Abstract
This study aimed to compare the differences in radiological outcomes and complications between single- and multilevel anterior cervical discectomy and fusion (ACDF) by using a polyetheretherketone (PEEK) cage–plate fusion system.
Fifty-seven patients who underwent ACDF via the PEEK cage–plate fusion system were enrolled and subjected to ≥6 months of follow-up. The patients were divided into 4 groups according to different cage–plate implantation levels: 1-level group (n = 17), 2-level group (n = 24), 3-level group (n = 12), and 4-level group (n = 4). Fusion time, changes in segment and global lordotic angle, subsidence rate, and changes in disc and adjacent segmental disc height were subjected to radiological evaluation.
The fusion period of multilevel ACDF was longer than that of single-level ACDF. The fusion period of the 3-level (4.09 ± 0.94, P = .004) and 4-level (5.25 ± 0.89, P = .004) group was also significantly longer than that of the 1-level group. The mean lordotic angle in all of the groups was changed in the immediate postoperative period and in the final follow-up. The cage subsidence rates were 11.76% (2/17) in the 1-level group, 20.83% (5/24) in the 2-level group, and 2/12 (16.67%) in the 3-level group. No subsidence occurred in the 4-level groups. Changes in the lower adjacent segmental disc height were significantly increased in multilevel ACDF compared with those in single-level ACDF.
Despite the longer fusion time, the outcomes of the proposed system were even better with the greater number of treatment levels by using PEEK cage–plate fusion system. Changes in the lower adjacent segmental disc height should also prolong follow-up duration to investigate the symptomatic adjacent segment degeneration in multilevel ACDF.
Keywords: adjacent segment degeneration, anterior cervical discectomy and fusion, cervical, degenerative disc disease, subsidence
1. Introduction
Anterior cervical discectomy and fusion (ACDF), first proposed by Smith and Robinson in 1958,[1] is considered a standard procedure for the treatment of cervical degenerative disc disease (DDD) following the failure of conservative treatments.[2–4] Although autologous iliac bone can provide solid fusion, donor-site morbidity and complications, such as subsidence, occur.[5–9] To resolve this problem, researchers developed various stand-alone cervical cages with different materials, such as stainless metal, titanium, carbon fiber, and polyetheretherketone (PEEK).[10,11] Cages with plates can also enhance stability, shorten fusion duration, and reduce the subsidence rate.[12]
High cage subsidence rates with high treatment levels remain controversial.[13] Cage–plate systems likely decrease the adjacent disc height and thus cause adjacent segment degeneration (ASD).[14,15] The main factor affecting ASD is other preoperative ASD out of adjacent segments.[16] To our knowledge, few studies have compared radiographic outcomes and complications between single- and multilevel ACDF.[17] In the present study, the use of a PEEK cage with a PEEK plate was retrospectively analyzed between single- and multilevel ACDF, which is more elastic and biocompatible than cages with steel and titanium plates. We hypothesized that a PEEK cage–plate fusion system could provide support capability and elasticity to prevent the incidence of subsidence with high treatment levels and provide improved outcomes. This study aimed to compare the differences in radiological outcomes and complications between single- and multilevel ACDF with PEEK cage–plate systems.
2. Methods
2.1. Patients
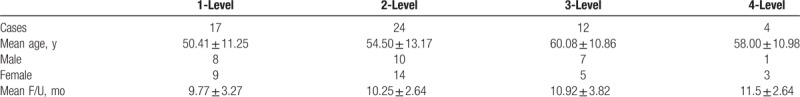
The study was performed at China Medical University Hospital and was approved by the local Institutional Review Board. A total of 57 patients who underwent ACDF by using a PEEK cage–plate system (Biomech-Paonan Biotech Co., Ltd., Taipei, Taiwan) for cervical DDD were enrolled from 2014 to 2016. The patients were divided into 4 groups according to different cage–plate implantation levels: 1-level group (n = 17), 2-level group (n = 24), 3-level group (n = 12), and 4-level group (n = 4). The mean age was 50.41 years (27–68 years) for 1-level, 54.50 years (35–86 years) for 2-level, 60.08 years (46–78 years) for 3-level, and 58.00 years (49–74 years) for the 4-level group. These groups consisted of males and females with the following ratios: 8:9 for 1-level group, 10:14 for 2-level group, 7:5 for 3-level group, and 1:3 for 4-level group. The mean follow-up period was 9.77 months (6–15 months) for 1-level, 10.25 months (7–18 months) for 2-level, 10.92 months (7–21 months) for 3-level, and 11.5 months (9–15 months) for the 4-level group (Table 1).
Table 1.
Patient demographic data.
2.2. Surgical procedure
All patients underwent surgery were performed by Han-Chung Lee using a standard Smith–Robinson approach under general anesthesia with the patients in supine position. A Caspar distractor was placed at a specific level, the anterior longitudinal ligament was cut, discectomy was performed, and the osteophyte was removed. The adjacent cartilage was also removed carefully to avoid excessive bony endplate destruction. Before the disc was inserted into the space, the optimal cage size was determined by inserting cage-shaped trial sticks (height = 5, 6, and 7 mm). A horse-shaped cage with a hollow cylinder was filled with biphasic calcium phosphate ceramic (Triosite, 40% b-tricalcium phosphate[b-TCP] and 60% hydroxyapatite; Biomatlante, France). For plate augmentation, the PEEK plate was used to fix the disc, and the cranial and the caudal vertebral body were fixed with screws. The operations were performed under the C-arm. All of the patients were instructed to wear a neck collar for 1 week.
2.3. Radiological assessment
Plain radiographs (anterior–posterior, lateral, and flexion–extension) obtained on preoperative, immediately after surgery, and at each follow-up were used to evaluate cervical alignment, segmental angle, and fusion status. Cervical lordosis was assessed using Cobb's angle. Global alignment was measured by determining Cobb's angle between the inferior endplate of C2 and C7 vertebral body. Segmental alignment was measured by Cobb's angle between the upper endplate of the cranial vertebral body and the lower endplate of the caudal vertebral body. An independent radiologist assessed the radiographs without the knowledge of clinical outcomes. The cage subsidence in the radiographs was defined as >3 mm reduction in the vertebral body height because of cage migration into the adjacent endplates between the immediate postoperative and the final follow-up. Fusion was characterized by <2° movement through lateral flexion–extension radiography, bridging bone between endplates, no signs of implant failure of PEEK cage–plate system, and <50% of radiolucency covering the implant's outer surface.[18] Disc height was measured as the distance between the center point of the inferior endplate of the upper vertebral body and the superior endplate of the lower vertebral body. Changes in disc height were determined on the basis of the differences between pre- and postoperation.
2.4. Statistical analysis
Data plotting and analysis were performed using GraphPad Prism. Data were represented as mean ± SD. Pre- and postoperative global and segmental angles were statistically assessed with Wilcoxon signed-rank test. Fusion time comparisons and adjacent height changes among groups with different ACDF levels by using the PEEK cage–plate system were statistically assessed with Mann–Whitney U test. Significance was set at P < .05.
3. Results
A total of 57 patients who underwent ACDF by using a PEEK cage–plate system (Fig. 1) for cervical DDD were enrolled from 2014 to 2016. Plain radiographs obtained on preoperative, immediately after surgery, and at each follow-up were used to evaluate cervical alignment, segmental angle, and fusion status (Fig. 2).
Figure 1.
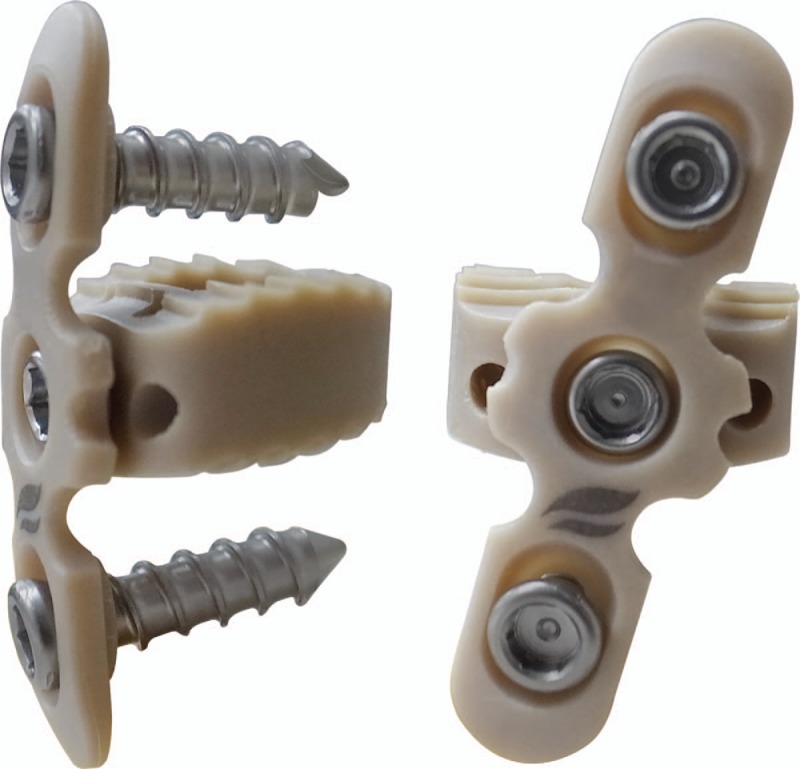
Proposed PEEK cage with a plate (Biomech-Paonan Biotech Co., Ltd., Taipei, Taiwan).
Figure 2.
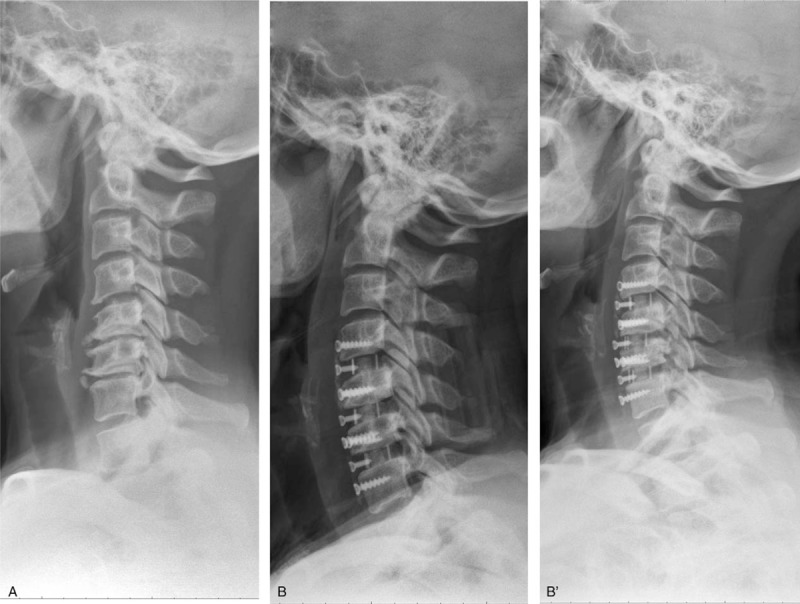
Preoperative (A), postoperative (B), and final follow-up (B’) lateral cervical radiographs showing the bony fusion at C4 to C7 levels with a PEEK cage–plate system.
The fusion time of multilevel ACDF was longer than that of single-level ACDF. The fusion of the 3-level (4.09 ± 0.94, P = .004) and 4-level (5.25 ± 0.89, P = .004) group was also significantly longer than that of the 1-level group (Table 2). This finding indicated that the PEEK cage–plate system provided milder fusion by requiring a longer period in the multilevel groups than in the single-level group. Global and segment lordotic angles were changed in the immediate postoperative period and in the final follow-up in all of the groups. The lordotic angles of the 2- and 3-level groups significantly changed (Table 3). However, the lordotic angle of the segment in the 2-level group was not significant (P = .059).
Table 2.
Fusion rate and mean fusion time.
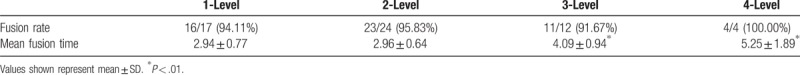
Table 3.
Mean lordotic angle of global and segment.
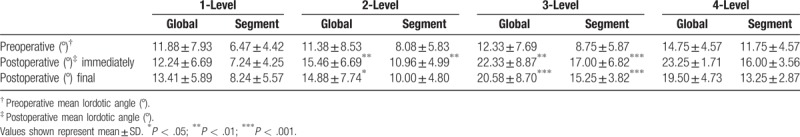
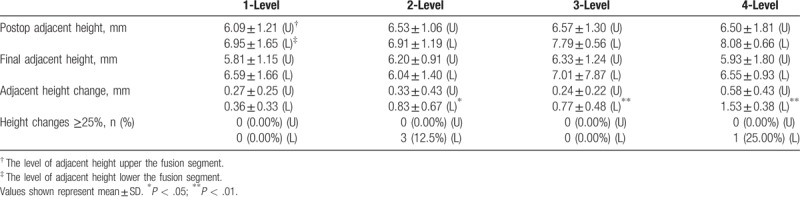
The cage subsidence rates were 11.76% (2/17) in the 1-level group, 20.83% (5/24) in the 2-level group, and 2/12 (16.67%) in the 3-level group. No subsidence occurred in the 4-level groups (Table 4). These subsidences did not cause clinical problems, suggesting that multilevel ACDF was recommended and performed using the PEEK cage–plate system. However, the changes in the lower adjacent segmental disc height significantly increased in the 2-level (0.83 ± 0.67, P = .0153), 3-level (0.77 ± 0.48, P = .0196), and 4-level (1.53 ± 0.38, P = .001) groups compared with the single-level (0.36 ± 0.33) ACDF (Table 5). Moreover, the 3 patients (12.5%) in 2-level group and 1 patient (25.00%) in 4-level group were degenerative changes (height changes ≥25%) in lower adjacent levels.
Table 4.
Changes in disc height.
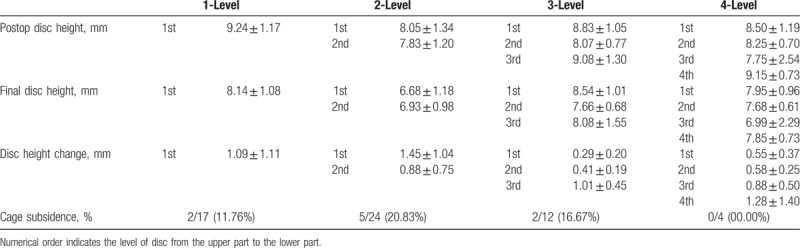
Table 5.
Changes in adjacent height.
To prevent symptomatic ASD, we should identify the changes in the adjacent disc height of patients, especially those diagnosed with other cases of preoperative segment degeneration.
4. Discussion
ACDF with a cervical cage for DDD treatment has become an alternative surgical procedure to prevent subsidence and donor-site complication caused by classical methods involving autologous iliac bone graft.[6–8,19] Nevertheless, these complications can be reduced by various stand-alone cervical cages composed of materials, such as titanium, carbon fiber, and PEEK, which provide stability, height restoration, and interbody fusion.[10,11,18] Donor-site morbidity impedes the efficient use of all types of these cervical cages. Titanium cages can restore the initial disc height and lordosis, although unfavorable outcomes and complications, such as cage subsidence, migration, disc height collapse, and kyphotic deformity, have been reported.[20–24] Metallic cages are radiopaque and thus unsuitable for observation under plain radiographs. Carbon fiber cages can be effective for cervical alignment and solid fusion.[25,26] Nevertheless, a high subsidence rate (29.2%) has been detected.[27] Comparatively, cages composed of PEEK materials are biocompatible and elasticity modulus is similar to that of the bone.[28,29] As a result, cage subsidence is reduced and solid fusion is facilitated. Moreover, bone fusion can be radiologically evaluated with plain radiographs because of the radiolucency of the PEEK cages.
Despite the advantages and the reduced risk of subsidence for ACDF with stand-alone PEEK cages, the occurrence of subsidence with a high treatment level is inevitable.[13] Although a PEEK cage with a plate, which is considered stable, can be used to prevent graft extrusion and increase the bone fusion rate,[30] a high rate of subsidence (23.8%) is detected with 3-level ACDF.[31] The rate of subsidence is similar between 2-level ACDF with PEEK cages with (30%) or without (31.81%) plate fixation containing screw.[32] To consider the excessive rigidity of plate fixation with screw, we retrospectively analyzed ACDF with a PEEK cage and a PEEK plate between single- and multilevel ACDF, which is more elastic and more biocompatible than cages with steel and titanium plate. Therefore, we determined whether the proposed PEEK cage–plate system could provide support capability and elasticity to prevent the incidence of subsidence with high treatment level and provide enhanced outcomes. In the present study, fusion time was longer than those of the single-level group. Therefore, this observation indicated that fusion in multilevel ACDF was milder than that in single-level ACDF. Global and lordotic angles increased in single- and multilevel ACDF. However, the segment lordotic angle in the 2-level group was not significant (P = .059) probably because of insufficient sample size. No changes in evident disc height in single- and multilevel groups were observed. The cage subsidence rates were 11.76% (2/17) in the 1-level group, 20.83% (5/24) in the 2-level group, and 2/12 (16.67%) in the 3-level group. No subsidence occurred in the 4-level groups (Table 4). Cage subsidence usually occurs within 3 months and does not progress thereafter.[31,33,34] Therefore, we suggested that outcomes could be enhanced by PEEK cages with PEEK plates, although treatment levels were high.
Another plate-related complications include ASD. ACDF using a cage with a plate increases the adjacent segmental motion and decreases the adjacent segmental disc height.[14] The main factor affecting ASD is preoperative other ASD out of adjacent segment. Patients over the age of 50 are at a high risk of developing ASD. The degenerative changes were indicated with disc signal change, anterior/posterior disc herniation, calcification of the anterior/posterior longitudinal ligament, anterior/posterior osteophytes, and a decrease in disc height of ≥25%.[16] In the present study, the lower adjacent segmental disc height significantly increased in the 2-level (0.83 ± 0.67, P = .0153), 3-level (0.77 ± 0.48, P = .0196), and 4-level (1.53 ± 0.38, P = .001) groups compared with the single-level (0.36 ± 0.33) ACDF (Table 5). Moreover, the 3 patients (12.5%) in 2-level group and 1 patient (25.00%) in 4-level group were high risk of degenerative changes (height changes ≥25%) in lower adjacent levels. This finding suggested that ASD should be identified, while multilevel ACDF is performed. High rates of plate-related complications involve dysphasia and ossification.[35,36] With technical advancements, these complications can be avoided. Dysphagia is associated with plate thickness and protrusion off the vertebral body.[37–39] Changes in cervical plate thickness can reduce the incidence of dysphagia. Additional plates should be placed ≥5 mm away from adjacent disc spaces to decrease the likelihood of moderate-to-severe adjacent-level ossification and thus prevent ossification.[35]
The present study is limited by several factors, namely, retrospective nature, small sample size, lack of control group, and dysphagia incidence. Therefore, a stand-alone cage group and dysphagia outcomes should be included. A prospective study comparing single- and multilevel ACDF and involving a larger sample size should be considered for further investigation.
5. Conclusions
Despite the longer fusion time, the proposed PEEK cage–plate system provided even better outcomes in multilevel groups by using PEEK cage–plate fusion system. Changes in lower adjacent height should also be identified to prevent symptomatic ASD in multilevel ACDF. Further investigations on the subsidence rate and changes in radiological outcomes should be performed to prolong follow-up.
Acknowledgment
We thank Chien-Ping Hsieh for assistance with manuscript preparation.
Author contributions
Conceptualization: Han-Chung Lee, Yueh-Sheng Chen.
Data curation: Han-Chung Lee, Chao-Hsuan Chen, Chih-Ying Wu, Jeng-Hung Guo, Yueh-Sheng Chen.
Formal analysis: Han-Chung Lee, Chao-Hsuan Chen, Chih-Ying Wu, Yueh-Sheng Chen.
Investigation: Han-Chung Lee, Jeng-Hung Guo, Yueh-Sheng Chen.
Methodology: Han-Chung Lee.
Project administration: Han-Chung Lee, Yueh-Sheng Chen.
Supervision: Han-Chung Lee.
Validation: Han-Chung Lee, Chao-Hsuan Chen, Chih-Ying Wu, Jeng-Hung Guo, Yueh-Sheng Chen.
Writing – original draft: Han-Chung Lee, Yueh-Sheng Chen.
Writing – review and editing: Han-Chung Lee, Yueh-Sheng Chen.
Han-Chung Lee orcid: 0000-0002-9471-1692.
Footnotes
Abbreviations: ACDF = anterior cervical discectomy and fusion, ASD = adjacent segment degeneration, DDD = degenerative disc disease, PEEK = polyetheretherketone.
The study was performed at the China Medical University Hospital and approved by the local Institutional Review Board (CMUH107-REC2-030).
The authors have no funding and conflicts of interest to disclose.
References
- [1].Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am 1958;40-A:607–24. [PubMed] [Google Scholar]
- [2].Chen Y, He Z, Yang H, et al. Anterior cervical diskectomy and fusion for adjacent segment disease. Orthopedics 2013;36:e501–8. [DOI] [PubMed] [Google Scholar]
- [3].Riew KD, Ecker E, Dettori JR. Anterior cervical discectomy and fusion for the management of axial neck pain in the absence of radiculopathy or myelopathy. Evid Based Spine Care J 2010;1:45–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Miller LE, Block JE. Safety and effectiveness of bone allografts in anterior cervical discectomy and fusion surgery. Spine 2011;36:2045–50. [DOI] [PubMed] [Google Scholar]
- [5].Palmer W, Crawford-Sykes A, Rose RE. Donor site morbidity following iliac crest bone graft. West Indian Med J 2008;57:490–2. [PubMed] [Google Scholar]
- [6].Silber JS, Anderson DG, Daffner SD, et al. Donor site morbidity after anterior iliac crest bone harvest for single-level anterior cervical discectomy and fusion. Spine 2003;28:134–9. [DOI] [PubMed] [Google Scholar]
- [7].Siddiqui AA, Jackowski A. Cage versus tricortical graft for cervical interbody fusion. A prospective randomised study. The Journal of bone and joint surgery. J Bone Joint Surg Br 2003;85:1019–25. [DOI] [PubMed] [Google Scholar]
- [8].Vavruch L, Hedlund R, Javid D, et al. A prospective randomized comparison between the cloward procedure and a carbon fiber cage in the cervical spine: a clinical and radiologic study. Spine 2002;27:1694–701. [DOI] [PubMed] [Google Scholar]
- [9].Yang JJ, Yu CH, Chang BS, et al. Subsidence and nonunion after anterior cervical interbody fusion using a stand-alone polyetheretherketone (PEEK) cage. Clin Orthop Surg 2011;3:16–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Kast E, Derakhshani S, Bothmann M, et al. Subsidence after anterior cervical inter-body fusion. A randomized prospective clinical trial. Neurosurg Rev 2009;32:207–14. [DOI] [PubMed] [Google Scholar]
- [11].Kulkarni AG, Hee HT, Wong HK. Solis cage (PEEK) for anterior cervical fusion: preliminary radiological results with emphasis on fusion and subsidence. Spine J 2007;7:205–9. [DOI] [PubMed] [Google Scholar]
- [12].Oh JK, Kim TY, Lee HS, et al. Stand-alone cervical cages versus anterior cervical plate in 2-level cervical anterior interbody fusion patients: clinical outcomes and radiologic changes. J Spinal Disord Tech 2013;26:415–20. [DOI] [PubMed] [Google Scholar]
- [13].Kao TH, Wu CH, Chou YC, et al. Risk factors for subsidence in anterior cervical fusion with stand-alone polyetheretherketone (PEEK) cages: a review of 82 cases and 182 levels. Arch Orthop Trauma Surg 2014;134:1343–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Ahn SS, Paik HK, Chin DK, et al. The fate of adjacent segments after anterior cervical discectomy and fusion: the influence of an anterior plate system. World Neurosurg 2016;89:42–50. [DOI] [PubMed] [Google Scholar]
- [15].Ji GY, Oh CH, Shin DA, et al. Stand-alone cervical cages versus anterior cervical plates in 2-level cervical anterior interbody fusion patients: analysis of adjacent segment degeneration. J Spinal Disord Tech 2015;28:E433–8. [DOI] [PubMed] [Google Scholar]
- [16].Ahn SS, So WS, Ku MG, et al. Radiologic findings and risk factors of adjacent segment degeneration after anterior cervical discectomy and fusion: a retrospective matched cohort study with 3-year follow-up using MRI. J Korean Neurosurg Soc 2016;59:129–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Nunley PD, Jawahar A, Kerr EJ, 3rd, et al. Choice of plate may affect outcomes for single versus multilevel ACDF: results of a prospective randomized single-blind trial. Spine 2009;9:121–7. [DOI] [PubMed] [Google Scholar]
- [18].Kandziora F, Pflugmacher R, Scholz M, et al. Treatment of traumatic cervical spine instability with interbody fusion cages: a prospective controlled study with a 2-year follow-up. Injury 2005;36Suppl. 2:B27–35. [DOI] [PubMed] [Google Scholar]
- [19].Banwart JC, Asher MA, Hassanein RS. Iliac crest bone graft harvest donor site morbidity. A statistical evaluation. Spine (Phila Pa 1976) 1995;20:1055–60. [DOI] [PubMed] [Google Scholar]
- [20].Chou YC, Chen DC, Hsieh WA, et al. Efficacy of anterior cervical fusion: comparison of titanium cages, polyetheretherketone (PEEK) cages and autogenous bone grafts. J Clin Neurosci 2008;15:1240–5. [DOI] [PubMed] [Google Scholar]
- [21].Hauerberg J, Kosteljanetz M, Boge-Rasmussen T, et al. Anterior cervical discectomy with or without fusion with ray titanium cage: a prospective randomized clinical study. Spine 2008;33:458–64. [DOI] [PubMed] [Google Scholar]
- [22].Kolstad F, Nygaard OP, Andresen H, et al. Anterior cervical arthrodesis using a “stand alone” cylindrical titanium cage: prospective analysis of radiographic parameters. Spine 2010;35:1545–50. [DOI] [PubMed] [Google Scholar]
- [23].Niu CC, Chen LH, Lai PL, et al. Trapezoidal titanium cage in anterior cervical interbody fusion: a clinical experience. Chang Gung Med J 2005;28:212–21. [PubMed] [Google Scholar]
- [24].Niu CC, Liao JC, Chen WJ, et al. Outcomes of interbody fusion cages used in 1 and 2-levels anterior cervical discectomy and fusion: titanium cages versus polyetheretherketone (PEEK) cages. J Spinal Disord Tech 2010;23:310–6. [DOI] [PubMed] [Google Scholar]
- [25].Marotta N, Landi A, Tarantino R, et al. Five-year outcome of stand-alone fusion using carbon cages in cervical disc arthrosis. Eur Spine J 2011;20Suppl. 1:S8–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].van der Haven I, van Loon PJ, Bartels RH, et al. Anterior cervical interbody fusion with radiolucent carbon fiber cages: clinical and radiological results. Acta Orthop Belg 2005;71:604–9. [PubMed] [Google Scholar]
- [27].Bartels RH, Donk RD, Feuth T. Subsidence of stand-alone cervical carbon fiber cages. Neurosurgery 2006;58:502–8. [DOI] [PubMed] [Google Scholar]
- [28].Toth JM, Wang M, Estes BT, et al. Polyetheretherketone as a biomaterial for spinal applications. Biomaterials 2006;27:324–34. [DOI] [PubMed] [Google Scholar]
- [29].Wenz LM, Merritt K, Brown SA, et al. In vitro biocompatibility of polyetheretherketone and polysulfone composites. J Biomed Mater Res 1990;24:207–15. [DOI] [PubMed] [Google Scholar]
- [30].Sudprasert W, Kunakornsawat S. A preliminary study of three and four levels degenerative cervical spondylosis treated with peek cages and anterior cervical plate. J Med Assoc Thai 2012;95:909–16. [PubMed] [Google Scholar]
- [31].Song KJ, Kim GH, Choi BY. Efficacy of PEEK cages and plate augmentation in three-level anterior cervical fusion of elderly patients. Clin Orthop Surg 2011;3:9–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Joo YH, Lee JW, Kwon KY, et al. Comparison of fusion with cage alone and plate instrumentation in two-level cervical degenerative disease. J Korean Neurosurg Soc 2010;48:342–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Barsa P, Suchomel P. Factors affecting sagittal malalignment due to cage subsidence in standalone cage assisted anterior cervical fusion. Eur Spine J 2007;16:1395–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Li Z, Zhao Y, Tang J, et al. A comparison of a new zero-profile, stand-alone Fidji cervical cage and anterior cervical plate for single and multilevel ACDF: a minimum 2-year follow-up study. Eur Spine J 2017;26:1129–39. [DOI] [PubMed] [Google Scholar]
- [35].Park JB, Cho YS, Riew KD. Development of adjacent-level ossification in patients with an anterior cervical plate. J Bone Joint Surg Am 2005;87:558–63. [DOI] [PubMed] [Google Scholar]
- [36].Yue WM, Brodner W, Highland TR. Persistent swallowing and voice problems after anterior cervical discectomy and fusion with allograft and plating: a 5- to 11-year follow-up study. Eur Spine J 2005;14:677–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Barbagallo GM, Romano D, Certo F, et al. Zero-P: a new zero-profile cage-plate device for single and multilevel ACDF. A single institution series with four years maximum follow-up and review of the literature on zero-profile devices. Eur Spine J 2013;22Suppl. 6:S868–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Chin KR, Eiszner JR, Adams SB., Jr Role of plate thickness as a cause of dysphagia after anterior cervical fusion. Spine 2007;32:2585–90. [DOI] [PubMed] [Google Scholar]
- [39].Yang H, Chen D, Wang X, et al. Zero-profile integrated plate and spacer device reduces rate of adjacent-level ossification development and dysphagia compared to ACDF with plating and cage system. Arch Orthop Trauma Surg 2015;135:781–7. [DOI] [PubMed] [Google Scholar]


