Abstract
Rationale:
Tailgut cysts are a type of very rare congenital polycystic lesions that are always located posterior to the rectum and anterior to the sacrum. The symptoms of tailgut cysts are nonspecific and misleading. Therefore, a full understanding of the characteristics of tailgut cysts is important for their diagnosis and treatment.
Patient concerns:
We report a 46-year-old female with a sacrococcygeal mass that had been present for about 2 years.
Diagnoses:
Pelvic magnetic resonance imaging (MRI) indicated several cystic masses, the largest of which had a diameter of about 2.8 cm, near the ligaments of the sacrospinous and rectum. Pathological examination confirmed the tailgut cysts, with no signs of malignant transformation.
Interventions:
The patient received complete surgical cysts resection, which was performed through the sacrococcygeal region.
Outcomes:
The patient recovered well with no obvious complication and was discharged on the sixth-day post-surgery. Follow-up 6 months later revealed no signs of cyst recurrence.
Lessons:
The symptoms and diagnostic characteristics of tailgut cysts should be fully understood. Complete surgical resection through the sacrococcygeal region is vital to treat tailgut cysts.
Keywords: magnetic resonance imaging, MRI, surgery, tailgut cyst
1. Introduction
Tailgut cysts, also termed retrorectal cystic hamartomas, are a very rare type of congenital cyst that are mainly located in the presacral space.[1] They have also been reported anterior to the rectum and perianally.[2,3] It is believed that tailgut cysts are derived from the remnant of the embryonic hindgut.[4,5] Tailgut cysts can occur in any age but are more in mid-fifth age females.[4] The clinical symptoms of tailgut cysts are nonspecific and misleading, and biopsy of the cyst always leads to infection and hemorrhage, which further increase the difficulty of radical resection.[3,4] Therefore, if the surgeons do not have sufficient understanding of the characteristics of tailgut cysts and certain concepts and skills for surgical resection, or cannot make a precise diagnosis, rapid recurrence after surgery may occur.
In this study, we report a rare case of tailgut cyst and share our experience of the diagnosis and treatment of tailgut cysts.
2. Case report
This study was approved by the Ethics Committee and Institutional Review Board of the Second Hospital of Jilin University, Changchun, China. Patient has provided informed consent for publication of the case.
A 46-year-old woman came to our hospital with a sacrococcygeal mass that had been present for about 2 years. She denied any nausea, vomiting, abdominal pain, abdominal distention, or fecal abnormalities. She defected 1 to 2 times 1 day and there was no black stool or purulent blood stool observed. There was also no sense of urgency when defecating. Furthermore, the patient also denied a history of diabetes, hypertension, coronary heart disease, or acute and chronic infectious diseases. However, she received teratoma resection surgery 6 years ago. The anorectal examination revealed that the color of the anus was normal, no solid mass could be felt when the forefinger was extended into the anus for about 7 cm, and no blood or pus was observed on the surface of the fingerstall. Pelvic magnetic resonance imaging (MRI) indicated several cystic masses, the largest of which had a diameter of about 2.8 cm, in the fifth sacral vertebra level, near the ligaments of the sacrospinous and rectum (Fig. 1). In addition, MRI also revealed patchy signals in the pelvic cavity with high signal intensity on both T1-weighted and T2-weighted images (Fig. 1). These signals were adjacent to the uterus and were considered to be pelvic effusion. No evidence of tumor invasion or pelvic or inguinal lymph node metastasis was observed. Based on the MRI results, the masses were considered to cysts. Thus, biopsy was not performed to avoid hepatoma formation and bleeding.
Figure 1.
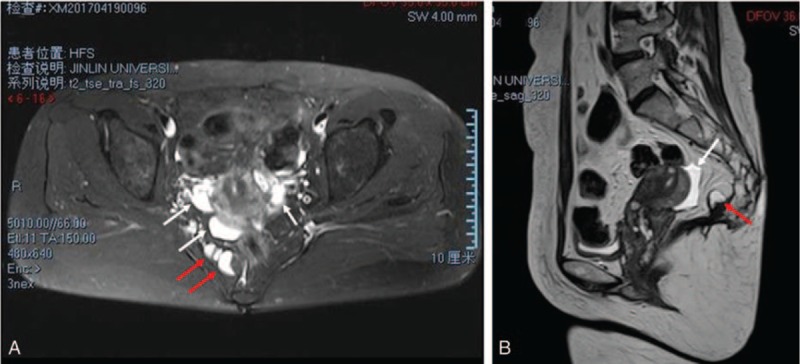
MRI evaluation of the tailgut cysts in (A) cross-section and (B) longitudinal section. Red arrows indicate the tailgut cysts and white arrows indicate pelvic effusion. MRI = magnetic resonance imaging.
At laparotomy, the patient underwent a 10 cm long incision located on the right side of the sacral anterior. Part of the sacrum was dissected to expose the surgical field. A 3.0 × 2.0 × 2.0 cm sized cystic mass (Fig. 2A) was observed near the posterior right rectum, and was carefully dissected. Furthermore, several small cystic masses (Fig. 2B) were observed near the rectum, which were also dissected successfully. Histopathological examination demonstrated multiple cysts that were covered with squamous and glandular epithelia (Fig. 3). In addition, fresh and old bleeding was observed around the walls of the cysts (Fig. 3). The patient recovered well and was discharged on the sixth-day post-surgery. Follow-up 6 months later revealed no signs of cyst recurrence.
Figure 2.
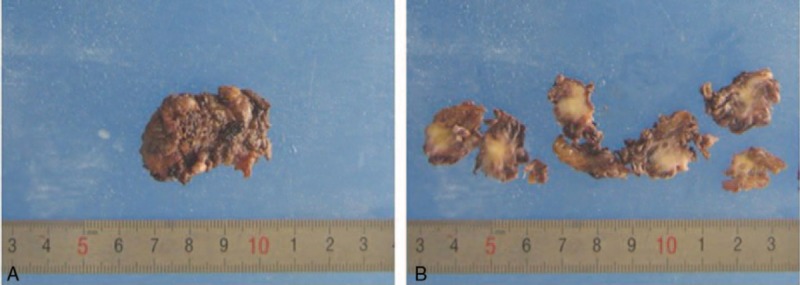
Gross pathology of the tailgut cysts. (A) A 3.0 × 2.0 × 2.0 cm sized cystic mass. (B) Multiple small tailgut cysts.
Figure 3.
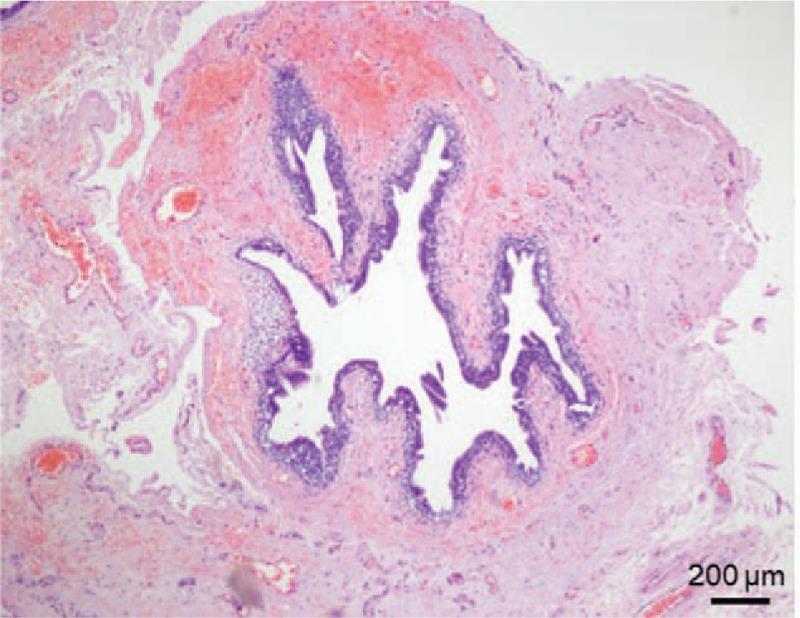
Histological examination (hematoxylin and eosin staining) of the tailgut cysts.
3. Discussion
Tailgut cysts are very rare congenital polycystic lesions that are always located in the anterior sacral space, which is the space that is posterior to the rectum and anterior to the sacrum. Goenuel et al first reported a case of tailgut cyst and concluded that the cyst was the remnant of the embryonic tailgut.[6] Epidemiological data showed that the majority of patients with tailgut cysts are female. However, some researchers believe that the true number of patients with tailgut cysts may be higher than just those in female patients because female patients have higher frequency of pelvic floor examination.[7]
Epidemiological data indicated that in the vast majority of patients, the cysts do not extend to the body surface.[4] As a result, the symptoms of tailgut cysts are nonspecific and obscure at the early stage. For the patients with obvious symptoms, the cysts always compress nearby tissues or organs and are always accompanied by infections.[8] For example, if the cysts compress the rectum, defecation can be abnormal and abdominal pain may be obvious; if the cysts compress the bladder or ureter, urination may be abnormal; and if the cysts compress the phrenic nerve, sciatic nerve, or psionic nerve, neuropathic pain may occur.[9] For the cysts that extend to the body surface, fistulas may be observed. In our report, the patient only had a 3 cm-sized sacrococcygeal mass (plus a few smaller cysts) with no other obvious symptoms. As a result, early diagnosis of tailgut cysts can be difficult and misleading. MRI improves tissue characterization and is usually used to diagnose tailgut cysts.[4] Unilocular or multilocular cystic appearance could be observed on MRI. The cysts usually present with low signal intensity on T1-weighted images and high signal intensity on T2-weighted images.[10,11] However, high signal intensity on T1-weighted images might also be observed because of the presence of mucinous material and hemorrhage within the cysts.[12] In our study, the cysts presented with high signal intensities on both T1-weighted and T2-weighted images, because a large area of hemorrhage was present within the cysts, based on the histopathological examination. In addition, small cysts often clustered together and a honeycomb pattern can sometimes be seen on MRI.[10] A computed tomography (CT) scan can also reveal the location, margins, and connections with the neighboring structures of the tailgut cysts. However, MRI is superior to CT to detect small cysts, because MRI provides a satisfactory view of the association of the cysts with the nearby rectum and bony structures.[13] Pathological examination is still the gold standard for the diagnosis of tailgut cysts. However, radiologically guided biopsy can lead to hemorrhage, which may further induce infection of the cysts.[4] As a result, for the cysts that seem invasive or malignant, biopsy can be performed. However, for solid and resectable cysts, surgical resection should be performed immediately instead of a biopsy.
The volume of the cysts is always large and malignant transformation often occurs; therefore, complete surgical resection is preferred for tailgut cysts.[14] Currently, there are 2 surgical methods for tailgut cysts: Open surgery and laparoscopic minimally invasive surgery.[4] Laparoscopic minimally invasive surgery has many advantages; however, the anterior space of the sacrum is small and the cysts are large, which leads to poor exposure of the surgical area and may result in incomplete resection. In addition, it is difficult to create a cavity for minimally invasive surgery if it is performed through the sacrococcygeal region.[4] Therefore, open surgery is suitable for the resection of tailgut cysts. Open surgery for tailgut cysts can be performed in 3 ways, including through the abdomen, the abdomen and sacrococcygeal region, and the sacrococcygeal region.[15] It is easy to detect and examine the cysts when performing abdominal surgery;[4] however, peritoneal adhesion, which is a common postoperative complication, may occur. When the surgery is performed through the abdomen and sacrococcygeal region, the body position of the patient should be changed during the operation, which might result in incision infection. Furthermore, injury to the body may be serious if the operation is performed through the abdomen and sacrococcygeal region.[4,15] However, when the surgery is performed through the sacrococcygeal region only, the surgical area can be well exposed, which benefits the complete resection of the tailgut cysts, decreases the recurrence rate of the cysts, and avoids complications. Moreover, the sacrococcygeal incision is more hidden than the other 2 methods, which can meet women's cosmetic requirements.[4,15]
In the reported case, tailgut cysts occurred in the sacrococcygeal region. MRI and histopathological examinations confirmed the diagnosis of tailgut cysts. Complete surgical resection was performed and the patient recovered well, with no cyst recurrence for 6 months. This study also shared our experience of the diagnosis and treatment of tailgut cysts.
Author contributions
Formal analysis: Kai Zhang.
Investigation: Jian Shi, Tongjun Liu.
Methodology: Kai Zhang, Tongjun Liu.
Project administration: Jian Shi, Kai Zhang.
Validation: Jian Shi.
Writing – original draft: Jiannan Li, Xiaowei Song.
Writing – review & editing: Kai Zhang, Tongjun Liu.
Footnotes
Abbreviation: MRI = magnetic resonance imaging.
JL and XS contributed equally to this work.
The authors have no conflicts of interest to disclose.
References
- [1].Mora-Guzman I, Casado APA, Sanchez AR, et al. Tailgut cysts: Presentation of four cases. Gastroenterol Hepatologia 2018;41:103–5. [DOI] [PubMed] [Google Scholar]
- [2].Levert LM, VavRooyen W, VandenBergen HA. Cysts of the tailgut. Eur J Surg 1996;162:149–52. [PubMed] [Google Scholar]
- [3].Sidoni A, Bucciarelli E. Ciliated cyst of the perineal skin. Am J Dermatopathol 1997;19:93–6. [DOI] [PubMed] [Google Scholar]
- [4].Patsouras D, Pawa N, Osmani H, et al. Management of tailgut cysts in a tertiary referral centre: a 10-year experience. Colorectal Dis 2015;17:724–9. [DOI] [PubMed] [Google Scholar]
- [5].Gouloumis AR, Tsakiraki Z, Zacharatou A, et al. The borderland of embryology and pathology revisited: two cases of tailgut cysts. Virchows Archiv 2017;471:S252–3. [Google Scholar]
- [6].GonuL II, Baglan T, Pala I, et al. Tailgut cysts: diagnostic challenge for both pathologists and clinicians. Int J Colorectal Dis 2007;22:1283–5. [DOI] [PubMed] [Google Scholar]
- [7].Saad RJ, Rao SSC, Koch KL, et al. Do stool form and frequency correlate with whole-gut and colonic transit? Results from a multicenter study in constipated individuals and healthy controls. Am J Gastroenterol 2010;105:403–11. [DOI] [PubMed] [Google Scholar]
- [8].Haider N, Shaheen I, Squire R, et al. Tailgut cysts in children: a report of two cases and literature review. Pediatr Surg Int 2015;31:597–601. [DOI] [PubMed] [Google Scholar]
- [9].Ostiz M, Yanguas N, Jimenez G, et al. Retrorectal cystic hamartoma (tailgut cyst): an uncommon cause of recurrent abdominal pain. An Sist Sanit Navar 2017;40:303–7. [DOI] [PubMed] [Google Scholar]
- [10].Aflalo-Hazan V, Rousset P, Mourra N, et al. Tailgut cysts: MRI findings. Eur Radiol 2008;18:2586–93. [DOI] [PubMed] [Google Scholar]
- [11].Shetty AS, Loch R, Yoo N, et al. Imaging of tailgut cysts. Abdom Imaging 2015;40:2783–95. [DOI] [PubMed] [Google Scholar]
- [12].Lim KE, Hsu WC, Wang CR. Tailgut cyst with malignancy: MR imaging findings. Am J Roentgenol 1998;170:1488–90. [DOI] [PubMed] [Google Scholar]
- [13].Yang DM, Park CH, Jin W, et al. Tailgut cyst: MRI evaluation. Am J Roentgenol 2005;184:1519–23. [DOI] [PubMed] [Google Scholar]
- [14].Charalampakis V, Stamatiou D, Christodoulakis M, et al. A large presacral tailgut cyst with a carcinoid tumor in a male: report of a case. Surg Today 2014;44:961–6. [DOI] [PubMed] [Google Scholar]
- [15].Volk A, Plodeck V, Toma M, et al. Treatment of tailgut cysts by extended distal rectal segmental resection with rectoanal anastomosis. Surg Today 2017;47:457–62. [DOI] [PubMed] [Google Scholar]


