Abstract
Rationale:
Because of the lack of an antidote or effective treatment, patients with severe acute diquat and glyphosate poisoning always died within a few hours. Extracorporeal membrane pulmonary oxygenation (ECMO), as an artificial heart-lung supporting system, can be applied to support lung that is expected to recover from reversible pathological damage. However, to our knowledge, the application of ECMO for patients with diquat and glyphosate poisoning has not been reported.
Patient concerns:
A 40-year-old man ingested in 100 ml of diquat (20 g/100 ml) and 400 ml glyphosate (41 g/100 ml) was admitted to the intensive care unit (ICU), immediately complicated by the development of ventricular fibrillation, respiratory failure, renal failure, and multi-organ failure.
Diagnosis:
Diquat and glyphosate poisoning were diagnosed by stated ingestion history, and the diagnostic criteria for acute respiratory distress syndrome (ARDS) and multi-organ dysfunction syndrome were also met.
Interventions:
He was treated with veno-venous ECMO.
Outcomes:
He was successfully transferred out of the ICU on day 46 and discharged on day 67. The computed tomography scan showed no obvious pulmonary fibrosis 2 months after poisoning.
Lessons:
ECMO may be effective in the treatment of patients with severe ARDS caused by diquat and glyphosate poisoning when conventional management does not work.
Keywords: case report, diquat, extracorporeal membrane oxygenation therapy, glyphosate, poisoning
1. Introduction
Diquat and glyphosate are widely used herbicides.[1,2] With the suspension of sales and domestic use of paraquat in China, diquat is becoming more and more widely used in agricultural production market, and the number of diquat poisoning cases is also gradually increasing. Ingestion of diquat and herbicides may cause severe and fatal poisoning.[1,3–5] Because of a lack of an antidote, the development of respiratory failure, renal failure, hypotension, and multi-organ dysfunction syndrome (MODS) is highly associated with poor prognosis.[6–9] As a technology capable of providing short-term mechanical support to the lungs, extracorporeal membrane pulmonary oxygenation (ECMO) was associated with reduced mortality in patients with very severe acute respiratory distress syndrome (ARDS).[10–13] However, no precedented experience could be followed in the treatment of diquat and glyphosate poisoning.[14–16] We herein report a case of an adult male patient with diquat and glyphosate poisoning who was successfully treated with ECMO therapy.
2. Case presentation
A 40-year-old man was admitted to the department of emergency in August 2018 due to committing suicide by intentional ingestion of about 100 ml diquat (20 g/100 ml) and 400 ml glyphosate (41 g/100 ml). His wife provided a history of depression. Three hours before admission, his family found the patient unconscious and his vomit around. He was immediately sent to the emergency department of our hospital. Gastric lavage with montmorillonite and endotracheal intubation were performed immediately and then the patient was transferred into the intensive care unit (ICU). Examination on admission to the ICU revealed ventricular fibrillation. His heart rate returned to normal after 20 minutes cardiopulmonary resuscitation and defibrillation. Ventricular fibrillation recurred 40 minutes later and the same treatment was given until he recovered. Physical examination revealed comatose with Glasgow Coma Scale score of 7. His temperature was 38.6°C with a normal heart rate of 68beats/min (bpm), blood pressure of 116 /76 mm Hg (with norepinephrine 10 ug/min) and respiratory rate 44/min (bpm). Oxygen saturation was about 90% using tracheal intubation and assisted ventilation (BIPAP mode was set with PC 20cmH20, PEEP 10cmH20, and FiO2 100%). Physical examination also showed oral and tracheal hemorrhage, wet rales over both lungs on pulmonary auscultation and abdominal distension. Within a few hours, his oxygen saturation fell to 85% on ventilation and progressive oliguria developed. Laboratory tests suggested severe hypoxia and liver and kidney function damage (Table 1). Bedside chest radiography suggested multiple exudations of both lungs (Fig. 1).
Table 1.
Laboratory tests on the first day and discharge.
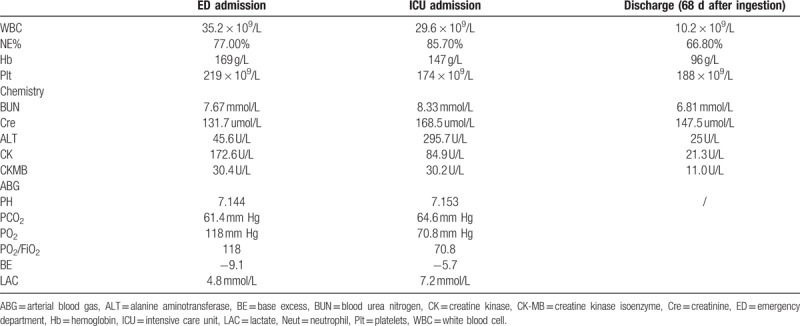
Figure 1.
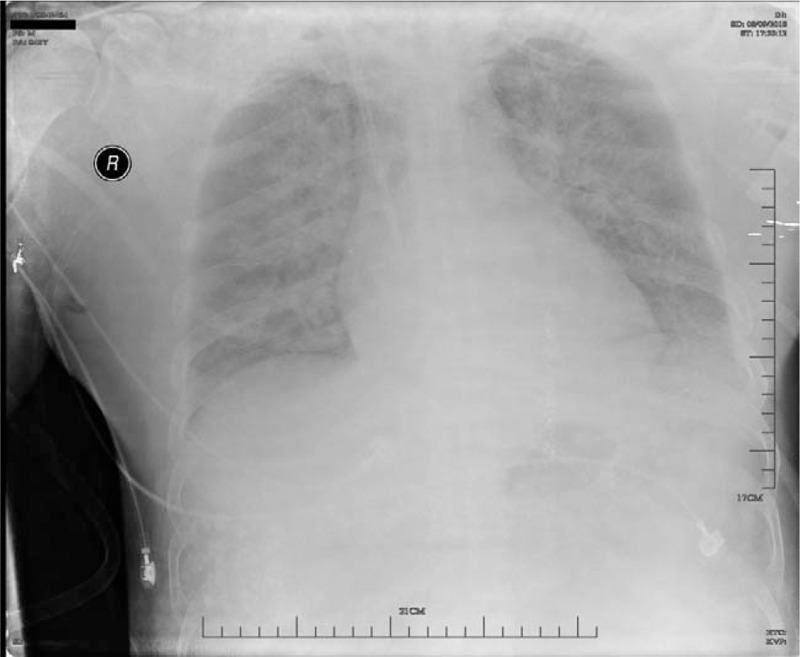
Chest X-ray on admission: Multiple exudative lesions in both lungs.
After successful cardiopulmonary resuscitation, resuscitation fluid to maintain blood pressure, protective lung ventilation strategy to maintain oxygenation, removement of toxins, antioxidant and antifibrotic treatment were given. However, his oxygenation deteriorated on day 2 with the PO2/FiO2 being less than 100. Veno-venous ECMO program was initiated on day 2 and he was weaned off ECMO support successfully after 140 hours. On day 9 after admission, endotracheal intubation and mechanical ventilation were removed. Immediately after admission, the patient was treated with continuous veno-venous hemofiltration (CVVH), but his renal function recovered slowly. He was withdrawn from CVVH on the 41st day after admission. The patient was discharged from the Department of Nephrology on day 46 and was discharged on the 68th day after admission. No obvious lesions were found in the chest CT on the 5th day after discharge (Fig. 2).
3. Discussion
Diquat and glyphosate, as the second and third most widely used herbicides in the world, are mainly used for weeding in agriculture.[1,2] Diquat sold in the market is mainly aqueous 20% solutions with the lethal dose to humans about 6 to 12 g.[17] Old age (>40 years), ingestion a large dose (>200 ml), an elevated creatinine level, acidosis, hyperkalemia, tachycardia, and respiratory failure requiring intubation are fatal risk factors for glyphosate poisoning.[6,7,9,17] Although much fewer cases of diquat and glyphosate poisoning were reported in the literature than those of paraquat poisoning, clinicians need to give greater attention to its high mortality rate.
The main mechanism of diquat toxicity is related to its redox cycle, inducing reactive oxygen species and reactive nitrogen species generation, oxidative stress, and cell death.[4,17–19] The precise mechanism of glyphosate poisoning is still unclear. Surfactants are considered the most toxic component in glyphosate.[20] It has been reported that surfactants can inhibit the oxidation of phosphine, damage cellular components, such as mitochondria, cell membrane, DNA, and protein synthetic machinery. The combined poisoning with diquat and glyphosate may aggravate the damage of vital organs such as lung and kidney.
The combined poisoning with diquat and glyphosate may cause severe mucosal damage including edema and hemorrhage.[4,5,17,21] Central nervous system symptoms include coma, epileptic seizures, and hemorrhage.[4,22] Shock and malignant arrhythmia may also occur in some cases.[3,4,17,23] The occurrence of complications is dose-related. The kidney is the main target organ and the main pathological changes involve tubular necrosis.[1,4,17,24] Renal toxicity and pulmonary toxicity seem to be responsible for mortality.[9] Respiratory system symptoms include bronchial pneumonia and pulmonary edema. Mechanical ventilation is required in severe cases.[3,4,17,21] Patients with acute lung injury in the early stage often complicated with severe pulmonary edema and other injuries because of aspiration, which will aggravate hypoxemia and threaten the patients’ lives. In this case, the patient suffered from severe ARDS not only due to the toxin damage but also severe aspiration.
There is no specific antidote for diquat and glyphosate.[1,2,4,17] The main treatment for systemic toxicity is toxins removal and active organ support therapy including administration of inhibitors on diquat-mediated enzymatic reaction activity or low molecular weight antioxidants. Other therapeutic strategies include reducing the absorption of toxins and promoting excretion.[4,17] However, in cases with severe ARDS and MODS, the routine lung protective ventilation strategies and organ function support cannot improve patients’ clinical condition.
In recent years, as a life-saving therapy, ECMO has been widely used in clinical practice.[14] ECMO is effective for patients with severe respiratory failure, which can prevent ventilator-related lung injury in a late stage.[10] The improvement in the patients’ severe hypoxia can avoid more serious hypoxia damage and secondary damage, thus preventing further aggravation of the disease. However, we still lack experience regarding the role of ECMO in the treatment of diquat and glyphosate poisoning, with few case reports.[12,15,16] It has been reported that ECMO was effective for patients with glyphosate poisoning complicated with cardiovascular and respiratory damage.
The use of ECMO in acute paraquat poisoning can serve as a transitional supportive therapy for lung transplantation.[16] There are also clinicians who question the effects of ECMO, considering that pulmonary fibrosis may occur in later stages, and this process cannot be reversed. Although the pathogenic mechanism of diquat is similar to that of paraquat, the clinical symptoms and late changes of patients with diquat poisoning are still different from those of the patients with paraquat poisoning. The incidence of pulmonary fibrosis is significantly lower than that of the patients with paraquat poisoning. It has even been reported that pulmonary fibrosis will not occur for patients with diquat poisoning.[4,17]
The patient, in this case, survived severe hypoxemia at the early stage of using ECMO, reducing further systemic organ damage caused by severe hypoxia. Extubation was successfully and the patient was discharged on the 68th day after admission. Chest CT showed no obvious pulmonary fibrotic lesions on the 73rd day after admission (Fig. 2).
Figure 2.
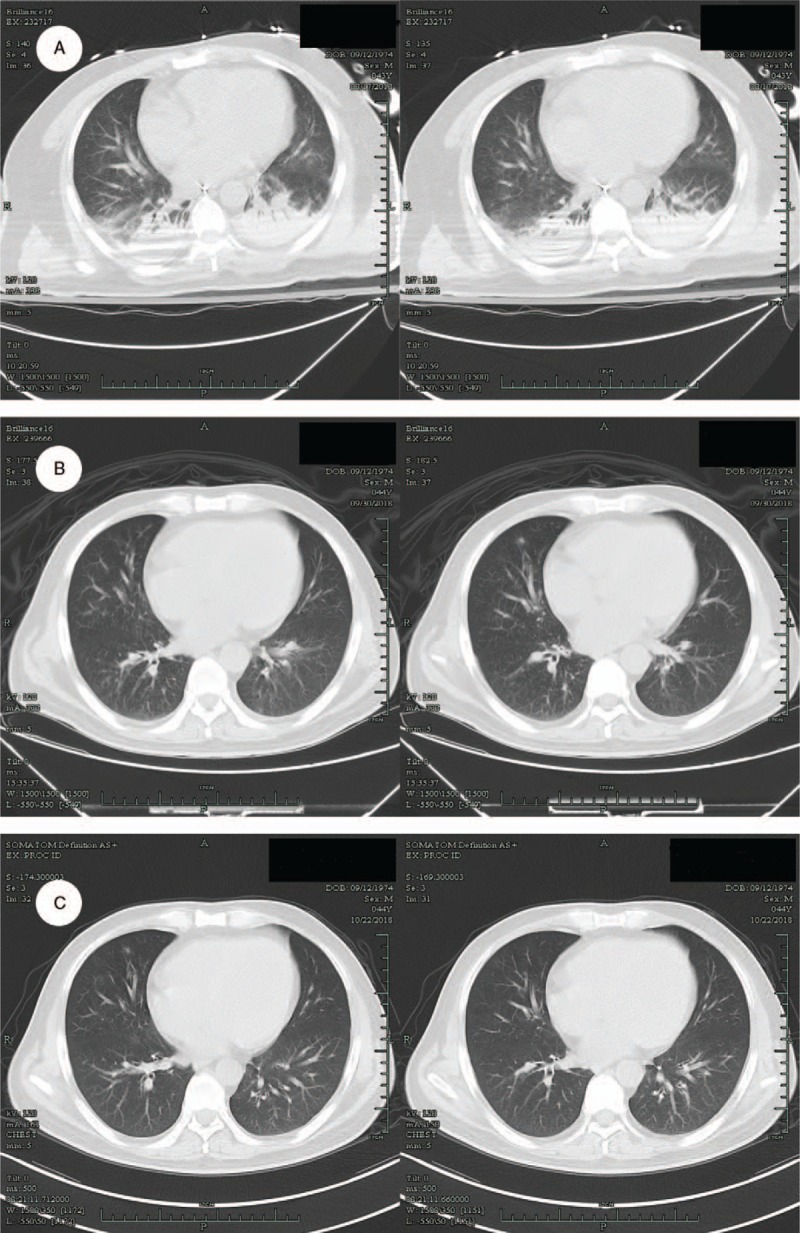
Imaging (A) The 8th day after poisoning: Multiple infiltration of the lower lobes of both lungs. (B) The 52th day after poisoning: There were few exudative lesions in both lungs and no obvious fibrotic lesions. (C) The 5th day after dischage: No obvious lesions were found in the both lungs.
In summary, we report the first case of successful treatment of combined diquat and glyphosate poisoning using ECMO. This case suggests that ECMO may be an effective treatment option for patients with severe diquat and glyphosate poisoning complicated with ARDS after failure of routine treatment.
Acknowledgments
The authors thank the patient and his family for allowing us to present the disease course in this report.
Author contributions
Data curation: Danqiong Wang, Weiwen Zhang, Jian Luo, Lihua Zhu, Jianhua Hu.
Project administration: Danqiong Wang, Weiwen Zhang.
Supervision: Danqiong Wang, Weiwen Zhang.
Visualization: Danqiong Wang, Weiwen Zhang.
Writing – original draft: Danqiong Wang, Weiwen Zhang.
Writing – review and editing: Danqiong Wang, Weiwen Zhang, Jian Luo, Lihua Zhu, Jianhua Hu.
Image diagnostic analysis: Guozheng Zhang.
Conceptualization: Danqiong Wang, Weiwen Zhang.
Data curation: Danqiong Wang, Weiwen Zhang, Jian luo, Lihua Zhu, Jianjian Hu.
Formal analysis: Danqiong Wang, Weiwen Zhang.
Investigation: Danqiong Wang, Weiwen Zhang.
Methodology: Danqiong Wang.
Project administration: Danqiong Wang.
Resources: Danqiong Wang.
Software: Guozheng Zhang.
Supervision: Danqiong Wang.
Writing – original draft: Danqiong Wang.
Writing – review and editing: Danqiong Wang, Weiwen Zhang, Jian luo, Lihua Zhu, Jianjian Hu.
Footnotes
Abbreviations: ARDS = acute respiratory distress syndrome, ECMO = extracorporeal membrane pulmonary oxygenation, ICU = intensive care unit, MODS = multi-organ dysfunction syndrome.
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
The authors have no conflicts of interest to disclose.
References
- [1].Fortenberry GZ, Beckman J, Schwartz A, et al. Magnitude and characteristics of acute paraquat- and diquat-related illnesses in the US: 1998–2013. Environ Res 2016;146:191–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Chen YJ, Wu ML, Deng JF, et al. The epidemiology of glyphosate-surfactant herbicide poisoning in Taiwan, 1986–2007: a poison center study. Clin Toxicol (Phila) 2009;47:670–7. [DOI] [PubMed] [Google Scholar]
- [3].Picetti E, Generali M, Mensi F, et al. Glyphosate ingestion causing multiple organ failure: a near-fatal case report. Acta Biomed 2018;88:533–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Magalhaes N, Carvalho F, Dinis-Oliveira RJ. Human and experimental toxicology of diquat poisoning: toxicokinetics, mechanisms of toxicity, clinical features, and treatment. Hum Exp Toxicol 2018;37:1131–60. [DOI] [PubMed] [Google Scholar]
- [5].Jovic-Stosic J, Babic G, Todorovic V. Fatal diquat intoxication. Vojnosanit Pregl 2009;66:477–81. [DOI] [PubMed] [Google Scholar]
- [6].Cho YS, Moon JM, Chun BJ, et al. Use of Qsofa Score in Predicting the Outcomes of Patients with Glyphosate Surfactant Herbicide Poisoning Immediately Upon Arrival at the Emergency Department. Shock (Augusta, Ga.), 2018. [DOI] [PubMed] [Google Scholar]
- [7].Cho YS, Chun BJ, Moon JM. The qSOFA score: a simple and accurate predictor of outcome in patients with glyphosate herbicide poisoning. Basic Clin Pharmacol Toxicol 2018;123:615–21. [DOI] [PubMed] [Google Scholar]
- [8].Roberts DM, Buckley NA, Mohamed F, et al. A prospective observational study of the clinical toxicology of glyphosate-containing herbicides in adults with acute self-poisoning. Clin Toxicol (Phila) 2010;48:129–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Lee CH, Shih CP, Hsu KH, et al. The early prognostic factors of glyphosate-surfactant intoxication. Am J Emerg Med 2008;26:275–81. [DOI] [PubMed] [Google Scholar]
- [10].Parekh M, Abrams D, Brodie D, et al. Extracorporeal membrane oxygenation for ARDS: optimization of lung protective ventilation. Respir Care 2018;63:1180–8. [DOI] [PubMed] [Google Scholar]
- [11].Goligher EC, Tomlinson G, Hajage D, et al. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome and posterior probability of mortality benefit in a post hoc bayesian analysis of a randomized clinical trial. JAMA 2018;320:2251–9. [DOI] [PubMed] [Google Scholar]
- [12].Ramanathan K, Tan CS, Rycus P, et al. Extracorporeal membrane oxygenation for poisoning in adult patients: outcomes and predictors of mortality. Intensive Care Med 2017;43:1538–9. [DOI] [PubMed] [Google Scholar]
- [13].Qian L, Zheng J, Xu H, et al. Extracorporeal membrane oxygenation treatment of a H7N9-caused respiratory failure patient with mechanical valves replacement history: a case report. Medicine 2016;95:e5052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Fan E, Gattinoni L, Combes A, et al. Venovenous extracorporeal membrane oxygenation for acute respiratory failure: a clinical review from an international group of experts. Intensive Care Med 2016;42:712–24. [DOI] [PubMed] [Google Scholar]
- [15].Chan CW, Wu IL, Lee CH, et al. Successful extracorporeal life support in a case of severe glyphosate-surfactant intoxication. Crit Care Med 2016;44:e45–47. [DOI] [PubMed] [Google Scholar]
- [16].Tang X, Sun B, He H, et al. Successful extracorporeal membrane oxygenation therapy as a bridge to sequential bilateral lung transplantation for a patient after severe paraquat poisoning. Clin Toxicol (Phila) 2015;53:908–13. [DOI] [PubMed] [Google Scholar]
- [17].Jones GM, Vale JA. Mechanisms of toxicity, clinical features, and management of diquat poisoning: a review. J Toxicol Clin Toxicol 2000;38:123–8. [DOI] [PubMed] [Google Scholar]
- [18].Circu ML, Maloney RE, Aw TY. Diquat-induced cellular pyridine nucleotide redox changes and alteration of metabolic enzyme activities in colonic carcinoma cells. Chem Biol Interact 2017;264:43–51. [DOI] [PubMed] [Google Scholar]
- [19].Fussell KC, Udasin RG, Gray JP, et al. Redox cycling and increased oxygen utilization contribute to diquat-induced oxidative stress and cytotoxicity in Chinese hamster ovary cells overexpressing NADPH-cytochrome P450 reductase. Free Radic Biol Med 2011;50:874–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Seok SJ, Park JS, Hong JR, et al. Surfactant volume is an essential element in. human toxicity in acute glyphosate herbicide intoxication. Clin Toxicol (Phila) 2011;49:892–9. [DOI] [PubMed] [Google Scholar]
- [21].Thakur DS, Khot R, Joshi PP, et al. Glyphosate poisoning with acute pulmonary edema. Toxicol Int 2014;21:328–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Saeed SA, Wilks MF, Coupe M. Acute diquat poisoning with intracerebral bleeding. Postgrad Med J 2001;77:329–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Moon JM, Chun BJ, Cho YS, et al. Cardiovascular effects and fatality may differ according to the formulation of glyphosate salt herbicide. Cardiovasc Toxicol 2018;18:99–107. [DOI] [PubMed] [Google Scholar]
- [24].Hantson P, Wallemacq P, Mahieu P. A case of fatal diquat poisoning: toxicokinetic data and autopsy findings. J Toxicol Clin Toxicol 2000;38:149–52. [DOI] [PubMed] [Google Scholar]


