Abstract
Background:
Deaths from fentanyl exposure continue to increase in the US. Fentanyl test strips are now available to test urine for presence of fentanyl, but additional testing methods are needed to determine past exposure and to determine exposure to specific analogs.
Objectives:
To investigate exposure to such analogs through hair-testing.
Methods:
40 individuals in inpatient detoxification (7.5% female) reporting past-month heroin use were surveyed and provided a hair sample to be tested at a later date. While results could not be provided to patients, they were asked how they would respond if informed that their hair tested positive for fentanyl. UHPLC-MS/MS was used to test for past exposure to fentanyl and six other novel synthetic opioids and fentanyl biomarkers/metabolites.
Results:
27.5% reported known fentanyl use in the past year and 67.5% reported suspected exposure. 97.5% (39 of 40) tested positive for fentanyl, 90.0% tested positive 4-ANPP (a biomarker) and norfentanyl (a metabolite); 82.5% tested positive for acetyl-fentanyl, 47.5% tested positive for furanyl-fentanyl, and 7.5% tested positive for U-47700. Most participants (82.5%) reported they would warn others about fentanyl if they learned their hair tested positive; 75.0% reported they would try to stop using heroin, and 65.0% reported they would ensure that someone nearby has naloxone to reverse a potential overdose.
Conclusions:
Hair testing is useful in detecting the past exposure to fentanyl, its analogs, and other novel synthetic opioids. Further research is needed to determine whether individuals who use heroin learning about exposure affects drug-taking and treatment-seeking behavior.
Keywords: heroin, fentanyl, adulterants, hair-testing
Introduction
Deaths related to use of fentanyl, its analogs, and novel synthetic opioids have more than doubled in the US from 9,580 in 2015 to 19,413 in 2016 (1). In 2016, fentanyl and/or its analogs were detected in almost half (46%) of opioid-related decedents (1). Fentanyl, a synthetic opioid, is 50–100 times more potent than morphine, and many of its analogs are thousands of times more potent than morphine (2,3). These compounds are increasingly adulterating heroin, often unbeknownst to individuals who use, increasing risk of overdose (4). Studies suggest many individuals who misuse opioids are concerned about unintentional exposure to fentanyl, although some individuals who use heroin seek out fentanyl. For example, one study found that 18% of homeless or marginally housed individuals who use opioids and tested positive for fentanyl reported known use (5). Studies of individuals who use drugs have found that 85–92% wanted to know if their drugs contain fentanyl (6,7). Thus, more research is needed not only to test for exposure to these compounds, but also to determine how individuals who use drugs learning about exposure may affect their drug-taking (e.g., harm reduction) and treatment-seeking behavior.
As the opioid crisis continues to worsen in the US, national and state-level statistics continue to focus largely on seizures, poisonings, and deaths related to exposure to fentanyl and its analogs (1,8,9). However, literature suggests variable awareness regarding the extent to which individuals who use heroin are aware of potential exposure to fentanyl (5,10–15). A new common method of determining recent exposure to fentanyl or its analogs is through urine testing (5). BTNX fentanyl test strips, for example, can rapidly detect fentanyl and many of its analogs in urine (5,7). However, such test strips cannot distinguish between fentanyl and its analogs or extent of exposure. Urine testing is also limited by the persistence of compounds being detectable for only ~3 days (16). Research utilizing fentanyl test strips to test urine (or to directly test drug samples) is in its infancy, and many clinicians do not routinely utilize fentanyl strips to test their patients.
While urine and drug sample testing for presence of fentanyl can provide useful information regarding recent exposure, additional testing methods are needed to help address limitations of urine and drug sample-testing. Our past work has determined that hair testing is an optimal biological matrix to obtain an extensive exposure history of past use of novel psychoactive substances (17–20). Although hair testing cannot detect very recent exposure (e.g., within a few days post-use) or yield immediate results, it allows wide-range monitoring of drug exposure over extended periods of time. Acquiring a more extensive history of exposure may be useful in informing prevention or harm reduction among individuals who use heroin or other drugs with potential for fentanyl adulteration.
Past exposure to fentanyl, its analogs, and other novel synthetic opioids was examined in a sample of individuals who recently used heroin. Beliefs and concerns about fentanyl were assessed and participants were asked how they would respond if they learned their hair had tested positive for fentanyl. Results will inform prevention and harm reduction among individuals who use drugs who are at risk for fentanyl exposure.
Methods
Participants and Procedure
Inpatients were recruited from the detoxification unit at Bellevue Hospital Center, a university-affiliated, public sector hospital in New York City. Patients were recruited from April through July of 2018. Individuals were approached by a research assistant within the inpatient unit to determine eligibility and interest in participation. To be eligible, inpatients had to 1) be at least 18 years of age, 2) report using heroin in the past 30 days, and 3) have adequate length/amount of hair for analysis (i.e., ~100 hairs, ≥1cm in length). While head hair was preferred, hair from the body (e.g., leg, arm, chest), face (e.g., beard), and pubic region were also acceptable. Eligible individuals provided informed consent, completed a brief survey on an electronic tablet (which typically took about 10 minutes to complete), and then provided a hair sample. A research assistant cut the hair sample with a scissor or buzzer from as close to the scalp or skin as possible. In some cases (e.g., for those providing pubic hair), the sample was cut by the participant in private upon receiving proper instructions. Participants completing the study received a $10 MetroCard. The Institutional Review Boards at New York University Langone Medical Center and Bellevue Hospital Center approved all study procedures. The response rate for participation was 83% with 40 patients participating in the study.
Measures
Participants were asked about demographic characteristics including age, race/ethnicity, education, income, and employment. With regard to heroin use, they were asked about route(s) of administration, whether heroin was used daily, the number of years they have been using heroin, and how many bags of heroin they use per day (on average). Participants were asked whether they had knowingly used fentanyl in the past 12 months, and they were asked about beliefs and concerns regarding potential fentanyl exposure. Although hair test results could not be provided to participants, they were asked whether they agreed with 7 statements regarding how they would respond if they learned that fentanyl was detected in their hair sample. Statements were based on previous qualitative studies of unintentional fentanyl exposure (6, 21, 22), and assessed whether they would 1) warn individuals they know who use heroin that they may be unknowingly using fentanyl, 2) try to stop using heroin, 3) use heroin more slowly or in smaller amounts, 4) take small test doses to see how they react, 5) make sure someone nearby has naloxone to reverse an overdose, 6) find a more trustworthy dealer, and 7) use drug test strips that can detect fentanyl.
Hair Analysis
The majority of participants provided hair from their head (57.5%, n=23), followed by leg (12.5%, n=5) or arm (12.5%, n=5), the chest (7.5%, n=3), beard (5.0%, n=2), and pubic region (5.0%, n=2). Hair was locked in a piece of aluminum foil and placed into a small envelope containing the participant’s identification number (to link test results to survey responses at a later date). A minimum quantity of 25 mg of hair was needed to perform the analysis. All samples were analyzed in their full length. The average length of head hair sample was 4.0 cm (median=3.0 cm), where the approximated diagnostic window is based on normal growth rate (1 cm=1 month). It was not possible to perform a segmental analysis or to test for other drugs (i.e., heroin), due to the low amount of available hair.
Hair testing was conducted using an on-purpose developed and validated ultra-high performance liquid chromatography–tandem mass spectrometry (UHPLC-MS/MS) method (20). The target analytes were 1) fentanyl, 2) carfentanil, 3) acetylfentanyl, 4) furanylfentanyl, 5) norfentanil, 6) 4-ANPP, and 7) U-47700. 4-ANPP is considered a biomarker of several fentanyl analogs, and norfentanil is a metabolite, so these were included in our testing (23). All fentanyl analogs and novel opioids examined were currently on the black market in the US (24). The parent drug usually represents the target analyte in the keratin matrix that incorporates it from sweat and/or bloodstream, the sebum, and/or from external contamination (25). The limits of detection (LODs) values were in the range 0.1–0.3 pg/mg for all analytes and the limits of quantitation (LOQs) values lied between 0.3–0.9 pg/mg.
Statistical Analysis
Hair results were dichotomized into whether or not exposure to each compound was detected and merged with participant survey data. Descriptive analyses were conducted to describe the participants and test results. Chi-square and Fisher’s Exact Test was used to examine whether there were differences between those reporting known fentanyl use vs. no known fentanyl use with regard to beliefs and concerns about fentanyl, behavioral aspirations related to test results, and testing positive for each separate analog.
Results
Table 1 presents the demographic and heroin use characteristics of the 40 participants. On average, participants were 41.5 years of age (SD=10.6, range=20–60); 75.0% reported using heroin daily, and on average, they had been using heroin for 12.8 (SD=11.7) years, and use 11.4 (SD=7.3) bags of heroin per day.
Table 1.
Demographic and heroin use characteristics (n=40).
| Characteristic | % (n) | Mean (SD) |
|---|---|---|
| Age – mean (SD) | 41.5 (10.6) | |
| Sex | ||
| Male | 92.5 (37) | |
| Female | 7.5 (3) | |
| Race/Ethnicity | ||
| White | 35.7 (15) | |
| Black | 20.0 (8) | |
| Hispanic | 40.0 (16) | |
| Other | 2.5 (1) | |
| Education | ||
| Less than High School | 22.5 (9) | |
| High School Diploma or Equivalent | 55.0 (22) | |
| Some College | 20.0 (8) | |
| College Degree | 2.5 (1) | |
| Weekly Income | ||
| $0-$100 | 35.0 (14) | |
| $101-$300 | 27.5 (11) | |
| >$300 | 37.5 (15) | |
| Employed | ||
| No | 67.5 (27) | |
| Yes | 32.5 (13) | |
| Heroin Use | ||
| Number of Years Using Heroin – mean (SD) | 12.8 (11.7) | |
| Number of Bags Used Daily – mean (SD) | 11.4 (7.3) | |
| Uses Heroin Daily | ||
| No | 25.0 (10) | |
| Yes | 75.0 (30) | |
| Route(s) of Administration in the Past Year | ||
| Snort Only | 50.0 (20) | |
| Inject Only | 25.0 (10) | |
| Snort and Inject | 10.0 (4) | |
| Snort and Smoke | 7.5 (3) | |
| Snort, Inject, and Smoke | 7.5 (3) |
Note. SD = standard deviation
Over a quarter (27.5%, n=11) of participants reported that they had knowingly used fentanyl within the past year. Table 2 presents descriptive statistics regarding beliefs and concerns about fentanyl. Two-thirds (67.5%) of participants reported suspecting they had been exposed to fentanyl. 87.5% of participants reported that they would want to know if they had been exposed to fentanyl, and about two-thirds (65.0%) reported being very or somewhat concerned about fentanyl adulteration. 30.0% reported believing they would be able to notice if their heroin contained fentanyl, and almost half (47.5%) reported that they expected their hair to test positive for fentanyl. The only significant difference between those reporting known use versus unknown use was with regard to expecting hair to test positive for fentanyl. Specifically, 90.9% of those reporting known use and 31.0% of those reporting no known use expected a positive result (p=.001).
Table 2.
Participant beliefs and concerns about fentanyl, anticipated reactions if learned about fentanyl exposure, and prevalence of testing positive for fentanyl or other analogs.
| Full Sample (n=40) |
Known Fentanyl Use (Self-Report) (27.5%, n=11) |
No Known Fentanyl Use (Self-Report) (72.5%, n=29) |
|
|---|---|---|---|
| Beliefs and Concerns about Fentanyl | % Agreement (n) | % Agreement (n) | % Agreement (n) |
| Would want to know if their heroin contains fentanyl | 87.5 (35) | 72.7 (8) | 93.1 (27) |
| Suspect they may have been exposed to fentanyl | 67.5 (27) | 72.7 (8) | 65.5 (19) |
| Concerned about fentanyl adulteration | 65.0 (26) | 54.6 (6) | 69.0 (20) |
| Expect their hair to test positive for fentanyl | 47.5 (19) | 90.9(10)* | 31.0 (9) |
| Believe they would notice if their heroin contained fentanyl | 30.0 (12) | 54.6 (6) | 20.7 (6) |
| Reaction if Learned Hair was Positive for Fentanyl | % Agreement (n) | % agreement (n) | % Agreement (n) |
| Warn users I know that they may be unknowingly using fentanyl | 82.5 (33) | 81.8 (9) | 82.8 (24) |
| Try to stop using heroin | 75.0 (30) | 72.7 (8) | 75.9 (22) |
| Use heroin more slowly or in smaller amounts | 67.5 (27) | 81.8 (9) | 62.1 (18) |
| Take a small test dose first to see how you react | 67.5 (27) | 72.7 (8) | 65.5 (19) |
| Make sure someone nearby has naloxone to reverse an overdose | 65.0 (26) | 81.8 (9) | 58.6 (17) |
| Find a more trustworthy dealer | 57.5 (23) | 54.6 (6) | 58.6 (17) |
| Use drug test strips that can detect fentanyl | 47.5 (19) | 54.6 (6) | 44.8 (13) |
| Compounds Detected in Hair Sample | % Positive (n) | % Positive (n) | % Positive (n) |
| Fentanyl | 97.5 (39) | 100.0 (11) | 96.6 (28) |
| 4-ANPP | 90.0 (36) | 90.9 (10) | 89.7 (26) |
| Norfentanyl | 90.0 (36) | 90.9 (10) | 89.7 (26) |
| Acetyl-fentanyl | 82.5 (33) | 90.9 (10) | 79.3 (23) |
| Furanyl-fentanyl | 47.5 (19) | 45.5 (5) | 48.3 (14) |
| U-47700 | 7.5 (3) | 18.2 (2) | 3.5 (1) |
p < .01
With regard to how participants felt they would respond if informed their hair tested positive for fentanyl (Table 2), 82.5% reported they would warn other individuals who use heroin about fentanyl adulteration; 75.0% reported they would try to stop using heroin, 67.5% reported they would use heroin more slowly or in smaller amounts; 67.5% reported they would take small tests doses first; 65.0% reported they would ensure that someone nearby has naloxone to reverse a potential overdose, 57.5% reported that they would find a more trustworthy dealer, and 47.5% reported they would use test strips that can detect fentanyl. No significant differences were detected for any of these behavior aspirations between those reporting known fentanyl use and those reporting no known use.
With respect to test results, all but one participant (39 of 40; 97.5%) tested positive for fentanyl. 90.0% also tested positive for 4-ANPP and norfentanyl; 82.5% tested positive for acetyl-fentanyl, 47.5% tested positive for furanyl-fentanyl, and 7.5% tested positive for U-47700. The participant who did not test positive for fentanyl also did not test positive for other compounds tested. Of the 39 patients testing positive, 71.8% were patients who denied known use. Prevalence of detecting positive for each of these compounds was further compared between those reporting known fentanyl use and those reporting no known use (Table 2) and no significant differences were detected. Figure 1a depicts the distributions of number of compounds detected according to whether known fentanyl use was reported and Figure 1b depicts the specific compounds detected for all participants and according to whether known fentanyl use was reported. Only five (12.8%) of those testing positive for fentanyl did not also test positive for at least one analog. Among those testing positive for fentanyl, 38.5% (n=15) tested positive for one analog, 43.6% (n=17) tested positive for two other analogs (with one testing positive for one analog and U-47700), and 5.1% (n=2) tested positive for two analogs and also tested positive for U-47700.
Figure 1a.
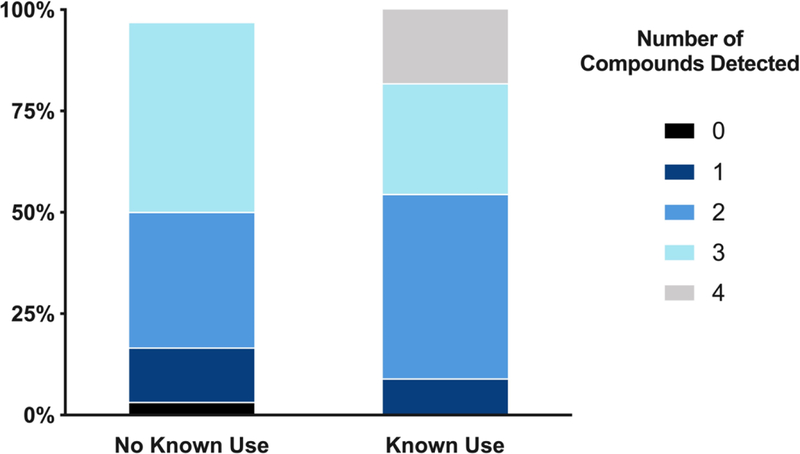
Number of compounds detected according to whether intentional fentanyl use was reported
Figure 1b.
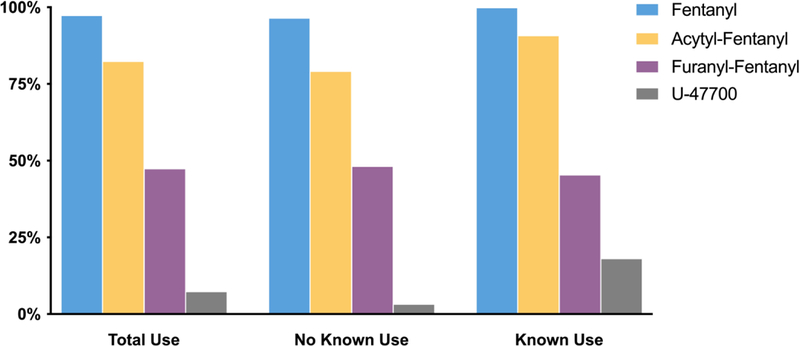
Specific compounds detected in the full sample and according to whether intentional fentanyl use was reported
Table 3 presents concentrations of analogs detected in each patient for descriptive purposes. Fentanyl concentrations were in the range 2.3–8600 pg/mg (mean=860 pg/mg, median=440 pg/mg). Acetylfentanyl concentrations were in the range 2.1–3200 pg/mg (mean=160 pg/mg, median=26 pg/mg). Furanylfentanyl concentrations were in the range 0.7–42 pg/mg (mean=8.0 pg/mg, median=1.6 pg/mg). In three samples, U-47700 was detected at very low levels (1.4–4.5 pg/mg).
Table 3.
Results from hair samples in pg/mg.
| Subject | Detected Analytes | |||||||
|---|---|---|---|---|---|---|---|---|
| Case | Length (cm) | Type of hair | Fentanyl | Acetyl fentanyl | Furanyl fentanyl | U-47700 | 4-ANPP | Norfentanyl |
| 1 | 1.5 | Arm | 800 | 12 | 42 | - | 54 | 60 |
| 2 | 1.5 | Arm | 8600 | 3200 | 1.4 | 1.9 | 1400 | 110 |
| 3 | 5.0 | Head | 480 | 28 | - | - | 70 | 35 |
| 4 | 5.5 | Head | 130 | 50 | - | - | 1.4 | 8.5 |
| 5 | 5.0 | Head | 77 | - | 3.1 | - | 8.9 | 5.0 |
| 6 | 7.0 | Head | 2200 | 26 | 12 | 4.5 | 61 | 199 |
| 7 | 3.0 | Head | 170 | 10 | 0.7 | - | 8.3 | 26 |
| 8 | 5.0 | Head | 23 | 5.9 | - | - | - | - |
| 9 | 2.5 | Leg | 57 | 5.2 | - | - | 2.4 | 3.0 |
| 10 | 1.0 | Beard | 51 | 2.1 | - | - | 9.9 | 10 |
| 11 | 1.0 | Beard | 450 | 3.5 | - | - | 6.3 | 58 |
| 12 | 3.0 | Arm | 650 | 190 | 14 | - | 16 | 16 |
| 13 | 8.0 | Head | 4.3 | - | - | - | - | - |
| 14 | 1.0 | Pubic | 380 | 19 | 2.7 | - | 12 | 30 |
| 15 | 3.0 | Head | 210 | 21 | - | - | 2.7 | 7.1 |
| 16 | 2.0 | Leg | 820 | 30 | 1.3 | - | 13 | 38 |
| 17 | 2.5 | Leg | 450 | 30 | 13 | - | 35 | 21 |
| 18 | 1.0 | Arm | 1400 | 95 | 0.8 | - | 100 | 56 |
| 19 | 4.0 | Head | 340 | 13 | 2.9 | - | 11 | 16 |
| 20 | 10 | Head | 2.3 | - | - | - | - | - |
| 21 | 1.0 | Leg | 520 | 33 | 4.4 | - | 56 | 21 |
| 22 | 3.0 | Chest | 2400 | 25 | - | - | 130 | 110 |
| 23 | 2.0 | Chest | 810 | 120 | 0.7 | - | 37 | 25 |
| 24 | 7.0 | Head | 440 | 67 | 0.8 | - | 5.1 | 20 |
| 25 | 5.0 | Head | 1100 | 3.7 | - | - | 64 | 69 |
| 26 | 1.5 | Chest | 430 | 130 | 0.9 | - | 12 | 15 |
| 27 | 6.0 | Head | 160 | - | - | - | 4.0 | 7.9 |
| 28 | 2.5 | Head | 370 | 7.1 | - | 1.4 | 57 | 32 |
| 29 | 2.0 | Head | 89 | - | - | - | 1.1 | 2.8 |
| 30 | 3.0 | Head | 330 | - | - | - | 3.4 | 18 |
| 31 | 1.0 | Publc | - | - | - | - | - | - |
| 32 | 13.0 | Head | 230 | 7.9 | 12 | - | 4.1 | 15 |
| 33 | 3.0 | Leg | 3000 | 730 | 0.9 | - | 71 | 210 |
| 34 | 1.0 | Arm | 1400 | 25 | 38 | - | 98 | 39 |
| 35 | 3.0 | Head | 1200 | 11 | - | - | 90 | 110 |
| 36 | 2.5 | Head | 290 | 15 | - | - | 3.1 | 10 |
| 37 | 20 | Head | 950 | 150 | 1.6 | - | 5.2 | 130 |
| 38 | 1.0 | Head | 1500 | 160 | - | - | 89 | 95 |
| 39 | 7.0 | Head | 1400 | 41 | - | - | 260 | 110 |
| 40 | 1.5 | Head | 440 | 54 | - | - | 120 | 21 |
| Positive findings | 39 | 33 | 19 | 3 | 36 | 36 | ||
| Mean (among positive) | 880.9 | 161.2 | 8.1 | 2.6 | 81.2 | 48.9 | ||
| Median (among positive) | 440 | 26 | 26 | 1.9 | 14.5 | 25.5 | ||
| Range (among positive) | 2.3–8600 | 2.1–3200 | 2.1–3200 | 1.4–4.5 | 1.1–1400 | 2.8–210 | ||
Discussion
To our knowledge, this is the first study to examine (unknown) exposure to fentanyl in individuals who use heroin via hair testing. Alarmingly, 98% of this sample (71.8% of whom denied known use) tested positive for fentanyl. Likewise, 85% of participants tested positive for one or more fentanyl analog and 7.5% tested positive for the novel synthetic opioid U-47700, suggesting exposure to more than one analog is common. Since hair analysis gives evidence of the cumulated incorporation into the matrix of the substances consumed over an extended period of time, it is difficult to speculate if fentanyl and its analogs were taken alone or simultaneously, and whether one analog (e.g., acetylfentanyl) was present as an impurity of the fentanyl.
Incidence of unknown fentanyl exposure in this study was higher than in recent fentanyl-testing studies. For example, a recent study of a sample of individuals in Canada who use drugs found that three-quarters (75%) of those reporting nonmedical opioid use and denying fentanyl use had their urine test positive for fentanyl (5). In a recent study of inpatients seeking opioid withdrawal management, of those denying known exposure to fentanyl, two-thirds tested positive for fentanyl via urine-testing (10). Similarly, a recent drug-testing study in Canada found that 91% of heroin samples submitted to a testing service tested positive for fentanyl via testing strips (26). Our results suggest that hair testing may prove beneficial in helping detect past exposure to specific compounds. Another benefit of hair testing is that past exposure (e.g., weeks or months prior to testing) can be detected and this information may be more valuable in some contexts in which only recent exposure is detected (e.g., through urine testing).
While over a quarter of participants reported having ever knowingly using fentanyl, large portions of participants reported that they would engage in various behavior changes if learning their hair had tested positive for fentanyl. Trials examining actual behavior changes in response to positive (and negative) results are needed. While more research is in fact needed, results indicate desire of individuals who use heroin to know whether they have been exposed to fentanyl and many report willingness to engage in behavioral change if provided with such results.
This study has limitations. The study focused on a relatively small sample of inpatients in a detoxification program that use heroin so results may not be fully generalizable. The study was underpowered to detect potential differences within such a small sample, but this study was conducted as a pilot to inform larger studies. Longitudinal studies are also needed to assess actual changes in behavior as self-reported intention to engage in a behavior does not necessarily translate into action. Mixed methods research in particular is needed to further investigate risk factors not only for ever being unintentionally exposed to fentanyl, but for exposure to multiple analogs—particularly of analogs that are much more potent and dangerous than fentanyl. Another limitation is that the questions about beliefs and concerns about fentanyl use, and about reactions if learned their hair tested positive, were not previously validated measures. It is also unknown to what extent these individuals already engaged in such harm reduction behaviors. Hair testing typically cannot reliably detect very recent exposure to drugs (e.g., within a few days to a week) as detection depends on rate of hair growth. Shorter hair samples limited our ability to detect less-recent exposure so shorter samples were more likely to lead to false-negatives with regard to exposure detection. Finally, it is possible that other opioids were present in hair samples that were not capable of being tested.
In conclusion, almost all participants in this sample tested positive for fentanyl and many others also tested positive for its analogs. Individuals who use heroin, clinicians, and public health experts alike can benefit from having such information on exposure to these highly potent and dangerous compounds. While hair testing cannot provide immediate results like urine test strips, it can provide clinicians and medical staff with extensive exposure histories of various compounds and this information can inform surveillance, prevention, and harm reduction. Thus, test results can be provided through person-level individual feedback or through relaying such information to overall populations at risk. Results suggest hair testing can provide valuable information to clinicians and epidemiologists in a time of the worsening opioid crisis in the US.
Acknowledgments
Research reported in this publication was supported by the National Institute on Drug Abuse of the National Institutes of Health under Award Number K01DA038800 (PI: Palamar) and K23DA042140 (PI: Tofighi). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Declaration of Interest: The authors declare no conflict of interest.
References
- 1.Jones CM, Einstein EB, Compton WM. Changes in synthetic opioid involvement in drug overdose deaths in the United States, 2010–2016. JAMA 2018;319(17):1819–21. doi: 10.1001/jama.2018.2844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Poklis A Fentanyl: a review for clinical and analytical toxicologists. J Toxicol Clin Toxicol 1995;33:439–47. [DOI] [PubMed] [Google Scholar]
- 3.Suzuki J, El-Haddad S. A review: fentanyl and non-pharmaceutical fentanyls. Drug Alcohol Depend 2017;171:107–16. doi: 10.1016/j.drugalcdep.2016.11.033. [DOI] [PubMed] [Google Scholar]
- 4.Ciccarone D, Ondocsin J, Mars SG. Heroin uncertainties: exploring users’ perceptions of fentanyl-adulterated and -substituted ‘heroin’. Int J Drug Policy 2017;46:146–55. doi: 10.1016/j.drugpo.2017.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jones AA, Jang K, Panenka WJ, Barr AM, MacEwan GW, Thornton AE, Honer WG. Rapid change in fentanyl prevalence in a community-based, high-risk sample. JAMA Psychiatry 2018;75(3):298–300. doi: 10.1001/jamapsychiatry.2017.4432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Krieger MS, Yedinak JL, Buxton JA, Lysyshyn M, Bernstein E, Rich JD, Green TC, Hadland SE, Marshall BDL. High willingness to use rapid fentanyl test strips among young adults who use drugs. Harm Reduct J 2018;15(1):7. doi: 10.1186/s12954-018-0213-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bloomberg American Health Initiative. Fentanyl overdose reduction checking analysis study Johns Hopkins Bloomberg School of Public Health; 2018. [Google Scholar]
- 8.U.S. Drug Enforcement Administration Diversion Control Division. NFLIS brief: fentanyl and fentanyl-related substances reported in NFLIS, 2015–2016 Springfeld, VA: US Drug Enforcement Administration; 2018. [Google Scholar]
- 9.Moore PQ, Weber J, Cina S, Aks S. Syndrome surveillance of fentanyl-laced heroin outbreaks: utilization of EMS, Medical Examiner and Poison Center databases. Am J Emerg Med 2017;35(11):1706–8. doi: 10.1016/j.ajem.2017.05.003. [DOI] [PubMed] [Google Scholar]
- 10.Kenney SR, Anderson BJ, Conti MT, Bailey GL, Stein MD. Expected and actual fentanyl exposure among persons seeking opioid withdrawal management. J Subst Abuse Treat 2018;86:65–9. doi: 10.1016/j.jsat.2018.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Macmadu A, Carroll JJ, Hadland SE, Green TC, Marshall BD. Prevalence and correlates of fentanyl-contaminated heroin exposure among young adults who use prescription opioids non-medically. Addict Behav 2017;68:35–8. doi: 10.1016/j.addbeh.2017.01.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Park JN, Weir BW, Allen ST, Chaulk P, Sherman SG. Fentanyl-contaminated drugs and non-fatal overdose among people who inject drugs in Baltimore, MD. Harm Reduct J 2018;15:34. doi: 10.1186/s12954-018-0240-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carroll JJ, Marshall BDL, Rich JD, Green TC. Exposure to fentanyl-contaminated heroin and overdose risk among illicit opioid users in Rhode Island: A mixed methods study. Int J Drug Policy 2017;46:136–45. doi: 10.1016/j.drugpo.2017.05.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention. Acetyl fentanyl overdose fatalities--Rhode Island, March-May 2013. MMWR Morb Mortal Wkly Rep 2013;62:703–4. [PMC free article] [PubMed] [Google Scholar]
- 15.Griswold MK, Chai PR, Krotulski AJ, Friscia M, Chapman B, Boyer EW, et al. Self-identification of nonpharmaceutical fentanyl exposure following heroin overdose. Clin Toxicol 2018;56:37–42. doi: 10.1080/15563650.2017.1339889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Silverstein JH, Rieders MF, McMullin M, Schulman S, Zahl K. An analysis of the duration of fentanyl and its metabolites in urine and saliva. Anesth Analg 1993;76(3):618–21. [DOI] [PubMed] [Google Scholar]
- 17.Palamar JJ, Salomone A, Vincenti M, Cleland CM. Detection of “bath salts” and other novel psychoactive substances in hair samples of ecstasy/MDMA/”Molly” users. Drug Alcohol Depend 2016;161:200–5. doi: 10.1016/j.drugalcdep.2016.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Palamar JJ, Salomone A, Gerace E, Di Corcia D, Vincenti M, Cleland CM. Hair testing to assess both known and unknown use of drugs amongst ecstasy users in the electronic dance music scene. Int J Drug Policy 2017;48:91–8. doi: 10.1016/j.drugpo.2017.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Salomone A, Palamar JJ, Gerace E, Di Corcia D, Vincenti M. Hair testing for drugs of abuse and new psychoactive substances in a high-risk population. J Anal Toxicol 2017;41(5):376–81. doi: 10.1093/jat/bkx020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Salomone A, Palamar JJ, Bigiarini R, Gerace E, Di Corcia D, Vincenti M. Detection of fentanyl analogs and synthetic opioids in real hair samples. J Anal Toxicol 2018:in press. doi: 10.1093/jat/bky093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mema SC, Sage C, Popoff S, Bridgeman J, Taylor D, Corneil T. Expanding harm reduction to include fentanyl urine testing: results from a pilot in rural British Columbia. Harm Reduct J 2018;15:19. doi: 10.1186/s12954-018-0224-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McKnight C, Des Jarlais DC. Being “hooked up” during a sharp increase in the availability of illicitly manufactured fentanyl: Adaptations of drug using practices among people who use drugs (PWUD) in New York City. Int J Drug Policy 2018;60:82–8. doi: 10.1016/j.drugpo.2018.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moody MT, Diaz S, Shah P, Papsun D, Logan BK. Analysis of fentanyl analogs and novel synthetic opioids in blood, serum/plasma, and urine in forensic casework. Drug Test Anal 2018;10(9):1358–67. doi: 10.1002/dta.2393. [DOI] [PubMed] [Google Scholar]
- 24.U.S. Drug Enforcement Administration. 2017 Emerging Threat Report 2018.
- 25.Kintz P, Salomone A, Vincenti M. Hair analysis in clinical and forensic toxicology San Diego, CA: Academic Press; 2015. [Google Scholar]
- 26.Tupper W, McCrae K, Garber I, Lysyshyn M, Wood E. Initial results of a drug checking pilot program to detect fentanyl adulteration in a Canadian setting. Drug Alcohol Depend 2018;190:242–5. doi: 10.1016/j.drugalcdep.2018.06.020. [DOI] [PubMed] [Google Scholar]


