Abstract
Background:
Crowdsourcing, the process of shifting individual tasks to a large group, may be useful for health communication, making it more people-centered. We aimed to evaluate whether a crowdsourced video is non-inferior to a social marketing video in promoting condom use.
Methods:
Men who have sex with men (MSM) (≥16 years old, had condomless sex within three months) were recruited and randomly assigned to watch one of the two videos in 2015. The crowdsourced video was developed through an open contest and the social marketing video was designed by using social marketing principles. Participants completed a baseline survey and follow-up surveys at three weeks and three months post-intervention. The outcome was compared with a non-inferiority margin of +10%.
Results:
Among the 1173 participants, 907 (77%) and 791 (67%) completed the three-week and three-month follow-ups. At three weeks, condomless sex was reported by 146/434 (33.6%) and 153/473 (32.3%) participants in the crowdsourced and social marketing arms, respectively. The crowdsourced intervention achieved non-inferiority (estimated difference: +1.3%, 95%CI: −4.8 to 7.4%). At three months, 196/376 (52.1%) and 206/415 (49.6%) individuals reported condomless sex in the crowdsourced and social-marketing arms (estimated difference: +2.5%, 95%CI: −4.5 to 9.5%). The two arms also had similar HIV testing rates and other condom-related secondary outcomes.
Conclusions:
Our study demonstrates that crowdsourced message is non-inferior to a social marketing intervention in promoting condom use among Chinese MSM. Crowdsourcing contests could have a wider reach than other approaches and create more people-centered intervention tools for HIV control.
Keywords: Condomless sex, Crowdsourcing, Health communication, Men who have sex with men, Randomized Controlled Trial
Short Summary:
The Crowdsourced intervention was non-inferior to social marketing intervention in promoting condom use with low cost. The two arms also had similar HIV testing rates and other condom-related secondary outcomes
Introduction
Health communication is the practice of using social media to promote healthy behaviors1. The explosion of new communication technologies has created new opportunities for promoting health2. This explosion is reflected in major public health initiatives focused on enhancing health communication in the United States3 and China4. Health communication interventions are especially helpful in improving health knowledge, supporting health services, and spurring behavior change. Health communication has been shown to increase demand for health services, reduce risk behaviors, and improve health service delivery5,6.
Many health communication interventions draw on the concept of social marketing, which is the systematic application of commercial marketing concepts and techniques to the planning, execution, analysis, and evaluation of programs7,8. Companies often use evidence-based social marketing principles to develop health communication intervention tools for health improvement7,8. Social marketing has emerged as a standard method for developing and implementing health communication interventions9. However, the social marketing approach has generally been a “top-down” approach, relying mostly on experts10. This approach may neglect the knowledge, creativity, and power of non-experts. Insufficient community engagement during the development of social marketing campaigns may result in ultimately less appealing and less effective campaigns.
Crowdsourcing, the process of shifting individual tasks to a group, has the potential to overturn the top-down paradigm of corporate health communication projects. Crowdsourcing differs from conventional health communication methods in two ways10. First, rather than using experts for idea generation, crowdsourcing methods assign idea-generating tasks to the community, promoting direct community engagement. Second, a crowdsourcing approach can be used to design more effective images, policy, and videos10,11. By using some principles of community-based participatory research (involving members of a study population as active and equal participants in the phases of intervention development), crowdsourcing can tap community wisdom to generate new messages to promote condom use among populations that have been challenging to reach through conventional health communication methods. China provides a favorable setting for evaluating crowdsourcing because of two trends. First, government policies encourage innovation, and specifically crowdsourcing, to improve health12. Second, China has large populations among second and third-tier cities, providing a range of in-person and online crowds. In addition, most of the current condom promotion strategies in China were only limited to community-based intervention (i.e. distribute condoms in venues) 13, and promote condom use through social media would be essential.
The purpose of this study was to compare the effectiveness of a crowdsourced video to a social marketing video in promoting condom use among high-risk MSM in China. And a non-inferiority randomized controlled trial was chosen for the following reasons: First, there is a well-established literature on social marketing approaches, and social marketing approach has emerged as a standard method for developing interventions9. Second, a previous study proved that crowdsourced video was non-inferior to social marketing intervention in promoting HIV testing among MSM14, but whether it is also non-inferior to social marketing intervention in promoting condom use is still unclear. Third, the rate of condomless sex is high among MSM in China15. Specifically, given crowdsourcing is a bottom-up approach10, it can substantially increase community engagement and reduce stigma16,17. We anticipated that a crowdsourced intervention has a high likelihood of motivating behavior change among MSM, including condom use.
Materials and Methods
Design
This non-inferiority randomized controlled trial (RCT) evaluated whether a crowdsourced video is non-inferior to a social marketing video in promoting condom use among MSM in China. A control group without a video intervention was not included. The study was conducted between November of 2015 to February of 2016. Prior to participant recruitment, a pilot study with 150 MSM was conducted to evaluate the survey instrument and inform sample size calculation.
The study protocol was approved by Chinese (Guangdong Provincial Centre for Skin Diseases and STI Control) and American (University of North Carolina at Chapel Hill and University of California, San Francisco, No. 15–1522) institutional review boards (Supplement A, Protocol), and has been published18.
Intervention development
This study used a one-minute crowdsourced video intervention and a social marketing video intervention. The crowdsourced video was developed through a crowdsourcing contest in 2015. The reasons for using crowdsourcing contest include: 1) crowdsourcing method is a bottom-up approach, and it uses some principles of community-based participatory research (CBPR), and it has strong potential to engage the people to participate in; 2) crowdsourcing approach was considered to a time-saving, cost-efficient, and useful approach for getting a variety of potentially compelling and effective health communication messages.19–21 We followed the following steps to develop the crowdsourced intervention. First, the eligibility of the crowdsourced video (one-minute short video, relevant, and has the potential to promote condom use among Chinese MSM) was determined by the organizers, and a call for entry was drafted and discussed. Second, the call for entries was publicized on the group websites (gay websites), and through lectures and interactive feedback sessions at college campuses (introduced the crowdsourcing contest through lectures and answered relevant questions to audiences after the lectures). The call for entries was also shared publicly on WeChat (an instant messaging system similar to Facebook and Twitter, with about 1 billion users). Anyone was eligible (not restricted to MSM) to submit a video, while a prize was only provided to the finalist video. After entries had been collected, a group of expert panel was recruited from public health, business, and research sectors selected the finalist video from all entries, by providing each of the video entries with a score of 1 to 10 (1 = worst, 10 = best). The judges identified the contest winner based on the capacity to reach untested individuals, generate excitement, and community responsiveness. Overall, 11 eligible videos were received and scored. The finalist video emphasized the protective function of condoms by showing a wall protecting against cartoon virus (http://v.qq.com/x/page/j0171qo8h75.html). The one-minute social marketing video was shot by a marketing company in Jinan (Shandong, China) following a script was written by social marketing experts in San Francisco (California, USA) and approved by young MSM in the gay community (http://v.qq.com/x/page/c016616uiyl.html). This social-marketing video was specifically designed for this study. It emphasized sexual health as love, with two men negotiating on condom use before having sex 18.
Setting and participants
This is an online RCT, and participants were recruited across China. We partnered with Danlan (Beijing, China), an organization that runs Blued (a gay partner-seeking mobile app with over 27 million users) to recruit the participants online. Banner advertisements were placed on the mobile app, inviting participants to join the survey. This organization also sent announcements through its social media platforms, WeChat and Weibo. All participants who clicked the link for the survey were screened for eligibility. Inclusion criteria included: born biologically as a male, anal sex with a man at least once during their lifetime, condomless anal or vaginal sex in the last three months, and at least 16 years of age. After meeting the screening criteria, participants were asked to sign the informed consent form electronically and to provide a mobile telephone number (only for follow up purpose) and finish an online baseline survey.
After the baseline survey, eligible participants were randomized in a 1:1 ratio using computer-based randomization in Qualtrics (Provo, Utah, USA). This is a blind study, participant recruitment, randomization, and intervention delivery were all computer-based, and the participants did not know whether the video they watched is a crowdsourced video. After finishing the baseline survey, all eligible participants viewed either the crowdsourced video or the social marketing video (without noticing which video they watched). The videos were embedded in the baseline survey, they have to watch the video before they can submit the survey. They completed three-week and three-month follow-up surveys after video watching to assess their condom use after the intervention.
At three weeks and three months post-intervention, the research group sent each participant a text message with a survey link. The surveys included 30 questions about the primary outcome (condom use) and secondary outcomes. Upon completion of the three-week and three-month post-intervention surveys, participants received a mobile credit valued at $16 USD (including $8 USD for the baseline survey) and $8 USD, respectively.
Outcomes
The primary outcome of this study was self-reported condomless sex with a man or woman in the three weeks and three months after intervention. Secondary outcomes for both three weeks and three months post-intervention included condomless sex with a man, condomless sex with a woman, improvement in condom use social norms, improvement in condom self-efficacy, condom negotiation, HIV testing, and syphilis testing.
The baseline survey collected data on socio-demographic characteristics including age, education, annual income, student status, marital status, self-identified sexual orientation, and disclosure of sexual orientation to healthcare provider(s).
Questions on condom use social norms investigated a participant’s perception of their friends’ attitudes towards condom use and safe sex. Each participant was asked to answer six survey items (five-point Likert scale:1=strongly disagree, 5=strongly agree)22. Mean social norm scores were compared to evaluate whether participants experienced a change in social norms after viewing the intervention. Questions on condom use self-efficacy investigated a participant’s intent to use condoms, also measured at both baseline and at the three weeks and three months follow-up, using seven survey items each graded on a five-point Likert scale (graded as above)23. Condom negotiation was defined as an attempt to convince an unwilling partner to use a condom.
Statistical analysis
The sample size for this non-inferiority RCT was determined to assume an equal probability of reporting condomless sex in the crowdsourced video and social marketing video arms. Assuming a 50% probability of condomless sex in each arm, a one-sided α of 2.5%, a non-inferiority limit of 10%, and loss to follow-up of 10%, a total of 1170 individuals was required (585 in each arm) to have 90% power (1-β).
Participant demographic characteristics and sexual risk behaviors were described in each of the intervention arms. The primary endpoint was evaluated using the difference in proportions between the two arms of participants still engaging in condomless sex within three weeks and three months after either intervention (crowdsourced minus social marketing), with a non-inferiority margin of +10%. The upper limit of a Wald 2-sided 95% confidence interval (CI) was used to evaluate non-inferiority.
For the primary outcome, a complete-case analysis was conducted only for participants who completed the three-week and three-month follow-up surveys. A multiple imputation method was conducted as a sensitivity analysis. Covariates in the imputation model were intervention arm, age group, education, home province, sexual orientation, the number of partners in the last three months (prior to baseline) and condom use during a first sexual encounter with another man. Statistical analyses were conducted using SAS version 9.4 (SAS Institute, Cary, NC, USA).
Effect modification was assessed using a linear probability model that included an interaction term between intervention arm and the specified covariate. The purpose of the effect modification is to analyze whether the intervention would have a different effect in different subgroups of MSM. The four pre-specified covariates (whether watched a condom promotion video in the last three weeks prior to intervention, whether watched a testing promotion video in the last three weeks prior to intervention, number of male partners in the last three months prior to intervention, and whether were students) were evaluated.
Results were reported following standardized guidelines (Supplement B, CONSORT Checklists). The study was registered with https://ClinicalTrials.gov(NCT02516930).
Results
Study participants
Overall, the study link was clicked 7892 times. Of these, 341 withdrew from the survey prior to eligibility screening, 5747 did not meet the inclusion criteria, and 194 withdrew before reaching the informed consent, and 413 people did not complete the baseline survey. From the 1197 people who finished our online survey, 24 people were further excluded (5 duplicates, and 19 invalids). Of the remaining 1173 individuals, 578 and 595 were randomly assigned to either the crowdsourced or the social marketing intervention group (Figure 1). Of the 1173 participants, 907 (77%) completed our three-week follow-up online survey, and 791 (67%) completed our three-month follow-up online survey. The response rate was comparable in both arms. The participants who responded to follow-up were similar to those who did not at three weeks, except marital status and sexual orientation (Supplement C).
Figure 1.
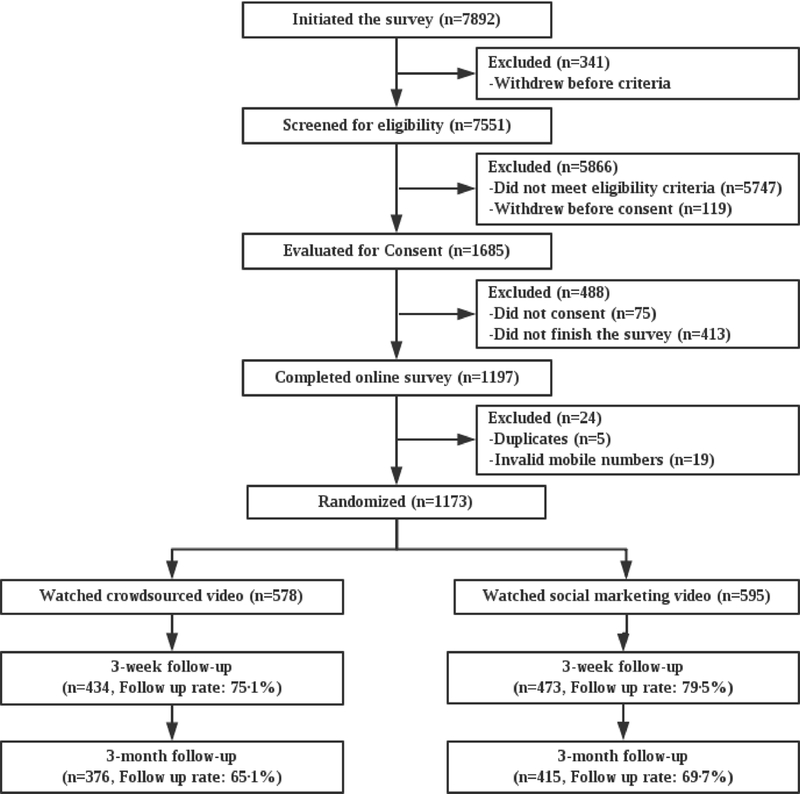
Study cohort (n=1173).
Overall, participants were recruited from 269 cities in 32 provinces of China. Of the 1173 participants, the majority were over 20 years old (71%), never married (83%), and had an annual income less than $15000 United States dollars (USD) (94%). Most of the participants self-identified as homosexual (70%) and over a third were students (36%). All participants identified as men and no participant identified as transgender. Demographics and behaviors were similar between the two intervention arms (Table 1).
Table 1.
Baseline characteristics of study participants recruited into the RCT in China, 2015 (n=1173) *.
| Crowdsourcing (n=578) |
Social Marketing (n=595) | ||
|---|---|---|---|
| Age (years) | 16–20 | 170(29%) | 168(28%) |
| 21–25 | 200(35%) | 221(37%) | |
| Over 25 | 208(36%) | 206(35%) | |
| Marital status | Never married | 473(82%) | 504(85%) |
| Ever married | 105(18%) | 91(15%) | |
| Education | High school or below | 174(30%) | 214(36%) |
| College | 164(28%) | 140(24%) | |
| Graduate education | 240(42%) | 241(41%) | |
| Annual income (USD) | 5,000 or less | 314(54%) | 322(54%) |
| 5001–15000 | 228(39%) | 237(40%) | |
| >15000 | 36(6%) | 36(6%) | |
| Sexual orientation | Homosexual | 412(71%) | 414(70%) |
| Bisexual | 166(29%) | 181(30%) | |
| Student | Yes | 217(38%) | 209(35%) |
| No | 361(62%) | 386(65%) | |
| Disclosure of sexual orientation to health providers | Yes | 180(31%) | 188(32%) |
| No | 398(69%) | 407(68%) | |
| Gender of first sexual partner | Male | 497(86%) | 517(87%) |
| Female | 81(14%) | 78(13%) | |
| Used condom during first sexual encounter with another man | Yes | 274(47%) | 294(49%) |
| No | 304(53%) | 301(51%) | |
| Number of male partners in the last three months | 0 partners | 21(4%) | 29(5%) |
| 1 partner | 266(46%) | 277(46%) | |
| 2 or more | 291(50%) | 289(49%) | |
| Have primary male partner in the last three months§ | Yes | 410(73%) | 419(73%) |
| No | 151(27%) | 153(27%) | |
| Have casual male partner in the last three months§ | Yes | 293(50%) | 309(54%) |
| No | 268(48%) | 263(46%) | |
Baseline characteristics are shown for individuals who had condomless sex in the last three months and were thus eligible for the randomized video intervention.
40 participants had no male partners in the last three months at baseline
Primary condom use outcome
Of the 907 respondents at three weeks, 299 (33%) reported engaging in condomless sex in the three weeks after watching their assigned condom promotion video. In the crowdsourced video arm, 146 of 434 (33.6%) reported condomless sex compared to 153 of 473 (32.3%) in the social marketing video arm. For the complete-case analysis (907 respondents), the estimated difference in proportions between arms was +1.3% (CI: −4.8%, 7.4%). The estimated difference in imputation analysis was +1.3% (95% CI: −4.1%, 6.6%) (Figure 2).
Figure 2.
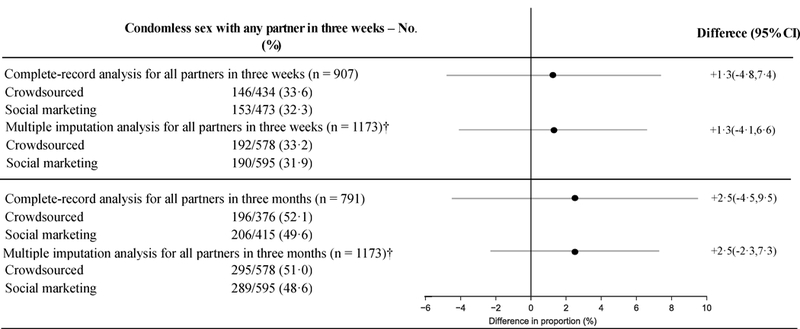
Non-inferiority analysis of the RCT in China, 2015 (n = 1173)
Of the 791 respondents at three months, 537 (68.0%) reported engaging in sex with male only, 28 (3.5%) reported engaged in sex with female only, and 65 (8.2%) reported engaging in sex with both male and female. 402 (50.8%) reported engaging in condomless sex after watching their assigned condom use promotion video. Among the 365 people who reported engaged in condomless sex with male partner in the past three months, 245 (67.1%) engaged in condomless sex with regular partner only, 83 (22.7%) engaged in condomless sex with casual partner only, and 37 (10.1%) engaged in condomless sex with both regular and casual partners. In addition, 58 men engaged in condomless sex with female partners in the last three months. In the crowdsourced video arm, 196 of 376 (52.1%) reported condomless sex compared to 206 of 415 (49.6%) in the social marketing video arm. For the complete-case analysis, the estimated difference in proportions between arms was +2.5% (95% CI: −4.5%, 9.5%, the non-inferiority criteria were met. No significant modification of the intervention effect was observed (Supplement D).
Secondary outcomes at three weeks
For the complete-case analysis, the estimated differences in proportion of condomless sex with a male or female partner between arms were +0.7% (95% CI: −5.2%, 6.6%) and +2.3% (95% CI: −0.8%, 5.3%) for the crowdsourced arm and social marketing arms, respectively (Figure 3).
Figure 3.
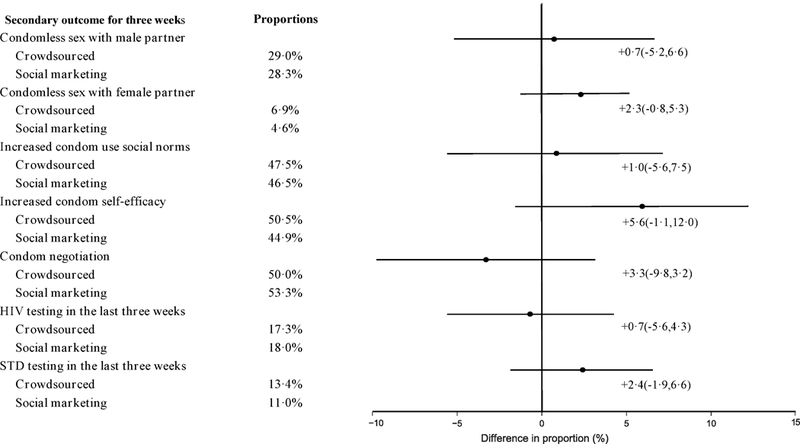
Non-inferiority analysis of secondary outcome at three weeks post-intervention of RCT in China, 2015 (n = 907).
The complete-case analysis showed that the estimated differences between the two intervention arms for condom social norms and condom use self-efficacy, respectively, were +1.0% (95% CI: −5.6%, 7.5%) and +5.6% (95% CI: −1.1%, 12.0%). The post-intervention condom negotiation rates were also similar between the two intervention arms, with a difference of −3.3% (95% CI: −9.8%, 3.2%). The estimated differences in proportions for HIV and syphilis testing between arms from the complete-case analysis were −0.7% (95% CI: −5.6%, 4.3%) and +2.4% (95% CI: −1.9%, 6.6%), respectively.
The secondary outcomes investigated at three months post-intervention are listed in Supplement E. They were similar to those at three weeks post-intervention. At three weeks and three months post-intervention, consistent increased mean total scores for condom use social norm and condom use self-efficacy were observed (Supplement F). Supplement F also indicated that there was no interaction between the other videos watching and the intervention on promoting condom use.
Discussion
This RCT demonstrated that a crowdsourced video was not inferior to a social marketing video in promoting condom use among high-risk MSM in China. Promoting condom use among MSM is challenging24. However, by engaging the community in developing novel and creative solutions,25 crowdsourcing has the potential to create effective interventions that are more acceptable to the community26. Our study extends previous research in condom use promotion among MSM by using crowdsourcing, recruiting only high-risk MSM at greatest risk for HIV, and evaluating both short- and medium-term effects of the intervention.
Our results showed that the video developed through crowdsourcing contest was not inferior to the social marketing video in promoting condom use. This finding is consistent with the sparse literature on using crowdsourcing as a health communications tool for intervention development25. However, the previous study indicated that health communication tools such as video interventions usually have short-term effects, observable immediately after viewing27. One potential method to increase the effect duration is to deliver the intervention through social media platforms more frequently. In addition, since all participants engaged in condomless sex within three months prior to the intervention, and about half of them consistently used condom within three months after the intervention, indicated that both interventions successfully increased condom use among Chinese MSM.
At three months post-intervention, we also found evidence of persistent effects from the crowdsourced intervention, both in the primary outcome (with roughly half of the participants engaging in condomless sex in the three-month post-intervention) and some secondary outcomes, including condom use self-efficacy and social norms total scores. This was especially important, considering the inclusion criteria for our study required participants to have had condomless sex in the three months prior to the study. Our results were promising in terms of the long-term effectiveness of a crowdsourced intervention. However, further research would be useful to determine the optimal frequency of campaigns.
This study has several policy and implementation implications. First, crowdsourcing contests are adaptable to many settings to develop local health campaigns. The multi-sectoral networks and infrastructure necessary for the implementation of such contests are commonly found in a wide range of low- and middle-income countries. By using such networks, crowdsourcing can be used to collect wisdom from large numbers of people to develop health communication tools that are responsive to local challenges. Furthermore, the crowdsourcing contest model used in this study and models using networks could be useful in settings where civil society organizations are constrained or less able to inform public health programs directly7.
Three potential limitations of our study merit discussion. First, the self-selection processes for trial participation itself is an intervention. Especially, the recruited participants were primarily MSM who were young and well educated28, cannot represent all MSM in China, and even cannot represent the registered gay dating app users. However, we anticipated that the bias of the self-selection process would be balanced between the two intervention groups. Second, one-third of participants were lost to follow-up at three months, which could have introduced a selection bias. However, both those who did and did not respond to the follow-up survey were similar in socio-demographic and sexual risk behaviors, and the imputation results accounting for non-response closely matched the complete case data. Third, all the behaviors measured in our study were self-reported, and social desirability bias may be a concern. However, since all of the surveys conducted in our study were computer based29, we anticipated that the strength of this bias was minimal. Fourth, some of our assumptions for sample size calculation (10% loss to follow-up) was not met, as around one-third of the participants lost to follow up in three months. This may reduce the power of the currently reported study. However, based on the remaining samples, our study did achieve a non-inferiority. Fifth, the sample size calculation was based on the primary outcome and may do not have enough power to detect the effect of modification.
Conclusions
While our study demonstrates that a crowdsourced video is non-inferior to social marketing tool in promoting condom use among Chinese MSM, research on crowdsourcing is still very limited. Future studies on crowdsourcing implementation should aim to refine crowdsourcing methods, employ versatile strategies to promote crowdsourcing contests, and induce and sustain community engagement during the entire crowdsourcing process. In addition, studies to evaluate the long-term effects of multiple crowdsourcing communication tools will be critical, as the effect of a single message intervention is very likely to fade over time.30
Supplementary Material
Protocol
CONSORT Checklist
Comparison of Socio-demographic and Sexual Risk Behaviours between Participants Who Did and Did Not Respond to Three Weeks Follow-up Survey in China, 2015 (n=1173)
Effect Modification Analysis of Crowdsourced and Social Marketing Interventions in RCT in China at Three Weeks Post-intervention, 2015 (n=907)
Secondary Outcomes of RCT at Three Months in China, 2015 (n =791)
Total Scales for Social Norm* and Self-efficacy# at Baseline, Three weeks and Three months among Chinese MSM, 2015 Note: *A total score for social norms was calculated at baseline and for both follow-up surveys at three-week and three-month post-intervention for all the six survey items (five-point Likert scale:1=strongly disagree, 5=strongly agree); # A total score for self-efficacy was calculated to reflect the condom use self-efficacy of the participants at baseline and for both follow-up surveys condom for all the seven survey items (five-point Likert scale:1=strongly disagree, 5=strongly
Acknowledgments:
Thanks to Dr. Joseph Eron and Richard Youngblood for reviewing a prior version of this manuscript. We thank all the study participants and staff members at SESH Global, Danlan, and the Guangdong Provincial Center for Skin Diseases and STI Control who contributed. A complete list of acknowledgments is available in the protocol.
Source of Funding:This study received support from the National Key Research and Development Program of China (2017YFE0103800), the National Institutes of Health (NIAID 1R01AI114310–01), UNC-South China STD Research Training Center (FIC 1D43TW009532–01), UNC Center for AIDS Research (NIAID 5P30AI050410), NIMH (R34MH109359), UJMT Fogarty Fellowship (FIC R25TW0093), the North Carolina Translational & Clinical Sciences Institute (1UL1TR001111), SMU Research Initiation Project (QD2017N030 , C1034448), Youth Talent Grant of Guangdong Province (2017WQNCX129), Social Science Young Teacher Supporting Project of Shenzhen University (18QNFC46), and SESH (Social Entrepreneurship to Spur Health) Global.
The funders had no role in study design, data collection, and analysis, decision to publish, or preparation of the manuscript.
Abbreviations
- CI
confidence interval
- MSM
Men who have sex with men
- RCT
randomized controlled trial
- STI
Sexually transmitted infection
Footnotes
Abstract Declaration: The author declared that the abstract of this manuscript has been published on the Lancet (Tang, W., Mao, J., Liu, C., Mollan, K., Li, H., Wong, T., Zhang, Y., Tang, S., Hudgens, M., Qin, Y. and Ma, B., 2016. Crowdsourcing health communication about condom use in men who have sex with men in China: a randomised controlled trial. The Lancet, 388, p.S73), with a link of https://www.sciencedirect.com/science/article/pii/S0140673616320001.
Licence statement: The original dataset of this study is free to share with anyone, and we have included a de-identified dataset for all the readers (Supplement G).
Conflicts of Interest: No conflicts of interest.
References
- 1.Babrow AS, Mattson M, Thompson T, et al. Theorizing about health communication. Handbook of health communication 2003:35–61. [Google Scholar]
- 2.Kreps GL, Neuhauser L. New directions in eHealth communication: opportunities and challenges. Patient education and counseling 2010;78(3):329–36. [DOI] [PubMed] [Google Scholar]
- 3.Emphasizing Parrott R. “communication” in health communication. Journal of Communication 2004;54(4):751–87. [Google Scholar]
- 4.Zhao Y Communication in China: Political economy, power, and conflict: Rowman & Littlefield Publishers 2008. [Google Scholar]
- 5.Ralph LJ, Berglas NF, Schwartz SL, et al. Finding teens in TheirSpace: using social networking sites to connect youth to sexual health services. Sexuality research and social policy 2011;8(1):38–49. [Google Scholar]
- 6.White RO, Eden S, Wallston KA, et al. Health communication, self-care, and treatment satisfaction among low-income diabetes patients in a public health setting. Patient education and counseling 2015;98(2):144–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wei C, Herrick A, Raymond HF, et al. Social marketing interventions to increase HIV/STI testing uptake among men who have sex with men and male-to-female transgender women. Cochrane Database Syst Rev 2011;9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bull SS, Levine DK, Black SR, et al. Social media–delivered sexual health intervention: a cluster randomized controlled trial. American journal of preventive medicine 2012;43(5):467–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gordon R, McDermott L, Stead M, et al. The effectiveness of social marketing interventions for health improvement: what’s the evidence? Public health 2006;120(12):1133–39. [DOI] [PubMed] [Google Scholar]
- 10.Zhang Y, Kim JA, Liu F, et al. Creative Contributory Contests to Spur Innovation in Sexual Health: 2 Cases and a Guide for Implementation. Sexually transmitted diseases 2015;42(11):625–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Qin Y, Liu F, Tang W, et al. HIV self-testing among high-risk men who have sex with men in China: a cross-sectional study. The Lancet 2016;388:S76. [Google Scholar]
- 12.China SCo. State Council Guidance on the accelerating of the building of innovation supporting platform of China. China: State Council of China 2015. [Google Scholar]
- 13.Duan Y, Zhang H, Wang J, et al. Community-based peer intervention to reduce HIV risk among men who have sex with men in Sichuan province, China. AIDS education and prevention : official publication of the International Society for AIDS Education 2013;25(1):38–48. doi: 10.1521/aeap.2013.25.1.38 [published Online First: 2013/02/08] [DOI] [PubMed] [Google Scholar]
- 14.UNAIDS, WHO. Ethical considerations in biomedical HIV prevention trials. Geneva: UNAIDS, 2012:80. [Google Scholar]
- 15.Tang W, Pan J, Jiang N, et al. Correlates of Chlamydia and gonorrhea infection among female sex workers: the untold story of Jiangsu, China. PloS one 2014;9(1):e85985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang TP, Liu C, Han L, et al. Community engagement in sexual health and uptake of HIV testing and syphilis testing among MSM in China: a cross‐sectional online survey. Journal of the International AIDS Society 2017;20(1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang W, Schaffer D, Tso LS, et al. Innovation contests to promote sexual health in china: a qualitative evaluation. BMC public health 2017;17(1):78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu C, Mao J, Wong T, et al. Comparing the effectiveness of a crowdsourced video and a social marketing video in promoting condom use among Chinese men who have sex with men: a study protocol. BMJ open 2016;6(10):e010755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hv Ess. Success Criteria and Strategies for Crowdsourcing www.slideshare.net2010 [cited 2017 May 18, 2017]. Available from: https://www.slideshare.net/searchbistro/harvesting-knowledge-how-to-crowdsource-in-2010 accessed Sep 17, 2010 2010.
- 20.Brabham DC. Crowdsourcing as a Model for Problem Solving An Introduction and Cases. Convergence 2008;14(1):75–90. doi: 10.1177/1354856507084420 [DOI] [Google Scholar]
- 21.Parvanta C, Roth Y, Keller H. Crowdsourcing 101 a few basics to make you the leader of the pack. Health promotion practice 2013;14(2):163–67. [DOI] [PubMed] [Google Scholar]
- 22.DeHart DD, Birkimer JC. Trying to practice safer sex: Development of the sexual risks scale. Journal of Sex Research 1997;34(1):11–25. [Google Scholar]
- 23.Brafford LJ, Beck KH. Development and validation of a condom self-efficacy scale for college students. Journal of American College Health 1991;39(5):219–25. [DOI] [PubMed] [Google Scholar]
- 24.Musinguzi G, Bastiaens H, Matovu JK, et al. Barriers to Condom Use among High Risk Men Who Have Sex with Men in Uganda: A Qualitative Study. PloS one 2015;10(7):e0132297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tang W, Han L, Best J, et al. Crowdsourcing HIV Test Promotion Videos: A Noninferiority Randomized Controlled Trial in China. Clin Infect Dis 2016;62(11):1436–42. [published Online First: 2016/05/01] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ranard BL, Ha YP, Meisel ZF, et al. Crowdsourcing—harnessing the masses to advance health and medicine, a systematic review. Journal of general internal medicine 2014;29(1):187–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vidanapathirana J, Abramson M, Forbes A, et al. Mass media interventions for promoting HIV testing. Cochrane Database Syst Rev 2005;3 [DOI] [PubMed] [Google Scholar]
- 28.Han L, Candidate B, Bien CH, et al. HIV self-testing among online MSM in China: implications for expanding HIV testing among key populations. Journal of acquired immune deficiency syndromes (1999) 2014;67(2):216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mao J, Liu C, Wong T, et al. Crowdsourcing Versus Social Marketing Video Campaigns to Promote Condom Use: A Non-inferiority Randomized Controlled Trial Among MSM and Transgender Individuals in China. 2016. International Behavioral Health conference Hongkong, 2015. [Google Scholar]
- 30.SESH Tucker JD. Crowdsourcing to promote HIV testing among MSM in China: study protocol for a stepped wedge randomized controlled trial. Trials 2017;18(1):447. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Protocol
CONSORT Checklist
Comparison of Socio-demographic and Sexual Risk Behaviours between Participants Who Did and Did Not Respond to Three Weeks Follow-up Survey in China, 2015 (n=1173)
Effect Modification Analysis of Crowdsourced and Social Marketing Interventions in RCT in China at Three Weeks Post-intervention, 2015 (n=907)
Secondary Outcomes of RCT at Three Months in China, 2015 (n =791)
Total Scales for Social Norm* and Self-efficacy# at Baseline, Three weeks and Three months among Chinese MSM, 2015 Note: *A total score for social norms was calculated at baseline and for both follow-up surveys at three-week and three-month post-intervention for all the six survey items (five-point Likert scale:1=strongly disagree, 5=strongly agree); # A total score for self-efficacy was calculated to reflect the condom use self-efficacy of the participants at baseline and for both follow-up surveys condom for all the seven survey items (five-point Likert scale:1=strongly disagree, 5=strongly


