Abstract
Severe fever with thrombocytopenia syndrome (SFTS) is an emerging infectious disease localized to China, Japan, and Korea that is characterized by severe hemorrhage and a high fatality rate. Currently, no specific vaccine or treatment has been approved for this disease. To develop a therapeutic agent for SFTS, we isolated antibodies from a phage-displayed antibody library that was constructed from a patient who recovered from SFTS virus (SFTSV) infection. One antibody, designated as Ab10, was reactive to the Gn envelope glycoprotein of SFTSV and protected host cells and A129 mice from infection in both in vitro and in vivo experiments. Notably, Ab10 protected 80% of mice, even when injected 5 days after inoculation with a lethal dose of SFTSV. Using cross-linker assisted mass spectrometry and alanine scanning, we located the non-linear epitope of Ab10 on the Gn glycoprotein domain II and an unstructured stem region, suggesting that Ab10 may inhibit a conformational alteration that is critical for cell membrane fusion between the virus and host cell. Ab10 reacted to recombinant Gn glycoprotein in Gangwon/Korea/2012, HB28, and SD4 strains. Additionally, based on its epitope, we predict that Ab10 binds the Gn glycoprotein in 247 of 272 SFTSV isolates previously reported. Together, these data suggest that Ab10 has potential to be developed into a therapeutic agent that could protect against more than 90% of reported SFTSV isolates.
Author summary
Severe fever with thrombocytopenia syndrome (SFTS) is an emerging infectious disease localized to China, Japan, and Korea. The tick-borne virus that causes SFTS has infected more than 5,000 humans, with a 6.4% to 20.9% fatality rate. Currently, there are no prophylactic or therapeutic measures against this virus. Historically, antibodies from patients who recovered from viral infection have been used to treat new patients, and commercially available antiviral monoclonal antibodies have been developed. Palivizumab was approved for the prophylaxis of respiratory syncytial virus (RSV) infection, and ibalizumab-uiyk was recently approved for the treatment of human immunodeficiency virus (HIV)-infected patients. To develop an antiviral monoclonal antibody for SFTS patients, we selected 10 antibodies from a patient who recovered from SFTS and found that one antibody potently inhibited SFTS viral infection both in vitro and in animal studies. We mapped the binding site of this antibody on the SFTS virus, which allowed us to predict that this antibody could bind 247 out of the 272 SFTS virus isolates reported to date. We anticipate that this antibody could be developed into a therapeutic treatment against SFTS.
Introduction
Since its isolation as a novel virus in 2011, cases of the acute infectious disease called severe fever with thrombocytopenia syndrome (SFTS)[1] have risen rapidly in China, Japan, and Korea, posing a risk to public health and increasing the fear of ticks that transmit the deadly SFTS virus (SFTSV). From 2011 to 2016, this emerging tick-borne virus infected 5,360 people in China with an average case fatality rate of 6.40%[2]. After initial reports in 2013 of sporadic SFTS cases in South Korea[3] and Japan[4], South Korea reported 605 cases with an average case fatality of 20.9%[5] and Japan reported 310 cases with an average fatality of 19.4%[6] from 2013 to 2017.
Ticks such as Haemaphysalis longicornis and Rhipicephalus microplus are implicated as the prominent vectors for transmitting SFTSV[7]. With regards to SFTSV hosts, various vertebrate species are considered to have been infected, as evidenced by high SFTSV seroprevalence in domestic animals in SFTS endemic regions[8,9]. Additionally, reported cases of human-to-human transmission through contact with blood or body fluid, including infections in healthcare workers from patients, pose a further threat to the public[10,11]. Furthermore, the discovery of H. longicornis tick in the United States indicates the possibility that SFTSV could spread to other continents, highlighting the need to prevent disease transmission[12].
SFTSV is a single-stranded negative-sense tripartite RNA virus that is classified as a member of the Phlebovirus genus, Phenuiviridae family, and Bunyaviriales order. The genome of SFTSV is comprised of L, M, and S segments, which encode the RNA-dependent RNA polymerase (L segment), envelope Gn glycoprotein (M segment), envelope Gc glycoprotein (M segment), nucleoprotein (S segment), and nonstructural proteins (S segment)[13]. A phylogenetic analysis based on genome sequences of SFTSV isolates found substantial genetic diversity and accumulated mutations, suggesting that SFTSV has existed for decades at minimum[14,15]. However, the difference in virulence between these SFTSV sub-lineages has yet to be determined.
The major clinical features of SFTS include high fever (body temperature ≥38°C), fatigue, malaise, anorexia, nausea, vomiting, diarrhea, thrombocytopenia, leukocytopenia, and abdominal pain[16,17]. In severe cases, SFTS can include central nervous system manifestations, hemorrhagic signs, and multiple organ dysfunction, which can lead to death[18–21]. No vaccines or therapeutics specific for SFTS have been approved for human use. Recently, a Phase 3 clinical trial of favipiravir (Avigan), a drug approved for the treatment of influenza virus infection in Japan, was initiated to expand its indication to SFTS treatment[22]. Monoclonal antibodies or convalescent sera from SFTS patients were tested to identify potential therapeutic intervention targets, resulting in the identification of SFTSV glycoproteins as molecules required for host cell entry[23,24] and also as critical targets for virus neutralization through the development of humoral immunity. Both the Gn and Gc envelope glycoproteins of SFTSV are type I transmembrane proteins, and Gc is proposed to be a membrane fusion protein critical for SFTSV infection[25]. This has also been shown in Rift Valley fever virus (RVFV)[26], which is a well-known phlebovirus, whereas the function of Gn remains largely elusive across all other species in the genus Phlebovirus. The structure of the Gn head domain, which is composed of three subdomains, was resolved in SFTSV and RVFV[27]. However, the homology and arrangement within subdomains differ considerably between the two viruses, and the structure of the Gn stem domain still remains unknown. Moreover, the generation of an antibody for these targets in infected humans is rare, due to the presence of immunodominant decoy epitopes in the nucleoprotein[28], which is a common phenomenon in a pathogenic virus-infected host[29]. In animal models, however, the protective effect of human convalescent sera was shown, suggesting that antibody therapy is possible[30]. Thus far, MAb4-5 is the only human neutralizing monoclonal antibody reported, and it was developed using a combinatorial human antibody library from five patients[31]. MAb4-5 binds to domain III of SFTSV Gn glycoprotein[27]. The neutralizing effect of MAb4-5 has been shown only in in vitro, and its in vivo efficacy remains to be shown.
In this study, we constructed an antibody library from a patient who recovered from SFTS and selected antibodies against the Gn and Gc glycoproteins. Among these antibodies, Ab10 bound to Gn glycoprotein and showed a potent neutralizing effect in vitro and protective effect in vivo. In addition, we characterized the conformational epitope of Ab10 using crosslinking coupled mass spectrometry and by testing its reactivity to alanine mutants, which allowed us to estimate the strain coverage of Ab10.
Results
Anti-Gn/Gc glycoprotein antibodies were selected from an antibody library generated from a convalescent SFTS patient
In human embryonic kidney (HEK) 293F cells, we produced Gn and Gc glycoproteins fused with a crystallizable fragment of the human immunoglobulin (Ig) heavy chain constant region (Gn-Fc and Gc-Fc) or those fused with the human Ig kappa light chain constant region (Gn-Cκ and Gc-Cκ) and then purified the proteins by affinity chromatography. We constructed the phage-displayed single-chain variable fragment (scFv) antibody library with a complexity of 1.3 × 109 colony forming units using peripheral blood mononuclear cells isolated from a patient who had recovered from SFTS. The phage-display antibody library with a coverage level of 730× was subjected to four rounds of biopanning against either the recombinant Gn-Fc or the Gc-Fc fusion proteins conjugated to paramagnetic beads. We randomly selected phagemid clones from the output titer plate from the last round of biopanning and subjected these clones to phage enzyme-linked immunosorbent assay (ELISA). To minimize the number of clones reactive to the Fc portion of fusion proteins, Gn-Cκ and Gc-Cκ were used as antigens. Positive clones were selected and subjected to Sanger sequencing to determine the scFv nucleotide sequence. We identified five clones reactive to Gn and five clones reactive to Gc. All of these scFv clones were expressed as a scFv antibody fused with Fc (scFv-Fc) in HEK293F cells and purified by affinity.
Ab10 mAb potently inhibited the amplification of SFTSV in vitro
We tested 10 antibodies for their ability to reduce cytopathic effects (CPE) caused by SFTSV (S1 Fig). One anti-Gn antibody, designated as Ab10, was extremely effective at neutralizing SFTSV, as shown by a reduction in the percentage of cells showing CPE from 90% to 10%. In the focus reduction neutralization test (FRNT), Ab10 also showed significantly higher potency compared to the other candidate antibodies (S2 Fig). The VH sequences of Ab10 had a 95.9% shared identity with the IGHV3-30*18 germline, excluding the heavy chain complementary determining region (HCDR) 3, whereas the Vκ sequence had 86.3% shared identity with the IGKV1-39*01 germline (S3 Fig).
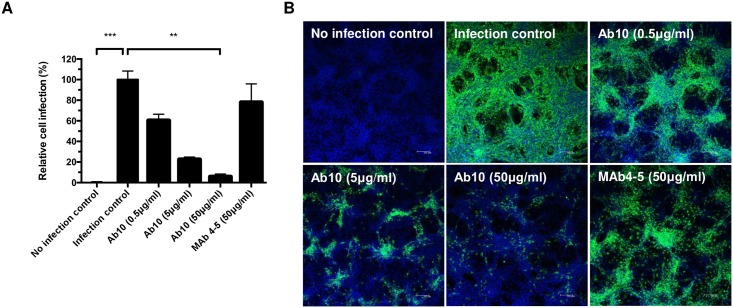
In an immunofluorescence assay (IFA) using Vero cells and an anti-Gn antibody, we determined the proportion of Gn glycoprotein producing cells, which were infected with SFTSV, to measure the neutralizing potency of Ab10. Only 5.6 ± 2.8% (mean ± s.d.) of Vero cells produced Gn glycoprotein when Ab10 was administered at a concentration of 50 μg/mL (956 nM) (Fig 1). When MAb4-5 antibody was applied at the same concentration, 77.8 ± 18.0% of the cells produced Gn glycoprotein. When cells were not protected by any antibody, all cells produced Gn glycoprotein and cells not incubated with SFTSV did not produce Gn glycoprotein.
Fig 1. Ab10 has in vitro neutralizing activity against severe fever with thrombocytopenia syndrome virus (SFTSV).
To measure neutralizing efficacy, Ab10 scFv-Fc fusion protein was mixed with 100 TCID50 of SFTSV (strain: Gangwon/Korea/2012) and added to Vero cells. After incubation for 1 h, the cells were washed and cultured for 2 days. Then, the Gn glycoprotein produced in infected Vero cells was detected in an immunofluorescence assay using anti-SFTSV Gn glycoprotein antibody, which did not compete with Ab10 in its binding, with at least five technical replicates. The fluorescence signal intensity of stained SFTSV Gn glycoprotein was used as a quantitative indicator for viral infection. (A) The proportion of infected cells compared to non-treated cells was defined as relative cell infection (%) and was plotted. Mab4-5 scFv-Fc fusion protein was also treated in a parallel experiment. Error bars represent standard deviations (s.d.), asterisks indicate a statistically significant difference as determined by a nonparametric Friedman test with a post hoc Dunn’s multiple comparison test (* P ≤ 0.05, ** P ≤ 0.01, *** P ≤ 0.001, **** P ≤ 0.0001). (B) Representative images of each treatment group are shown (scale bar, 100 μm). SFTSV Gn glycoprotein and nuclei were stained with FITC (green) and DAPI (blue), respectively.
Ab10 protected mice from SFTSV infection, even with treatment delayed up to 3 days
For the animal study, the lethal dose of the Gangwon/Korea/2012 strain of SFTSV was determined in type I interferon (interferon α/β) receptor gene (IFNAR1)-deficient A129 mice (n = 4 per group). The mice were subcutaneously injected with a dose of either 20 or 2 × 105 plaque forming units (PFUs), and the mortality of mice was monitored (S4 Fig). Because all mice died at 7 days post-infection (d.p.i.) even when injected with only 20 PFU, doses of 2 and 20 PFU were chosen for further studies.
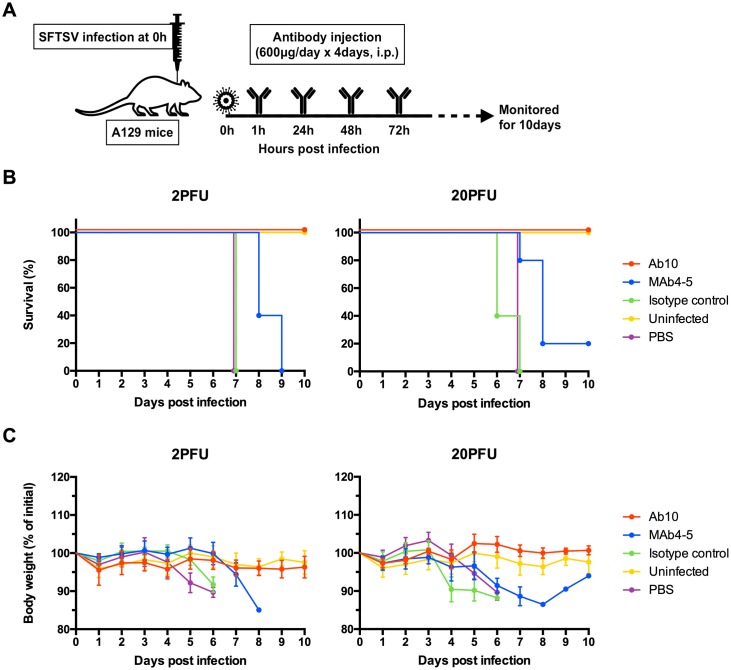
Using the antibody protection model, A129 mice (n = 5 per group) were subcutaneously injected with the Gangwon/Korea/2012 strain of SFTSV at a dose of either 2 or 20 PFU. After 1 h, mice were intraperitoneally administered with either phosphate-buffered saline (PBS), Ab10, MAb4-5, or a human IgG1 isotope control antibody at a dose of 600 μg (approximately corresponding to 30 mg/kg of body weight); for 4 days at 24 h intervals, the injection of the same amount of antibody was performed (Fig 2A).
Fig 2. Ab10 protected mice from SFTSV infection.
The overall scheme for the administration of virus and antibody is described in (A). Eight-week-old A129 mice (n = 5 per group) were inoculated with 2 or 20 PFU of SFTSV through a subcutaneous route. At 1, 24, 48, and 72 h post-infection, infected mice were intraperitoneally administered with 600 μg of Ab10, MAb4-5, IgG1 isotype control antibody, or PBS vehicle control. Percentages of survival (B) and body weight relative to the day of virus inoculation (C) were monitored daily until 10 days post-infection. Survival was determined by the Kaplan-Meier method. Relative body weight values in (C) are presented as the means with standard deviations of surviving mice in each group.
In the groups treated with PBS or an isotype control antibody, all mice died within 7 days at both viral doses (Fig 2B and 2C). At 4 d.p.i. with a dose of 2 PFU, approximately 10% of body weight was lost; at 3 d.p.i. with 20 PFU, 10–15% of body weight was lost. All mice treated with Ab10 survived both viral doses and did not have any weight loss. With MAb4-5 treatment, death occurred in all mice treated with a 2 PFU viral dose and in 80% of mice treated with a 20 PFU dose. Significant weight losses were also observed in all these mice.
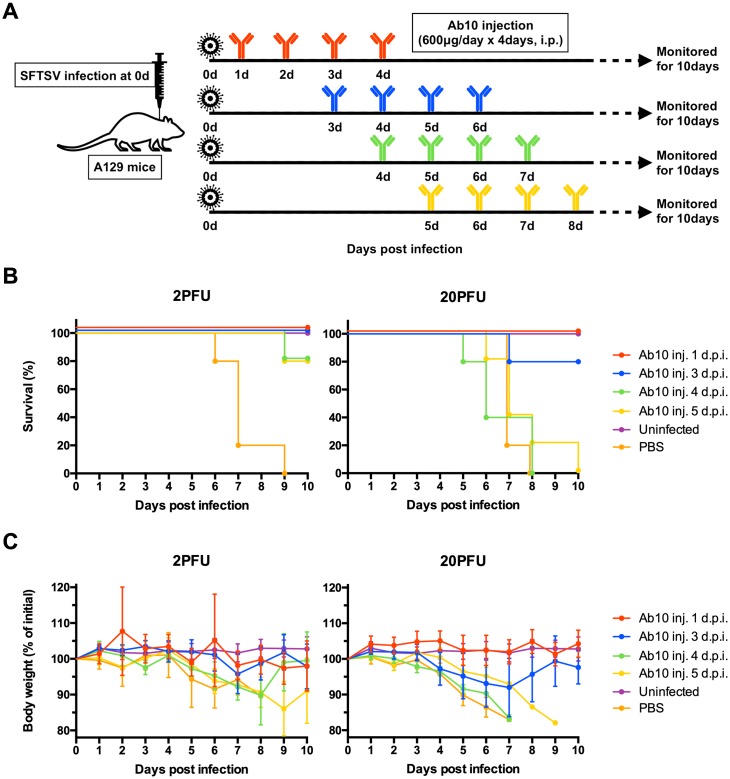
In the delayed treatment model, the antibody treatment started from 1, 3, 4, or 5 d.p.i. and continued for 4 consecutive days (Fig 3A). At a 2 PFU viral dose, all mice survived when treatments with Ab10 were delayed until 3 d.p.i., and 80% survived when the treatments were delayed until 4 or 5 d.p.i. (Fig 3B and 3C). Mice not treated until 4 d.p.i. had significant weight loss. At a 20 PFU viral dose, delaying Ab10 antibody treatment until 1 or 3 d.p.i. protected all or 80% of mice, respectively. Mice with treatment delayed until 1 d.p.i. did not lose weight, whereas mice with treatment delayed until 3 d.p.i. lost 8% of their body weight. When treatment was delayed until 4 d.p.i. or later, all the mice died.
Fig 3. Delayed administration of Ab10 also protected mice from SFTSV infection up to 3 days after inoculation of the virus.
The overall scheme for the virus challenge and delayed antibody administration is described in (A). Eight-week-old A129 mice (n = 5 per group) were inoculated with 2 or 20 PFU of SFTSV through a subcutaneous route. From 1, 3, 4, or 5 days post-infection, infected mice were intraperitoneally administered with 600 μg of Ab10 per day for 4 consecutive days. Percentages of survival (B) and weight relative to the day of virus inoculation (C) were monitored daily until 10 days post-infection. Survival was determined by the Kaplan-Meier method. The values in (C) are presented as the means with standard deviations of surviving mice in each group.
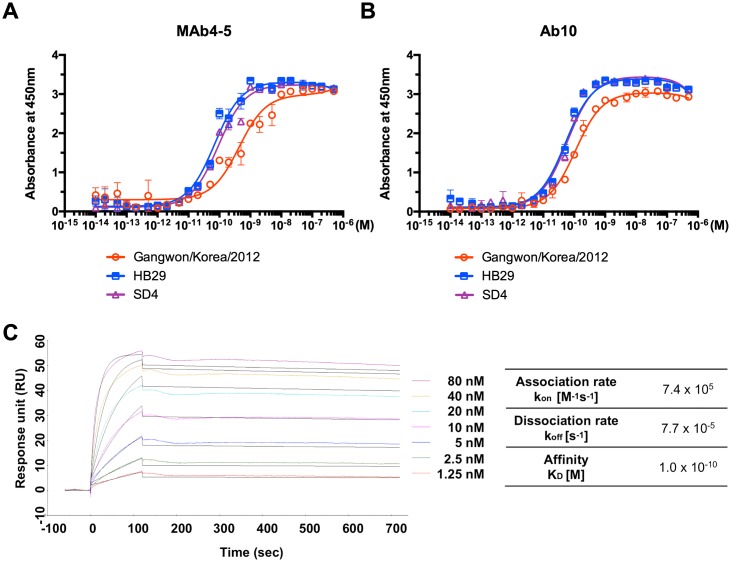
Ab10 binds to recombinant Gn glycoprotein with high affinity in a broad variety of strains
To check the reactivity of Ab10 to SFTSV strains other than Gangwon/Korea/2012, we overexpressed and purified recombinant Gn glycoproteins of other SFTSV strains. Binding of Ab10 to intact virus particles was also confirmed using an ELISA with a virus-coated microtiter plate (S5 Fig). Among the 272 SFTSV strain sequences deposited in the Virus Pathogen Database and Analysis Resource (ViPR), we selected the strains HB29, AH15, SD4, and YG1, each belong to different clusters (S6 Fig), to compare their reactivity with well-known virus isolates from China and Japan. We successfully overexpressed Gn glycoprotein from HB29 and SD4 as a Fc fusion protein and subjected these proteins to ELISAs. Ab10 IgG1 successfully bound to Gn glycoproteins from the HB29 and SD4 strains in a dose-dependent manner at concentrations ranging from 10 pM to 1 nM (Fig 4A). Additionally, the amount of antibody bound to the HB29 and SD4 Gn glycoproteins coated on the ELISA plate was higher than that of the Gangwon/Korea/2012 glycoproteins, at most of the tested concentrations. We also found that MAb4-5 was reactive to Gn glycoprotein from the HB29 and SD4 strains (Fig 4B).
Fig 4. Ab10 also bound to Gn glycoprotein of HB29 and SD4 strains with comparable affinity to that of Gangwon/Korea 2012.
Binding properties of human IgG1 monoclonal antibody Ab10 (A) and MAb4-5 (B) to the recombinant Gn glycoprotein ectodomain of Gangwon/Korea 2012, HB29, and SD4 strains were measured by enzyme-linked immunosorbent assay (ELISA). Non-linear regression curves were fitted to a one site specific saturation binding model and the mean absorbance at 450 nm with standard deviation (s.d.) error bars are shown at each antibody concentration. (C) Surface plasmon analysis of Ab10 antibody was performed on the CM5 chip with an immobilized anti-histidine antibody binding to a poly-histidine tagged SFTSV Gn ectodomain. The experimental data at concentrations of 80, 40, 20, 10, 5, 2.5, and 1.25 nM Ab10 antibody are shown in color, and the fitted curves are shown in black. Calculated rate constants are shown in the table.
We used surface plasmon resonance analyses to determine the kinetics of Ab10 binding to the Gn glycoprotein of Gangwon/Korea/2012. Ab10 bound to Gn glycoprotein with an equilibrium dissociation constant (KD) of 104 pM and with an association rate (kon) of 7.4 × 105 M-1s-1 and a dissociation rate (koff) of 7.7 × 10−5 s-1 (Fig 4C).
Ab10 binds to a non-linear epitope on domain II and the stem region of the Gn glycoprotein
In an immunoblot analysis using recombinant Gn glycoprotein from the Gangwon/Korea/2012 strain, Ab10 did not react to Gn glycoprotein, whereas some other anti-Gn antibodies were reactive (S7 Fig). Based on this observation, we assumed that the antibody reacted to a non-linear epitope.
To discover the site where Ab10 binds, we performed crosslinking coupled mass spectrometry using a deuterium isotope-labeled homo-bifunctional linker, which forms covalent bonds between amino acid residues within the interface of the antibody-antigen complex as described previously[32]. We found that cross-linkers bound to five amino acid residues (318Y, 324R, 326K, 328Y, and 331S) within domain II of the SFTSV Gn glycoprotein and also to four amino acid residues (371K, 372S, 379H, and 383S) within the stem region (Fig 5A).
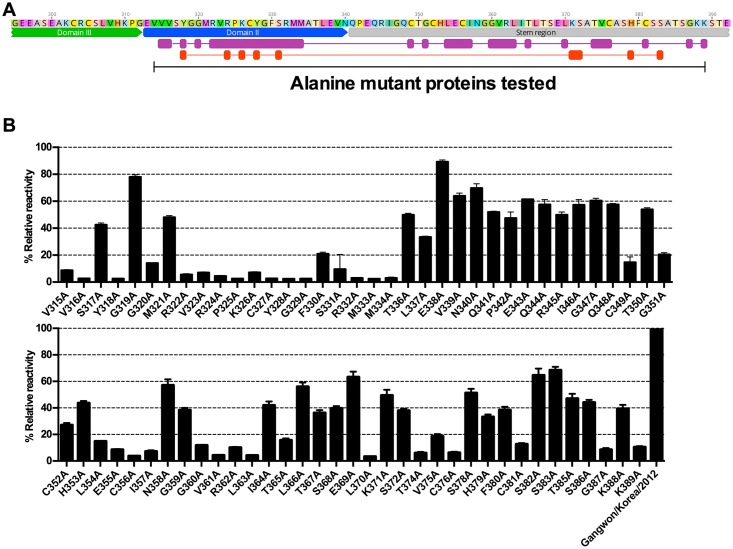
Fig 5. The epitope of Ab10 was determined by alanine mutant analysis.
The conformational epitope of Ab10 antibody on the Gn glycoprotein ectodomain was determined by measuring antibody binding activity to recombinant mutant proteins with amino acid residues that were substituted with alanine at residues corresponding to 315–389. (A) Epitopes predicted by cross-linker assisted mass spectrometry are shown in red, and alanine substituted residues that affected Ab10 antibody binding are shown in purple. The overlapping domain II (blue annotation) and region upstream of the stem region (gray annotation) are also indicated. (B) The reactivity of Ab10 to each alanine mutant is represented as relative reactivity, which was calculated using absorbance values (Abs) as follows: % Relative reactivity = [100 × {(Abs of mutant captured by Ab10) / (Abs of mutant captured by HA antibody)} / {(Abs of wildtype captured by Ab10) / (Abs of wildtype captured by HA antibody)}]. Bars indicate the mean and standard deviation (s.d.).
Based on this observation, we prepared several alanine-replacement mutants that spanned from 315V to 389K, and tested their reactivity to Ab10 using ELISAs. All the mutants were expressed with an HA peptide at the carboxy terminus and the tags were used to measure the relative amount of each mutant. Alanine mutant proteins were captured by the Ab10 antibody, which was coated on the ELISA plate. Then, we measured the amount of captured mutant proteins by detecting the Fc portion of protein. The signals detected by capturing the HA peptide were used to normalize expression of mutant proteins. We measured the reactivity of Ab10 to alanine mutant Gn proteins, relative to wild type Gn glycoprotein, and found that alanine replacement of the amino acid residues in domain II from V315 to M334 resulted in reduced relative reactivity of Ab10 by more than 60%, except for S317, G319, and M321. This finding was consistent with our results deduced from the crosslinking coupled mass spectrometry (Fig 5A and 5B).
In the stem region, replacing the cystine residues (C349, C356, C376, and C381) reduced the relative reactivity by more than 80%. This observation was consistent with a previous report that the structural stability of Gn was disrupted by a C356A mutation[27]. Also, mutation of the flanking residues of cystine, corresponding to G351, L354, E355, I357, T374, and V375 also reduced the reactivity by over 60%. Of the mutated residues that were distant from cysteine residues, mutation of G360, V361, R362, L363, T365, L370, G387, and K389 residues reduced the relative reactivity by more than 80%. The other mutations had minor effects on reactivity. Overall, Ab10 binding to Gn was predicted to be affected by 25 amino acid residues within domain II and the stem region of SFTSV Gn glycoprotein. Given that Gn glycoproteins from 247 isolates have conserved sequences for these 25 amino acid residues, we expect that Ab10 can react with 90.8% (247 out of 272) of SFTSV isolates currently reported (S8 Fig).
Discussion
Antibodies play a pivotal role in preventing viral entry into cells and can induce lysis of infected cells through antibody-dependent cellular cytotoxicity or complement-dependent cytotoxicity[33–35]. Polysera from recovered patients or from vaccinated donors have been used as prophylactic agents for various viral diseases, including hepatitis B and rabies[36]. As an alternative approach, virus-directed monoclonal antibodies have also been developed and tested as therapies or as prophylaxis for viral diseases. Palivizumab (Synagis) was market-approved for the prophylaxis of RSV in 1998. In addition, antibodies against HIV[37–39], RSV[40], Ebola virus[41] and influenza virus[42,43] demonstrated potent efficacy in animal models. Antibodies targeting emerging or re-emerging viruses including MERS-CoV[44–46] and Zika virus[47–49] were also developed and are being tested in clinical trials. In the past several decades, antibodies have become one of the major therapeutic agents for cancer and autoimmune disease with indications that have rapidly broadened in recent years. Recent technical improvements in the discovery and manufacturing steps of therapeutic antibody production have also allowed rapid and successful antibody development to combat emerging infectious diseases[50].
Until now, SFTS patients have been reported from China, South Korea, and Japan, and the number of patients has increased each year[2,5,6]. However, SFTS fatality varies among the three countries[21]. The average case fatality rate in China from 2011 to 2016 was 6.40%[2]. Those in South Korea and Japan after 2013 were much higher; 20.9%[5] and 19.4%[6], respectively. In the Virus Pathogen Database and Analysis Resource (ViPR), 272 sequences of SFTSV isolates are currently deposited. However, it is unknown if there is any significant variability in the virulence of these isolates. Previous reports showed that mice died 5 to 7 days after infection with 106 focus forming units (FFU) of the YG1 strain[30] or 106 TCID50 of the SPL010 strain[51]. Based on these observations, we first inoculated A129 mice with 2 × 105 PFU of the Gangwon/Korea/2012 strain and observed that all mice died 4 days after infection. With a 20 PFU dose of the Gangwon/Korea/2012 strain, mice died 5 to 7 days after infection. This increased virulence was also reported by a study that showed a similar fatality rate in STAT2 knockout Syrian hamsters challenged with 10 PFU of the HB29 strain[52].
We have also observed a discrepancy in the body weights at death between our study and that of another group. In our data, A129 mice died after losing 15% of their body weight. But in a study using the SPL010 strain, mice died after losing 30% of their body weight[51]. These results might be due to a difference in virulence between the strains. Such differences in virulence between strains of the RVFV, a phlebovirus similar to SFTSV, have been reported[53].
The mechanisms of antibody inhibition of viral replication inside host cells have been studied extensively, especially in the case of influenza virus. The most-widely known mechanism is binding of an antibody to the portion of the virus that interacts with the host cell receptor, thereby blocking the interaction between the virus and the host cell[54]. Another group of antibodies was reported to bind the stem region of influenza hemagglutinin that is critical for conformational rearrangements that occur during membrane fusion[55–57]. This mechanism has more potential to be utilized for clinical development, because the stem region has fewer mutations than the receptor binding site. Additionally, several groups, including ours, have elucidated unconventional virus neutralizing mechanisms that affect the infection steps that occur after membrane fusion[58,59].
In our crosslinking coupled mass spectrometry and alanine mutant studies, the Ab10 epitope was confined to domain II and the stem region of the Gn glycoprotein. Although the crystal structure of the phlebovirus Gn glycoprotein stem region has not yet been solved, a recent report showed a cryo-electron microscopy map of RVFV, and depicted the crystal structure of the RVFV Gn glycoprotein head region without a stem region[60]. The report also describes the membrane fusion mechanism of RVFV that is mediated by a low pH induced exposure of the hydrophobic Gc fusion loop. At a neutral pH, the Gn domain II (β-ribbon domain) shields the Gc fusion loop in the pre-fusion state and prevents premature fusion. Based on this report, we hypothesize that Ab10 simultaneously binds to domain II and the stem region of the Gn glycoprotein and prevents un-shielding of the Gc fusion loop.
In conclusion, Ab10 is a monoclonal antibody that has shown therapeutic efficacy in a mouse SFTSV infection model. Although the neutralization efficacy of Ab10 was only tested in the Gangwon/Korea/2012 strain that was cultured in Vero cells, we confirmed its binding capability to recombinant SFTSV Gn in the HB29 and SD4 strains, which are both from China. According to the epitope revealed in this study, Ab10 is estimated to interact with the majority of SFTSV isolates currently reported. Based on these results, we believe that Ab10 has sufficient potential to be developed as a prophylactic and therapeutic agent for a broad variety of SFTS isolates.
Materials and methods
Ethics statements: Human subjects and animal models
The studies involving recovered patient’s blood samples were reviewed and approved by the Institutional Ethics Review Board of Seoul National University Hospital (IRB approval number: 1405-031-576). All of the patients were adults and submitted written informed consent. All animal studies were conducted in an Animal Biosafety Level 3 (ABSL-3) facility at the Institut Pasteur Korea according to the principles established by the Animal Protection Act and the Laboratory Animal Act in Republic of Korea. Interferon α/β receptor knockout (IFNAR1-/-, A129) mice (B&K Universal, Hull, UK) were bred, raised, and genotyped at the Institut Pasteur Korea. All experimental procedures were reviewed and approved by the Institutional Animal Care and Use Committee at the Institut Pasteur Korea (Animal protocol number: IPK-17003-1).
Production of recombinant SFTSV Gn/Gc glycoprotein fusion proteins
The SFTSV Gn glycoprotein amino acid sequences of various isolates used in this study were retrieved from the Virus Pathogen Database and Analysis Resource (ViPR). To obtain SFTSV Gn glycoprotein ectodomain coding DNA strands, human codon optimized DNA sequences corresponding to amino acid sequences from 20 to 452 of GenBank Accession No. ADZ04471 (Strain HB29), ADZ04477 (Strain SD4), ADZ04486 (Strain AH 15), BAN58185 (Strain YG1), AGT98506 (Strain Gangwon/Korea/2012) were synthesized (GenScript, Piscataway, NJ, USA and Integrated DNA Technologies, Coralville, IA, USA). Human codon optimized DNA sequence of SFTSV Gc ectodomain of strain Gangwon/Korea/2012, corresponding to the sequence from 563 to 1035 of AGT98506, was also synthesized. For the overexpression and purification of recombinant SFTSV Gn/Gc glycoprotein ecotodomain fused to the Fc region of human immunoglobulin heavy constant gamma1 (IGHG1), termed Gn-Fc/Gc-Fc, or fused to the human immunoglobulin kappa constant region (IGKC), termed Gn-Cκ/Gn-Cκ, SFTSV Gn/Gc glycoprotein ectodomain encoding genes were cloned into the modified pCEP4 vector (V04450, Invitrogen, Carlsbad, CA, USA) with a leader sequence of the human immunoglobulin kappa chain, two Sfil restriction enzyme sites, and the Fc region of human IGHG1 or human immunoglobulin kappa constant region, as previously described[61,62]. Subsequently, the vectors were used to transfect HEK 293F (R79007, Invitrogen) or Expi293F cells (A14527, Invitrogen) using polyethylenimine (23966–1; Polysciences, Warrington, PA, USA), then the transfected cells were cultured in FreeStyle 293 expression medium (12338026; Gibco, Thermo Fisher Scientific, Waltham, MA, USA). Overexpressed recombinant SFTSV Gn and Gc glycoprotein fusion proteins were purified by affinity chromatography using MabSelect or KappaSelect columns with the ÄKTA Pure chromatography system (11003495, 17545811, 29018225; GE Healthcare, Chicago, IL, USA), following the protocol provided by the manufacturer.
For alanine-scanning mutagenesis, SFTSV Gn glycoprotein with amino acid residues (315–389) substituted with alanine were produced by cloning synthesized DNA fragments (Integrated DNA Technologies) into a modified pCEP4 vector, as described above. Subsequently, influenza hemagglutinin (HA) tag sequence (YPYDVPDYA) was introduced to the C-terminus of the Fc region of human immunoglobulin heavy gamma1 and the whole protein, designated as Gn-Fc-HA, was produced as described above.
In order to produce histidine tagged SFTSV Gn glycoprotein, a ligand for surface plasmon resonance analysis, a Gn-Cκ with six carboxy-terminal poly-histidine residues was designed and produced as described above.
Human antibody library construction and antibody selection
Peripheral blood mononuclear cells of a patient who recovered from SFTS were collected using a Ficoll-Paque density gradient medium (17144002; GE Healthcare). Total RNA was isolated using TRIzol Reagent (15596018; Invitrogen), and cDNA was synthesized using a SuperScript III first-strand cDNA synthesis kit with oligo dT priming (18080051; Invitrogen). From this cDNA, a phage-display library of human single-chain variable fragments (scFv) was constructed, and four rounds of biopanning were performed to select scFv antibody clones from the library, as previously described[63,64]. For each round of biopanning, recombinant SFTSV Gn-Fc coated onto paramagnetic Dynabeads (14302D, Invitrogen) were used. To select SFTSV glycoprotein binding clones, phage ELISA was performed as previously described, using Gn or Gc glycoprotein-coated microtiter plates, scFv displaying phages, and horseradish peroxidase (HRP) conjugated anti-M13 antibody (11973-MM05, Sino Biological, Beijing, China)[64]. The nucleotide sequences of positive scFv clones were determined by Sanger nucleotide sequencing (Cosmogenetech, Seoul, South Korea). Germline sequences of selected antibody variable regions were analyzed by the National Center for Biotechnology Information (NCBI) IgBLAST.
Production of single-chain variable fragment antibodies and IgG1 antibodies against SFTSV Gn glycoprotein
The genes encoding the variable heavy chain and variable light chain of Ab10 and MAb4-5[31] were synthesized (Integrated DNA Technologies, GenScript) and fused with the human heavy chain constant region gene (IgG1) and human kappa light chain gene, and then cloned into an eukaryotic expression vector, as described previously[65,66]. The expression vectors were transfected into HEK 293F cells. The IgG1 molecule was purified from the culture supernatant by affinity chromatography using MabSelect as described above. Genes encoding the scFv-Fc fusion protein and the scFv-Cκ fusion protein were synthesized and cloned into a pCEP4 vector (Invitrogen). After transfection into HEK 293F cells, the recombinant proteins were overexpressed and purified as described above.
SFTSV preparation and immunofluorescent imaging-based neutralization test
The SFTSV strain of Gangwon/Korea/2012[3] was propagated in Vero cells (10081, Korean Cell Link Bank) with Roswell Park Memorial Institute (RPMI)-1640 medium (LM 011–01; Welgene, Daegu, South Korea) supplemented with 2% heat-inactivated fetal bovine serum (16000044; Gibco) and penicillin-streptomycin (10378016; Gibco). The fifty-percent tissue culture infective dose (TCID50) values were titrated on Vero cells using the Reed-Muench method[67]. Ab10 or MAB4-5 scFv-Fc fusion protein was serially diluted in 10-fold increments from a 50 μg/mL concentration, then mixed with an equal volume of 100 TCID50 SFTSV and incubated at 37°C for 1 h. The virus-antibody mixture was transferred onto Vero cells in 8-well chamber slides (154534; Thermo Scientific, Waltham, MA, USA) and incubated at 37°C for 1 h. For the no-infection-control group, no virus was added to the cells. In contrast, for the infection-control group, no antibody was incubated with the virus. After removing the virus-antibody mixture, cells were cultured for 2 days. For the IFA, cultured cells were fixed with 4% paraformaldehyde in PBS for 1 h at room temperature. Slides were blocked and permeabilized with PBS containing 0.1% Triton X-100 and 1% bovine serum albumin, followed by incubation with 5 μg/mL of anti-SFTSV Gn glycoprotein antibody[68] at 4°C overnight. After washing, cells were incubated for 1 h at room temperature with 1:100 diluted fluorescein isothiocyanate (FITC)-conjugated anti-rabbit IgG Fc antibody (111-095-046; Jackson ImmunoResearch, West Grove, PA, USA). To stain the nucleus, 4’,6-diamidino-2-phenylindole dihydrochloride (DAPI) was used. Fluorescence image of cells was monitored under a confocal laser scanning microscope (TCS SP8; Leica, Wetzlar, Germany).
In vivo efficacy test
For animal experiments, the titer of SFTSV was measured by plaque forming assays[69]. Ten-fold serial dilutions of SFTSV were inoculated onto monolayers of Vero cells in 6-well tissue culture plates for 1 h at room temperature. After removal of the virus, cells were washed three times with PBS and incubated with Dulbecco’s Modified Eagle’s Medium (12100–046; Gibco) based overlay medium containing 0.7% agar (214010; BD Biosciences, San Jose, CA, USA) for 7 days. For visualization of plaques, the overlay medium was removed and the cells were fixed with 4% paraformaldehyde in PBS, followed by staining with 0.05% (w/v) crystal violet solution (C0775; Sigma-Aldrich, St. Louis, MO USA). Either 2 or 20 plaque forming units (PFU) of Gangwon/Korea/2012 strain SFTSV in 200 μL of PBS were inoculated in 8- to 10-week-old male or female A129 mice by a subcutaneous (s.c.) injection route. After 1 h of infection, mice were administered with Ab10 IgG1 antibody or a PBS vehicle control through an intraperitoneal (i.p.) injection route, at 30 mg/kg of body weight for every 24 h for a consecutive 4 days. Palivizumab (MedImmune, Gaithersburg, MD, USA) or Mab4-5 IgG1 was used as an isotype control or a positive control antibody, respectively. In the delayed treatment model, the infected mice were treated with antibodies at 1, 3, 4, or 5 days post-infection (d.p.i.) for 4 days consecutively. Body weight and survival of mice were monitored until 10 days post-infection.
Enzyme-linked immunosorbent assays
In order to measure the binding activities of the Ab10 and MAb4-5 IgG1 antibodies, 96-well half-area microplates (3690; Corning, Corning, NY, USA) were coated with Gn-Fc fusion protein and incubated at 4°C overnight. Plates were blocked with 3% skim milk in PBS for 1 h at room temperature. The plates were then washed with PBS and received antibodies that were 10-fold serially diluted from 1 μM to 10 μM in blocking buffer. The plates were then incubated for 2 h at room temperature and washed three times with 0.05% Tween20 in PBS solution. Then, 50 μL of HRP-conjugated anti-human Ig kappa light chain antibody (AP502P; Chemicon, Temecula, CA, USA) diluted in blocking buffer (1:5000) was added into each well. Then, plates were incubated for 1 h at room temperature. After washing, each well received 50 μL of 3,3′,5,5′-tetramethylbenzidine (TMB) substrate solution (34028; Thermo Scientific). The color reaction was stopped by adding 50 μL of 2 M sulfuric acid. The absorbance of each well was measured at 450 nm using a microplate spectrophotometer (Multiskan GO; Thermo Scientific).
Surface plasmon resonance analysis of Ab10
The kinetics of Ab10 and Gn glycoprotein binding were measured by surface plasmon resonance analysis, using a Biacore T200 instrument with sensor chip CM5, amine coupling kit, and his capture kit (28975001, 29149603, BR100050, 28995056; GE Healthcare). We followed the recommended manufacturer’s protocol for the procedures and conditions of reaction buffers, flow times, flow rates, and concentration of analytes. Briefly, anti-histidine antibody was immobilized on an activated CM5 chip, followed by a deactivation step. Then, histidine tagged Gn-Cκ was injected over the flow cells prior to antibody injection. For the association step, all of the Ab10 IgG1 antibody in PBS at concentrations of two-fold increments ranging from 1.25 nM to 80 nM was injected for 3 min. For the dissociation step, PBS containing 0.005% of Tween20 was injected for 5 min. After each dissociation step, chip regeneration was performed.
Conformational epitope mapping by crosslinking coupled mass spectrometry
The epitope of Ab10 antibody was first determined by analyzing the complex of Ab10 antibody and SFTSV Gn-Cκ antigen linked with deuterated cross-linkers (CovalX, Zürich, Switzerland), as previously described[32]. Briefly, antibody, antigen, and antibody/antigen complexes were characterized by high mass matrix-assisted laser desorption/ionization (MALDI) mass spectrometry using a MALDI TOF/TOF tandem mass spectrometer (Autoflex III; Bruker, Billerica, MA, USA) equipped with an interaction module (HM4; CovalX, Zürich, Switzerland). Afterwards, the antibody/antigen complex was crosslinked with DSS d0/d12 isotope-labeled homobifunctional N-hydroxysuccinimide esters, followed by reduction alkylation using dithiothreitol, iodoacetamide, and urea. To digest the reduced complex, a proteolytic buffer composed of trypsin, chymotrypsin, endoproteinase Asp-N, elastase, and thermolysin was used. The sample was then analyzed by nano-liquid chromatography (Ultimate 3000; Dionex, Sunnyvale, CA, USA) and Orbitrap mass spectrometry (Q Exactive Hybrid Quadrupole-Orbitrap; Thermo Scientific).
ELISA for epitope mapping
To measure the binding activities of Ab10 to mutated Gn, Ab10 scFv-Cκ antibody and an anti-influenza virus hemagglutinin antibody (clone 12CA5; Bio X Cell, Lebanon, NH, USA) were coated on a microplate, in parallel. Then, plates were blocked with 3% skim milk in PBS for 1 h at room temperature. Transiently transfected cell supernatant containing recombinant Gn-Fc-HA proteins with alanine substitution was added to each well. After incubation for 2 h at room temperature, the microplate was washed three times with 0.05% Tween20 in PBS solution. Then, HRP-conjugated anti-human IgG Fc antibody (31423; Invitrogen) diluted in blocking buffer was added to each well. The plate was incubated for 1 h at room temperature. After washing, each well received 50 μL of 3,3′,5,5′-tetramethylbenzidine (TMB) substrate solution (34028; Thermo Scientific). The color reaction was stopped by adding 50 μL of 2 M sulfuric acid. The absorbance of each well was measured at 450 nm using a microplate spectrophotometer (Multiskan GO; Thermo Scientific). Relative reactivity was calculated using absorbance values (Abs) as follows: % relative reactivity = [100 × {(Abs of mutant captured by Ab10) / (Abs of mutant captured by HA antibody)} / {(Abs of wildtype captured by Ab10) / (Abs of wildtype captured by HA antibody)}].
Data analysis
ELISA and IFA data including statistical comparisons were analyzed and graphed using GraphPad Prism software (San Diego, CA, USA). Fluorescent signals measured by confocal microscopy were quantified using Leica Application Suite Advanced Fluorescence software. Mass spectrometry data were analyzed using XQuest and Stavrox software. Plasmon surface resonance data were analyzed using BIAevaluation software. Visualization, alignment, and phylogenic analyses of amino acid sequences were performed with Geneious software.
Supporting information
The cytopathic effects (CPE) of SFTSV on Vero cells were monitored to evaluate the protective effect of antibody clones. Candidate antibodies (scFv-Fc format) were mixed with 100 TCID50 of SFTSV (strain: Gangwon/Korea/2012) at a final concentration of 50 μg/mL and the mixtures were incubated for 1 h. SFTSV-antibody mixtures were then transferred to Vero cells at 80% confluency grown in 96-well tissue culture plates, and were incubated for 1 h. Then, cells were washed with PBS and incubated with fresh growth medium for 96 h. Cells were observed under a microscope to evaluate CPE and brightfield images are shown (scale bar: 100 μm). In the control groups, cells not incubated with virus (Uninfected), cells infected without antibody treatment (Infected), cells incubated with virus, and the isotype control antibody (Isotype control antibody) were employed.
(TIF)
Thirty to fifty focus forming units (FFU) of SFTSV were incubated with serially diluted scFv-Fc fusion proteins for 1 h at room temperature and transferred to Vero cells in a 24-well tissue culture plate. After incubation for 1 h at 37°C in a 5% CO2 incubator, the cells were overlaid with 0.5% methylcellulose in RPMI medium with 2% fetal bovine serum and cultured for 2 days. Cells were fixed with ice-cold methanol for 15 min and incubated with 1% bovine serum albumin in PBS for 1 h. Then, SFTSV localized clusters (foci) were visualized by incubating with 1 μg/mL of anti-SFTSV Gc glycoprotein antibody (Clone Ab3 from patent PCT/KR2017/003156) for 1 h, followed by incubation with 1:2,000 diluted goat anti-rabbit IgG Fc fragment specific antibody, conjugated with HRP (111-035-008; Jackson ImmunoResearch, West Grove, PA, USA) for 30 min and DAB substrate (K5007-BC; Dako). The percentage of neutralization was calculated for each diluted solution of antibody as the percentage of decreased fraction in the number of foci compared to that of the virus without incubation of scFv-Fc fusion protein. An irrelevant scFv-Fc fusion protein was used as an isotype control. Dose-response curves were drawn by non-linear regression analyses (variable slope model) and 50% FRNT values were determined from graphs using GraphPad Prism6 software.
(TIF)
The amino acid sequence of the light chain variable region (A) and heavy chain variable region (B) are shown. Blue letters indicate complementary determining regions (CDR) of each variable region defined by the International Immunogenetics Information System (IMGT).
(TIF)
The 8-week-old A129 mice (n = 4 per group) were inoculated with 2×105 or 2×101 PFU of SFTSV (strain: Gangwon/Korea/2012) or PBS vehicle control using a subcutaneous route. The percentage survival was monitored daily until 8 days post-infection. Survival was determined by the Kaplan-Meier method.
(TIF)
To examine binding activity of Ab10 antibody to SFTSV generated from Vero cells, serially diluted viral supernatants of SFTSV infected cells with a determined titer or the supernatant of mock-infected cells was coated onto microtiter plates (2692; Costar) at 4°C overnight. Fifty to five thousand PFU of SFTSV were used to coat each well. The plates were then incubated with serial dilutions of Ab10 antibody or Palivizumab as an isotype control, followed by HRP-conjugated anti-human IgG Fc antibody (31423; Invitrogen). Reactions were developed by adding TMB substrate (34028; Thermo Scientific) and were terminated by adding 2 M sulfuric acid. The absorbance was measured at 450 nm. The amount of virus coated on each microplate well is indicated on the top of each graph, and the mean absorbance with standard deviation (s.d.) error bars is shown for each antibody concentration. Absorbance of Ab10 antibody bound to SFTSV-coated wells (red), Palivizumab bound to SFTSV-coated wells (blue), Ab10 antibody bound to mock-virus coated wells (magenta), and Palivizumab bound to mock-virus coated wells (purple) are shown in the graph.
(TIF)
The amino acid sequence of Gn glycoprotein from 272 SFTSV isolates deposited in ViPR were used for analysis. The sequences were trimmed to retain the amino acid residues from 20–452 that corresponded to the ectodomain. Trimmed sequences were analyzed, and a phylogenetic tree was built in a circular tree layout using the neighbor-joining method with a Jukes-Cantor genetic distance model. The names of isolates are labeled beside the tip of each branch. Asterisks at the tip of branches indicate the isolates that were tested for binding activity of Ab10.
(TIF)
Recombinant SFTSV Gn-Cκ was prepared with sample buffer and reducing agent (NP0008 and NP0004; Invitrogen). The samples were then separated on a polyacrylamide gel (NP0321BOX; Invitrogen) by electrophoresis and transferred to a nitrocellulose membrane. After blocking with 5% (w/v) skim milk in Tris-buffered saline (pH 7.4) the membrane was incubated with 100 ng/mL of five (Ab6 to Ab10) SFTSV Gn specific antibodies in a scFv-Fc format. Gn bound antibodies were probed with HRP-conjugated anti-human IgG Fc antibody (31423; Invitrogen). To confirm the presence of Gn-Cκ protein, HRP-conjugated anti-human Ig kappa light chain antibody (AP502P, Chemicon, Temecula, CA, USA) was used to directly detect Gn-Cκ. The blots were visualized using a chemiluminescent substrate (34578; Thermo Scientific).
(TIF)
The amino acid sequence of Gn glycoprotein from the 272 SFTSV isolates deposited in ViPR were analyzed. The sequences were trimmed to retain the amino acids from 313–389 that correspond to the residues recognized by Ab10. Trimmed sequences were analyzed, and a phylogenetic tree was built in a circular tree layout using the neighbor-joining method with a Jukes-Cantor genetic distance model. The names of isolates are written beside the tip of each branch. Strain names labeled in red indicate that the Gn glycoprotein of the indicated strain is predicted to not interact with Ab10.
(TIF)
Acknowledgments
We thank Myung Jin Lee and Su Jin Choi for setting up the initial experimental conditions for the virus neutralization assay.
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
This research was supported by the Commercialization Promotion Agency for Research and Development outcomes (COMPA), the National Research Foundation of Korea (NRF), funded by the Ministry of Science, ICT (MSIT), Republic of Korea (grant number: 2017K000459, 2017M3A9G6068245). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Yu X-J, Liang M-F, Zhang S-Y, Liu Y, Li J-D, Sun Y-L, et al. Fever with Thrombocytopenia Associated with a Novel Bunyavirus in China. N Engl J Med. 2011;364: 1523–1532. 10.1056/NEJMoa1010095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sun J, Lu L, Wu H, Yang J, Ren J, Liu Q. The changing epidemiological characteristics of severe fever with thrombocytopenia syndrome in China, 2011–2016. Sci Rep. 2017;7: 9236 10.1038/s41598-017-08042-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim K-H, Yi J, Kim G, Choi SJ, Jun KI, Kim N-H, et al. Severe fever with thrombocytopenia syndrome, South Korea, 2012. Emerging Infect Dis. 2013;19: 1892–1894. 10.3201/eid1911.130792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Takahashi T, Maeda K, Suzuki T, Ishido A, Shigeoka T, Tominaga T, et al. The first identification and retrospective study of Severe Fever with Thrombocytopenia Syndrome in Japan. J Infect Dis. Oxford University Press; 2014;209: 816–827. 10.1093/infdis/jit603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Korea Centers for Disease Control and Prevention. Disease information (Severe Fever with Thrombocytopenia Syndrome, SFTS). In: cdc.go.kr [Internet]. 9 Feb 2018 [cited 22 Jun 2018]. http://www.cdc.go.kr/CDC/health/CdcKrHealth0101.jsp?menuIds=HOME001-MNU1132-MNU1147-MNU0746-MNU2423&fid=7956&cid=70361
- 6.National Institute of Infectious Diseases, Japan. Severe Fever with Thrombocytopenia Syndrome (SFTS). In: niid.go.jp [Internet]. 25 Jul 2018 [cited 15 Aug 2018]. https://www.niid.go.jp/niid/ja/diseases/sa/sfts.html
- 7.Zhang Y-Z, Zhou D-J, Qin X-C, Tian J-H, Xiong Y, Wang J-B, et al. The ecology, genetic diversity, and phylogeny of Huaiyangshan virus in China. Journal of Virology. American Society for Microbiology; 2012;86: 2864–2868. 10.1128/JVI.06192-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Niu G, Li J, Liang M, Jiang X, Jiang M, Yin H, et al. Severe fever with thrombocytopenia syndrome virus among domesticated animals, China. Emerging Infect Dis. 2013;19: 756–763. 10.3201/eid1905.120245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang Y-Z, Xu J. The emergence and cross species transmission of newly discovered tick-borne Bunyavirus in China. Current Opinion in Virology. 2016;16: 126–131. 10.1016/j.coviro.2016.02.006 [DOI] [PubMed] [Google Scholar]
- 10.Liu Y, Li Q, Hu W, Wu J, Wang Y, Mei L, et al. Person-to-person transmission of severe fever with thrombocytopenia syndrome virus. Vector Borne Zoonotic Dis. 2012;12: 156–160. 10.1089/vbz.2011.0758 [DOI] [PubMed] [Google Scholar]
- 11.Gai Z, Liang M, Zhang Y, Zhang S, Jin C, Wang S-W, et al. Person-to-Person Transmission of Severe Fever With Thrombocytopenia Syndrome Bunyavirus Through Blood Contact. Clin Infect Dis. Oxford University Press; 2012;54: 249–252. 10.1093/cid/cir776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rainey T, Occi JL, Robbins RG, Egizi A. Discovery of Haemaphysalis longicornis (Ixodida: Ixodidae) Parasitizing a Sheep in New Jersey, United States. J Med Entomol. Oxford University Press; 2018;55: 757–759. 10.1093/jme/tjy006 [DOI] [PubMed] [Google Scholar]
- 13.Liu S, Chai C, Wang C, Amer S, Lv H, He H, et al. Systematic review of severe fever with thrombocytopenia syndrome: virology, epidemiology, and clinical characteristics. Rev Med Virol. Wiley-Blackwell; 2014;24: 90–102. 10.1002/rmv.1776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu L, Chen W, Yang Y, Jiang Y. Molecular evolution of fever, thrombocytopenia and leukocytopenia virus (FTLSV) based on whole-genome sequences. Infection, Genetics and Evolution. 2016;39: 55–63. 10.1016/j.meegid.2015.12.022 [DOI] [PubMed] [Google Scholar]
- 15.Zhan J, Wang Q, Cheng J, Hu B, Li J, Zhan F, et al. Current status of severe fever with thrombocytopenia syndrome in China. Virologica Sinica. Springer Singapore; 2017;32: 51–62. 10.1007/s12250-016-3931-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu Q, He B, Huang S-Y, Wei F, Zhu X-Q. Severe fever with thrombocytopenia syndrome, an emerging tick-borne zoonosis. Lancet Infect Dis. 2014;14: 763–772. 10.1016/S1473-3099(14)70718-2 [DOI] [PubMed] [Google Scholar]
- 17.Kato H, Yamagishi T, Shimada T, Matsui T, Shimojima M, Saijo M, et al. Epidemiological and Clinical Features of Severe Fever with Thrombocytopenia Syndrome in Japan, 2013–2014. Xing Z, editor. PLoS ONE. Public Library of Science; 2016;11: e0165207 10.1371/journal.pone.0165207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gai Z-T, Zhang Y, Liang M-F, Jin C, Zhang S, Zhu C-B, et al. Clinical Progress and Risk Factors for Death in Severe Fever with Thrombocytopenia Syndrome Patients. J Infect Dis. Oxford University Press; 2012;206: 1095–1102. 10.1093/infdis/jis472 [DOI] [PubMed] [Google Scholar]
- 19.Ding Y-P, Liang MF, Ye J-B, Liu Q-H, Xiong C-H, Long B, et al. Prognostic value of clinical and immunological markers in acute phase of SFTS virus infection. Clin Microbiol Infect. 2014;20: O870–8. 10.1111/1469-0691.12636 [DOI] [PubMed] [Google Scholar]
- 20.Shin J, Kwon D, Youn S-K, Park J-H. Characteristics and Factors Associated with Death among Patients Hospitalized for Severe Fever with Thrombocytopenia Syndrome, South Korea, 2013. Emerging Infect Dis. 2015;21: 1704–1710. 10.3201/eid2110.141928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li H, Lu Q-B, Xing B, Zhang S-F, Liu K, Du J, et al. Epidemiological and clinical features of laboratory-diagnosed severe fever with thrombocytopenia syndrome in China, 2011–17: a prospective observational study. Lancet Infect Dis. Elsevier; 2018. 10.1016/S1473-3099(18)30293-7 [DOI] [PubMed] [Google Scholar]
- 22.Cyranoski D. East Asia braces for surge in deadly tick-borne virus. Nature. 2018;556: 282–283. 10.1038/d41586-018-04486-6 [DOI] [PubMed] [Google Scholar]
- 23.Hofmann H, Li X, Zhang X, Liu W, Kühl A, Kaup F, et al. Severe fever with thrombocytopenia virus glycoproteins are targeted by neutralizing antibodies and can use DC-SIGN as a receptor for pH-dependent entry into human and animal cell lines. Journal of Virology. American Society for Microbiology; 2013;87: 4384–4394. 10.1128/JVI.02628-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sun Y, Qi Y, Liu C, Gao W, Chen P, Fu L, et al. Nonmuscle myosin heavy chain IIA is a critical factor contributing to the efficiency of early infection of severe fever with thrombocytopenia syndrome virus. Journal of Virology. American Society for Microbiology; 2014;88: 237–248. 10.1128/JVI.02141-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Plegge T, Hofmann-Winkler H, Spiegel M, Pöhlmann S. Evidence that Processing of the Severe Fever with Thrombocytopenia Syndrome Virus Gn/Gc Polyprotein Is Critical for Viral Infectivity and Requires an Internal Gc Signal Peptide. Xing Z, editor. PLoS ONE. Public Library of Science; 2016;11: e0166013 10.1371/journal.pone.0166013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dessau M, Modis Y. Crystal structure of glycoprotein C from Rift Valley fever virus. Proc Natl Acad Sci USA. National Acad Sciences; 2013;110: 1696–1701. 10.1073/pnas.1217780110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wu Y, Zhu Y, Gao F, Jiao Y, Oladejo BO, Chai Y, et al. Structures of phlebovirus glycoprotein Gn and identification of a neutralizing antibody epitope. Proc Natl Acad Sci USA. National Acad Sciences; 2017;114: E7564–E7573. 10.1073/pnas.1705176114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yu L, Zhang L, Sun L, Lu J, Wu W, Li C, et al. Critical Epitopes in the Nucleocapsid Protein of SFTS Virus Recognized by a Panel of SFTS Patients Derived Human Monoclonal Antibodies. Dübel S, editor. PLoS ONE. Public Library of Science; 2012;7: e38291 10.1371/journal.pone.0038291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jin J, Park C, Cho S-H, Chung J. The level of decoy epitope in PCV2 vaccine affects the neutralizing activity of sera in the immunized animals. Biochemical and Biophysical Research Communications. 2018;496: 846–851. 10.1016/j.bbrc.2018.01.141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shimada S, Posadas-Herrera G, Aoki K, Morita K, Hayasaka D. Therapeutic effect of post-exposure treatment with antiserum on severe fever with thrombocytopenia syndrome (SFTS) in a mouse model of SFTS virus infection. Virology. 2015;482: 19–27. 10.1016/j.virol.2015.03.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Guo X, Zhang L, Zhang W, Chi Y, Zeng X, Li X, et al. Human antibody neutralizes severe Fever with thrombocytopenia syndrome virus, an emerging hemorrhagic Fever virus. Clin Vaccine Immunol. American Society for Microbiology; 2013;20: 1426–1432. 10.1128/CVI.00222-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pimenova T, Nazabal A, Roschitzki B, Seebacher J, Rinner O, Zenobi R. Epitope mapping on bovine prion protein using chemical crosslinking and mass spectrometry. Journal of Mass Spectrometry. Wiley-Blackwell; 2008;43: 185–195. 10.1002/jms.1280 [DOI] [PubMed] [Google Scholar]
- 33.Corti D, Misasi J, Mulangu S, Stanley DA, Kanekiyo M, Wollen S, et al. Protective monotherapy against lethal Ebola virus infection by a potently neutralizing antibody. Science. American Association for the Advancement of Science; 2016;351: 1339–1342. 10.1126/science.aad5224 [DOI] [PubMed] [Google Scholar]
- 34.Liu Q, Fan C, Li Q, Zhou S, Huang W, Wang L, et al. Antibody-dependent-cellular-cytotoxicity-inducing antibodies significantly affect the post-exposure treatment of Ebola virus infection. Sci Rep. Nature Publishing Group; 2017;7: 45552 10.1038/srep45552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gunn BM, Yu W-H, Karim MM, Brannan JM, Herbert AS, Wec AZ, et al. A Role for Fc Function in Therapeutic Monoclonal Antibody-Mediated Protection against Ebola Virus. Cell Host & Microbe. Elsevier; 2018;24: 221–233.e5. 10.1016/j.chom.2018.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Walker LM, Burton DR. Passive immunotherapy of viral infections: “super-antibodies” enter the fray. Nat Rev Immunol. Nature Publishing Group; 2018;18: 297–308. 10.1038/nri.2017.148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bar KJ, Sneller MC, Harrison LJ, Justement JS, Overton ET, Petrone ME, et al. Effect of HIV Antibody VRC01 on Viral Rebound after Treatment Interruption. N Engl J Med. 2016;375: 2037–2050. 10.1056/NEJMoa1608243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Scheid JF, Horwitz JA, Bar-On Y, Kreider EF, Lu C-L, Lorenzi JCC, et al. HIV-1 antibody 3BNC117 suppresses viral rebound in humans during treatment interruption. Nature. 2016;535: 556–560. 10.1038/nature18929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Caskey M, Schoofs T, Gruell H, Settler A, Karagounis T, Kreider EF, et al. Antibody 10–1074 suppresses viremia in HIV-1-infected individuals. Nat Med. Nature Publishing Group; 2017;23: 185–191. 10.1038/nm.4268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhu Q, McLellan JS, Kallewaard NL, Ulbrandt ND, Palaszynski S, Zhang J, et al. A highly potent extended half-life antibody as a potential RSV vaccine surrogate for all infants. Sci Transl Med. American Association for the Advancement of Science; 2017;9: eaaj1928. 10.1126/scitranslmed.aaj1928 [DOI] [PubMed] [Google Scholar]
- 41.PREVAIL II Writing Group, Multi-National PREVAIL II Study Team, Davey RT, Dodd L, Proschan MA, Neaton J, et al. A Randomized, Controlled Trial of ZMapp for Ebola Virus Infection. N Engl J Med. Massachusetts Medical Society; 2016;375: 1448–1456. 10.1056/NEJMoa1604330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yu F, Song H, Wu Y, Chang SY, Wang L, Li W, et al. A Potent Germline-like Human Monoclonal Antibody Targets a pH-Sensitive Epitope on H7N9 Influenza Hemagglutinin. Cell Host & Microbe. Cell Press; 2017;22: 471–483.e5. 10.1016/j.chom.2017.08.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Paules CI, Lakdawala S, McAuliffe JM, Paskel M, Vogel L, Kallewaard NL, et al. The Hemagglutinin A Stem Antibody MEDI8852 Prevents and Controls Disease and Limits Transmission of Pandemic Influenza Viruses. J Infect Dis. 8 ed. 2017;216: 356–365. 10.1093/infdis/jix292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ying T, Du L, Ju TW, Prabakaran P, Lau CCY, Lu L, et al. Exceptionally potent neutralization of Middle East respiratory syndrome coronavirus by human monoclonal antibodies. Doms RW, editor. Journal of Virology. American Society for Microbiology; 2014;88: 7796–7805. 10.1128/JVI.00912-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Corti D, Zhao J, Pedotti M, Simonelli L, Agnihothram S, Fett C, et al. Prophylactic and postexposure efficacy of a potent human monoclonal antibody against MERS coronavirus. PNAS. National Academy of Sciences; 2015;112: 10473–10478. 10.1073/pnas.1510199112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pascal KE, Coleman CM, Mujica AO, Kamat V, Badithe A, Fairhurst J, et al. Pre- and postexposure efficacy of fully human antibodies against Spike protein in a novel humanized mouse model of MERS-CoV infection. PNAS. National Academy of Sciences; 2015;112: 8738–8743. 10.1073/pnas.1510830112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sapparapu G, Fernandez E, Kose N, Bin Cao, Fox JM, Bombardi RG, et al. Neutralizing human antibodies prevent Zika virus replication and fetal disease in mice. Nature. 2016;540: 443–447. 10.1038/nature20564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wang Q, Yang H, Liu X, Dai L, Ma T, Qi J, et al. Molecular determinants of human neutralizing antibodies isolated from a patient infected with Zika virus. Sci Transl Med. American Association for the Advancement of Science; 2016;8: 369ra179–369ra179. 10.1126/scitranslmed.aai8336 [DOI] [PubMed] [Google Scholar]
- 49.Robbiani DF, Bozzacco L, Keeffe JR, Khouri R, Olsen PC, Gazumyan A, et al. Recurrent Potent Human Neutralizing Antibodies to Zika Virus in Brazil and Mexico. Cell. 2017;169: 597–609.e11. 10.1016/j.cell.2017.04.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Marston HD, Paules CI, Fauci AS. Monoclonal Antibodies for Emerging Infectious Diseases—Borrowing from History. N Engl J Med. 2018;378: 1469–1472. 10.1056/NEJMp1802256 [DOI] [PubMed] [Google Scholar]
- 51.Tani H, Fukuma A, Fukushi S, Taniguchi S, Yoshikawa T, Iwata-Yoshikawa N, et al. Efficacy of T-705 (Favipiravir) in the Treatment of Infections with Lethal Severe Fever with Thrombocytopenia Syndrome Virus. Duprex WP, editor. mSphere. 2016;1: e00061–15. 10.1128/mSphere.00061-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gowen BB, Westover JB, Miao J, Van Wettere AJ, Rigas JD, Hickerson BT, et al. Modeling Severe Fever with Thrombocytopenia Syndrome Virus Infection in Golden Syrian Hamsters: Importance of STAT2 in Preventing Disease and Effective Treatment with Favipiravir. Ross SR, editor. Journal of Virology. American Society for Microbiology; 2017;91: e01942–16. 10.1128/JVI.01942-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ikegami T, Balogh A, Nishiyama S, Lokugamage N, Saito TB, Morrill JC, et al. Distinct virulence of Rift Valley fever phlebovirus strains from different genetic lineages in a mouse model. McElroy AK, editor. PLoS ONE. Public Library of Science; 2017;12: e0189250 10.1371/journal.pone.0189250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Weis W, Brown JH, Cusack S, Paulson JC, Skehel JJ, Wiley DC. Structure of the influenza virus haemagglutinin complexed with its receptor, sialic acid. Nature. 1988;333: 426–431. 10.1038/333426a0 [DOI] [PubMed] [Google Scholar]
- 55.Tharakaraman K, Subramanian V, Cain D, Sasisekharan V, Sasisekharan R. Broadly Neutralizing Influenza Hemagglutinin Stem-Specific Antibody CR8020 Targets Residues that Are Prone to Escape due to Host Selection Pressure. Cell Host & Microbe. Elsevier; 2014;15: 644–651. 10.1016/j.chom.2014.04.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wu Y, Cho M, Shore D, Song M, Choi J, Jiang T, et al. A potent broad-spectrum protective human monoclonal antibody crosslinking two haemagglutinin monomers of influenza A virus. Nat Comms. Nature Publishing Group; 2015;6: 7708 10.1038/ncomms8708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chai N, Swem LR, Park S, Nakamura G, Chiang N, Estevez A, et al. A broadly protective therapeutic antibody against influenza B virus with two mechanisms of action. Nat Comms. Nature Publishing Group; 2017;8: 14234 10.1038/ncomms14234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.VanBlargan LA, Goo L, Pierson TC. Deconstructing the Antiviral Neutralizing-Antibody Response: Implications for Vaccine Development and Immunity. Microbiology and Molecular Biology Reviews. American Society for Microbiology; 2016;80: 989–1010. 10.1128/MMBR.00024-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yoon A, Yi KS, Chang SY, Kim SH, Song M, Choi JA, et al. An Anti-Influenza Virus Antibody Inhibits Viral Infection by Reducing Nucleus Entry of Influenza Nucleoprotein. PLoS ONE. 2015;10: e0141312 10.1371/journal.pone.0141312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Halldorsson S, Li S, Li M, Harlos K, Bowden TA, Huiskonen JT. Shielding and activation of a viral membrane fusion protein. Nat Comms. Nature Publishing Group; 2018;9: 349 10.1038/s41467-017-02789-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Park S, Lee D-H, Park J-G, Lee YT, Chung J. A sensitive enzyme immunoassay for measuring cotinine in passive smokers. Clin Chim Acta. 2010;411: 1238–1242. 10.1016/j.cca.2010.04.027 [DOI] [PubMed] [Google Scholar]
- 62.Lee Y, Kim H, Chung J. An antibody reactive to the Gly63|[ndash]|Lys68 epitope of NT-proBNP exhibits O-glycosylation-independent binding. Experimental & Molecular Medicine. Nature Publishing Group; 2014;46: e114 10.1038/emm.2014.57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Andris-Widhopf J, Steinberger P, Fuller R, RADER C, BARBAS CF III. Generation of Human scFv Antibody Libraries: PCR Amplification and Assembly of Light- and Heavy-Chain Coding Sequences. Cold Spring Harbor Protocols. Cold Spring Harbor Laboratory Press; 2011;2011: pdb.prot065573–pdb.prot065573. 10.1101/pdb.prot065573 [DOI] [PubMed] [Google Scholar]
- 64.BARBAS CF III, Burton DR, Scott JK, Silverman GJ. Phage Display: A Laboratory Manual. Cold Spring Harbor Laboratory Press; 2001. 10.1086/420571 [DOI] [Google Scholar]
- 65.Lee S, Yoon I-H, Yoon A, Cook-Mills JM, Park C-G, Chung J. An antibody to the sixth Ig-like domain of VCAM-1 inhibits leukocyte transendothelial migration without affecting adhesion. J Immunol. American Association of Immunologists; 2012;189: 4592–4601. 10.4049/jimmunol.1103803 [DOI] [PubMed] [Google Scholar]
- 66.Kim H-Y, Tsai S, Lo S-C, Wear DJ, Izadjoo MJ. Production and Characterization of Chimeric Monoclonal Antibodies against Burkholderia pseudomallei and B. mallei Using the DHFR Expression System. Chakravortty D, editor. PLoS ONE. Public Library of Science; 2011;6: e19867 10.1371/journal.pone.0019867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.REED LJ, MUENCH H. A SIMPLE METHOD OF ESTIMATING FIFTY PER CENT ENDPOINTS. Am J Epidemiol. Oxford University Press; 1938;27: 493–497. 10.1093/oxfordjournals.aje.a118408 [DOI] [Google Scholar]
- 68.Kang CK, Choi SJ, Koh J, Jeon YK, Kim KH, Chung J, et al. 18F-FDG PET and histopathologic findings in a patient with severe fever with thrombocytopenia syndrome. Ticks and Tick-borne Diseases. 2018;9: 972–975. 10.1016/j.ttbdis.2018.03.030 [DOI] [PubMed] [Google Scholar]
- 69.DULBECCO R, VOGT M. Some problems of animal virology as studied by the plaque technique. Cold Spring Harb Symp Quant Biol. 1953;18: 273–279. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The cytopathic effects (CPE) of SFTSV on Vero cells were monitored to evaluate the protective effect of antibody clones. Candidate antibodies (scFv-Fc format) were mixed with 100 TCID50 of SFTSV (strain: Gangwon/Korea/2012) at a final concentration of 50 μg/mL and the mixtures were incubated for 1 h. SFTSV-antibody mixtures were then transferred to Vero cells at 80% confluency grown in 96-well tissue culture plates, and were incubated for 1 h. Then, cells were washed with PBS and incubated with fresh growth medium for 96 h. Cells were observed under a microscope to evaluate CPE and brightfield images are shown (scale bar: 100 μm). In the control groups, cells not incubated with virus (Uninfected), cells infected without antibody treatment (Infected), cells incubated with virus, and the isotype control antibody (Isotype control antibody) were employed.
(TIF)
Thirty to fifty focus forming units (FFU) of SFTSV were incubated with serially diluted scFv-Fc fusion proteins for 1 h at room temperature and transferred to Vero cells in a 24-well tissue culture plate. After incubation for 1 h at 37°C in a 5% CO2 incubator, the cells were overlaid with 0.5% methylcellulose in RPMI medium with 2% fetal bovine serum and cultured for 2 days. Cells were fixed with ice-cold methanol for 15 min and incubated with 1% bovine serum albumin in PBS for 1 h. Then, SFTSV localized clusters (foci) were visualized by incubating with 1 μg/mL of anti-SFTSV Gc glycoprotein antibody (Clone Ab3 from patent PCT/KR2017/003156) for 1 h, followed by incubation with 1:2,000 diluted goat anti-rabbit IgG Fc fragment specific antibody, conjugated with HRP (111-035-008; Jackson ImmunoResearch, West Grove, PA, USA) for 30 min and DAB substrate (K5007-BC; Dako). The percentage of neutralization was calculated for each diluted solution of antibody as the percentage of decreased fraction in the number of foci compared to that of the virus without incubation of scFv-Fc fusion protein. An irrelevant scFv-Fc fusion protein was used as an isotype control. Dose-response curves were drawn by non-linear regression analyses (variable slope model) and 50% FRNT values were determined from graphs using GraphPad Prism6 software.
(TIF)
The amino acid sequence of the light chain variable region (A) and heavy chain variable region (B) are shown. Blue letters indicate complementary determining regions (CDR) of each variable region defined by the International Immunogenetics Information System (IMGT).
(TIF)
The 8-week-old A129 mice (n = 4 per group) were inoculated with 2×105 or 2×101 PFU of SFTSV (strain: Gangwon/Korea/2012) or PBS vehicle control using a subcutaneous route. The percentage survival was monitored daily until 8 days post-infection. Survival was determined by the Kaplan-Meier method.
(TIF)
To examine binding activity of Ab10 antibody to SFTSV generated from Vero cells, serially diluted viral supernatants of SFTSV infected cells with a determined titer or the supernatant of mock-infected cells was coated onto microtiter plates (2692; Costar) at 4°C overnight. Fifty to five thousand PFU of SFTSV were used to coat each well. The plates were then incubated with serial dilutions of Ab10 antibody or Palivizumab as an isotype control, followed by HRP-conjugated anti-human IgG Fc antibody (31423; Invitrogen). Reactions were developed by adding TMB substrate (34028; Thermo Scientific) and were terminated by adding 2 M sulfuric acid. The absorbance was measured at 450 nm. The amount of virus coated on each microplate well is indicated on the top of each graph, and the mean absorbance with standard deviation (s.d.) error bars is shown for each antibody concentration. Absorbance of Ab10 antibody bound to SFTSV-coated wells (red), Palivizumab bound to SFTSV-coated wells (blue), Ab10 antibody bound to mock-virus coated wells (magenta), and Palivizumab bound to mock-virus coated wells (purple) are shown in the graph.
(TIF)
The amino acid sequence of Gn glycoprotein from 272 SFTSV isolates deposited in ViPR were used for analysis. The sequences were trimmed to retain the amino acid residues from 20–452 that corresponded to the ectodomain. Trimmed sequences were analyzed, and a phylogenetic tree was built in a circular tree layout using the neighbor-joining method with a Jukes-Cantor genetic distance model. The names of isolates are labeled beside the tip of each branch. Asterisks at the tip of branches indicate the isolates that were tested for binding activity of Ab10.
(TIF)
Recombinant SFTSV Gn-Cκ was prepared with sample buffer and reducing agent (NP0008 and NP0004; Invitrogen). The samples were then separated on a polyacrylamide gel (NP0321BOX; Invitrogen) by electrophoresis and transferred to a nitrocellulose membrane. After blocking with 5% (w/v) skim milk in Tris-buffered saline (pH 7.4) the membrane was incubated with 100 ng/mL of five (Ab6 to Ab10) SFTSV Gn specific antibodies in a scFv-Fc format. Gn bound antibodies were probed with HRP-conjugated anti-human IgG Fc antibody (31423; Invitrogen). To confirm the presence of Gn-Cκ protein, HRP-conjugated anti-human Ig kappa light chain antibody (AP502P, Chemicon, Temecula, CA, USA) was used to directly detect Gn-Cκ. The blots were visualized using a chemiluminescent substrate (34578; Thermo Scientific).
(TIF)
The amino acid sequence of Gn glycoprotein from the 272 SFTSV isolates deposited in ViPR were analyzed. The sequences were trimmed to retain the amino acids from 313–389 that correspond to the residues recognized by Ab10. Trimmed sequences were analyzed, and a phylogenetic tree was built in a circular tree layout using the neighbor-joining method with a Jukes-Cantor genetic distance model. The names of isolates are written beside the tip of each branch. Strain names labeled in red indicate that the Gn glycoprotein of the indicated strain is predicted to not interact with Ab10.
(TIF)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.