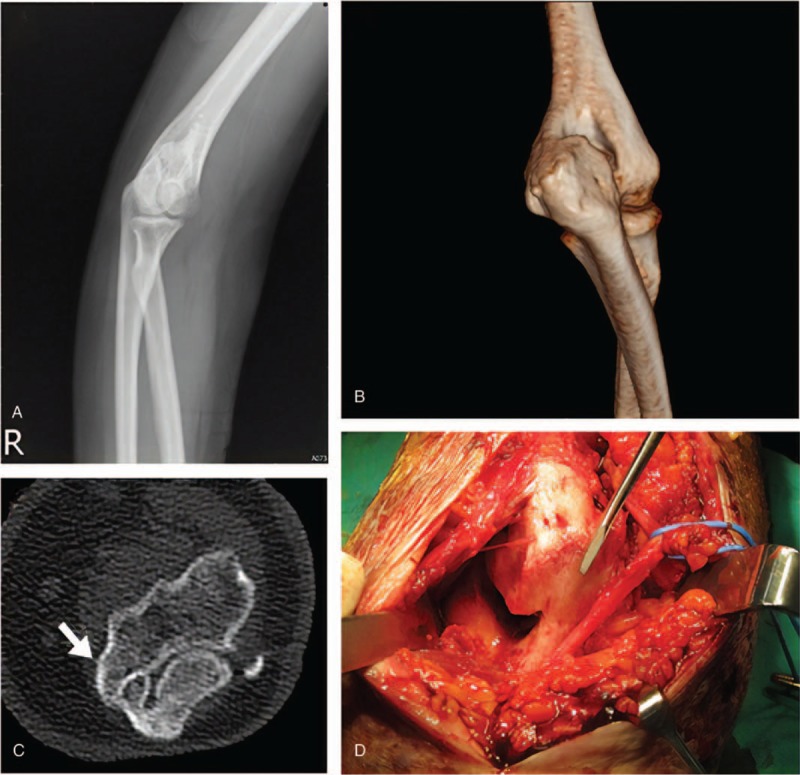
Abstract
Rationale:
Heterotopic ossification (HO), which is defined as the formation of new bone in tissues that do not normally ossify, is an infrequent yet debilitating complication of burns. Herein, we report three patients who suffered from elbow HO after burn injury due to a dust explosion event. This is a case report that includes the most cases involved in a single mass casualty incident in the presented literature.
Patient concerns:
Case 1: A 28-year-old man presented with second-to-third degree 88% total body surface area (TBSA) burns after the explosion event. He complained of decreased progressive bilateral elbow range of motion (ROM) for 1.5 months after the burn injury.
Case 2: A 28-year-old woman presented with second-to-third degree 50% TBSA burns and complained of decreased progressive bilateral elbow ROM with intolerable pain on elbow extension for 1 month after the burn injury.
Case 3: A 22-year-old man presented with second-to-third degree 90% TBSA burns and complained of significantly decreased left elbow ROM with intolerable pain 5 months after the burn injury.
Diagnosis:
The follow-up radiograph of the symptomatic elbow of these three patients revealed heterotopic ossification formation. Three-dimensional reconstruction computed tomography performed preoperatively showed that HO mainly affected the humeroulnar joint.
Interventions:
We treated all three patients with surgical elbow HO resection and ulnar nerve transposition, followed by immediate passive ROM exercise since postoperative day 1 and continuous physical therapy.
Outcomes:
In case 1, the documented ROM gain on the last follow-up (18.5 months after surgery) was 30° in the right elbow and 118° in the left elbow. In case 2, the follow-up time was 21 months and the documented ROM gain on the last follow-up was 120° in the right elbow and 90° in the left elbow. In case 3, the follow-up time was 20 months and the documented left elbow ROM gain on the last follow-up was 40°.
Lessons:
We discuss our experience of treating postburn HO and review the recent literature. The postburn HO treatment results of early surgical excision combined with immediate postoperative physical therapy were satisfactory.
Keywords: burns, dust, elbow, explosion, heterotopic ossification
1. Introduction
Heterotopic ossification (HO), which is defined as the formation of new bone in tissues that do not normally ossify,[1] is an infrequent yet debilitating complication of burns. The elbow is the most affected joint and has mostly adjacent or overlying burns, which cause functional impairment.[2] Although some studies have reported the use of conservative treatment of elbow HO,[3,4] surgical resection tends to be more effective and has a low recurrence rate.[2]
On July 27, 2015, an explosion occurred at approximately 8:30 PM after colored powder was sprayed over “Color Play Asia” party goers at the Formosa Fun Coast Water Park in New Taipei City, Taiwan. According to the statistical data from the Ministry of Health and Welfare of Taiwan, the dust explosion burned 499 people, including 248 patients with >40% total burn surface area (TBSA) injuries and 21 patients with >80% TBSA injuries. Fifteen people eventually died.[5] Initially, 56 patients were sent to our institution; 18 of these patients were admitted to the intensive care unit (ICU).
We present a case report involving three patients, all victims of the explosion event, who were diagnosed as having elbow HO formation several months after burn injury. Both elbows of the first and second patients and one elbow of the third patient were affected. Elbow range of motion (ROM) limitation and functional impairment were the main problems described by the patients, and none of the patients complained of ulnar nerve dysfunction symptoms preoperatively. We treated the patients with surgical HO resection and ulnar nerve transposition after we noted that the soft tissue condition was stable, followed by immediate postoperative physical therapy.
This is a case report that includes the most cases (3 patients with total of five elbow joints) involved in a single mass casualty incident in the presented literature. We hope that by providing our experience of treating the elbow HO patients in this event, more data would be available for establishing further systemic treatment protocol. We also reviewed the literatures concerning the diagnosis, treatment, and outcomes of surgical correction of HO in burn patients, with the goal of applying improved methods to our clinical practice (Table 1).
Table 1.
Details of the patients’ profiles.
2. Case 1
A previously healthy 28-year-old man presented with second-to-third degree 88% TBSA burns after the colored powder explosion event. His hospitalization course included initial resuscitation at the emergency department after 77 days in the burn ICU and 52 days of inpatient care. Extensive surgical debridement and skin grafting were performed nine times during this hospitalization course. The passive elbow ROM physical therapy was started on the second day of the ICU stay, and the active ROM training was started 1.5 months after the burn injury. He continued with outpatient rehabilitation, and the attending physiotherapist noted gradually increased stiffness over his bilateral elbow joints. Severe scar contracture over his left elbow was also noted. Follow-up radiographs obtained 8 months after the injury demonstrated persistent HO in both elbows. The range of flexion/extension ROM of the right and left elbowswas10°–60° and 120°–122°, respectively.
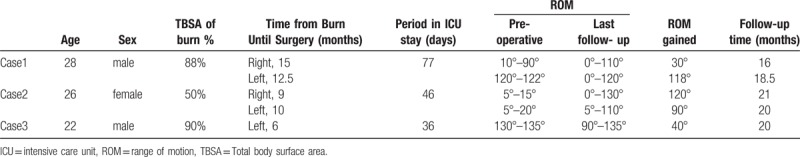
Left elbow scar contracture release and skin grafting were performed initially. After the skin around the elbow healed, we performed HO excision as completely as possible and checked the integrity of the medial/lateral collateral ligament over the bilateral elbows (surgical time,12.5 months postburn) (Fig. 1). The same surgical procedure was performed for right elbow 2.5 months later. The intraoperative ROM reached 0° to 130° bilaterally.
Figure 1.
A-B: Left elbow scar contracture release and skin grafting, C-D: heterotopic ossification excision through single posterior midline incision. We identified the released ulnar nerve and ensured that the lateral collateral ligament complex and the anterior band of the medial collateral ligament were intact.
The passive ROM exercise was started on postoperative day 1, followed by ROM exercises once the surgical stitches were removed. After discharge, the patient was asked to perform both ROM exercises and elbow stretching at least 30 minutes daily. Gentle passive rather than active ROM exercises were performed initially. The stretching was performed to reach the upper limit of elbow extension, as tolerable as possible. The outpatient clinic follow-up was arranged once every 2 weeks in the beginning to monitor the surgical wound healing and elbow ROM improvement. After 3 months of follow-up, the duration of clinic visit was changed to once per month. The postoperative ROMs documented in the last follow-up (16 months after right elbow surgery and 18.5 months after left elbow surgery) were 0° to 110° for the right elbow and 0° to 120° for the left elbow. The increase in ROM was 30° for the right elbow and 118° for the left elbow (Fig. 2) postoperatively.
Figure 2.

The pictures show that the range of motion of the patient's left elbow could reach near full extension to 120° flexion 16 months after surgery.
3. Case 2
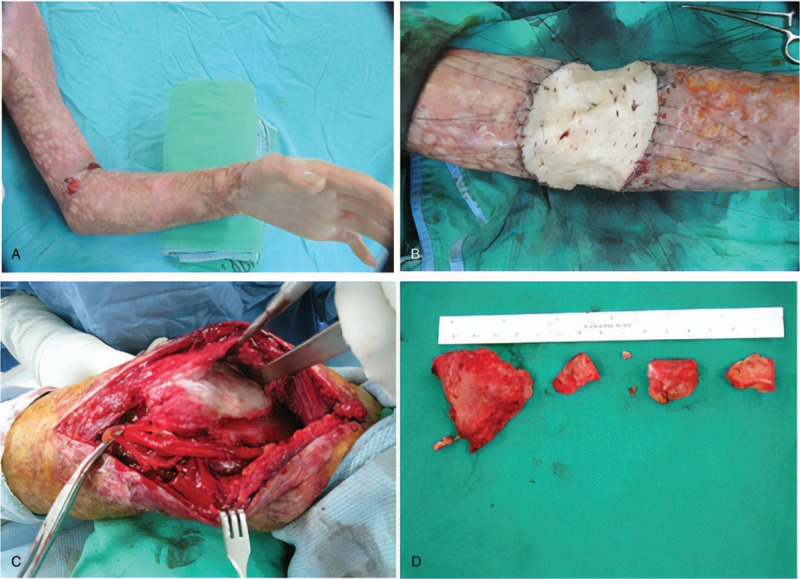
A previously healthy 26-year-old woman was sent to the emergency room with second-to-third degree 50% TBSA burns after the colored powder explosive event. The hospitalization course included 44 days of burn ICU stay and 46 days of inpatient care. Wound infection with sepsis was noted, and surgical wound debridement was performed several times. The passive elbow ROM physical therapy was started on the fourth day in ICU, and active ROM training was started 1 month after the burn injury. Both hand and elbow stiffness were noted by the attending physiotherapist 1 month after the burn, and the patient complained of progressive pain when moving her elbow. Follow-up radiographs obtained 3 months after injury demonstrated persistent HO in both elbows. The ROM/extension ROM of the right and left elbow were 5°–15° and 5°–20°, respectively. Preoperative radiographic and three-dimensional computed tomography (CT) showed that HO mainly affected the humeroulnar joint and encased the ulnar nerve (Fig. 3). Surgical excision of HO and ulnar nerve transposition were performed (right elbow: 9 months, left elbow: 10.5 months postburn). The postoperative protocol was same as that for case 1, that is, early passive ROM exercise on postoperative day 1 and active ROM exercise and stretching after relative stable wound condition was noted. The outpatient clinic was also arranged once every 2 weeks in the initial 3 months, followed by monthly clinic follow-up. The ROM recorded on 21 months postoperatively were 0° to 130° for the right elbow and 5° to 110° for the left elbow. The patient was satisfied with her increased ROM, and her pain was relieved.
Figure 3.
A-B: Preoperative radiography and reconstructed computed tomography (CT) scan reveal heterotopic ossification over the humeroulnar joint. C-D: The encased ulnar nerve is shown on the CT image and was released during surgery.
4. Case 3
A previously healthy 22-year-old man, also a victim of the same colored powder explosive event, was initially treated at another medical center for second-to-third degree 90% TBSA burns. According to the medical documentation, his hospitalization course included endotracheal intubation, 36 days of burn ICU stay, and a series of surgical debridement and skin grafting. He subsequently came to our outpatient department with the chief complaint of intolerable pain in the left elbow and ROM limitation 5 months after the burn injury.
The radiographs demonstrated HO formation in the left elbow. The range of flexion/extension ROM of the left elbow was 130° to 135°. Preoperative three-dimensional CT showed that HO affected the humeroulnar joint. Surgical excision of HO and ulnar nerve transposition were performed 6 months after the burn injury, followed by early passive ROM exercise and tolerable elbow joint stretching exercise. Regular outpatient clinic follow-up was arranged once every 2 to 4 weeks. The ROM recorded at 20 months postoperatively was 90° to 135° for the left elbow, and no recurrence of HO was noted on radiographic examination.
5. Discussion
The first case of HO associated with burn injury documented in the English literature was described in 1957.[6] However, until now, the definitive pathophysiology has remained unknown. HO has been found in patients with traumatic injuries, such as closed head injuries, spinal cord trauma, and burns. Peterson et al described the model of burn-enhanced bone formation, which may explain why HO developed in our burn injury patients.[7] The incidence of HO ranges from 0.2% to 5.6% in burn injury patients.[8–12] In this mass casualty incident, the incidence of elbow HO in the burn patients treated in our institution was 3.6% (2/56).
The most commonly affected joint requiring surgical intervention appears to be the elbow, followed by the hip joints.[11] Additionally, the humeroulnar joint is most frequently affected in elbow joint HO formation.[13] Postburn HO is frequently noted in patients with a long ICU course, prolonged mechanical ventilation, and immobilization.[8] The risk of HO formation increases with the percentage of TBSA and arm, head/neck, and trunk burns that require grafting. A recent study showed that for every 1% increase in TBSA up to a TBSA of 30%, the risk of HO increased by 13%. A scoring system is also available for physicians to predict further HO formation in burn patients at higher risk.[12]
The main purpose of the operation is to restore the functional ROM of the affected elbow. Previous biomechanical studies have shown that normal elbow ROM is from 0° (full extension) to 145° flexion, and most activities of daily living are performed within an arc of motion from 30° to 130°.[14] All three patients in this series developed elbow ROM limitations and impaired daily function. The symptoms of ulnar nerve dysfunction (numbness, paresthesia, clumsiness with the hand, hand weakness, and atrophy) might be related to nerve entrapment and indicate a need for further surgical decompression.[2,11,15]
In preoperative planning, both superficial and deep contractures should be considered. The extension of contractures, degrees of ROM, and limitations will determine different contracture release procedures. According to the algorithm modified by Hudson and Renshaw, mild soft tissue contractures (<50% ROM limitation) might be treated with Z-plasty or V-Y plasty; however, patients with severe contractures (>50% ROM limitation) might need skin grafting or flap reconstruction.[16]
The timing of HO excision has been discussed for a long time. The maturity of HO was considered in determining the timing of surgery. Bone scans have been used to detect the presence of HO, which detect sooner than conventional X-ray radiography. However, the scans can remain positive years after burn injury because of the inflammation process.[2,11,15] The serum alkaline phosphatase level is also unreliable for elbow HO detection in burn patients because in this group of patients, the heterotopic bone formation is insufficient to elevate the serum alkaline phosphatase level.[17,18] The radiographic evidence of ossification maturity (corticated margins, stable size, and appearance on serial radiographs) and matured scar tissue usually noted approximately 9 to 12 months after a burn also can help determine the timing of surgical intervention.[19] Tsionos et al have advocated treatment including early surgical resection (mean delay of 12 months; in 20 cases, the delay was ≤9.5 months) followed by rigorous postoperative physiotherapy, which has achieved ideal ROM restoration and patient satisfaction in their patients. Once surgical resection is considered, preoperative three-dimensional reconstruction CT imaging is helpful for determining the affected joint (humeroulnar joint and proximal radioulnar joint), extension of HO, and even ulnar nerve encasement.[15] CT also can provide reference images to surgeons for determining the approach needed.
In discussions of the ROM improvement after surgical HO excision, a previous systemic review study by Veltman et al determined a 75° (range, 65°–105°) ROM improvement in burn injury patients with restricted motion of the elbow and 79° (range, 56°–121°) improvement in patients with elbow ankylosis after HO excision surgery.[20]
For preventing HO recurrence, nonsteroidal anti-inflammatory drugs (NSAIDs) have been noted to be effective in preventing HO formation in major hip surgery.[21] In clinical use for burn patients, Tsionos et al treated a patient with indomethacin for 3 weeks after HO excision.[15] However, because of the potential risk of gastrointestinal side effects of prolonged use of NSAIDS, Manske and colleagues modified the NSAID use to three doses of ketorolac 30 mg intravenously every 8 hours for patients without a history of gastrointestinal ulcers or renal disease.[19] In our clinical practice, we gave piroxicam 20 mg once daily postoperatively to these three patients for 1 week. On the other hand, bisphosphonate has limited use in HO prevention in burn injury patients.[2]
The use of radiotherapy for preventing HO formation after hip procedures has been reported in several studies.[22–24] However, in burn injury patients, there is a lack of evidence supporting the routine use of radiotherapy. Additionally, the possible risk of soft tissue complications, especially in patients with skin grafts or flap reconstructions, should be considered before subjecting them to radiotherapy.
Postoperative ROM exercises are important for maintaining functional joint movement. The recent literature recommends initiating postoperative ROM exercises immediately[19,25] with passive ROM exercises on the first 2 days, followed by alternating splint and strengthening exercises for 6 months postoperatively.[19]
There are some limitations to this case report. Among all the burn victims, the incidence of HO at our institution was 3.6% (2/56), which just partially represented the incidence of this single event. It needs more cross-institutional data collection for measuring the incidence completely. Besides, since we focused on only the postburn HO patients of this event, we did not include the elbow HO patient treated at our institution previously.
6. Conclusion
In this small case series, we determined the incidence of postburn HO formation after a single burn event because most of the victims were treated at our institution. Our experience with these patients showed that once the soft tissue condition was found to be stable, early surgical HO excision combined with early postoperative physical therapy appeared to provide the ideal ROM improvement for postburn elbow HO. Additionally, NSAID scan help prevent HO recurrence. However, there is still not enough evidence yet to support the use of radiotherapy and bisphosphonates in the prevention of postburn HO formation.
Author contributions
Conceptualization: Hsu-Yu Ho.
Resources: Hsu-Yu Ho.
Supervision: Ji-Ying Chen, Yung-Chang Lu.
Writing – original draft: Ji-Ying Chen, Chun Wei Fu.
Writing – review & editing: Ji-Ying Chen, Chun Wei Fu.
Ji-Ying Chen orcid: 0000-0001-8154-594X.
Footnotes
Abbreviations: CT = computed tomography, HO = heterotopic ossification, ICU = intensive care unit, NSAIDs = nonsteroidal anti-inflammatory drugs, ROM = range of motion, TBSA = total body surface area.
All three patients have provided informed consent for publication of the cases.
The case report was approved by the Institutional Review Board Approval of Clinical Trial of MacKay Memorial Hospital, Taipei, Taiwan, ROC.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Sawyer JR, Myers MA, Rosier RN, et al. Heterotopic ossification: clinical and cellular aspects. Calcif Tissue Int 1991;49:208–15. [DOI] [PubMed] [Google Scholar]
- [2].Pontell ME, Sparber LS, Chamberlain RS. Corrective and reconstructive surgery in patients with postburn heterotopic ossification and bony ankylosis: an evidence-based approach. J Burn Care Res 2015;36:57–69. [DOI] [PubMed] [Google Scholar]
- [3].Esselman PC, Thombs BD, Magyar-Russell G, et al. Burn rehabilitation: state of the science. Am J Phys Med Rehabil 2006;85:383–413. [DOI] [PubMed] [Google Scholar]
- [4].Coons D, Godleski M. Range of motion exercises in the setting of burn-associated heterotopic ossification at the elbow: case series and discussion. Burns 2013;39:e34–8. [DOI] [PubMed] [Google Scholar]
- [5].Ministry of Health and Welfare of Taiwan - Summary of the Provision of Medical Assistance to the Formosa Fun Coast Dust Explosion Over the Past Five Months https://www.mohw.gov.tw/cp-115-302-2.html 2015. Accessed January 10, 2017. [Google Scholar]
- [6].Johnson JT. Atypical myositis ossificans. J Bone Joint Surg Am 1957;39-a:189–93. [PubMed] [Google Scholar]
- [7].Peterson JR, De La Rosa S, Sun H, et al. Burn injury enhances bone formation in heterotopic ossification model. Ann Surg 2014;259:993–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Chen HC, Yang JY, Chuang SS, et al. Heterotopic ossification in burns: our experience and literature reviews. Burns 2009;35:857–62. [DOI] [PubMed] [Google Scholar]
- [9].Levi B, Jayakumar P, Giladi A, et al. Risk factors for the development of heterotopic ossification in seriously burned adults: A National Institute on Disability, Independent Living and Rehabilitation Research burn model system database analysis. J Trauma Acute Care Surg 2015;79:870–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Orchard GR, Paratz JD, Blot S, et al. Risk factors in hospitalized patients with burn injuries for developing heterotopic ossification--a retrospective analysis. J Burn Care Res 2015;36:465–70. [DOI] [PubMed] [Google Scholar]
- [11].Hunt JL, Arnoldo BD, Kowalske K, et al. Heterotopic ossification revisited: a 21-year surgical experience. J Burn Care Res 2006;27:535–40. [DOI] [PubMed] [Google Scholar]
- [12].Schneider JC, Simko LC, Goldstein R, et al. Predicting heterotopic ossification early after burn injuries: a risk scoring system. Ann Surg 2017;266:179–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Holguin PH, Rico AA, Garcia JP, et al. Elbow anchylosis due to postburn heterotopic ossification. J Burn Care Rehabil 1996;17:150–4. [DOI] [PubMed] [Google Scholar]
- [14].Morrey BF, Askew LJ, Chao EY. A biomechanical study of normal functional elbow motion. J Bone Joint Surg Am 1981;63:872–7. [PubMed] [Google Scholar]
- [15].Tsionos I, Leclercq C, Rochet JM. Heterotopic ossification of the elbow in patients with burns. Results after early excision. J Bone Joint Surg Br 2004;86:396–403. [DOI] [PubMed] [Google Scholar]
- [16].Hudson DA, Renshaw A. An algorithm for the release of burn contractures of the extremities. Burns 2006;32:663–8. [DOI] [PubMed] [Google Scholar]
- [17].Munster AM, Bruck HM, Johns LA, et al. Heterotopic calcification following burns: a prospective study. J Trauma 1972;12:1071–4. [DOI] [PubMed] [Google Scholar]
- [18].Garland DE, Hanscom DA, Keenan MA, et al. Resection of heterotopic ossification in the adult with head trauma. J Bone Joint Surg Am 1985;67:1261–9. [PubMed] [Google Scholar]
- [19].Manske MC, Hanel DP. Postburn contractures of the elbow and heterotopic ossification. Hand Clin 2017;33:375–88. [DOI] [PubMed] [Google Scholar]
- [20].Veltman ES, Lindenhovius AL, Kloen P. Improvements in elbow motion after resection of heterotopic bone: a systematic review. Strategies Trauma Limb Reconstr 2014;9:65–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Neal BC, Rodgers A, Clark T, et al. A systematic survey of 13 randomized trials of non-steroidal anti-inflammatory drugs for the prevention of heterotopic bone formation after major hip surgery. Acta Orthop Scand 2000;71:122–8. [DOI] [PubMed] [Google Scholar]
- [22].Ayers DC, Pellegrini VD, Jr, Evarts CM. Prevention of heterotopic ossification in high-risk patients by radiation therapy. Clin Orthop Relat Res 1991;87–93. [PubMed] [Google Scholar]
- [23].Seegenschmiedt MH, Keilholz L, Martus P, et al. Prevention of heterotopic ossification about the hip: final results of two randomized trials in 410 patients using either preoperative or postoperative radiation therapy. Int J Radiat Oncol Biol Phys 1997;39:161–71. [DOI] [PubMed] [Google Scholar]
- [24].Pakos EE, Ioannidis JP. Radiotherapy vs. nonsteroidal anti-inflammatory drugs for the prevention of heterotopic ossification after major hip procedures: a meta-analysis of randomized trials. Int J Radiat Oncol Biol Phys 2004;60:888–95. [DOI] [PubMed] [Google Scholar]
- [25].Maender C, Sahajpal D, Wright TW. Treatment of heterotopic ossification of the elbow following burn injury: recommendations for surgical excision and perioperative prophylaxis using radiation therapy. J Shoulder Elbow Surg 2010;19:1269–75. [DOI] [PubMed] [Google Scholar]


