rosenberg R, Schaid DJ, Schupf N, Stern Y, Sweet RA, Mayeux R (2016) The Role of Cardiovascular Risk Factors and Stroke in Familial Alzheimer Disease. JAMA Neurol 73, 1231–1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [343].Dong J, Wyss A, Yang J, Price TR, Nicolas A, Nalls M, Tranah G, Franceschini N, Xu Z, Schulte C, Alonso A, Cummings SR, Fornage M, Zaykin D, Li L, Huang X, Kritchevsky S, Liu Y, Gasser T, Wilson RS, De Jager PL, Singleton AB, Pinto JM, Harris T, Mosley TH Jr., Bennett DA, London S, Yu L, Chen H (2017) Genome-Wide Association Analysis of the Sense of Smell in U.S. Older Adults: Identification of Novel Risk Loci in African-Americans and European-Americans. Mol Neurobiol 54, 8021–8032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [344].Dodge HH, Zhu J, Woltjer R, Nelson PT, Bennett DA, Cairns NJ, Fardo DW, Kaye JA, Lyons DE, Mattek N, Schneider JA, Silbert LC, Xiong C, Yu L, Schmitt FA, Kryscio RJ, Abner EL (2017) Risk of incident clinical diagnosis of Alzheimer’s disease-type dementia attributable to pathology-confirmed vascular disease. Alzheimers Dement 13, 613–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [345].Kelly A, Calamia M, Koval A, Terrera GM, Piccinin AM, Clouston S, Hassing LB, Bennett DA, Johansson B, Hofer SM (2016) Independent and interactive impacts of hypertension and diabetes mellitus on verbal memory: A coordinated analysis of longitudinal data from England, Sweden, and the United States. Psychol Aging 31, 262–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [346].Abner EL, Kryscio RJ, Schmitt FA, Fardo DW, Moga DC, Ighodaro ET, Jicha GA, Yu L, Dodge HH, Xiong C, Woltjer RL, Schneider JA, Cairns NJ, Bennett DA, Nelson PT (2017) Outcomes after diagnosis of mild cognitive impairment in a large autopsy series. Ann Neurol 81, 549–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [347].Thaker AA, Weinberg BD, Dillon WP, Hess CP, Cabral HJ, Fleischman DA, Leurgans SE, Bennett DA, Hyman BT, Albert MS, Killiany RJ, Fischl B, Dale AM, Desikan RS (2017) Entorhinal Cortex: Antemortem Cortical Thickness and Postmortem Neurofibrillary Tangles and Amyloid Pathology. AJNR Am J Neuroradiol 38, 961–965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [348].Graham EK, Rutsohn JP, Turiano NA, Bendayan R, Batterham PJ, Gerstorf D, Katz MJ, Reynolds CA, Sharp ES, Yoneda TB, Bastarache ED, Elleman LG, Zelinski EM, Johansson B, Kuh D, Barnes LL, Bennett DA, Deeg DJH, Lipton RB, Pedersen NL, Piccinin AM, Spiro A 3rd, Muniz-Terrera G, Willis SL, Schaie KW, Roan C, Herd P, Hofer SM, Mroczek DK (2017) Personality Predicts Mortality Risk: An Integrative Data Analysis of 15 International Longitudinal Studies. J Res Pers 70, 174–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [349].Tan CH, Fan CC, Mormino EC, Sugrue LP, Broce IJ, Hess CP, Dillon WP, Bonham LW, Yokoyama JS, Karch CM, Brewer JB, Rabinovici GD, Miller BL, Schellenberg GD, Kauppi K, Feldman HA, Holland D, McEvoy LK, Hyman BT, Bennett DA, Andreassen OA, Dale AM, Desikan RS (2018) Polygenic hazard score: an enrichment marker for Alzheimer’s associated amyloid and tau deposition. Acta Neuropathol 135, 85–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [350].Proust-Lima C, Philipps V, Dartigues JF, Bennett DA, Glymour MM, Jacqmin-Gadda H, Samieri C (2017) Are latent variable models preferable to composite score approaches when assessing risk factors of change? Evaluation of type-I error and statistical power in longitudinal cognitive studies. Stat Methods Med Res, 962280217739658. [DOI] [PubMed] [Google Scholar]
- [351].Knopman DS, Parisi JE, Salviati A, Floriach-Robert M, Boeve BF, Ivnik RJ, Smith GE, Dickson DW, Johnson KA, Petersen LE, McDonald WC, Braak H, Petersen RC (2003) Neuropathology of cognitively normal elderly. J Neuropathol Exp Neurol 62, 1087–1095. [DOI] [PubMed] [Google Scholar]
- [352].Price JL, McKeel DW Jr., Buckles VD, Roe CM, Xiong C, Grundman M, Hansen LA, Petersen RC, Parisi JE, Dickson DW, Smith CD, Davis DG, Schmitt FA, Markesbery WR, Kaye J, Kurlan R, Hulette C, Kurland BF, Higdon R, Kukull W, Morris JC (2009) Neuropathology of nondemented aging: presumptive evidence for preclinical Alzheimer disease. Neurobiol Aging 30, 1026–1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [353].SantaCruz KS, Sonnen JA, Pezhouh MK, Desrosiers MF, Nelson PT, Tyas SL (2011) Alzheimer disease pathology in subjects without dementia in 2 studies of aging: the Nun Study and the Adult Changes in Thought Study. J Neuropathol Exp Neurol 70, 832–840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [354].Monsell SE, Mock C, Hassenstab J, Roe CM, Cairns NJ, Morris JC, Kukull W (2014) Neuropsychological changes in asymptomatic persons with Alzheimer disease neuropathology. Neurology 83, 434–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [355].Green MS, Kaye JA, Ball MJ (2000) The Oregon brain aging study: neuropathology accompanying healthy aging in the oldest old. Neurology 54, 105–113. [DOI] [PubMed] [Google Scholar]
- [356].Galvin JE, Powlishta KK, Wilkins K, McKeel DW Jr., Xiong C, Grant E, Storandt M, Morris JC (2005) Predictors of preclinical Alzheimer disease and dementia: a clinicopathologic study. Arch Neurol 62, 758–765. [DOI] [PubMed] [Google Scholar]
- [357].Balasubramanian AB, Kawas CH, Peltz CB, Brookmeyer R, Corrada MM (2012) Alzheimer disease pathology and longitudinal cognitive performance in the oldest-old with no dementia. Neurology 79, 915–921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [358].Mintun MA, Larossa GN, Sheline YI, Dence CS, Lee SY, Mach RH, Klunk WE, Mathis CA, DeKosky ST, Morris JC (2006) [11C]PIB in a nondemented population: potential antecedent marker of Alzheimer disease. Neurology 67, 446–452. [DOI] [PubMed] [Google Scholar]
- [359].Pike KE, Savage G, Villemagne VL, Ng S, Moss SA, Maruff P, Mathis CA, Klunk WE, Masters CL, Rowe CC (2007) Beta-amyloid imaging and memory in non-demented individuals: evidence for preclinical Alzheimer’s disease. Brain 130, 2837–2844. [DOI] [PubMed] [Google Scholar]
- [360].Reiman EM, Chen K, Liu X, Bandy D, Yu M, Lee W, Ayutyanont N, Keppler J, Reeder SA, Langbaum JB, Alexander GE, Klunk WE, Mathis CA, Price JC, Aizenstein HJ, DeKosky ST, Caselli RJ (2009) Fibrillar amyloid-beta burden in cognitively normal people at 3 levels of genetic risk for Alzheimer’s disease. Proc Natl Acad Sci U S A 106, 6820–6825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [361].Sojkova J, Zhou Y, An Y, Kraut MA, Ferrucci L, Wong DF, Resnick SM (2011) Longitudinal patterns of beta-amyloid deposition in nondemented older adults. Arch Neurol 68, 644–649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [362].Braskie MN, Klunder AD, Hayashi KM, Protas H, Kepe V, Miller KJ, Huang SC, Barrio JR, Ercoli LM, Siddarth P, Satyamurthy N, Liu J, Toga AW, Bookheimer SY, Small GW, Thompson PM (2010) Plaque and tangle imaging and cognition in normal aging and Alzheimer’s disease. Neurobiol Aging 31, 1669–1678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [363].Merrill DA, Siddarth P, Saito NY, Ercoli LM, Burggren AC, Kepe V, Lavretsky H, Miller KJ, Kim J, Huang SC, Bookheimer SY, Barrio JR, Small GW (2012) Self-reported memory impairment and brain PET of amyloid and tau in middle-aged and older adults without dementia. Int Psychogeriatr 24, 1076–1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [364].Sutphen CL, Jasielec MS, Shah AR, Macy EM, Xiong C, Vlassenko AG, Benzinger TL, Stoops EE, Vanderstichele HM, Brix B, Darby HD, Vandijck ML, Ladenson JH, Morris JC, Holtzman DM, Fagan AM (2015) Longitudinal Cerebrospinal Fluid Biomarker Changes in Preclinical Alzheimer Disease During Middle Age. JAMA Neurol 72, 1029–1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [365].Bischof GN, Rodrigue KM, Kennedy KM, Devous MD Sr., Park DC (2016) Amyloid deposition in younger adults is linked to episodic memory performance. Neurology 87, 2562–2566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [366].Jack CR Jr., Wiste HJ, Weigand SD, Therneau TM, Knopman DS, Lowe V, Vemuri P, Mielke MM, Roberts RO, Machulda MM, Senjem ML, Gunter JL, Rocca WA, Petersen RC (2017) Age-specific and sex-specific prevalence of cerebral beta-amyloidosis, tauopathy, and neurodegeneration in cognitively unimpaired individuals aged 50–95 years: a cross-sectional study. Lancet Neurol 16, 435–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [367].Jack CR, Bennett DA, Blennow K (2018) 2018 NIA-AA research framework to investigate the Alzheimer’s disease continuum. [DOI] [PMC free article] [PubMed]
- [368].Jack CR Jr., Bennett DA, Blennow K, Carrillo MC, Feldman HH, Frisoni GB, Hampel H, Jagust WJ, Johnson KA, Knopman DS, Petersen RC, Scheltens P, Sperling RA, Dubois B (2016) A/T/N: An unbiased descriptive classification scheme for Alzheimer disease biomarkers. Neurology 87, 539–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [369].(2001) Pathological correlates of late-onset dementia in a multicentre, community-based population in England and Wales. Neuropathology Group of the Medical Research Council Cognitive Function and Ageing Study (MRC CFAS). Lancet 357, 169–175. [DOI] [PubMed] [Google Scholar]
- [370].Sonnen JA, Larson EB, Crane PK, Haneuse S, Li G, Schellenberg GD, Craft S, Leverenz JB, Montine TJ (2007) Pathological correlates of dementia in a longitudinal, population-based sample of aging. Ann Neurol 62, 406–413. [DOI] [PubMed] [Google Scholar]
- [371].White L, Small BJ, Petrovitch H, Ross GW, Masaki K, Abbott RD, Hardman J, Davis D, Nelson J, Markesbery W (2005) Recent clinical-pathologic research on the causes of dementia in late life: update from the Honolulu-Asia Aging Study. J Geriatr Psychiatry Neurol 18, 224–227. [DOI] [PubMed] [Google Scholar]
- [372].Nelson PT, Abner EL, Schmitt FA, Kryscio RJ, Jicha GA, Smith CD, Davis DG, Poduska JW, Patel E, Mendiondo MS, Markesbery WR (2010) Modeling the association between 43 different clinical and pathological variables and the severity of cognitive impairment in a large autopsy cohort of elderly persons. Brain Pathol 20, 66–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [373].Brenowitz WD, Hubbard RA, Keene CD, Hawes SE, Longstreth WT Jr., Woltjer RL, Kukull WA (2017) Mixed neuropathologies and associations with domain-specific cognitive decline. Neurology 89, 1773–1781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [374].Brenowitz WD, Hubbard RA, Keene CD, Hawes SE, Longstreth WT Jr., Woltjer RL, Kukull WA (2017) Mixed neuropathologies and estimated rates of clinical progression in a large autopsy sample. Alzheimers Dement 13, 654–662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [375].Azarpazhooh MR, Avan A, Cipriano LE, Munoz DG, Sposato LA, Hachinski V (2017) Concomitant vascular and neurodegenerative pathologies double the risk of dementia. Alzheimers Dement. [DOI] [PubMed] [Google Scholar]
- [376].Gold G, Giannakopoulos P, Herrmann FR, Bouras C, Kovari E (2007) Identification of Alzheimer and vascular lesion thresholds for mixed dementia. Brain 130, 2830–2836. [DOI] [PubMed] [Google Scholar]
- [377].Matthews FE, Brayne C, Lowe J, McKeith I, Wharton SB, Ince P (2009) Epidemiological pathology of dementia: attributable-risks at death in the Medical Research Council Cognitive Function and Ageing Study. PLoS Med 6, e1000180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [378].Vemuri P, Lesnick TG, Przybelski SA, Knopman DS, Lowe VJ, Graff-Radford J, Roberts RO, Mielke MM, Machulda MM, Petersen RC, Jack CR Jr., (2017) Age, vascular health, and Alzheimer disease biomarkers in an elderly sample. Ann Neurol 82, 706–718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [379].Marnane M, Al-Jawadi OO, Mortazavi S, Pogorzelec KJ, Wang BW, Feldman HH, Hsiung GY (2016) Periventricular hyperintensities are associated with elevated cerebral amyloid. Neurology 86, 535–543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [380].Lo RY, Jagust WJ (2012) Vascular burden and Alzheimer disease pathologic progression. Neurology 79, 1349–1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [381].Barulli D, Stern Y (2013) Efficiency, capacity, compensation, maintenance, plasticity: emerging concepts in cognitive reserve. Trends Cogn Sci 17, 502–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [382].Valenzuela MJ (2008) Brain reserve and the prevention of dementia. Curr Opin Psychiatry 21, 296–302. [DOI] [PubMed] [Google Scholar]
- [383].Fratiglioni L, Wang HX (2007) Brain reserve hypothesis in dementia. J Alzheimers Dis 12, 11–22. [DOI] [PubMed] [Google Scholar]
- [384].Esiri MM, Chance SA (2012) Cognitive reserve, cortical plasticity and resistance to Alzheimer’s disease. Alzheimers Res Ther 4, 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [385].Negash S, Wilson RS, Leurgans SE, Wolk DA, Schneider JA, Buchman AS, Bennett DA, Arnold SE (2013) Resilient brain aging: characterization of discordance between Alzheimer’s disease pathology and cognition. Curr Alzheimer Res 10, 844–851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [386].Terracciano A, Iacono D, O’Brien RJ, Troncoso JC, An Y, Sutin AR, Ferrucci L, Zonderman AB, Resnick SM (2013) Personality and resilience to Alzheimer’s disease neuropathology: a prospective autopsy study. Neurobiol Aging 34, 1045–1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [387].Farias ST, Chand V, Bonnici L, Baynes K, Harvey D, Mungas D, Simon C, Reed B (2012) Idea density measured in late life predicts subsequent cognitive trajectories: implications for the measurement of cognitive reserve. J Gerontol B Psychol Sci Soc Sci 67, 677–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [388].Farfel JM, Nitrini R, Suemoto CK, Grinberg LT, Ferretti RE, Leite RE, Tampellini E, Lima L, Farias DS, Neves RC, Rodriguez RD, Menezes PR, Fregni F, Bennett DA, Pasqualucci CA, Jacob Filho W (2013) Very low levels of education and cognitive reserve: a clinicopathologic study. Neurology 81, 650–657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [389].Del Ser T, Hachinski V, Merskey H, Munoz DG (1999) An autopsy-verified study of the effect of education on degenerative dementia. Brain 122 ( Pt 12), 2309–2319. [DOI] [PubMed] [Google Scholar]
- [390].Brayne C, Ince PG, Keage HA, McKeith IG, Matthews FE, Polvikoski T, Sulkava R (2010) Education, the brain and dementia: neuroprotection or compensation? Brain 133, 2210–2216. [DOI] [PubMed] [Google Scholar]
- [391].Koepsell TD, Kurland BF, Harel O, Johnson EA, Zhou XH, Kukull WA (2008) Education, cognitive function, and severity of neuropathology in Alzheimer disease. Neurology 70, 1732–1739. [DOI] [PubMed] [Google Scholar]
- [392].Erten-Lyons D, Woltjer RL, Dodge H, Nixon R, Vorobik R, Calvert JF, Leahy M, Montine T, Kaye J (2009) Factors associated with resistance to dementia despite high Alzheimer disease pathology. Neurology 72, 354–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [393].Yaffe K, Weston A, Graff-Radford NR, Satterfield S, Simonsick EM, Younkin SG, Younkin LH, Kuller L, Ayonayon HN, Ding J, Harris TB (2011) Association of plasma beta-amyloid level and cognitive reserve with subsequent cognitive decline. Jama 305, 261–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [394].Landau SM, Marks SM, Mormino EC, Rabinovici GD, Oh H, O’Neil JP, Wilson RS, Jagust WJ (2012) Association of lifetime cognitive engagement and low beta-amyloid deposition. Arch Neurol 69, 623–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [395].Oh H, Razlighi QR, Stern Y (2017) Multiple pathways of reserve simultaneously present in cognitively normal older adults. Neurology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [396].O’Shea DM, Fieo RA, Hamilton JL, Zahodne LB, Manly JJ, Stern Y (2015) Examining the association between late-life depressive symptoms, cognitive function, and brain volumes in the context of cognitive reserve. Int J Geriatr Psychiatry 30, 614–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [397].Steffener J, Barulli D, Habeck C, O’Shea D, Razlighi Q, Stern Y (2014) The role of education and verbal abilities in altering the effect of age-related gray matter differences on cognition. PLoS One 9, e91196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [398].Soldan A, Pettigrew C, Li S, Wang MC, Moghekar A, Selnes OA, Albert M, O’Brien R (2013) Relationship of cognitive reserve and cerebrospinal fluid biomarkers to the emergence of clinical symptoms in preclinical Alzheimer’s disease. Neurobiol Aging 34, 2827–2834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [399].Marques P, Moreira P, Magalhaes R, Costa P, Santos N, Zihl J, Soares J, Sousa N (2016) The functional connectome of cognitive reserve. Hum Brain Mapp 37, 3310–3322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [400].Stern Y, Zarahn E, Habeck C, Holtzer R, Rakitin BC, Kumar A, Flynn J, Steffener J, Brown T (2008) A common neural network for cognitive reserve in verbal and object working memory in young but not old. Cereb Cortex 18, 959–967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [401].Iacono D, Markesbery WR, Gross M, Pletnikova O, Rudow G, Zandi P, Troncoso JC (2009) The Nun study: clinically silent AD, neuronal hypertrophy, and linguistic skills in early life. Neurology 73, 665–673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [402].Perez-Nievas BG, Stein TD, Tai HC, Dols-Icardo O, Scotton TC, Barroeta-Espar I, Fernandez-Carballo L, de Munain EL, Perez J, Marquie M, Serrano-Pozo A, Frosch MP, Lowe V, Parisi JE, Petersen RC, Ikonomovic MD, Lopez OL, Klunk W, Hyman BT, Gomez-Isla T (2013) Dissecting phenotypic traits linked to human resilience to Alzheimer’s pathology. Brain 136, 2510–2526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [403].Beeri MS, Haroutunian V, Schmeidler J, Sano M, Fam P, Kavanaugh A, Barr AM, Honer WG, Katsel P (2012) Synaptic protein deficits are associated with dementia irrespective of extreme old age. Neurobiol Aging 33, 1125.e1121–1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [404].Head E, Corrada MM, Kahle-Wrobleski K, Kim RC, Sarsoza F, Goodus M, Kawas CH (2009) Synaptic proteins, neuropathology and cognitive status in the oldest-old. Neurobiol Aging 30, 1125–1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [405].Camicioli R, Howieson D, Oken B, Sexton G, Kaye J (1998) Motor slowing precedes cognitive impairment in the oldest old. Neurology 50, 1496–1498. [DOI] [PubMed] [Google Scholar]
- [406].Buracchio T, Dodge HH, Howieson D, Wasserman D, Kaye J (2010) The Trajectory of Gait Speed Preceding Mild Cognitive Impairment. Arch Neurol 67, 980–986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [407].Marquis S MMHDB, et al. (2002) INdependent predictors of cognitive decline in healthy elderly persons. Archives of Neurology 59, 601–606. [DOI] [PubMed] [Google Scholar]
- [408].Mielke MM, Roberts RO, Savica R, Cha R, Drubach DI, Christianson T, Pankratz VS, Geda YE, Machulda MM, Ivnik RJ, Knopman DS, Boeve BF, Rocca WA, Petersen RC (2012) Assessing the Temporal Relationship Between Cognition and Gait: Slow Gait Predicts Cognitive Decline in the Mayo Clinic Study of Aging. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [409].Verghese J, Lipton RB, Hall CB, Kuslansky G, Katz MJ, Buschke H (2002) Abnormality of Gait as a Predictor of Non-Alzheimer’s Dementia. New England Journal of Medicine 347, 1761–1768. [DOI] [PubMed] [Google Scholar]
- [410].Albers MW, Gilmore GC, Kaye J, Murphy C, Wingfield A, Bennett DA, Boxer AL, Buchman AS, Cruickshanks KJ, Devanand DP, Duffy CJ, Gall CM, Gates GA, Granholm AC, Hensch T, Holtzer R, Hyman BT, Lin FR, McKee AC, Morris JC, Petersen RC, Silbert LC, Struble RG, Trojanowski JQ, Verghese J, Wilson DA, Xu S, Zhang LI (2015) At the interface of sensory and motor dysfunctions and Alzheimer’s disease. Alzheimers Dement 11, 70–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [411].PBLPA Daviglus Ml, et al. (2011) Risk factors and preventive interventions for alzheimer disease: State of the science. Archives of Neurology 68, 1185–1190. [DOI] [PubMed] [Google Scholar]
- [412].Reitz C, Brayne C, Mayeux R (2011) Epidemiology of Alzheimer disease. Nat Rev Neurol 7, 137–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [413].Wilson RS, Segawa E, Buchman AS, Boyle PA, Hizel LP, Bennett DA (2012) Terminal Decline in Motor Function. Psych & Aging 4, 988–1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [414].Nadkarni NK, Lopez OL, Perera S, Studenski SA, Snitz BE, Erickson KI, Mathis CA, Nebes RD, Redfern M, Klunk WE (2017) Cerebral Amyloid Deposition and Dual-Tasking in Cognitively Normal, Mobility Unimpaired Older Adults. J Gerontol A Biol Sci Med Sci 72, 431–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [415].Tian Q, Resnick SM, Bilgel M, Wong DF, Ferrucci L, Studenski SA (2017) beta-Amyloid Burden Predicts Lower Extremity Performance Decline in Cognitively Unimpaired Older Adults. J Gerontol A Biol Sci Med Sci 72, 716–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [416].Del Campo N, Payoux P, Djilali A, Delrieu J, Hoogendijk EO, Rolland Y, Cesari M, Weiner MW, Andrieu S, Vellas B (2016) Relationship of regional brain beta-amyloid to gait speed. Neurology 86, 36–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [417].Wennberg AM, Savica R, Mielke MM (2017) Association between Various Brain Pathologies and Gait Disturbance. Dement Geriatr Cogn Disord 43, 128–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [418].Nadkarni NK, Perera S, Snitz BE, Mathis CA, Price J, Williamson JD, DeKosky ST, Klunk WE, Lopez OL (2017) Association of Brain Amyloid-beta With Slow Gait in Elderly Individuals Without Dementia: Influence of Cognition and Apolipoprotein E epsilon4 Genotype. JAMA Neurol 74, 82–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [419].Wolpert DM, Landy MS (2012) Motor control is decision-making. Curr Opin Neurobiol 22, 996–1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [420].Amboni M, Barone P, Hausdorff JM (2013) Cognitive contributions to gait and falls: Evidence and implications. Mov Disord 28, 1520–1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [421].Berg D, Postuma RB, Adler CH, Bloem BR, Chan P, Dubois B, Gasser T, Goetz CG, Halliday G, Joseph L, Lang AE, Liepelt-Scarfone I, Litvan I, Marek K, Obeso J, Oertel W, Olanow CW, Poewe W, Stern M, Deuschl G (2015) MDS research criteria for prodromal Parkinson’s disease. Mov Disord 30, 1600–1611. [DOI] [PubMed] [Google Scholar]
- [422].Gorelick PB, Scuteri A, Black SE, DeCarli C, Greenberg SM, Iadecola C, Launer LJ, Laurent S, Lopez OL, Nyenhuis D, Petersen RC, Schneider JA, Tzourio C, Arnett DK, Bennett DA, Chui HC, Higashida RT, Lindquist R, Nilsson PM, Roman GC, Sellke FW, Seshadri S (2011) Vascular Contributions to Cognitive Impairment and Dementia. Stroke 42, 2672–2713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [423].Triebel KL, Martin R, Griffith HR, Marceaux J, Okonkwo OC, Harrell L, Clark D, Brockington J, Bartolucci A, Marson DC (2009) Declining financial capacity in mild cognitive impairment: A 1-year longitudinal study. Neurology 73, 928–934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [424].Sinz H, Zamarian L, Benke T, Wenning GK, Delazer M (2008) Impact of ambiguity and risk on decision making in mild Alzheimer’s disease. Neuropsychologia 46, 2043–2055. [DOI] [PubMed] [Google Scholar]
- [425].Griffith HR, Dymek MP, Atchison P, Harrell L, Marson DC (2005) Medical decision-making in neurodegenerative disease: mild AD and PD with cognitive impairment. Neurology 65, 483–485. [DOI] [PubMed] [Google Scholar]
- [426].Zamarian L, Weiss EM, Delazer M (2011) The impact of mild cognitive impairment on decision making in two gambling tasks. J Gerontol B Psychol Sci Soc Sci 66, 23–31. [DOI] [PubMed] [Google Scholar]
- [427].Spreng RNP, Karlawish JM, Marson DCM (2016) Cognitive, social, and neural determinants of diminished decision-making and financial exploitation risk in aging and dementia: A review and new model. J Elder Abuse Negl 28, 320–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [428].Finucane ML, Gullion CM (2010) Developing a tool for measuring the decision-making competence of older adults. Psychol Aging 25, 271–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [429].Finucane ML, Mertz CK, Slovic P, Schmidt ES (2005) Task complexity and older adults’ decision-making competence. Psychol Aging 20, 71–84. [DOI] [PubMed] [Google Scholar]
- [430].Denburg NL, Tranel D, Bechara A (2005) The ability to decide advantageously declines prematurely in some normal older persons. Neuropsychologia 43, 1099–1106. [DOI] [PubMed] [Google Scholar]
- [431].Denburg NL, Cole CA, Hernandez M, Yamada TH, Tranel D, Bechara A, Wallace RB (2007) The orbitofrontal cortex, real-world decision making, and normal aging. Ann N Y Acad Sci 1121, 480–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [432].Deakin J, Aitken M, Robbins T, Sahakian BJ (2004) Risk taking during decision-making in normal volunteers changes with age. J Int Neuropsychol Soc 10, 590–598. [DOI] [PubMed] [Google Scholar]
- [433].Smith SG, Jackson SE, Kobayashi LC, Steptoe A (2017) Social Isolation, Health Literacy, and Mortality Risk: Findings From the English Longitudinal Study of Ageing. Health Psychol. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [434].Baker DW, Wolf MS, Feinglass J, Thompson JA (2008) Health literacy, cognitive abilities, and mortality among elderly persons. J Gen Intern Med 23, 723–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [435].Eppinger B, Schuck NW, Nystrom LE, Cohen JD (2013) Reduced striatal responses to reward prediction errors in older compared with younger adults. J Neurosci 33, 9905–9912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [436].Halfmann K, Hedgcock W, Kable J, Denburg NL (2016) Individual differences in the neural signature of subjective value among older adults. Soc Cogn Affect Neurosci 11, 1111–1120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [437].Rogalsky C, Vidal C, Li X, Damasio H (2012) Risky decision-making in older adults without cognitive deficits: an fMRI study of VMPFC using the Iowa Gambling Task. Soc Neurosci 7, 178–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [438].Samanez-Larkin GR, Kuhnen CM, Yoo DJ, Knutson B (2010) Variability in nucleus accumbens activity mediates age-related suboptimal financial risk taking. J Neurosci 30, 1426–1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [439].Matthews SC, Simmons AN, Lane SD, Paulus MP (2004) Selective activation of the nucleus accumbens during risk-taking decision making. Neuroreport 15, 2123–2127. [DOI] [PubMed] [Google Scholar]
- [440].Cummings JL, Morstorf T, Zhong K (2014) Alzheimer’s disease drug-development pipeline: few candidates, frequent failures. Alzheimers Res Ther 6, 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [441].Gauthier S, Albert M, Fox N, Goedert M, Kivipelto M, Mestre-Ferrandiz J, Middleton LT (2016) Why has therapy development for dementia failed in the last two decades? Alzheimers Dement 12, 60–64. [DOI] [PubMed] [Google Scholar]
- [442].Sloane PD, Zimmerman S, Suchindran C, Reed P, Wang L, Boustani M, Sudha S (2002) The public health impact of Alzheimer’s disease, 2000–2050: potential implication of treatment advances. Annu Rev Public Health 23, 213–231. [DOI] [PubMed] [Google Scholar]
- [443].Cummings J, Lee G, Mortsdorf T, Ritter A, Zhong K (2017) Alzheimer’s disease drug development pipeline: 2017. Alzheimers Dement (N Y) 3, 367–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [444].Future Cases of Dementia among People Born in 2015 & the Dementia Drug Pipeline, https://www.ohe.org/news/future-cases-dementia-among-people-born-2015-dementia-drug-pipeline, Accessed 01/18/2018.
- [445].Reiman EM, Langbaum JB, Fleisher AS, Caselli RJ, Chen K, Ayutyanont N, Quiroz YT, Kosik KS, Lopera F, Tariot PN (2011) Alzheimer’s Prevention Initiative: a plan to accelerate the evaluation of presymptomatic treatments. J Alzheimers Dis 26 Suppl 3, 321–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [446].Mills SM, Mallmann J, Santacruz AM, Fuqua A, Carril M, Aisen PS, Althage MC, Belyew S, Benzinger TL, Brooks WS, Buckles VD, Cairns NJ, Clifford D, Danek A, Fagan AM, Farlow M, Fox N, Ghetti B, Goate AM, Heinrichs D, Hornbeck R, Jack C, Jucker M, Klunk WE, Marcus DS, Martins RN, Masters CM, Mayeux R, McDade E, Morris JC, Oliver A, Ringman JM, Rossor MN, Salloway S, Schofield PR, Snider J, Snyder P, Sperling RA, Stewart C, Thomas RG, Xiong C, Bateman RJ (2013) Preclinical trials in autosomal dominant AD: implementation of the DIAN-TU trial. Rev Neurol (Paris) 169, 737–743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [447].Sperling RA, Rentz DM, Johnson KA, Karlawish J, Donohue M, Salmon DP, Aisen P (2014) The A4 study: stopping AD before symptoms begin? Sci Transl Med 6, 228fs213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [448].Anderson RM, Hadjichrysanthou C, Evans S, Wong MM (2017) Why do so many clinical trials of therapies for Alzheimer’s disease fail? Lancet 390, 2327–2329. [DOI] [PubMed] [Google Scholar]
- [449].Buchman AS, Schneider JA, Leurgans S, Bennett DA (2008) Physical frailty in older persons is associated with Alzheimer disease pathology. Neurology 71, 499–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [450].Wilson RS, Leurgans SE, Boyle PA, Schneider JA, Bennett DA (2010) Neurodegenerative basis of age-related cognitive decline. Neurology 75, 1070–1078. [DOI] [PMC free article] [PubMed] [Google Scholar]