Supplemental Digital Content is available in the text
Keywords: emergency medical center, fit factor, N95 respirator, training
Abstract
Introduction:
N95 or higher filtering respirators have been recommended in healthcare settings, although there is still a risk of infection due to the improper selection and wearing of respirators. We aimed to assess the effects of training with N95 or higher filter respirators on the protection performance of respirators among healthcare providers in the emergency medical center (EMC).
Methods:
This randomized crossover study evaluated 23 healthcare providers. Quantitative fit tests (QNFTs) were performed before and after training using three types of N95 or higher filter respirators (cup-type, fold-type, valve-type). Training was performed by lecture, real-time feedback, and fit check. The primary outcome was the fit factor, and the secondary outcomes were overall fit factor, adequate protection rate, and respiratory preference.
Results:
Fit factors, overall fit factor, and adequate protection rate were higher after training than before training for the 3 types of respirators (all P < .05). For normal breathing, fit factors before and after training were 121 (10–185) vs 192 (161–200) for cup-type, 200 (39–200) vs 200 (200–200) for fold-type, and 85 (18–157) vs 173 (117–200) for valve-type. For normal breathing, the adequate protection rates before and after training were 62 (0–100) vs 100 (90–100) for cup-type, 100 (0–100) vs 100 (100–100) for fold-type, and 19 (0–100) vs 100 (44–100) for valve-type (all P < .05). The most preferred respirator type was the valve-type (10 persons, 45.5%).
Conclusions:
Training on wearing an N95 or higher respirator improved the protection performance of respirators among healthcare providers working in the EMC. The selection of proper respirators and training would be beneficial to the safety of healthcare providers.
1. Introduction
Healthcare providers are at risk of exposure to infectious diseases. In particular, as seen during the MERS (Middle East respiratory syndrome) outbreak of South Korea in 2015,[1,2] healthcare providers working in the emergency medical center (EMC) are at the forefront of exposure to infections by droplet or airborne transmission. During the MERS outbreak in South Korea in 2015, infections in the EMC accounted for 91 (49%) of the 186 hospital-related infections.[3] There are several reasons that the risk of infection is increased in the EMC:
-
(1)
overcrowding in the emergency department, which is a limited space[4];
-
(2)
numerous invasive procedures generating droplets, such as endotracheal intubation and chest compression[5,6];
-
(3)
patients visiting the EMC who have not undergone an evaluation of infection[7]; and
-
(4)
incomplete understanding of personal protective equipment (PPE), such as respirators.[8]
The most representative PPE item for preventing droplet and airborne transmission is the respirator. The American Centers for Disease Control and Prevention (CDC) guidelines recommend extended use and limited reuse of N95 filtering facepiece respirators that are certified by the National Institute for Occupational Safety and Health (NIOSH).[9,10] N95 respirators are intended to block the invasion of particles such as pathogens or droplets with diameters between 0.02 and 0.2 μm and filter over 95% of the fine particles without resistance to oil particles.[9] In European medical environments, the FFP3 filter respirator certified in accordance with the European type respiratory protection standard EN 149 is recommended.[11]
Unfortunately, healthcare providers can still be exposed to infectious agents while wearing certified N95 respirators. The protection performance of N95 respirators is dependent on the filter's performance and sealability, which is determined by the shape of the sealing surface, the pressure generated by the respirator, the breathing flow rate, and the wearer's movements.[12–17] Face seal leakage is the main component of respirator leakage.[11,13]
Thus, N95 respirators need to be evaluated to confirm sufficiently tight sealability in order to prevent infection transmission. Moreover, the Occupational Safety and Health Administration (OSHA) (29 CFR 1910.134) requires an annual respirator fit test to confirm the fit of any respirator that forms a tight seal on the wearer's face before it is used in the workplace. There are qualitative fit tests (QLFTs) and quantitative fit tests (QNFTs) that are approved and recommended by OSHA.[18] The QLFT is based on the wearer's senses of taste and smell using isoamyl acetate, saccharin, Bitrex (denatonium benzoate), or irritant smoke. The QNFT measures the fit factor by numerical value using the fit test equipment and eight movements performed for 1 minute each: normal breathing, deep breathing, moving head side to side, moving head up and down, bending over, talking, and normal breathing again.[19]
In addition to the fit test, there have been many efforts to improve the protection performance of the N95 respirator in the medical environment. Many invasive techniques, such as endotracheal intubation or chest compressions, increase the risk of infection by creating droplets. Kang et al[20] demonstrated that using a video laryngoscope rather than a direct laryngoscope in endotracheal intubation may reduce the risk of infection by reducing respirator leakage. Shin et al[21] showed that it is possible to improve the protection performance of N95 respirators when performing chest compressions, which can cause leakage of a respirator, if a respirator is appropriately selected and the wearer is trained to wear a respirator.
There have been many efforts to improve the protection performance of the N95 respirator to prevent infection transmission. Lee et al[8] showed that the protection performance of N95 respirators among healthcare providers in the EMC is lower than expected and that there is a difference in the protection performance depending on the type of respirator. Or and Kim demonstrated that training nursing students to properly wear N95 respirators improves respirator protection performance.[22,23] However, no previous study has evaluated the effect of training on improving the protection performance of N95 or higher filter respirators among healthcare providers working in the EMC. Therefore, we conducted this study to evaluate the effect of training wearing N95 or higher filter respirators on healthcare providers in the EMC.
2. Materials and methods
2.1. Study design
This prospective randomized crossover simulation study was conducted at Hanyang University Medical Centre in January 2016. The local ethics committee approved this study in November 2015 (HY-15-10-14). The study protocol was registered with the Clinical Research Information Service before study initiation (cris.nih.go.kr: HYI-15-187-1).
2.2. Participants
We recruited healthcare providers working in EMCs of tertiary hospitals in Korea in January 2016. All participants were healthy volunteers who were 16–60 years old and had experience with training in how to wear an N95 respirator within the previous 3 years. We excluded subjects who had lung disease, musculoskeletal disease, or oral and maxillofacial abnormalities. All participants signed a written consent form before study inclusion. In the preliminary study that was conducted to calculate the number of samples, four participants were assessed for the fit factor before and after the training during the movement of grimacing. The mean and standard deviation of fit factor before training were 43.1 and 73.3, and the mean and standard deviation of fit factor after training were 86.5 and 75.4. Using G-power 3.1.9.2 (Heine Heinrich University, Dusseldorf, Germany), the calculated effect size was 0.58, the alpha error was 0.05, and the power was 0.8. The calculated number of samples was 21, and thus, 23 participants were enrolled considering a 10% dropout rate.
2.3. Equipment and materials
Three types of N95 or higher filter respirators were selected for this study:
-
(1)
cup-type respirator, which is preformed to a cup shape (3M 1860 or 3M 1860S (size small); 3M, Elyria, OH, USA);
-
(2)
fold-type respirator, which is flexible and free-folded (3M 1870); and
-
(3)
valve-type respirator, which is similar to the fold type with the valve reducing exhalation resistance (3M 9332).
We selected these three respirators because they were commonly used during the MERS outbreak in South Korea in 2015. The QNFT for respirators was performed using a PortaCount Plus (TSI, Inc., St. Paul, MN, USA) (Fig. 1). This device is equipped with two sampling tubes, where one sampling tube is exposed to the atmosphere to measure ambient particles and the other sampling tube is connected to the respirator to measure particles in the respirator. The fit factor was calculated using the ratio of measured ambient particles to measured particles in respirators. The maximum fit factor score was set to 200, and fit factors of more than 100 were defined as adequate protection, which meant passing a QNFT. The two tubes were fixed by a wire hanging around the neck.
Figure 1.
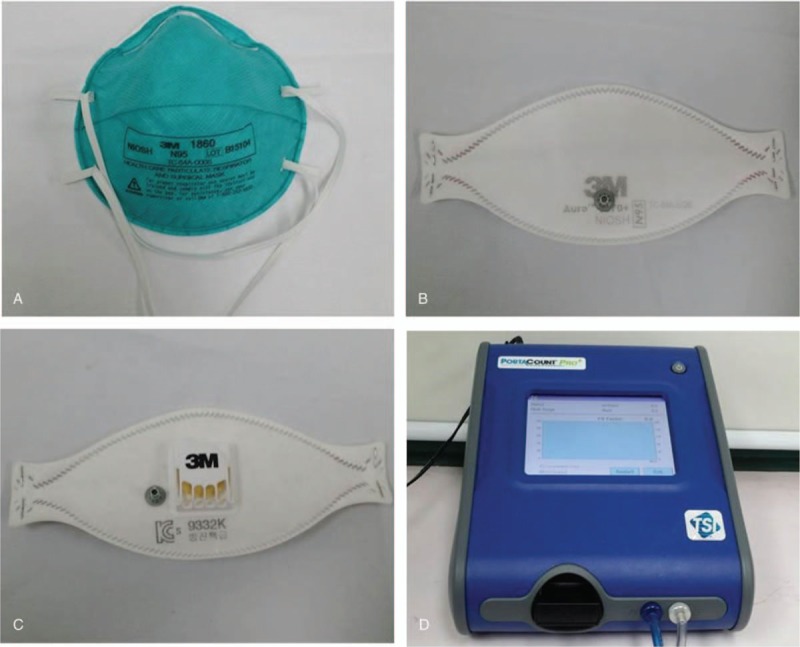
Three types of respirators with an N95 or higher filter and the device for quantitative fit test. (A) Cup-type respirator that is preformed to a cup shape (3M 1860 or 3M 1860S (small size)). (B) Fold-type respirator, which is flexible and free-folded (3M 1870). (C) Valve-type respirator, which is similar to the fold-type with the valve reducing exhalation resistance (3M 9332). (D) The quantitative fit test was performed using a PortaCount Plus (TSI Inc., St. Paul, MN).
NIOSH used an anthropological database to create a fit test panel called the NIOSH bivariate panel[24] representing Americans using filter respirators. The NIOSH bivariate panel is based on face length and face width. The respirator wearers measure the length and width of the face according to the NIOSH bivariate panel. Then, they are classified into large, medium, and small sizes and the appropriate size filter respirator (Fig. 2) is chosen. The NIOSH bivariate panel included 96.7% of American men and 98.7% of American women.[25] In the current study, participants were given appropriately sized respirators according to the NIOSH panel. The cup-type respirator is available in 3M 1860 for people who need a large and medium size and 3M 1860S for people who need a small size. Both the fold-type and the valve-type respirators are flexible and foldable, so they are worn in one size regardless of the size of the NIOSH panel.
Figure 2.
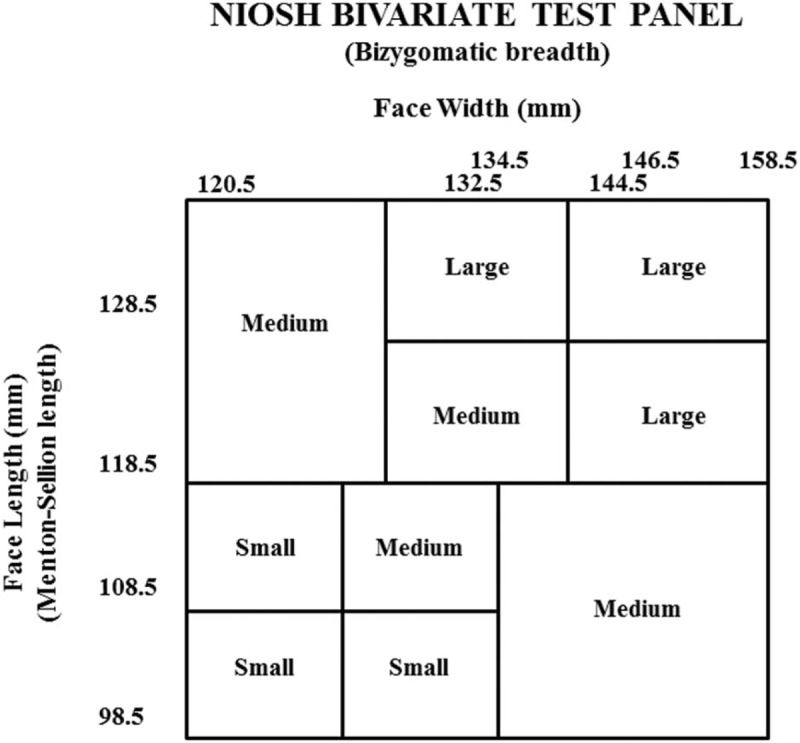
NIOSH bivariate panel. The face size (small, medium, large) is determined by both face length and face width. This panel represents 95% of respirator wearers.
Based on the CDC recommendation, we prepared training materials produced by the faculty of the Infection Control Department at Hanyang University Medical Centre (Supplement 1).
2.4. Interventions
All participants completed a brief questionnaire about demographic information (age, sex, body weight, and height), clinical career, and prior experience of donning respirators. A total of 23 participants were enrolled and randomly allocated to 3 groups according to the first type of respirator that was worn (www.random.org; Fig. 3). All participants were prohibited from smoking, eating, and drinking (except for water) for at least 30 min before and during the quantitative fit test. The fit test was performed in the resuscitation room in the EMC (24.3 m3) without operating air conditioning systems to minimize any confounding effect of the air conditioning system on the concentration of particles. All steps were done by Hongjung Kim who was an emergency physician. Then, those assessing outcomes were blinded.
Figure 3.
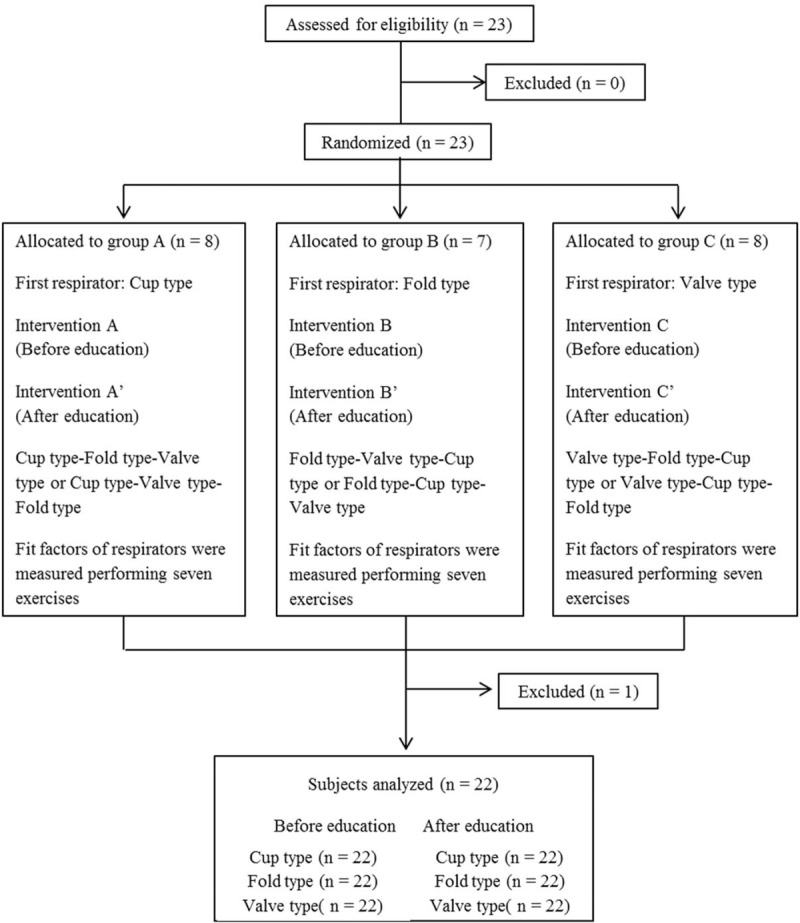
Diagram showing the flow chart of the study.
We used a TSI model 8026 Particle Generator to generate a sodium chloride aerosol and ensure that the ambient air contained at least 100 particles per cc in the proper size range.[26] All participants were given respirators based on their face size as recommended by the NIOSH panel.[25] Fit factors for the three types of respirators were measured while participants performed the following seven movements for 1 minute per movement by OSHA respiratory protection regulation: (1) normal breathing, (2) deep breathing, (3) moving the head side to side, (4) moving the head up and down, (5) reading the rainbow passage aloud, (6) grimacing and (7) bending at the waist. All participants had an approximately 2-min break between each test of movement. After that, all participants had a rest for 30 min and then had training in how to wear a respirator properly. After training, fit factors for the three types of respirators were measured again performing the seven movements as before.
We implemented training on wearing a respirator by a lecture with training materials produced by the faculty of the Infection Control Department. After that, all participants had 30 minutes of training to wear respirators, and they received real-time feedback by educators and feedback by fit check. We showed them how to wear respirators in a multistep process: (1) donning it correctly, (2) making adjustments for a secure facial seal, (3) confirming the fit, and (4) properly removing it.[27] The participants followed each step and received feedback immediately. The fit check (also known as seal check) is a procedure advocated by CDC, a self-check the wearer performs to detect air leakage of the respirator. The fit check includes both positive and negative pressure checks. To perform the positive pressure check, the wearer places both hands over the front of the respirator and exhales gently into the respirator. The face fit is considered acceptable if a slight positive pressure can be made inside the respirator without outward leakage of air at the seal. To perform the negative pressure check, the wearer covers the respirator with the palm of the hands and inhales gently so that the respirator collapses slightly and holds the breath for ten seconds. If the respirator collapses slightly but remains in shape and no inward leakage of air is detected, the tightness of the respirator is considered acceptable.[28] All processes were conducted by the faculty of the Infection Control Department at Hanyang University Medical Centre.
2.5. Outcomes
Primary outcomes were the fit factors of the three respirators during movements before and after training. Secondary outcomes were overall fit factor, adequate protection rate, and the preference of the respirator. The overall fit factor was calculated from the individual fit factors determined for each test movement performed by each participant.[8]
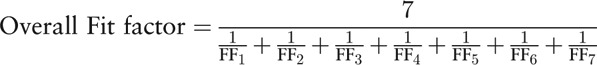 |
FFn is the fit factor of n movement of one participant.
The adequate protection rate was defined as the percentage of fit factors ≥100, as this suggests that the respirator provided proper protection. The preference of the respirator was recorded by asking the participants to indicate their preferred respirator to use in clinical situations after the end of study.
2.6. Statistical analysis
The data were compiled using a standard spreadsheet application (Excel; Microsoft, Redmond, WA, USA) and were analyzed using Statistical Package for the Social Sciences for Windows (version 20.0; IBM Corp., Armonk, NY, USA). Categorical data were reported in absolute numbers and percentages, and continuous data were reported in median values and interquartile ranges when the data were not normally distributed. The Wilcoxon signed-rank was used to test for differences in non-normally distributed variables such as fit factor, overall fit factor, and adequate protection rate before and after training (differences with a P-value of <.05 were statistically significant). The difference in the fit factors of the three respirators was verified using the Friedman test (differences with a P-value of <.05 were statistically significant). Post hoc analysis between the two groups was performed using the Wilcoxon signed-rank test with Bonferroni correction (differences with a P-value of <.017 were statistically significant)
3. Results
3.1. General characteristics
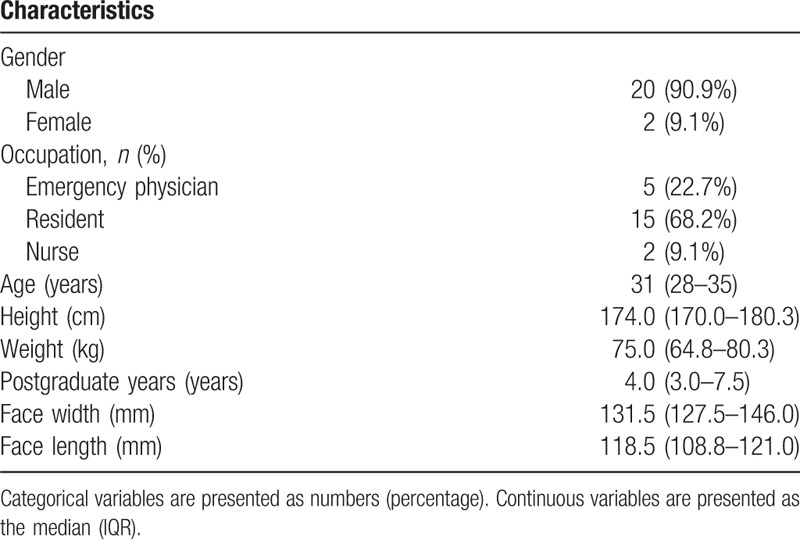
A total of 23 participants participated, but one participant was excluded because of experiencing discomfort during the fit test, and a total of 22 participants completed the study. The general characteristics of the participants are shown in Table 1. All participants had experience with training on how to wear an N95 respirator within the previous 3 years.
Table 1.
Demographic characteristics (n = 22).
3.2. NIOSH panel
All participants in this study were matched with the NIOSH bivariate test panel; 8 participants (36.4%) had a large face, 7 (31.8%) had a medium face, and 7 (31.8%) had a small face (Fig. 4). Fold-type and valve-type respirators can be worn as one size regardless of the size according to the NIOSH panel, so all 22 participants wore the same size. For the cup-type respirator, 15 participants (large and medium) wore model 1860, and 7 (small size) wore model 1860S.
Figure 4.
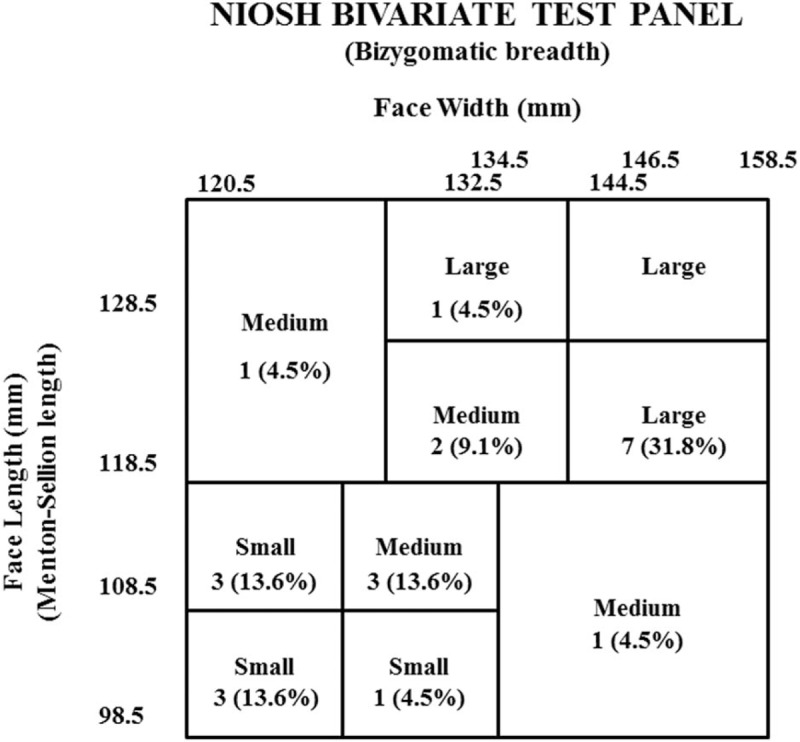
Distribution of participants according to the NIOSH bivariate panel. Categorical variables are given as numbers (percentage). Eight participants were large, 7 were medium, and 7 were small.
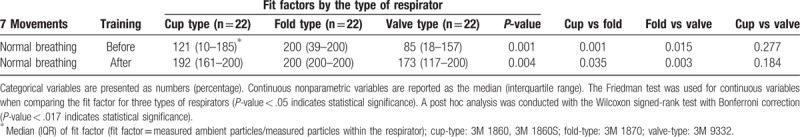
3.3. Fit factors during the performance of the seven movements before and after training
The fit factor for the three types of respirators was higher after training than before during all movements (all P < .05). The fit factor for the three types of respirators was lowest during grimacing of all movements after and before training. The fold type showed the highest fit factor for all movements after training (Table 2). Furthermore, fold-type respirators showed a higher fit factor than valve-type and cup-type respirators in normal breathing before and after training (Table 3). The overall fit factor for the three types of respirators was higher after training than before during all movements (all P < .05).
Table 2.
Comparison of fit factors determined by the quantitative fit test before and after fitting training for the three types of respirators.
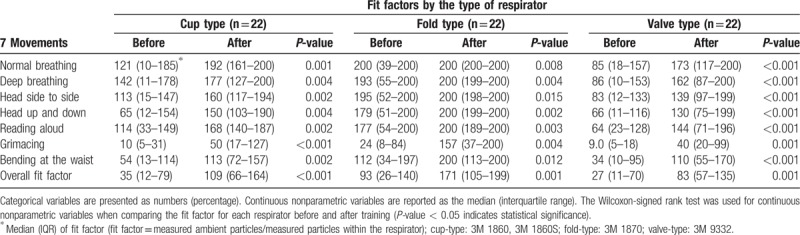
Table 3.
Comparison of fit factors among the three types of respirators determined by the quantitative fit test before and after fitting training.
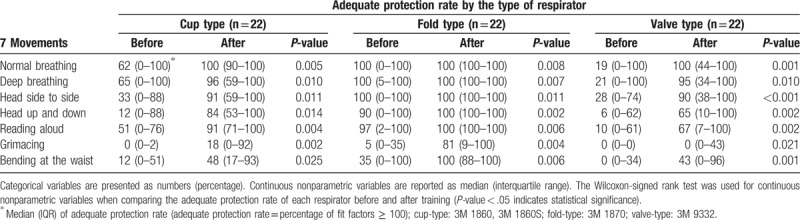
3.4. Adequate protection rate during performance of the seven movements before and after training
The adequate protection rate of the three types of respirators was higher after training than before in all seven movements (all P < .05) (Table 4). The adequate protection rate was the lowest during grimacing among all movements in the three types of respirators before and after training. The adequate protection rate of the fold-type respirator in all movements except grimacing was 100% after training. The adequate protection rate of the three respirators during normal breathing was 100% after training.
Table 4.
Comparison of adequate protection rate determined by the quantitative fit test before and after fitting training for the three types of respirators.
3.5. Preference
Ten participants (45.5%) preferred the valve-type respirator, 9 (40.9%) preferred the fold-type respirator, and 3 (13.6%) preferred the cup-type respirator.
4. Discussion
Healthcare providers working in the EMC are at the forefront of exposure to infection. An N95 or higher filter respirator is recommended to be worn to prevent droplet or airborne transmission.[9] However, the protection performance of the respirator could be poor due to leakage between the face and respirator. This study was conducted to evaluate the effect of training wearing an N95 or higher filter respirator on healthcare providers in the EMC.
Many training methods for protective performance have been developed. There are four different types of training media: (1) printed training books, (2) noninteractive videos, (3) computer-based training, or (4) direct interactive training.[27] Additionally, there are several ways in which participants can obtain feedback: (1) direct feedback by educator, (2) fit check (self-check), and (3) real-time quantitative test using the PortaCount Plus. Eckerman and Lundeen demonstrated the superiority of direct interactive training for teaching occupational safety and health information in working adults.[29] Therefore, we selected direct interactive training as the training method and real-time feedback by educator and fit check. Respirator use is a multistep process including correctly donning the gear, making adjustments for a secure facial seal, confirming the fit, and properly removing the respirator. In this simulation study, educators took note of the above procedures and provided detailed and practical training to each participant on each procedure and gave feedback. For each of the procedures, we were especially careful about putting the straps in place because this mistake was often made during the procedures.[27]
As shown in Tables 2 and 4, this simulation study revealed that training healthcare providers in the EMC could significantly improve the fit factor and adequate protection rate of the three types of respirators. The clinical experience of all participants in this study was more than three years, and they had been trained to wear respirators and had experience wearing respirators. Nevertheless, proper protection performance of the respirator could not be expected before training and was improved after training. As seen in Table 4, particularly adequate protection showed 100% of normal breathing after training regardless of respirator type. The training on respirators for healthcare providers in the EMC helped to improve protection performance. Considering that the training time was less than 30 min and that the training consists of feedback by the educator and a fit check by the participants, the improvement effect of training on the protection performance of the respirator can be judged to be large without other equipment and long training times. The protection performance of respirators was improved after training, but it is also important to choose the right respirator because the respirator with the highest protective performance was still the highest after training. Therefore, the choice of a proper respirator is important.[8]
The fit factor and adequate protection rate were the lowest during grimacing regardless of the type of respirator (Table 4). In the grimacing movement, the fit factor before training was 10 (5–31) for cup-type, 24 (8–84) for fold-type, and 9 (5–18) for valve-type (Table 2), and the adequate protection rate before training was 0% (0–2) for cup-type, 5% (0–35) for fold-type, and 0% (0–0) for valve-type (Table 4). During the grimacing movement, the fit factor after training was 50 (17–127) for cup-type, 157 (37–200) for fold-type, and 40 (20–99) for valve-type (Table 2), and the adequate protection rate after training was 18% (0–92) for cup-type, 81% (9–100) for fold-type, and 0% (0–43) for valve-type (Table 4). As we can see, it was difficult to say that adequate protection was achieved. Grimacing movement disturbs the adhesion between the face and the filter respirator and causes leakage. Even if one wears an N95 respirator, he/she should avoid movements that disturb adhesion, such as grimacing movements, where the risk of transmission exists.
After all the simulations were completed, participants were asked which respirator they would like to wear in the clinical situation of outbreak of infectious disease. Of the participants, 10 (45.5%) preferred the valve-type, 9 (40.9%) preferred the fold-type, and 3 (13.6%) preferred the cup-type respirator. The cup-type respirator is made of a hard material, so the pressure on the face produced by the strap and the respirator is felt to be greater than that of other types of respirators, resulting in discomfort and decreased preference. In one study, cup-type respirators were proved to produce greater pressure at the same fit factor than fold-type respirators.[30] Valve-type respirators were preferred because they allowed the wearer to feel more comfortable due to the valve, which reduced breathing resistance.[30,31]
In cases of outbreaks of new infectious diseases or biological terror attacks, N95 or higher filter respirators should be worn for a long time. In one study, wearing a respirator for a long time did not create clinical physiological burdens. However, wearers showed subjective discomfort and symptoms.[32] If the respirator causes discomfort, compliance with wearing respirators could be reduced. Therefore, wearing comfortable and preferred respirators is important.[33,34] The better the adhesion of the respirator, the more the pressure on the face and the discomfort increases. Decreased pressure between the respirator and face can be comfortable but leaky.[30,32] A fold-type respirator can be preferred to cup-type when it is necessary to wear the respirator for a long time, since a cup-type respirator creates increased pressure at the same fit factor compared with a fold-type respirator.[30]
There are some limitations to this study. First, the three filter respirators are not the same grade and classification. The researchers used three types of filter respirators that were routinely used in Korea during the outbreak of MERS. The cup-type (3M 1860) and fold-type (3M 1870) respirators are NIOSH certified N95 filter respirators, while the valve-type (3M 9332) respirators are FFP3 filter respirators certified in the European standard EN 149. Second, there are hundreds of filter respirators, but only three types of filter respirators were used in this study. Third, participants in this study worked in only one EMC, and only two nurses participated. Because healthcare providers have different training and clinical experience depending on the institute and occupation, conducting simulations including more occupations and institutions is necessary. Fourth, only one method of training was selected. Fifth, this study did not investigate the sustained effect of training. OSHA requires respirator users to be trained and pass the fit test annually.[19]
5. Conclusions
In the case of healthcare providers in the EMC, the protection performance of the respirator was significantly improved by training regardless of the respirator type. Healthcare providers in the EMC should not only wear N95 or higher filter respirators but also be trained on how to wear respirators.
Author contributions
Conceptualization: Juncheol Lee, Sanghyun Lee, Jaehoon Oh, Hyunggoo Kang.
Data curation: Hongjung Kim, Hyunggoo Kang.
Formal analysis: Hongjung Kim, Juncheol Lee, Sanghyun Lee, Hyunggoo Kang.
Investigation: Hongjung Kim, Sanghyun Lee.
Methodology: Hongjung Kim, Juncheol Lee, Sanghyun Lee, Boseung Kang.
Project administration: Hongjung Kim, Juncheol Lee, Boseung Kang.
Resources: Hongjung Kim, Juncheol Lee, Jaehoon Oh, Boseung Kang, Hyunggoo Kang.
Software: Hongjung Kim.
Supervision: Sanghyun Lee.
Validation: Sanghyun Lee, Jaehoon Oh, Tae Ho Lim.
Visualization: Sanghyun Lee.
Writing – original draft: Hongjung Kim, Juncheol Lee.
Writing – review & editing: Hongjung Kim, Juncheol Lee, Sanghyun Lee, Jaehoon Oh, Boseung Kang, Tae Ho Lim, Hyunggoo Kang.
Hongjung Kim orcid: 0000-0003-4003-8612.
Supplementary Material
Footnotes
Abbreviations: CDC = American Centers for Disease Control and Prevention, EMC = emergency medical center, FFP = filtering facepiece respirator, MERS = Middle East respiratory syndrome, NIOSH = National Institute for Occupational Safety and Health, OSHA = Occupational Safety and Health Administration, PPE = personal protective equipment, QLFT = qualitative fit tests, QNFT = quantitative fit tests.
HK and JL contributed equally to this study.
The authors have no conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
References
- [1].Shin N, Kwag T, Park S, et al. Effects of operational decisions on the diffusion of epidemic disease: a system dynamics modeling of the MERS-CoV outbreak in South Korea. J Theor Biol 2017;421:39–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Kim SW, Park JW, Jung H-D, et al. Risk factors for transmission of Middle East respiratory syndrome coronavirus infection during the 2015 outbreak in South Korea. Clin Infect Dis 2017;64:551–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Lee KH. Emergency medical services in response to the Middle East respiratory syndrome outbreak in Korea. J Korean Med Assoc 2015;58:611–6. [Google Scholar]
- [4].Di Somma S, Paladino L, Vaughan L, et al. Overcrowding in emergency department: an international issue. Intern Emerg Med 2015;10:171–5. [DOI] [PubMed] [Google Scholar]
- [5].Denis MA, Ecochard R, Bernadet A, et al. Risk of occupational blood exposure in a cohort of 24,000 hospital healthcare workers: position and environment analysis over three years. J Occup Environ Med 2003;45:283–8. [DOI] [PubMed] [Google Scholar]
- [6].Kelen GD, Hansen KN, Green GB, et al. Determinants of emergency department procedure- and condition-specific universal (barrier) precaution requirements for optimal provider protection. Ann Emerg Med 1995;25:743–50. [DOI] [PubMed] [Google Scholar]
- [7].Niska R, Bhuiya F, Xu J. National Hospital Ambulatory Medical Care Survey: 2007 emergency department summary. Natl Health Stat Report 2010;1–31. [PubMed] [Google Scholar]
- [8].Lee S, Kim H, Lim T, et al. Simulated workplace protection factors for respirators with N95 or higher filters for health care providers in an emergency medical centre: a randomized crossover study. Hong Kong J Emerg Med 2017;24:282–9. [Google Scholar]
- [9].Centers for Disease Control and Prevention. 2007 Guideline for isolation precautions: preventing transmission of infectious agents in health care settings. http://www.cdc.gov/ncidod/dhqp/pdf/guidelines/Isol. http://www.ajicjournal.org/article/S0196-6553(07)00740-7/fulltext?mobileUi=0 2007. Accessed July 3, 2009. [Google Scholar]
- [10].Tablan OC, Anderson LJ, Besser R, et al. Guidelines for preventing health-care—associated pneumonia, 2003: recommendations of CDC and the Healthcare Infection Control Practices Advisory Committee. MMWR Recomm Rep 2004;53:1–36. [PubMed] [Google Scholar]
- [11].Transmission Based Precautions Literature Review: Respiratory Protective Equipment (RPE). National Infection Prevention and Control Manual, National Services Scotland Website. http://www.nipcm.hps.scot.nhs.uk/documents/tbp-respiratory-protective-equipment-rpe/ Published October 6, 2017. Accessed November, 14, 2018. [Google Scholar]
- [12].Lei Z, Ji X, Li N, et al. Simulated effects of head movement on contact pressures between headforms and N95 filtering facepiece respirators part 2: simulation. Ann Occup Hyg 2014;58:1186–99. [DOI] [PubMed] [Google Scholar]
- [13].Crutchfield CD, Fairbank EO, Greenstein SL. Effect of test exercises and mask donning on measured respirator fit. Appl Occup Environ Hyg 1999;14:827–37. [DOI] [PubMed] [Google Scholar]
- [14].Grinshpun SA, Haruta H, Eninger RM, et al. Performance of an N95 filtering facepiece particulate respirator and a surgical mask during human breathing: two pathways for particle penetration. J Occup Environ Hyg 2009;6:593–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Rengasamy S, Eimer BC. Nanoparticle penetration through filter media and leakage through face seal interface of N95 filtering facepiece respirators. Ann Occup Hyg 2012;56:568–80. [DOI] [PubMed] [Google Scholar]
- [16].Lei Z, Yang J, Zhuang Z, et al. Simulation and evaluation of respirator faceseal leaks using computational fluid dynamics and infrared imaging. Ann Occup Hyg 2013;57:493–506. [DOI] [PubMed] [Google Scholar]
- [17].Myers WR, Zhuang Z. Field performance measurements of half-facepiece respirators: developing probability estimates to evaluate the adequacy of an APF of 10. Am Ind Hyg Assoc J 1998;59:796–801. [DOI] [PubMed] [Google Scholar]
- [18].Hospital Respiratory Protection Program Toolkit. Occupational Safety and Health Administration Website. https://www.osha.gov/Publications/OSHA3767.pdf Published May 2015, Accessed November 14, 2018. [Google Scholar]
- [19].Occupational Safety and Health Administration. Fit Testing Procedures (Mandatory) 1910.134 App A. Occupational Safety and Health Administration Website. https://www.osha.gov/pls/oshaweb/owadisp.show_document?p_id=9780&p_table=STANDARDS Published April 23, 1998, Updated August 4, 2004, Accessed November 14, 2018. [Google Scholar]
- [20].Kang H, Lee Y, Lee S, et al. Protection afforded by respirators when performing endotracheal intubation using a direct laryngoscope, GlideScope®, and i-gel® device: a randomized trial. PLoS One 2018;13:e0195745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Shin H, Oh J, Lim TH, et al. Comparing the protective performances of 3 types of N95 filtering facepiece respirators during chest compressions: a randomized simulation study. Medicine (Baltimore) 2017;96:e8308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Or P, Chung J, Wong T. Does training in performing a fit check enhance N95 respirator efficacy? Workplace Health Saf 2012;60:511–5. [DOI] [PubMed] [Google Scholar]
- [23].Kim H, Baek JE, Seo HK, et al. Comparison of fit factor for healthcare workers before and after training with the N95 mask. J Korean Soc Occup Environ Hyg 2014;24:528–35. [Google Scholar]
- [24].Zhuang Z, Groce D, Ahlers HW, et al. Correlation between respirator fit and respirator fit test panel cells by respirator size. J Occup Environ Hyg 2008;5:617–28. [DOI] [PubMed] [Google Scholar]
- [25].Zhuang Z, Bradtmiller B, Shaffer RE. New respirator fit test panels representing the current U.S. Civilian work force. J Occup Environ Hyg 2007;4:647–59. [DOI] [PubMed] [Google Scholar]
- [26].Niezgoda G, Kim JH, Roberge RJ, et al. Flat fold and cup-shaped N95 filtering facepiece respirator face seal area and pressure determinations: a stereophotogrammetry study. J Occup Environ Hyg 2013;10:419–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Harber P, Boumis RJ, Su J, et al. Component analysis of respirator user training. J Occup Environ Hyg 2013;10:556–63. [DOI] [PubMed] [Google Scholar]
- [28].Centers for Disease Control and Prevention (CDC). Laboratory performance evaluation of N95 filtering facepiece respirators, 1996. MMWR Morb Mortal Wkly Rep 1998;47:1045–9. [PubMed] [Google Scholar]
- [29].Eckerman DA, Lundeen CA, Steele A, et al. Interactive training versus reading to teach respiratory protection. J Occup Health Psychol 2002;7:313–23. [PubMed] [Google Scholar]
- [30].Shenal BV, Radonovich LJ, Cheng J, et al. Discomfort and exertion associated with prolonged wear of respiratory protection in a health care setting. J Occup Environ Hyg 2012;9:59–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Roberge RJ, Kim JH, Benson S. N95 filtering facepiece respirator deadspace temperature and humidity. J Occup Environ Hyg 2012;9:166–71. [DOI] [PubMed] [Google Scholar]
- [32].Rebmann T, Carrico R, Wang J. Physiologic and other effects and compliance with long-term respirator use among medical intensive care unit nurses. Am J Infect Control 2013;41:1218–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].National Academies Press (US), Larson EL, Liverman CT. Preventing Transmission of Pandemic Influenza and Other Viral Respiratory Diseases: Personal Protective Equipment for Healthcare Personnel: Update 2010. 2011. [PubMed] [Google Scholar]
- [34].Baig AS, Knapp C, Eagan AE, et al. Health care workers’ views about respirator use and features that should be included in the next generation of respirators. Am J Infect Control 2010;38:18–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


