Abstract
To evaluate retrospectively any association between the degree of deformity correction by medial open-wedge high tibial osteotomy (HTO) and patellofemoral joint degeneration. We hypothesized that development of patellofemoral joint degeneration depended on the degree of intraoperative deformity correction.
Fifty-seven patients who underwent medial open-wedge HTO for treatment of osteoarthritis in one knee were included in this study. Knees were classified into degeneration (D) and non-degeneration (ND) groups according to worsening of the patellar and/or femoral trochlear cartilage at the time of hardware removal (D group, 27 knees) and no degeneration or improvement (ND group, 30 knees). We compared pre- to post-surgery change in hip-knee-ankle angle (HKA) and medial-proximal-tibial angle (MPTA), open-wedge HTO correction angle, and arthroscopic findings between groups.
Mean age, height, weight, and body mass index were 54.1 ± 9.9 years, 160.4 ± 8.7 cm, 66.4 ± 12.1 kg, and 25.7 ± 3.3 kg/m2, respectively. Change in both HKA and MPTA differed significantly between groups. The MPTA cut-off values to predict patellofemoral degeneration were determined to be 10°, associated with an AUC of 0.75 (95% confidence interval [CI] 0.62–0.87).
This study evaluated retrospectively the effect of the correction angle during medial open-wedge HTO on patellofemoral joint degeneration. If deformity correction exceeds an MPTA of 10° during open-wedge HTO, degeneration of patellofemoral joint needs to be considered.
Level of evidence: Level IV.
Keywords: cartilage degeneration, high tibial osteotomy, patellofemoral joint
1. Introduction
Medial open-wedge high tibial osteotomy (HTO) using a locking plate is the standard surgical method in treatment of medial knee osteoarthritis providing favorable outcomes.[1–3] In medial open-wedge HTO, osteotomy is applied at a proximal site of the tibial tuberosity, and the alignment is corrected from the varus to the valgus by opening the medial side of the tibia. This results in a shift in tibial tuberosity from the joint surface toward the distal side, a downward shift of the patella to a lower level, and an increase in patellofemoral pressure, changes that may be problematic.[4] However, medial open-wedge HTO may sometimes result in significant degeneration in the patellofemoral joint cartilage, which may subsequently influence the patellofemoral joint.[5] In contrast, a cadaveric study showed that a 15-mm opening of the osteotomized region resulted in significantly higher patellofemoral joint pressure than a 10-mm opening,[6] suggesting that, among medial open-wedge HTO-related factors, the degree of correction influences the patellofemoral joint. If large deformity correction negatively influences the patellofemoral joint, other surgical procedure might be a better option. We hypothesized that a large degree of deformity correction in medial open-wedge HTO would negatively influence the patellofemoral joint, whereas a small degree of deformity correction would have little effect. This study tested our hypothesis by retrospectively examining cases to assess the influence of the correction angle in medial open-wedge HTO on subsequent degeneration of patellofemoral joint cartilage. We compared the medial open-wedge HTO correction angle and arthroscopic findings in available patients before and after their surgical treatment.
2. Materials and methods
This study was approved by the Institutional Review Board of Kyoto Interdisciplinary Institute Hospital of Community Medicine (ERB-29-1) and all subjects provided written informed consent (29th May, 2017).
2.1. Patients
We conducted a retrospective case-series study of 57 consecutive patients (15 men, 42 women), who underwent medial open-wedge HTO for treatment of medial knee osteoarthritis between January 2009 and June 2015 in the Orthopaedics Department of Kyoto Prefectural University of Medicine and Kyoto Interdisciplinary Institute Hospital of Community Medicine. Inclusion criteria was Kellgren-Lawrence classification grade 2 or 3; symptomatic unicompartmental osteoarthritis of medial femorotibial joint; flexion contracture less than 10°; and younger than 70 years old. Exclusion criteria was Kellgren-Lawrence classification grade 4; osteoarthritis of the medial femorotibial joint; infection; inflammatory disease such as rheumatoid arthritis; symptomatic patellofemoral osteoarthritis; and osteotomy below the tibial tubercle. Past histories included medial meniscus resection in 2 knees, and tibial fracture in one knee. Horizontal tear of the medial meniscus was observed in 31 knees of which partial resection was performed in 20. Autologous osteochondral transplantation at the medial femoral condyle was performed in 4 knees. During this period, one patient with osteotomy below the tibial tubercle was excluded. The social profiles of the patients were unknown.
2.2. Surgical procedure and planning for hardware removal
Medial open-wedge osteotomy was performed 35 mm below medial tibial plateau. We decided the correction angle according to the method reported by Miniaci et al.[7] Each patient was placed in the supine position. Knee arthroscopy was performed before osteotomy. An oblique surgical incision was made on the superomedial side of the tibia, and a medial locking compression plate (TomoFix, Synthes, Solothurn, Switzerland)[8] was used after bi-plane osteotomy.[9] Osteotomy was performed proximal to the tibial tuberosity. To achieve suitable realignment of the lower limb resulting in valgus correction, the target mechanical axis was 62.5% from the medial edge of the tibial plateau to its entire length (Fujisawa point).[10] The osteotomy gap in all patients was augmented with beta-tricalcium phosphate (Osferion; Olympus, Tokyo, Japan).
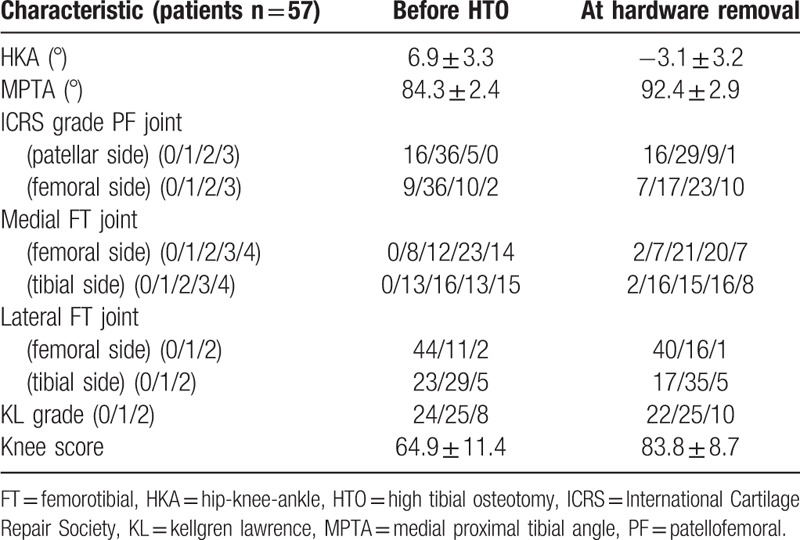
Partial weight bearing was permitted the day after surgery, and full weight bearing was permitted 3 weeks after surgery. Patients generally underwent plate removal and second-look arthroscopy an average 20.5 ± 8.8 months after medial open-wedge HTO (Table 1).
Table 1.
Pre- and intra-operative patient characteristics.
2.3. Clinical outcomes and radiological evaluations
Patients were evaluated clinically by determining their American Knee Society Scores before medial open-wedge HTO and after implant removal. The hip-knee-ankle (HKA) angle and the medial proximal tibial angle (MPTA) were measured by long-leg full-weight-bearing radiograph to assess the severity of varus deformity and the degree of postoperative valgus correction (Fig. 1). Change in HKA and MPTA from pre- to post-surgery were designated ΔHKA and ΔMPTA, respectively. The occurrence of patellar tracking defects was assessed radiographically by measuring lateral tilt and congruence angles on images of the flexed patellar axis. Patellar height was determined by measuring the Insall-Salvati ratio and the Blackburne Peel ratio.[11] Patellofemoral osteoarthritis was evaluated using Kellgren and Lawrence grading. Radiographic evaluations were measured twice by the same observer at different times to determine intraobserver reliability, and blindly and independently by two different observers (EO and SN) to determine interobserver reliability.
Figure 1.
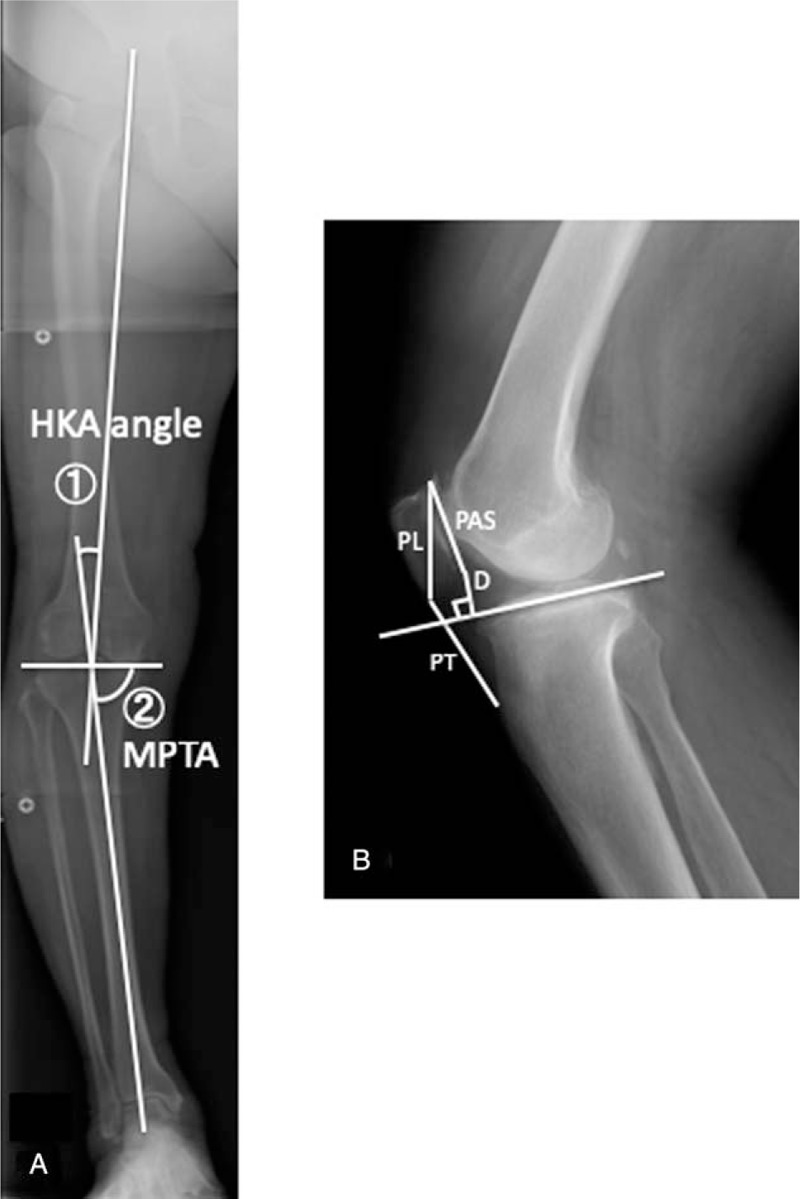
(A) Method for measurement of hip-knee-ankle angle (HKA) and medial proximal tibial angle (MPTA). (B) Method for measurement of the Insall-Salvati ratio (PT/PL) and Blackburne-Peel ratio (D/PAS). D = shortest distance between the most distal region of the patella and the line tangent to the articular surface of the tibial plateau. PAS = length of the articular surface of the patella, PL = longest longitudinal length of the patella, PT = length of the patellar tendon.
2.4. Evaluation of osteoarthritis of the patellofemoral joint
The condition of the patellofemoral articular cartilage was assessed by two-stage arthroscopy, performed before and after medial open-wedge HTO, and the presence of chondral lesions was determined for the patella and femoral trochlea. International Cartilage Repair Society (ICRS) grades were determined by arthroscopy before and after medial open-wedge HTO.[12] The second-look arthroscopy findings were compared with the first-look arthroscopy findings. Worsening of the patellar and/or femoral trochlear cartilage (evaluated by ICRS grading) was regarded as degeneration group (D group), whereas no change or improvement was regarded as non-degeneration (ND group). Three orthopedic surgeons (EO, SN, and YA) evaluated the arthroscopic findings independently, and ICRS grades were decided by agreement among 2 or more surgeons. Patients’ demographic and clinical characteristics and degree of valgus correction were compared between D and ND groups.
2.5. Statistical analysis
Data were expressed as means ± SD and analyzed using EZR (Saitama Medical Center, Jichi Medical University), a graphical user interface for R (The R Foundation for Statistical Computing, version 2.13.0). Significant differences between the D and ND groups in demographic characteristics, clinical scores, and radiographically measured parameters were analyzed using Student's t test, and differences in ICRS grade of the patellofemoral joint were analyzed using the Chi-square test. Receiver operating characteristic (ROC) curves were analyzed to determine ΔMPTA cut-off values and calculate sensitivity, specificity, and area under curve (AUC). In all analyses, P < .05 was defined as statistically significant. For comparison of ΔMPTA between the D and ND groups, a total of 38 patients were required to show a significant difference at an α level of 0.05 and a β level of 80%. Interclass correlation coefficients (ICCs) were calculated with a two-way random model using SPSS (version 21.0 for Windows; IBM, Chicago, IL).
3. Results
3.1. Clinical outcomes
At the time of medial open-wedge HTO, mean patient age was 54.1 ± 9.9 years, mean height was 160.4 ± 8.7 cm, mean body weight was 66.4 ± 12.1 kg, and mean body mass index was 25.7 ± 3.3 kg/m2. The mean knee score before surgery was 64.9 ± 11.4, improving to 83.8 ± 8.7 after surgery. No patient developed any complications, including infection or false joint. The average opening width of the medial side of the tibia was 11.3 ± 2.7 mm (range, 7–16 mm). Anterior knee pain was present in 2 knees (4%) after medial open-wedge HTO.
3.2. Radiological measurements
The mean HKA changed from 6.9 ± 3.3° before surgery to −3.1 ± 3.2° after surgery, and the mean MPTA changed from 84.3 ± 2.4° before surgery to 92.4 ± 2.9° after surgery.
3.3. Comparison of patients’ demographic data and clinical outcomes among patients with and without progression of patellofemoral osteoarthritis
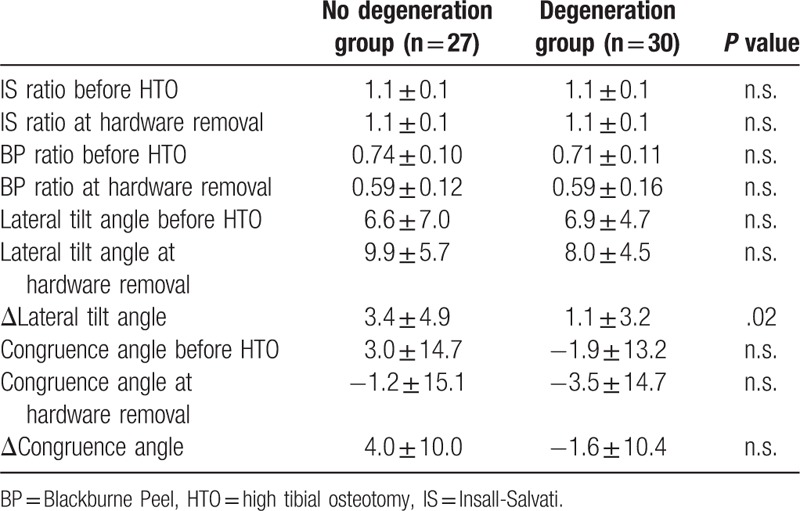
The ND and D groups comprised 27 and 30 knees, respectively. The two groups did not differ significantly in age at initial surgery, sex distribution, body mass index, time to hardware removal, or knee score at medial open-wedge HTO and hardware removal (Table 2). The ND and D groups differed significantly in HKA (5.7 ± 2.8° vs. 8.0 ± 3.4°) and MPTA (85.1 ± 2.1° vs. 83.6 ± 2.4°) at the time of medial open-wedge HTO (Table 3), but not at the time of hardware removal. ΔHKA and ΔMPTA, representing change in HKA and MPTA, respectively, differed significantly between the two groups, P < .05. There was no significance between group difference in Kellgren-Laurence grade of the patellofemoral joint on both the patellar and femoral sides at the time of medial open-wedge HTO, nor in the height and shift of the patella (Table 4). Δlateral tilt angle, representing the change of lateral tilt angle, differed significantly between groups, P < .05.
Table 2.
Baseline demographic and clinical characteristics.
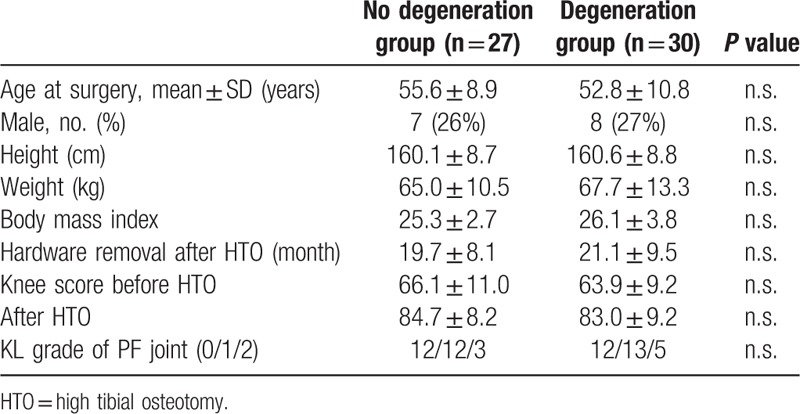
Table 3.
Knee alignment, cartilage degeneration, and clinical scores of patients in the degeneration and non-degeneration groups.
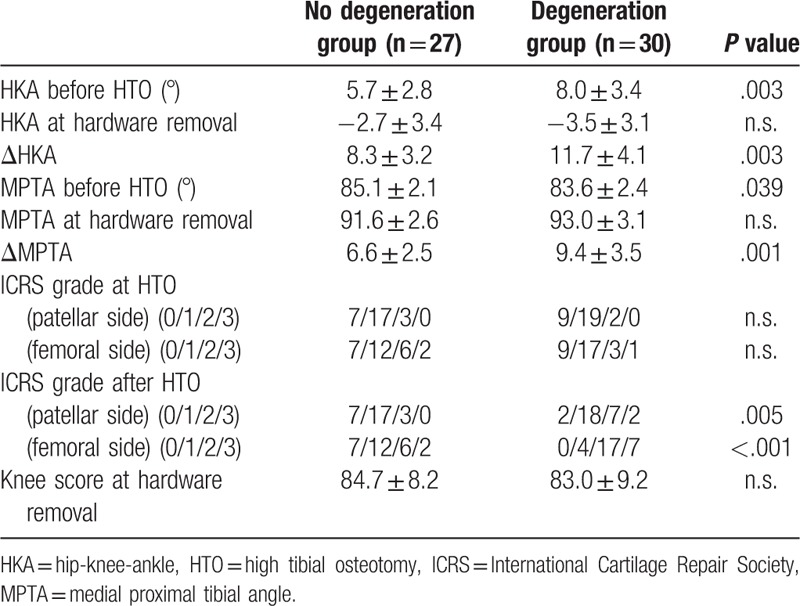
Table 4.
Patellar alignment in the degeneration and non-degeneration groups.
ROC curves were constructed to show the relationship between true positives and false positives, using ΔMPTA to predict patellofemoral degeneration. The ΔMPTA cut-off values were determined to be 10°, associated with an AUC of 0.75 (95% confidence interval [CI] 0.62–0.87) (Fig. 2). The sensitivity and specificity were 56.7% and 88.9%, respectively.
Figure 2.
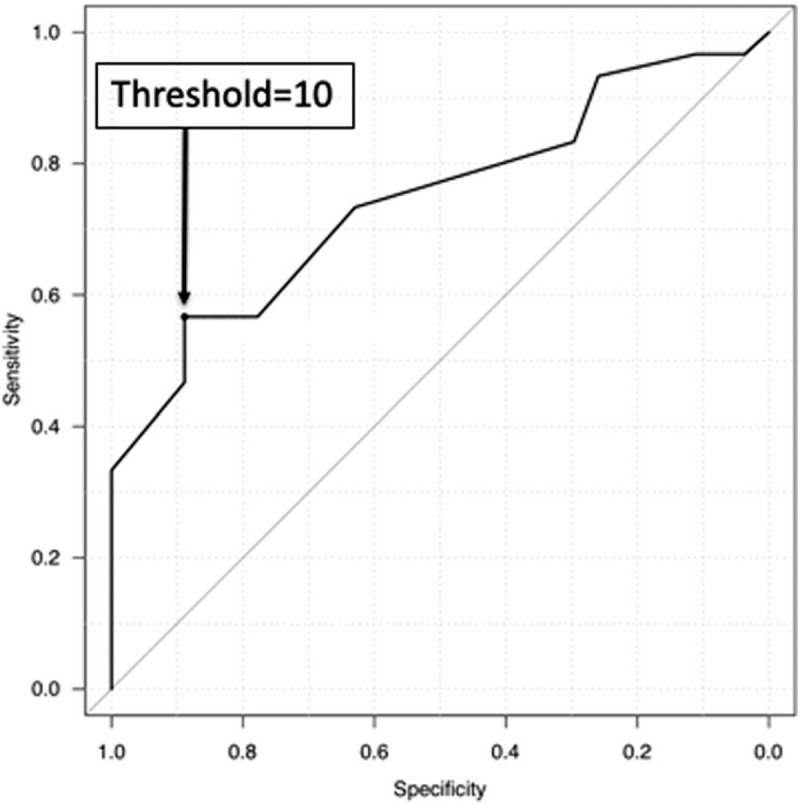
Receiver operating characteristic (ROC) curve of ΔMPTA.
4. Discussion
Our data showed a relationship between the degree of deformity correction and progressive degeneration of patellofemoral joint cartilage after medial open-wedge HTO (Fig. 3).
Figure 3.

Representative patient of D group (48-year-old woman). (A) Arthroscopic findings at HTO showed slight fibrillation of patellofemoral cartilage (ICRS grade 1). (B) At hardware removal, osteoarthritis of patellofemoral cartilage was worse (ICRS grade 3). HTO = high tibial osteotomy, ICRS = International Cartilage Repair Society.
Medial open-wedge HTO is a joint-conserving treatment generally performed for medial knee osteoarthritis.[13] This procedure, during which an osteotomy for the opening is applied proximal to the tibial tuberosity, has generally yielded favorable clinical outcomes, with postoperative lower limb alignment on the coronal plane considered important. We found that, when the target correction angle was set at a mechanical axis deviation of 62.5% as recommended,[10] the mean HKA changed from 6.9° before surgery to −3.1° after surgery, and the knee score improved significantly. Because a mechanical axis deviation of 62.5% is reported to correspond to 3.1° valgus,[14] the target alignment on the coronal plane was achieved, confirming medial open-wedge HTO in our patient population resulted in favorable clinical outcomes.
Negative effects of medial open-wedge HTO on the patellofemoral joint are regarded as complications of surgery.[2] A cadaveric study reported that medial open-wedge HTO significantly increased pressure on the patellofemoral cartilage at 30°, 60°, and 90° flexion.[15] Moreover, medial open-wedge HTO was found to significantly aggravate degeneration of the patellofemoral joint cartilage.[5] In the present study, degeneration of the patellofemoral joint cartilage progressed similarly in 30 of the 57 knees that underwent medial open-wedge HTO. Degeneration, however, did not progress in 27 knees, indicating that effects of medial open-wedge HTO on the patellofemoral joint vary.
To identify factors that may cause this variation in effect on the patellofemoral joint, preoperative, intraoperative, and postoperative factors were compared between our ND group, in which cartilage properties did not change after surgery, and the D group, in which cartilage degeneration progressed. The two groups did not differ significantly in baseline demographic characteristics, clinical scores before and after surgery, severity of patellofemoral joint degeneration at the time of medial open-wedge HTO, and time to hardware removal. In contrast, ΔHKA and ΔMPTA differed significantly among these two groups, thereby demonstrating an association between the degree of deformity correction and patellofemoral joint degeneration after medial open-wedge HTO. ROC analysis showed that the cut-off value of patellofemoral joint degeneration was ΔMPTA = 10°. Therefore, a greater degree of deformity correction during medial open-wedge HTO may increase the risk of postoperative patellofemoral joint degeneration.
On the other hand, regarding the clinical symptoms with the progression of osteoarthritis in patellofemoral joint after open-wedge HTO, it has been reported that progress of osteoarthritis of the patellofemoral joint does not affect HTO performance in mid-term grades.[16] Likewise, in the present study no significant difference was observed in clinical scores between the two groups at about 2 years post-surgery. Patellofemoral osteoarthritis worsened in about half of the patients, so long-term follow-up in these patients is necessary.
Patella baja is a mechanism that affects the degree of deformity correction on the patellofemoral joint resulting from medial open-wedge HTO. The Blackburne-Peel ratio, a measure of patellar height, is reduced significantly by medial open-wedge HTO.[17] In this study, the Blackburne-Peel ratio decreased significantly after surgery, but its mean value in both the ND and D groups was 0.59, higher than the criterion for a patella baja, and did not differ significantly between these two groups. These findings indicate that postoperative patellar height was not associated with degeneration of the patellofemoral joint cartilage.
In contrast, a cadaveric study reported that the difference in the medial open-wedge HTO-associated correction angle changed the kinematics of the patellofemoral joint.[4] In this study, Δlateral tilt angle was significantly different between the ND group and D group in the evaluation of patellofemoral joint compatibility. Taken together with our findings, these results indicate that an increase in the angle opened by medial open-wedge HTO may have influenced the cartilage by changing the kinematics of the patellofemoral joint.
This study had several limitations. One limitation was that it was a retrospective design. Another limitation was the absence of a significant difference in clinical outcomes between the two groups. Because repeat arthroscopy to evaluate postoperative degeneration of the patellofemoral joint cartilage was performed within a relatively short period of time after medial open-wedge HTO, long-term follow-up may be necessary.
5. Conclusion
This study evaluated retrospectively the effect of the correction angle during medial open-wedge HTO on patellofemoral joint degeneration. If deformity correction exceeds an MPTA of 10° during open-wedge HTO, degeneration of patellofemoral joint needs to be considered.
Author contributions
Conceptualization: Keiichiro Ueshima.
Data curation: Shuji Nakagawa, Yusuke Nakayama.
Formal analysis: Hiroyuki Kan, Yuta Fujii.
Investigation: Yuji Arai.
Methodology: Kazuya Ikoma.
Supervision: Toshikazu Kubo.
Validation: Hiroaki Inoue.
Writing – original draft: Eigo Otakara.
Writing – review & editing: Hiroyoshi Fujiwara.
Footnotes
Abbreviations: AUC = area under curve, HKA = hip-knee-ankle, HTO = high tibial osteotomy, ICRS = International Cartilage Repair Society, MPTA = medial proximal tibial angle, ROC = receiver operation characteristic.
Funding: There were no funding resources.
The authors declare there are no conflicts of interest.
References
- [1].Floerkemeier S, Staubli AE, Schroeter S, et al. Outcome after high tibial open-wedge osteotomy: a retrospective evaluation of 533 patients. Knee Surg Sports Traumatol Arthrosc 2013;21:170–80. [DOI] [PubMed] [Google Scholar]
- [2].Goshima K, Sawaguchi T, Sakagoshi D, et al. Age does not affect the clinical and radiological outcomes after open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 2017;25:918–23. [DOI] [PubMed] [Google Scholar]
- [3].Jung WH, Chun CW, Lee JH, et al. Comparative study of medial opening-wedge high tibial osteotomy using 2 different implants. Arthroscopy 2013;29:1063–71. [DOI] [PubMed] [Google Scholar]
- [4].Gaasbeek R, Welsing R, Barink M, et al. The influence of open and closed high tibial osteotomy on dynamic patellar tracking: a biomechanical study. Knee Surg Sports Traumatol Arthrosc 2007;15:978–84. [DOI] [PubMed] [Google Scholar]
- [5].Kim KI, Kim DK, Song SJ, et al. Medial open-wedge high tibial osteotomy may adversely affect the patellofemoral joint. Arthroscopy 2017;33:811–6. [DOI] [PubMed] [Google Scholar]
- [6].Javidan P, Adamson GJ, Miller JR, et al. The effect of medial opening wedge proximal tibial osteotomy on patellofemoral contact. Am J Sports Med 2013;41:80–6. [DOI] [PubMed] [Google Scholar]
- [7].Miniaci A, Ballmer FT, Ballmer PM, et al. Proximal tibial osteotomy. A new fixation device. Clin Orthop Relat Res 1989;246:250–9. [PubMed] [Google Scholar]
- [8].Dexel J, Fritzsche H, Beyer F, et al. Open-wedge high tibial osteotomy: incidence of lateral cortex fractures and influence of fixation device on osteotomy healing. Knee Surg Sports Traumatol Arthrosc 2017;25:832–7. [DOI] [PubMed] [Google Scholar]
- [9].Lobenhoffer P, Agneskirchner JD. Improvements in surgical technique of valgus high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 2003;11:132–8. [DOI] [PubMed] [Google Scholar]
- [10].Fujisawa Y, Masuhara K, Shiomi S. The effect of high tibial osteotomy on osteoarthritis of the knee. An arthroscopic study of 54 knee joints. Orthop Clin North Am 1979;10:585–608. [PubMed] [Google Scholar]
- [11].Insall J, Salvati E. Patella position in the normal knee joint. Radiology 1971;101:101–4. [DOI] [PubMed] [Google Scholar]
- [12].Mainil-Varlet P, Aigner T, Brittberg M, et al. Histological assessment of cartilage repair: a report by the Histology Endpoint Committee of the International Cartilage Repair Society (ICRS). J Bone Joint Surg Am 2003;85suppl 2:45–57. [PubMed] [Google Scholar]
- [13].Amendola A, Bonasia DE. Results of high tibial osteotomy: review of the literature. Int Orthop 2010;34:155–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].van de Pol GJ, Verdonschot N, van Kampen A. The value of the intra-operative clinical mechanical axis measurement in open-wedge valgus high tibial osteotomies. Knee 2012;19:933–8. [DOI] [PubMed] [Google Scholar]
- [15].Stoffel K, Willers C, Korshid O, et al. Patellofemoral contact pressure following high tibial osteotomy: a cadaveric study. Knee Surg Sports Traumatol Arthrosc 2007;15:1094–100. [DOI] [PubMed] [Google Scholar]
- [16].Goshima K, Sawaguchi T, Shigemoto K, et al. Patellofemoral osteoarthritis progression and alignment changes after open-wedge high tibial osteotomy do not affect clinical outcomes at mid-term follow-up. Arthroscopy 2017;33:1832–9. [DOI] [PubMed] [Google Scholar]
- [17].Wright JM, Heavrin B, Begg M, et al. Observations on patellar height following opening wedge proximal tibial osteotomy. Am J Knee Surg 2001;14:163–73. [PubMed] [Google Scholar]


