Abstract
Rationale:
Adequate stability of traumatic anterior shoulder dislocation without any obvious damage to the anterior capsulolabral structure in elderly patients can be achieved by treating the associated rotator cuff injuries. However, in case of recurrent shoulder dislocation despite rotator cuff repair, the repaired rotator cuff may be weakened or reruptured and is often impossible to repair again. Therefore, the role of the rotator cuff as a shoulder stabilizer cannot be expected. Even if the anterior joint capsule is left, it is too weak to imbrication either. An additional anterior structural reconstruction that can replace the rotator cuff and capsule is needed to prevent recurrence.
Patient concerns:
A 59-year-old man visited our clinic because of traumatic anterior dislocation of the right shoulder combined with anterior–superior rotator cuff tear. Because there was no obvious anterior capsulolabral injury, he underwent arthroscopic rotator cuff repair only. Postoperative rehabilitation was maintained; however, anterior shoulder dislocation recurred 10 months postoperatively.
Diagnosis:
Physical examination revealed anterior instability in abduction and external rotation of the shoulder joint. Magnetic resonance imaging suggested retear of the repaired anterior–superior rotator cuff and Hill–Sachs lesion of the humeral head.
Interventions:
Diagnostic arthroscopy was performed. The reruptured rotator cuff seemed impossible to repair; thus, arthroscopic remplissage procedure was performed for engaging the Hill–Sachs lesion. In addition, open pectoralis major tendon transfer for anterior stabilization was performed via the deltopectoral approach.
Outcomes:
At the 12-month follow-up, the patient showed good clinical outcomes, including internal rotation of the shoulder joint without recurrent instability.
Lesson:
Recurrent anterior shoulder dislocation after primary surgery in the elderly may be a challenging situation for surgeons. In patients with irreparable anterior rotator cuff tear and for whom reconstruction of the anterior glenoid is not indicated, pectoralis major tendon transfer is a good treatment option for satisfactory clinical outcomes without recurrence.
Keywords: elderly, pectoralis muscles, rotator cuff tears, shoulder dislocation, tendon transfer
1. Introduction
The shoulder joint is the most commonly dislocated joint in the body. Although Rowe[1] reported that the incidence of traumatic anterior shoulder dislocation was not different between individuals older and younger than 45 years, the prevalence of traumatic anterior shoulder dislocation in the elderly has increased recently because of lifestyle changes and prolonged life expectancy.
Anterior shoulder dislocation has been well known to occur because of anterior capsulolabral complex injury, whereas concomitant rotator cuff tear is more common in elderly patients than in younger patients due to tissue elasticity degeneration.[2,3] Although the recurrence rate after traumatic shoulder dislocation associated with anterior capsulolabral lesions is relatively lower in elderly patients, the complications related with rotator cuff tear are more likely to occur, and the clinical outcomes and prognosis in elderly patients are different from those in younger patients.[4,5]
Therefore treatment strategy of shoulder dislocation in elderly patients should consider these rotator cuff injury–related factors. However, the management consensus in elderly patients after traumatic shoulder dislocation is still less clearly defined. Furthermore, recurrent dislocation after primary stabilization surgery in elderly patients is more difficult and challenging to shoulder surgeons. We present a case of successful treatment with pectoralis major tendon transfer for a recurrent anterior shoulder dislocation combined with irreparable rotator cuff tear after arthroscopic rotator cuff repair for primary traumatic anterior shoulder dislocation in an elderly patient.
2. Case description
This case report was approved by the Institutional Review Board of Soonchunhyang University Hospital, and the patient provided written informed consent for publication of this case report and accompanying images. A 59-year-old man visited our outpatient department because of anterior dislocation of the right shoulder. Two weeks prior, he experienced direct trauma to the right shoulder when he fell off the car and underwent manual reduction of anterior dislocation of the right shoulder at another hospital. He complained of persistent pain and limitation of shoulder motion after trauma. Physical examination revealed nearly zero degree of active forward flexion and abduction of the arm, and decreased skin sensation in the deltoid area. We found no wound and no disturbance of blood circulation. On plain radiography, the humeral head was well reduced into the normal glenohumeral joint without definite osteoarthritic changes. Magnetic resonance imaging (MRI) revealed a complete retracted tear of the supraspinatus tendon and subscapularis tendon without muscle fatty degeneration (Fig. 1A, B). Mild Hill–Sachs lesion was observed,[6] but no Bankart lesion was suspected. Electromyography testing showed incomplete injury of the axillary and suprascapular nerves. He underwent arthroscopic surgery. On diagnostic arthroscopy, no definite anterior glenolabral lesion and engaging Hill–Sachs lesion were observed. Torn supraspinatus tendon and subscapularis tendon were repaired with bioabsorbable suture anchors (Healix suture anchor, DePuy Mitek, Raynham, MA) by using a single-row technique. Postoperatively, he maintained shoulder immobilization sling with an abduction pillow for 6 weeks, followed by passive range of motion (ROM) exercise and active ROM exercise progressively. At 10 weeks postoperatively, he demonstrated full active forward flexion and internal rotation and recovery of sensory deficit. However, he exhibited recurrent dislocation during shoulder stretch 3 months postoperatively and underwent manual reduction. After 3 weeks of additional immobilization, he restarted physical therapy with muscle strengthening. Thereafter, he restored active ROM gradually, including external rotation and abduction. At 10 months postoperatively, he visited our clinic with redislocation during abduction and external rotation of the shoulder. He underwent manual reduction at another hospital before revisitation. On plain radiography, the humeral head was reduced into the joint, and physical examination revealed no disturbance of blood circulation and no neurological abnormality. MRI revealed retear of the repaired supraspinatus tendon and subscapularis tendon with medial retraction (Fig. 2A, B). Posterosuperior bony defect of the humeral head was observed, but definite bony Bankart lesion was not suspected. Revision surgery was planned. On diagnostic arthroscopy, previous repaired rotator cuff was ruptured with cutting of suture materials and was severely retracted and scarred. Reruptured rotator cuff was impossible to repair because of atrophy. Engaging Hill–Sachs lesion was observed (Fig. 3). No definite anterior labral tear and bony defect of the glenoid were observed, but the capsule was too thin and too weak for capsulolabral repair to be performed. Remplissage procedure using all suture anchors (Q–fix suture anchor, Smith & Nephew, Austin, TX) for engaging Hill-Sachs lesion was only performed with arthroscopy. After completion of the arthroscopic procedure, the patient position was changed to beach-chair position from lateral decubitus, and standard deltopectoral skin incision was made. Anterior structures, including the lesser tuberosity, were exposed. The capsule was weak and stretched, and the subscapularis tendon was torn and retracted with atrophy (Fig. 4). For the tendon transfer, blunt dissection was performed between the sternocostal head and clavicular head of the pectoralis major muscle, and the sternocostal head was sharply elevated at the humeral insertion site. The elevated sternocostal head of the pectoralis major muscle was transferred superior to the musculocutaneous nerve and deep to the conjoined tendon. The transferred pectoralis major tendon was securely fixed to the lesser tuberosity with suture anchors (Q–fix suture anchor, Smith & Nephew) (Fig. 5A, B). The patient maintained a shoulder immobilization sling with an abduction pillow for 6 weeks postoperatively, and pendulum exercise and passive forward flexion and internal rotation ROM exercise were allowed after 2 weeks postoperatively. After 6 weeks postoperatively, the sling was removed, and gentle active ROM exercise was started. At 3 months postoperatively, muscle strengthening exercise was started. At 1-year follow–up, the patient demonstrated full ROM, including internal rotation (Fig. 6A, B, C). He had no limitation of daily activity. He revealed negative results on belly press and lift-off tests. We found no instability during abduction and external rotation.
Figure 1.
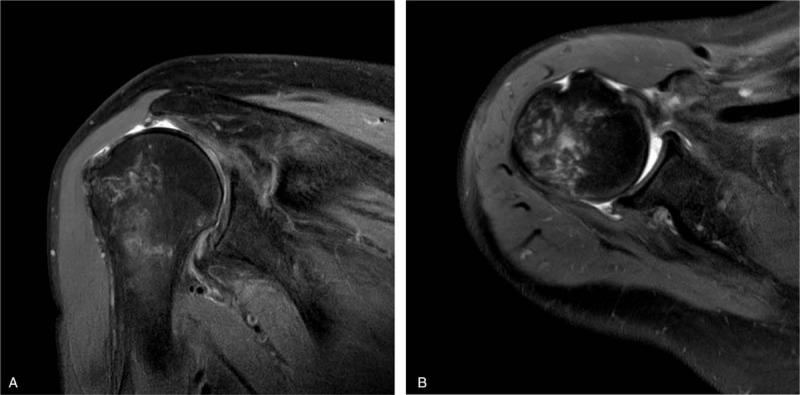
A coronal plane T2-weighted magnetic resonance image (MRI) (A) and an axial plane T2-weighted image (B) exhibiting complete, retracted tear of the supraspinatus tendon and subscapularis tendon without muscle fatty degeneration.
Figure 2.
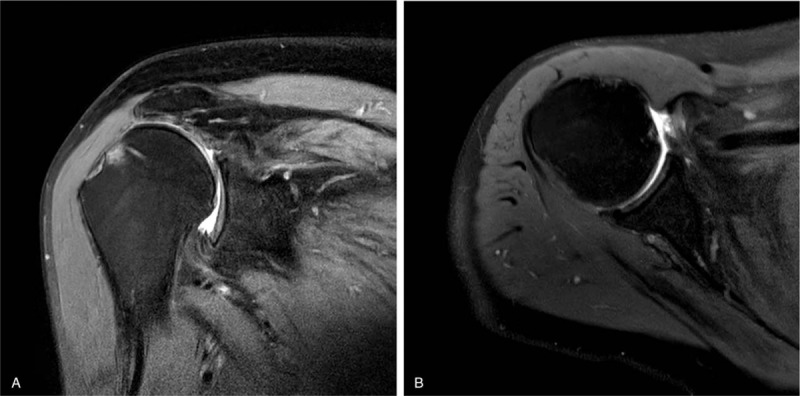
A coronal plane T2-weighted magnetic resonance image (MRI) (A) and an axial plane T2-weighted image (B) exhibiting retear of the supraspinatus tendon and subscapularis tendon with severe medial retraction.
Figure 3.
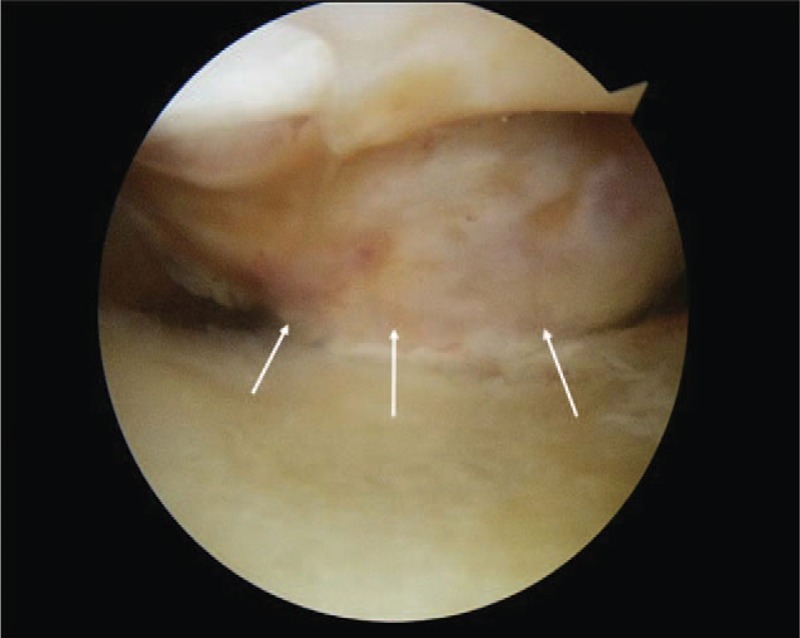
Arthroscopic finding exhibiting engaging Hill–Sachs lesion (arrows).
Figure 4.
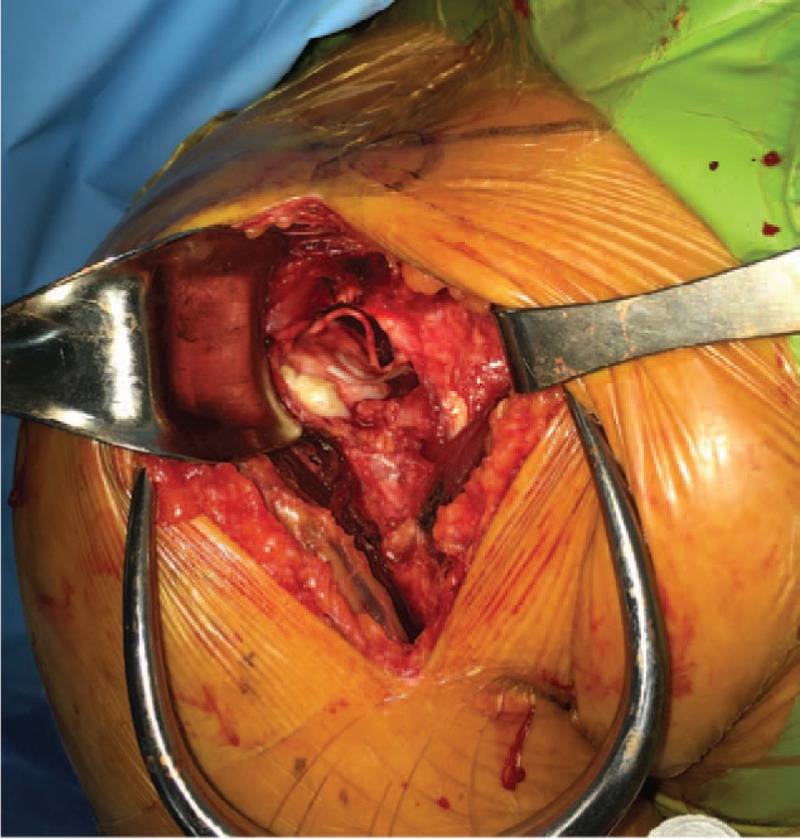
The capsule was weak and stretched, and the subscapularis tendon was torn and retracted with atrophy. Cut suture materials are observed.
Figure 5.
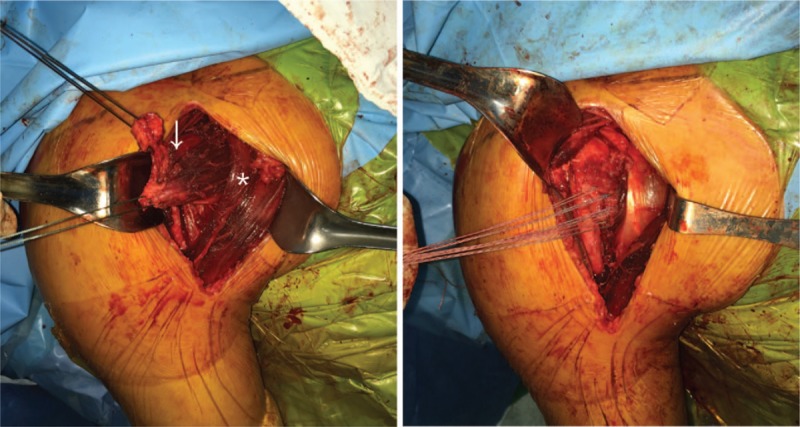
A, The sternocostal head of the pectoralis major muscle (arrow) is transferred deep to the conjoined tendon (asterisk) via deltopectoral approach. B, The transferred tendon is securely fixed to the lesser tuberosity with suture anchors.
Figure 6.

The patient demonstrated full range of forward flexion (A), internal rotation (B), and external rotation (C).
3. Discussion
It is certain that successful stabilization and functional recovery can be expected by nonsurgical treatment of primary traumatic anterior shoulder dislocation without concomitant injury in elderly patients. However, concomitant rotator cuff injury more commonly occurs in elderly patients. Surgical treatment should be required if there is a possibility of complication or recurrent dislocation. Therefore, considering the age, activity level, characteristics of rotator cuff tear, presence of anterior capsulolabral lesion, and number of dislocation are important for determining treatment modalities of shoulder dislocation in elderly patients. The choice of treatment should be more careful, particularly in the case of recurrent dislocation after primary stabilization surgery.
The relationship between shoulder dislocation and rotator cuff tear is unclear whether anterior shoulder dislocation may cause rupture of weakened rotator cuff (“anterior mechanism”), or weakened rotator cuff does not act properly as a posterior stabilizer, inducing movement imbalances (“posterior mechanism”).[7,8] The rotator cuff acts as a force couple by itself and is an important stabilizing structure of the glenohumeral joint. In addition, the subscapularis tendon acts in part as an anterior buttress.[9] Some studies have reported that rotator cuff repair alone can achieve satisfactory clinical outcomes without recurrence in isolated rotator cuff tears, and even with anterior capsulolabral lesion, if there is a rotator cuff tear more than a large size, rotator cuff repair alone can achieve sufficient stabilization.[10–12]
In this patient, there was no obvious damage to the anterior capsulolabral complex, and rotator cuff repair was performed for massive sized anterior–superior rotator cuff tear. However, at 10 months postoperatively, massive sized retear of the rotator cuff with recurrent dislocation occurred. The definite soft tissue and bony Bankart lesion were not observed during this time. Neviaser and Neviaser[13] reported that recurrent anterior shoulder dislocation after the age of 40 years can be caused by rupture of rotator cuff tendon and shoulder capsule without any labral lesion, and repair of these torn structures may restore stability and motion. However, in this patient, the reruptured rotator cuffs and anterior capsule were considered irreparable due to severe retraction and muscle degeneration. Hill–Sachs lesion was observed in preoperative MRI, and the infraspinatus tendon was maintained. Arthroscopic remplissage procedure was considered for posterior stabilization. Subsequently, determining the treatment modality for anterior stabilization is important. Remplissage procedure alone could not achieve anterior stability of the glenohumeral joint. Our patient was not indicated for bony reconstruction surgery, such as Latarjet procedure, because of no anterior glenoid bone loss. Without subscapularis tendon, the force couple function of the rotator cuff cannot be expected. In addition, anterior–superior escape of the humeral head may occur in patients with chronic subscapularis muscle insufficiency because of the absence of anterior restraint.[14]
Management of irreparable subscapularis tendon may include the use of dermal allograft or tendon transfer. Pectoralis major tendon transfer is the most commonly used surgical procedure for massive anterior–superior rotator cuff tear or isolated irreparable subscapularis tear.[15,16] Pectoralis major tendon transfer was reported to be effective as an anterior stabilizer in recurrent anterior shoulder dislocation associated with an irreparable subscapularis tears, which is similar to this case.[17] Pectoralis major tendon transfer can effectively replace the function of the anterior buttress and subscapularis tendon when transferred deep to the conjoined tendon. Therefore, tendon transfer may reduce abnormal wear of the glenohumeral joint and also reduce the risk of early arthritis.
At 1 year postoperatively, the patient showed good clinical outcome without recurrent instability, and internal rotation function of the shoulder joint revealed satisfactory result. For patients with recurrent instability after primary rotator cuff repair, pectoralis major tendon transfer is one of the good option for anterior stabilization. It can prevent further recurrence and complications associated with torn subscapularis and stretched capsule.
4. Conclusions
The treatment plan of elderly patients with recurrent dislocation and anterior–superior massive rotator cuff tear should be based on several factors such as age, activity level, and characteristics of combined injuries. Recurrent dislocation without glenoid bone loss or anterior labral injury is not an indication of Latarjet procedure or Bankart repair. However, posterior stabilization alone is insufficient to obtain normal stability and movement of the glenohumeral joint because of the function of subscapularis tendon and capsule as an anterior restraint is absent. In these patients, pectoralis major tendon transfer may help restore shoulder mechanics and also provide good clinical outcomes without recurrence of dislocation.
Acknowledgments
The authors would like to thank the Soonchunhyang University Research Fund for support.
Author contributions
Conceptualization: Jun Bum Kim, Sijohn Hong, Chang Hyun Kim.
Data curation: Jun Bum Kim, Soon Do Wang, Chang Hyun Kim.
Investigation: Soon Do Wang.
Project administration: Jun Bum Kim.
Supervision: Jun Bum Kim, Sijohn Hong.
Writing – original draft: Chang Hyun Kim.
Writing – review and editing: Jun Bum Kim, Sijohn Hong, Soon Do Wang, Chang Hyun Kim.
Chang Hyun Kim orcid: 0000-0002-2539-1058.
Footnotes
Abbreviations: MRI = magnetic resonance imaging, ROM = range of motion.
JBK and SJH contributed equally to this study.
No benefit in any form was received or will be received from a commercial party related directly or indirectly to the subject of this article.
The authors have no potential conflicts of interest to disclose.
References
- [1].Rowe CR. Prognosis in dislocations of the shoulder. J Bone Joint Surg Am 1956;38-A:957–77. [PubMed] [Google Scholar]
- [2].Gombera MM, Sekiya JK. Rotator cuff tear and glenohumeral instability: a systematic review. Clin Orthop Relat Res 2014;472:2448–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Loew M, Thomsen M, Rickert M, et al. Injury pattern in shoulder dislocation in the elderly patient [in German]. Unfallchirurg 2001;104:115–8. [DOI] [PubMed] [Google Scholar]
- [4].Antonio GE, Griffith JF, Yu AB, et al. First-time shoulder dislocation: high prevalence of labral injury and age-related differences revealed by MR arthrography. J Magn Reson Imaging 2007;26:983–91. [DOI] [PubMed] [Google Scholar]
- [5].Maier M, Geiger EV, Ilius C, et al. Midterm results after operatively stabilised shoulder dislocations in elderly patients. Int Orthop 2009;33:719–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Rowe CR, Zarins B, Ciullo JV. Recurrent anterior dislocation of the shoulder after surgical repair. Apparent causes of failure and treatment. J Bone Joint Surg Am 1984;66:159–68. [PubMed] [Google Scholar]
- [7].Loehr JF, Helmig P, Sojbjerg JO, et al. Shoulder instability caused by rotator cuff lesions. An in vitro study. Clin Orthop Relat Res 1994;84–90. [PubMed] [Google Scholar]
- [8].Porcellini G, Paladini P, Campi F, et al. Shoulder instability and related rotator cuff tears: arthroscopic findings and treatment in patients aged 40 to 60 years. Arthroscopy 2006;22:270–6. [DOI] [PubMed] [Google Scholar]
- [9].Hsu HC, Boardman ND, 3rd, Luo ZP, et al. Tendon-Defect and muscle-unloaded models for relating a rotator cuff tear to glenohumeral stability. J Orthop Res 2000;18:952–8. [DOI] [PubMed] [Google Scholar]
- [10].Shin SJ, Yun YH, Kim DJ, et al. Treatment of traumatic anterior shoulder dislocation in patients older than 60 years. Am J Sports Med 2012;40:822–7. [DOI] [PubMed] [Google Scholar]
- [11].Itoi E, Tabata S. Rotator cuff tears in anterior dislocation of the shoulder. Int Orthop 1992;16:240–4. [DOI] [PubMed] [Google Scholar]
- [12].Simank HG, Dauer G, Schneider S, et al. Incidence of rotator cuff tears in shoulder dislocations and results of therapy in older patients. Arch Orthop Trauma Surg 2006;126:235–40. [DOI] [PubMed] [Google Scholar]
- [13].Neviaser RJ, Neviaser TJ. Recurrent instability of the shoulder after age 40. J Shoulder Elbow Surg 1995;4:416–8. [DOI] [PubMed] [Google Scholar]
- [14].Li X, Cusano A, Eichinger J. Eden-Hybinette and pectoralis major transfer for recurrent shoulder instability due to failed Latarjet and chronic subscapularis rupture. Orthopedics 2017;40:e182–7. [DOI] [PubMed] [Google Scholar]
- [15].Elhassan B, Ozbaydar M, Massimini D, et al. Transfer of pectoralis major for the treatment of irreparable tears of subscapularis: does it work? J Bone Joint Surg Br 2008;90:1059–65. [DOI] [PubMed] [Google Scholar]
- [16].Nelson GN, Namdari S, Galatz L, et al. Pectoralis major tendon transfer for irreparable subscapularis tears. J Shoulder Elbow Surg 2014;23:909–18. [DOI] [PubMed] [Google Scholar]
- [17].Wirth MA, Rockwood CA., Jr Operative treatment of irreparable rupture of the subscapularis. J Bone Joint Surg Am 1997;79:722–31. [DOI] [PubMed] [Google Scholar]


