Abstract
Background:
Sex differences are known to exist in the management of older patients presenting with acute myocardial infarction (AMI). Few studies have examined the incidence and risk factors of AMI among young patients, or whether clinical management differs by sex.
Methods:
The Atherosclerosis Risk in Communities (ARIC) Surveillance study conducts hospital surveillance of AMI in 4 US communities (MD, MN, MS, and NC). AMI was classified by physician review, using a validated algorithm. Medications and procedures were abstracted from the medical record. Our study population was limited to young patients aged 35–54 years.
Results:
From 1995–2014, 28,732 weighted hospitalizations for AMI were sampled among patients aged 35–74. Of these, 8,737 (30%) were young. The annual incidence of AMI hospitalizations increased for young women but decreased for young men. The overall proportion of AMI admissions attributable to young patients steadily increased, from 27% in 1995–1999 to 32% in 2010–2014 (P for trend =0.002), with the largest increase observed in young women. History of hypertension (59% to 73%, P for trend<0.0001) and diabetes mellitus (25% to 35%, P for trend<0.0001) also increased among young AMI patients. Compared to young men, young women presenting with AMI were more often black and had a greater comorbidity burden. In adjusted analyses, young women had a lower probability of receiving lipid-lowering therapies (RR = 0.87; 95% CI: 0.80 – 0.94), non-aspirin antiplatelets (RR = 0.83; 95% CI: 0.75 – 0.91), beta blockers (RR = 0.96; 95% CI: 0.91 – 0.99), coronary angiography (RR = 0.93; 95% CI: 0.86 – 0.99) and coronary revascularization (RR = 0.79; 95% CI: 0.71 – 0.87). However, 1-year all-cause mortality was comparable for women vs. men (HR=1.10; 95% CI: 0.83 – 1.45).
Conclusion:
The proportion of AMI hospitalizations attributable to young patients increased from 1995–2014 and was especially pronounced among women. History of hypertension and diabetes among young patients admitted with AMI increased over time as well. Compared with young men, young women presenting with AMI had a lower likelihood of receiving guideline-based AMI therapies. A better understanding of factors underlying these changes is needed to improve care of young patients with AMI.
Keywords: Acute myocardial infarction, epidemiology, sex differences
Introduction
Although there has been a dramatic decrease in mortality from coronary artery disease over the past four decades in the US, this favorable trend does not appear to extend to young adults, especially younger women (1,2). Similarly, acute myocardial infarction (AMI) hospitalizations among young adults have not declined (2), highlighting the need to investigate AMI in the young, a demographic group often overlooked in cardiovascular research. An increasing prevalence of obesity, cardiometabolic risk factors, and adverse health behaviors have been postulated to contribute to the observed plateau in life expectancy in the US (3,4) and beyond (5). Greater burden of cardiometabolic risk factors may also lead to earlier incidence of AMI at a younger age. Previous investigations from the Atherosclerosis Risk in Communities (ARIC) study have reported a decline in AMI incidence among 35- to 74-year olds from 1987 to 2008 (6). In the present investigation, we examine contemporary trends in the incidence of AMI admissions among young (35–54-year-old) women and men, who were sampled from 21 hospitals by the ARIC Surveillance study from 1995 to 2014. We also examine whether clinical management and mortality differ by sex in young patients with AMI. Although sex differences in AMI management have been well-described in older populations (7,8), it is uncertain whether this trend extends to younger patients presenting with AMI.
Methods
ARIC Study Community Surveillance
The ARIC study’s data and materials are publicly available (9). As previously described (6,10) the ARIC study has conducted community surveillance of hospitalizations for AMI in 4 geographically-defined regions of the US (Forsyth County, North Carolina; Washington County, Maryland; Jackson, Mississippi and 8 northwest suburbs of Minneapolis, Minnesota). All surveillance protocols were approved by local Institutional Review Boards. Informed consent was not required, because data were anonymized by redacting personal identifiers. Community residents aged 35–74 years were considered eligible for surveillance in 1987–2004, with eligibility expanded to 35–84 years from 2005–2014. Hospitalizations were randomly sampled among strata based on race, sex, ARIC community, and International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) discharge codes: 402, 410–414, 427, 428 and 518.4. The underlying population size of residents within the 4 ARIC Communities was interpolated and extrapolated from the US Census population estimates, as previously described (6). For the purposes of this analysis, we considered patients 35–54 years to be “young”, a cutpoint consistent with prior studies (2) and representative of the lower half of the original age distribution sampled in ARIC. Importantly, hospitalizations were not sampled within any particular strata of age, provided that cases were 35–74 in 1987–2004, and 35–84 in 2005–2014. Our analysis was limited to young patients (35–54 years old), with the proportion of AMI hospitalizations attributable to young patients estimated from the total sample of AMI patients aged 35–74 years. We excluded patients 75–85 years of age as this age group was only sampled between years 2005 to 2014.
Clinical Covariates and Demographic Data
Clinical and demographic data were collected from the hospital record by trained abstractors, using physician notes, laboratory reports, patient histories, and discharge summaries. Diabetes mellitus was defined by documented history of diabetes mellitus or glucose-lowering therapy use. Hypertension was defined by documented hypertension in the medical record.
Electrocardiography
The first, third, and the last 12-lead electrocardiograms (ECG) over the course of hospitalization were obtained from the medical record and coded electronically at the Minneapolis ECG Reading Center (11).
Chest Pain
Presence of chest pain was abstracted from the medical record, with origin determined by review of physician notes. Any mention of substernal pressure, tightness, or pain precipitated by exertion or excitement was considered evidence of chest pain of cardiac origin. Chest pain specified in the physician notes as “unknown origin” or “undiagnosed” was considered “unknown.”
Acute Myocardial Infarction Classification
As previously described (10,11), events were classified by the ARIC study as definite, probable, suspected, or no MI, based on ECG evidence (evolving diagnostic, diagnostic, evolving ST-segment/T-wave changes, equivocal, or absent/uncodable), presence of chest pain, and cardiac biomarkers (which were considered “abnormal” if ≥2x the upper limit of normal (ULN), and “equivocal” if exceeding the ULN but <2x the ULN) (6). Classification criteria remained constant over the study period and are detailed in the ARIC Study surveillance manual (12). Classification of an event as definite or probable AMI required the presence of at least one of the following: 1) evolving diagnostic ECG pattern 2) diagnostic ECG pattern and abnormal biomarkers, 3) cardiac pain and abnormal biomarkers, 4) cardiac pain and equivocal biomarkers with evolving ST-segment/T-wave pattern or diagnostic ECG pattern, or 5) abnormal biomarkers with evolving ST-segment/T-wave pattern.
Biomarkers
Laboratory values for biomarkers of cardiac injury were recorded for the first 4 days of hospitalization. The laboratory-specified ULN was recorded, and biomarker values were abstracted chronologically, recording up to 3 measurements per day.
Medical Therapies
Medications were recorded if administered during hospitalization or prescribed at hospital discharge. Aspirin required routine rather than pro re nata administration for abstraction. Non-aspirin antiplatelet therapy was recorded as a single category and included P2Y12 inhibitors (cangrelor, clopidogrel, prasugrel, ticagrelor, ticlopidine), glycoprotein IIb/IIIa inhibitors (abciximab, eptifibatide, tirofiban), phosphodiesterase 3 inhibitors (cilostazol), phosphodiesterase 5 inhibitors (dipyridamole), and protease-activated receptor-1 antagonists (vorapaxar). Beta blockers included β1 adrenergic antagonists. Angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers (ACEi/ARB) were recorded as a single category. Lipid-lowering agents included statins, niacin, and fibrates.
Procedures
Echocardiography, stress testing, angiography and revascularization procedures were abstracted from the medical record. Echocardiography included transthoracic and transesophageal echocardiograms. Stress testing included exercise testing (treadmill or bicycle ergometer), stress echocardiography, cardiac stress magnetic resonance imaging, and nuclear stress tests. Revascularization included percutaneous coronary intervention or coronary artery bypass graft surgery.
Mortality Outcomes
In-hospital, 28-day, and 1-year mortality were ascertained by the ARIC Study, which linked hospitalizations with the National Death Index. Cardiovascular death was defined by death due to “diseases of the circulatory system” (ICD-9 codes 390–459 and ICD-10 codes I00-I99).
Statistical Analysis
All statistical analyses were carried out using SAS 9.4 (SAS Institute; Cary, NC). Statistical tests and models accounted for the stratified sampling design and were weighted by the inverse of the sampling probability (13). Continuous variables were assessed for normality and compared using the difference in least square means from weighted linear regression. Categorical variables were compared using Rao-Scott χ2 tests. The annual incidence of AMI hospitalizations among young patients was calculated by dividing the weighted number of sampled AMI hospitalizations by the total number of ARIC residents aged 35–54 years. Although the ARIC study expanded the sampling to include patients aged 75–84 from 2005–2014, we analyzed the percentage of young community residents relative to the total population of 35–74-year-old residents of the ARIC communities. Similarly, the proportion of AMI hospitalizations attributable to young patients was examined among 35–74-year-old patients admitted with AMI across all years of observation. Trends over time were visually plotted and analyzed across 5-year intervals (1995–1999, 2000–2004, 2005–2009, 2010–2014) using logistic regression, with year categories regressed as an ordinal variable. Trends in the prevalence of cardiovascular risk factors were limited to comorbidities routinely abstracted across all study periods.
Among young patients, the relative probabilities of women vs. men receiving guideline-directed AMI medications (aspirin, other antiplatelets, beta blockers, and lipid-lowering medications) or undergoing invasive procedures (angiography and revascularization) were compared in 5-year intervals and in the aggregate. Associations were derived from multivariable logistic regression, with odds ratios converted into relative risks (RR) and 95% confidence intervals (CI) (14). Models were adjusted for race, geographic region, and year of admission. As sensitivity analyses, we also stratified the models by race, limited the population to patients with first-occurring AMI, and additionally adjusted for comorbidities and complications (diabetes mellitus, acute heart failure / pulmonary edema, ventricular fibrillation, cardiac arrest, and cardiogenic shock). One-year all-cause mortality was compared between young women and men using multivariable Cox regression, adjusted for race, geographic location, and year of admission.
Results
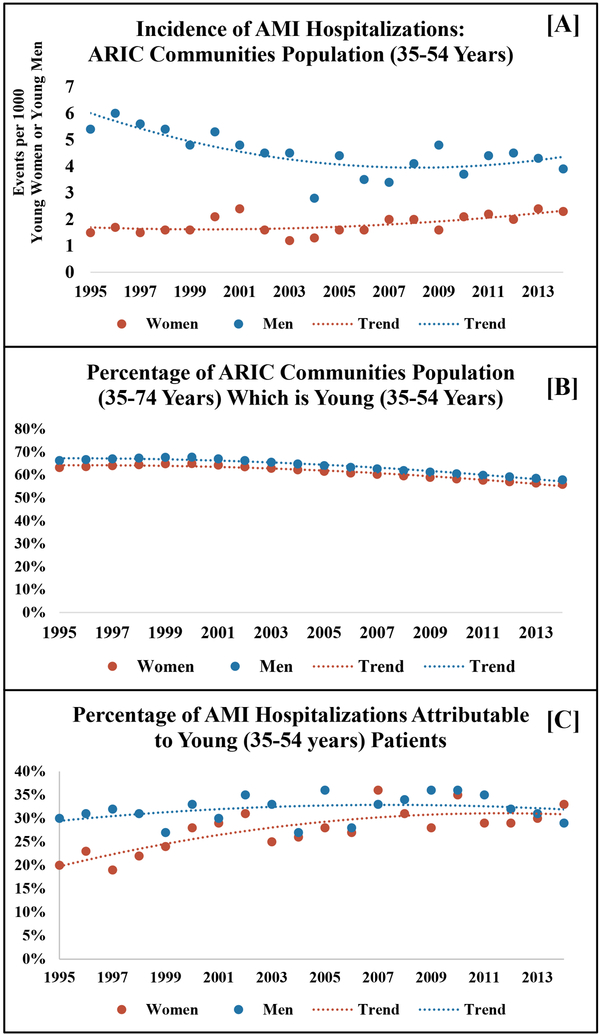
The annual incidence of AMI hospitalizations decreased from 1995 to 2014 among male ARIC community residents aged 35–54. In contrast, a declining incidence of AMI hospitalizations was not observed for women aged 35–54 (Figure 1a.). Evidence of population aging was noted for both sexes, with the percentage of ARIC community residents aged 35–54 declining over time relative to the entire population of 35–74-year-old residents (Figure 1b.). However, the annual proportion of AMI admissions attributable to young patients steadily increased over time, with the largest increase observed in women (Figure 1c.). When analyzed across 5-year intervals (1995–1999, 2000–2004, 2005–2009, and 2010–2014), the proportion of AMI admissions attributable to young patients significantly increased, from 27% to 32%; P for trend<0.0001 (21% to 31% among women [P for trend <0.0001] and 30% to 33% among men [P for trend = 0.1]. Stratified trends among black women, white women, black men, and white men are shown in Table 1.
Figure 1:
Temporal trends in the incidence of acute myocardial infarction among residents of the ARIC communities who are young (35–54 years), [Panel A]; the percentage of total ARIC communities residents (35–74 years) who are young (35–54 years), [Panel B]; and the percentage of 35–74-year-old patients admitted with acute myocardial infarction who are young (35–54 years), [Panel C]. The Atherosclerosis Risk in Communities Surveillance Study, 1995–2014.
Table 1:
Proportion of patients admitted with acute myocardial infarction who are young (35–54 years), relative to the entire demographic subgroup sample of 35–74-year-old patients presenting with acute myocardial infarction. The Atherosclerosis Risk in Communities Surveillance Study, 1995–2014.
| AMI | 1995–1999 | 2000–2004 | 2005–2009 | 2010–2014 | 20-Year | ||||
|---|---|---|---|---|---|---|---|---|---|
| Total | Proportion | Total | Proportion | Total | Proportion | Total | Proportion | Trend | |
| Sampled | Young | Sampled | Young | Sampled | Young | Sampled | Young | P-value | |
| All | 7605 | 2073 (27%) | 6398 | 1941 (30%) | 6563 | 2118 (32%) | 8166 | 2605 (32%) | 0.002 |
| Women | 2548 | 546 (21%) | 2219 | 622 (28%) | 2398 | 722 (30%) | 3209 | 993 (31%) | <0.0001 |
| Men | 5056 | 1527 (30%) | 4179 | 1319 (32%) | 4166 | 1396 (34%) | 4956 | 1612 (33%) | 0.1 |
| Black Women | 769 | 248 (32%) | 776 | 292 (38%) | 935 | 368 (39%) | 1582 | 605 (38%) | 0.2 |
| White Women | 1779 | 298 (17%) | 1443 | 330 (23%) | 1462 | 355 (24%) | 1627 | 388 (24%) | 0.003 |
| Black Men | 1024 | 454 (44%) | 1072 | 478 (45%) | 1273 | 615 (48%) | 2114 | 825 (39%) | 0.1 |
| White Men | 4033 | 1072 (27%) | 3107 | 841 (27%) | 2893 | 781 (27%) | 2842 | 787 (28%) | 0.6 |
From 1995–2014, medical records from 28,732 weighted AMI hospitalizations (15,081 unweighted) were abstracted from sampled patients aged 35–74. Of these, 8,737 (30%) were young, constituting our study population (Table 2). Compared with young men, young women were more often black (52% vs. 41%), and more likely to have medical insurance (85% vs. 78%), history of hypertension (71% vs. 64%), diabetes mellitus (39% vs. 26%), chronic kidney disease (24% vs. 19%), and prior stroke (10% vs. 6%), when aggregated across 1995–2014. However, young women were less likely to be smokers (48% vs. 57%). During the hospital visit, acute pulmonary edema / heart failure was more frequent among women (28% vs. 22%). On the other hand, young women were less likely to have ST-segment elevation myocardial infarction (STEMI) compared with their male counterparts (16% vs. 26%).
Table 2:
Demographics and clinical characteristics of young patients (35–54 years) admitted with acute myocardial infarction. The Atherosclerosis Risk in Communities Surveillance Study, 1995–2014.
| Women | Men | ||
|---|---|---|---|
| Characteristic | N=2884 | N=5853 | P-value |
| Demographics | |||
| Age (mean ± SE) | 48 ± 0.2 | 48 ± 0.1 | 0.2 |
| Black | 1513 (52%) | 2372 (41%) | <0.0001 |
| Heath insurance* | 1449 (85%) | 2342 (78%) | 0.003 |
| Medical History | |||
| Smoking | 1348 (48%) | 3276 (57%) | <0.0001 |
| Hypertension | 2023 (71%) | 3715 (64%) | 0.0005 |
| Diabetes mellitus | 1110 (39%) | 1534 (26%) | <0.0001 |
| Chronic kidney disease† | 433 (24%) | 612 (19%) | 0.07 |
| Prior revascularization | 642 (22%) | 1418 (24%) | 0.3 |
| Prior myocardial infarction | 750 (26%) | 1588 (28%) | 0.5 |
| Stroke | 280 (10%) | 338 (6%) | 0.0003 |
| Hospital Visit | |||
| ST-segment elevation‡ | 420 (16%) | 1368 (26%) | <0.0001 |
| Acute heart failure / pulmonary edema | 797 (28%) | 1289 (22%) | 0.004 |
| Cardiogenic Shock | 82 (3%) | 120 (2%) | 0.2 |
| Ventricular fibrillation / cardiac arrest | 203 (7%) | 316 (5%) | 0.09 |
Health insurance status not routinely abstracted prior to 2005, and available for 4699 patients
Serum creatinine not routinely abstracted prior to 2005, and available for 3719 patients. Chronic kidney disease defined by estimated glomerular filtration rate <45 mL/min/1.73 m2 using Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) formula, or receipt of hemodialysis.
Classifications of ST-segment elevated myocardial infarction vs. non-ST-segment elevation myocardial infarction available in a subset of patients (n=7844) with sufficient electrocardiographic data.
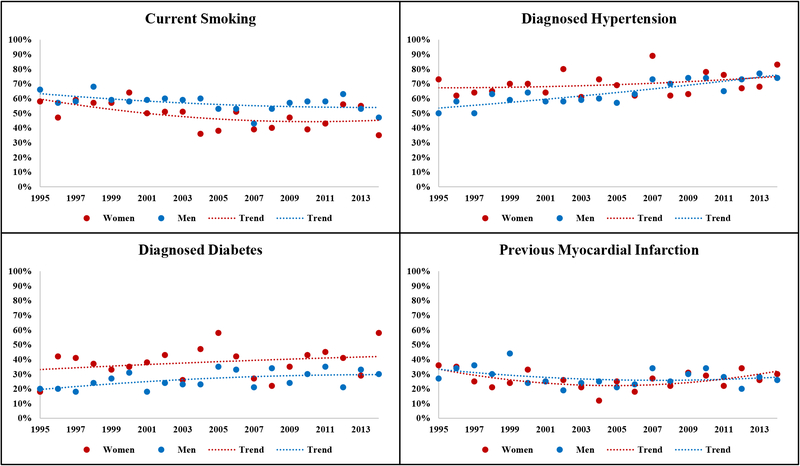
Among young women and men admitted with AMI, the annual prevalence of smoking steadily decreased, while the prevalence of hypertension and diabetes increased (Figure 2). History of previous AMI remained stable over time. When examined across 5-year intervals, the overall prevalence of hypertension significantly increased (59% to 73%, P for trend <0.0001) as did prevalence of diabetes mellitus (25% to 35%, P for trend <0.0001). On the other hand, prevalence of smoking significantly decreased (60% to 52%, P for trend =0.0002) and history of prior AMI remained comparable (32% to 27%, P for trend=0.1), Table 3.
Figure 2:
Prevalence and temporal trends in cardiovascular risk factors among young (35–54 years) women and men presenting with acute myocardial infarction. The Atherosclerosis Risk in Communities Surveillance Study, 1995–2014.
Table 3:
Prevalence and temporal trends in cardiovascular risk factors among young (35–54-year-old) patients presenting with acute myocardial infarction. The Atherosclerosis Risk in Communities Surveillance Study, 1995–2014.
| 1995–1999 | 2000–2004 | 2005–2009 | 2010–2014 | Trend | |
|---|---|---|---|---|---|
| Entire Sample | N=2073 | N=1941 | N=2118 | N=2605 | P-value |
| Smoking | 1188 (60%) | 1085 (57%) | 1023 (49%) | 1329 (52%) | 0.0002 |
| Hypertension | 1178 (59%) | 1221 (63%) | 1432 (68%) | 1906 (73%) | <0.0001 |
| Diabetes | 516 (25%) | 552 (28%) | 666 (31%) | 910 (35%) | <0.0001 |
| Prior MI | 641 (32%) | 457 (24%) | 537 (26%) | 703 (27%) | 0.1 |
| Women | N=546 | N=622 | N=722 | N=993 | |
| Smoking | 282 (56%) | 310 (51%) | 306 (43%) | 449 (46%) | 0.01 |
| Hypertension | 352 (66%) | 432 (70%) | 500 (70%) | 740 (75%) | 0.05 |
| Diabetes | 186 (34%) | 237 (38%) | 257 (36%) | 429 (36%) | 0.07 |
| Prior MI | 149 (28%) | 151 (24%) | 174 (25%) | 276 (28%) | 0.8 |
| Men | N=1527 | N=1319 | N=1396 | N=1612 | |
| Smoking | 906 (62%) | 774 (59%) | 716 (52%) | 880 (56%) | 0.02 |
| Hypertension | 827 (56%) | 789 (60%) | 932 (68%) | 932 (68%) | <0.0001 |
| Diabetes | 330 (22%) | 315 (24%) | 409 (29%) | 481 (30%) | 0.001 |
| Prior MI | 492 (34%) | 306 (23%) | 363 (27%) | 427 (27%) | 0.06 |
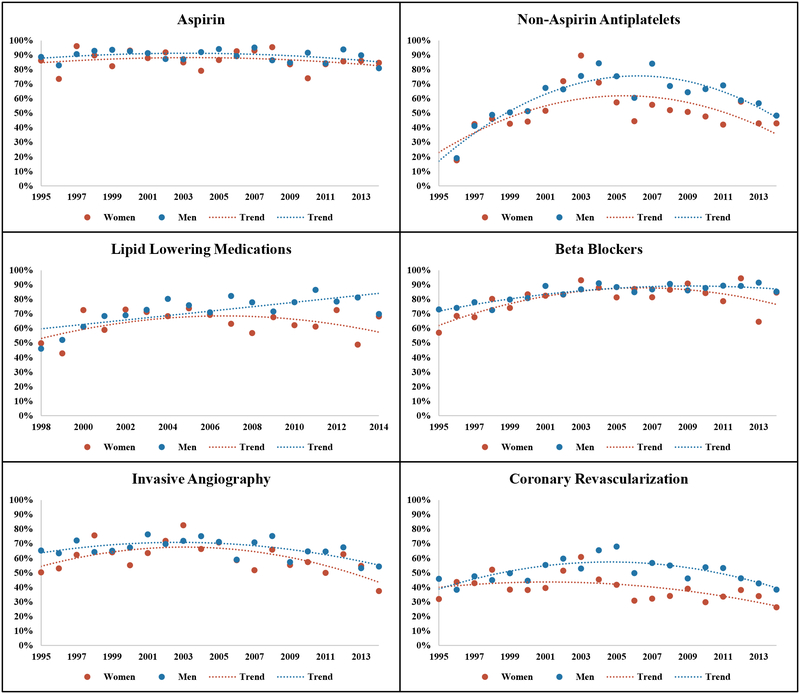
Compared with young men, at the time of hospitalization, young women were less likely to be administered lipid-lowering medications (63% vs. 72%; P <0.0001), non-aspirin antiplatelet therapy (51% vs. 62%; P<0.0001), beta blockers (81% vs. 84%; =0.04), or ACEi/ARBs (59% vs. 64%; P=0.02); and less often underwent invasive coronary angiography (59% vs. 66%; P=0.0009) or revascularization (38% vs. 50%; P<0.0001). However, women were more likely to be imaged by echocardiography (58% vs. 53%; P=0.008). Aspirin administration (86% vs. 89%; P=0.09); and non-invasive stress testing (7% vs. 8%; P=0.6) did not differ by sex. Annual trends in the administration of therapies for young women and men presenting with AMI are shown in Figure 3.
Figure 3:
Annual trends* in administration of guideline-directed therapies among young (35–54 years) women and men presenting with acute myocardial infarction. The Atherosclerosis Risk in Communities Surveillance Study, 1995–2014.
*Footnote: Non-aspirin antiplatelets not routinely abstracted prior to 1996. Lipid lowering agents not routinely abstracted prior to 1998
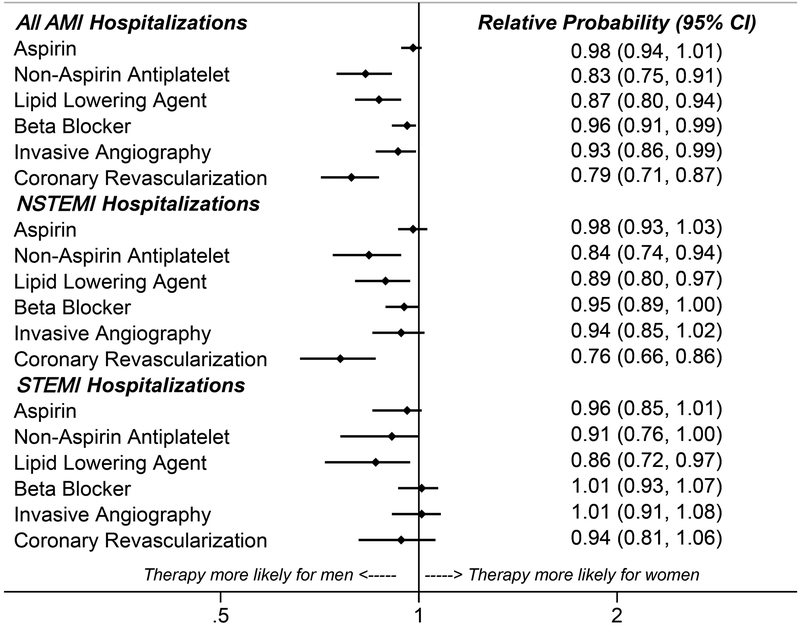
When aggregated across 1995 – 2014 and adjusted for race, ARIC center, and year of admission, women had a 13% lower probability of receiving lipid-lowering agents (RR = 0.87; 95% CI: 0.80 – 0.94), 17% lower probability of receiving non-aspirin antiplatelets (RR = 0.83; 95% CI: 0.75 – 0.91), 7% lower probability of receiving angiography (RR = 0.93; 95% CI: 0.86 – 0.99), and 21% lower probability of receiving revascularization (RR = 0.79; 95% CI: 0.71 – 0.87). The adjusted probabilities of aspirin administration (RR = 0.98; 95% CI: 0.94 – 1.01) and receipt of beta blockers (RR = 0.96; 95% CI: 0.91 – 0.99) were comparable. As shown in Figure 4, lower utilization of non-aspirin antiplatelets and lipid-lowering agents persisted for women relative to men, irrespective of non-ST-segment elevation myocardial infarction (NSTEMI) or STEMI classification. However, the overall sample of patients classified with STEMI was small (n=1,788). Adjusted probabilities of guideline-directed AMI therapies were consistently lower for young women compared to young men when stratified by race, when limiting the population to patients with first-time AMI, or with additional adjustment for clinical course and comorbidities (Supplemental Tables 1–3).
Figure 4:
Relative probabilities* of young women vs. young men receiving guideline-directed therapies for acute myocardial infarction. The Atherosclerosis Risk in Communities Surveillance study, 1995–2014.
Footnote: Models adjusted for race, geographic location (Forsyth County, NC; Jackson, MS; Minneapolis, MN; or Washington County, MD), and year of hospital admission).
When grouped into 5-year intervals, emerging sex differences were observed for receipt of lipid-lowering agents and coronary revascularization (Table 4); probabilities of receiving other guideline-directed therapies changed little over time between the 2 sexes.
Table 4:
Relative probabilities of guideline-directed therapies, comparing young (34–54-year-old) women and men presenting with acute myocardial infarction. The Atherosclerosis Risk in Communities Surveillance Study, 1995–2014.
| Women vs. Men (ref.): Relative Probabilities* | Trend‡ | ||||
|---|---|---|---|---|---|
| Therapy | 1995–1999 | 2000–2004 | 2005–2009 | 2010–2014 | P-value |
| Aspirin | 0.96 (0.86 – 1.02) | 0.98 (0.90 – 1.04) | 1.02 (0.93 – 1.06) | 0.96 (0.86 – 1.03) | 0.8 |
| Non-Aspirin Antiplatelet† | --- | 0.95 (0.83 – 1.06) | 0.75 (0.61 – 0.89) | 0.79 (0.65 – 0.94) | 0.3 |
| Lipid Lowering Agent† | --- | 1.01 (0.89 – 1.11) | 0.86 (0.72 – 0.98) | 0.80 (0.67 – 0.91) | 0.005 |
| Beta Blocker | 0.94 (0.83 – 1.04) | 1.00 (0.92 – 1.06) | 0.98 (0.89 – 1.04) | 0.92 (0.81 – 0.99) | 0.2 |
| Invasive Angiography | 0.94 (0.82 – 1.06) | 0.95 (0.84 – 1.06) | 0.91 (0.76 – 1.05) | 0.88 (0.73 – 1.03) | 0.3 |
| Revascularization | 0.97 (0.81 – 1.14) | 0.88 (0.74 – 1.02) | 0.63 (0.49 – 0.79) | 0.72 (0.56 – 0.88) | 0.002 |
Models adjusted for race (black or white), geographic location (Forsyth County, NC; Jackson, MS; Minneapolis, MN; or Washington County, MD), and year of hospital admission.
Non-aspirin antiplatelets not routinely abstracted prior to 1996. Lipid lowering agents not routinely abstracted prior to 1998.
Management trends over time assessed by testing the multiplicative interaction between sex and time, adjusted for race, geographic location, and year of admission
Among these young AMI patients, the overall all-cause mortality was modest and similar between women and men (1% vs. 2% for in-hospital, 4% each for 28-day, and 9% vs. 7% for 1-year). Annual trends in all-cause mortality are shown in Supplemental Figure 1. Cardiovascular mortality was also similar between women and men (1% each for in-hospital, 2% each for 28-day), but marginally higher for women by 1 year of follow up (5% vs. 3%; p=0.08). After adjustment for race, hospital geographic location, and year of admission, the hazard of 1-year all-cause mortality was comparable for women vs. men (HR = 1.10; 95% CI: 0.83 – 1.45).
Discussion
In this community-based surveillance of patients hospitalized with AMI, we observed a significant increase in patients presenting with AMI who were <55 years of age from 1995 to 2014. This trend parallels an increase in cardiovascular risk factors, including hypertension and diabetes mellitus, in this population. However, the increasing proportion of AMI attributable to young patients was most pronounced among women. Relative to young men, young women had a higher comorbidity burden, and a lesser likelihood of undergoing an invasive strategy or being managed with guideline-based ACS medications.
Previous studies in the U.S. have investigated hospitalizations among young patients using administrative claims records (2). In contrast, the ARIC Surveillance study classifies AMI by standardized physician review of the medical record, providing a more comprehensive event classification and allowing an analysis of trends spanning several decades. The increase in AMI hospitalizations attributable to young patients is staggering in the background of the aging general US population (15). Ideally, prevention of atherosclerotic cardiovascular disease should begin early in adolescence and young adulthood; however, few tools exist to assess the risk of coronary disease in these age groups (16). This likely results in decreased recognition of risk factors in young adults and suboptimal utilization of preventive strategies. An analysis from the Partners YOUNG-MI registry reported a low proportion (12.5%) of young adult patients on statins at the time of AMI; the authors advocate for improved risk assessment tools in this age group (17). Similarly, in the Variation in Recovery: Role of Gender on Outcomes of Young AMI Patients (VIRGO) study, only half of young AMI patients believed they were at risk for heart disease prior their event, despite a high overall prevalence of cardiac risk factors (18,19).
While the proportion of young AMI hospitalizations remained fairly stable across 1995–2014 among men, AMI hospitalizations attributable to young patients steadily increased among women, becoming comparable to that of young men in more recent years. Our observations complement Canadian registries reporting an increase in AMI hospitalizations among women (20). The reasons for the rise in AMI hospitalizations among young women is likely multifactorial but may be related to modifiable risk factors. In the ARIC Community Surveillance study, young women presenting with AMI had more comorbidities and traditional risk factors than their male counterparts with AMI. This may be reflective of trends in the general non-hospitalized population. In an analysis from the National Health and Nutritional Examination Survey comparing 1988–1994 and 1999–2004, the mean Framingham coronary risk score improved for men while it worsened for women, narrowing the gap in cardiovascular risk between sexes (21). We also noted that young women were more likely to be insured, which may have influenced care-seeking behavior and AMI hospitalizations (22).
Clinical improvement in AMI management is an important priority for the Centers for Medicare and Medicaid Services (CMS) Inpatient Quality Reporting program (23). Quality improvement initiatives have led to better outcomes for patients with AMI, irrespective of sex (23). In this analysis from the ARIC Community Surveillance, young women presenting with AMI had a higher comorbidity burden and were less likely to undergo angiography or be managed by guideline-based ACS medications. These observations are consistent with the VIRGO Study, which reported greater prevalence of diabetes mellitus, heart failure, chronic obstructive pulmonary disease, chronic kidney disease, and morbid obesity among women compared with men (18,19). An association between higher comorbidity burden and lower likelihood of angiography or evidence-based care has been reported in older patients presenting with AMI (24,25). Whether these associations extend to young adults with a lower likelihood of frailty is uncertain. It is possible that a greater proportion of women presented with type 2 myocardial infarction, given their greater comorbidity burden and decreased rates of revascularization. Although sex differences in management of AMI based are well known in older adults (7,8), few studies to date have demonstrated sex-specific differences in management of AMI among young patients (26,27).
Although the Centers for Medicare and Medicaid Services Inpatient Quality Improvement Program has focused on improving management and outcomes of patients with AMI, few initiatives have focused on improving cardiometabolic risk profiles, particularly for women (1). Traditionally misconceived as a “man’s disease”, recognition of cardiovascular risk in female patients is lower than for male patients with similar risk profiles (28). However, atherosclerotic cardiovascular disease is the leading cause of death in women (1). Moreover, there are several non-traditional cardiac risk factors unique to women, such as gestational diabetes mellitus, preeclampsia, eclampsia, and early menopause or menarche (29,30). Social determinants of health such as psychosocial stressors and poverty, both with higher prevalence in women, are also associated with increased cardiovascular risk (28,31).
We believe an integrated, multifaceted approach is needed to promote effective primordial, primary, and secondary prevention strategies among at-risk women. To understand further the distinct cardiovascular risk profile and to define treatment pathways in women, clinical trials could be designed specifically for women. Guidelines focused on preventing cardiovascular diseases in women should continue to be updated and implemented in practice, to assist clinicians in clinical decision-making (32). Expanding initiatives such as the American Heart Association Go Red for Women campaign to increase awareness about cardiovascular disease risk in women through media and other outlets should also be encouraged.
Our study has some limitations. The ARIC Community Surveillance Study is localized to 4 US communities and may not be generalizable to the entire nation. Clinical data were limited by availability in the medical record and abstraction priority. Temporal changes in diagnostic testing and documentation may have influenced trends in risk factors over time. We were unable to evaluate trends in obesity, but the prevalence of diabetes mellitus significantly increased from 1995–2014; associations between diabetes mellitus and obesity are well-established (33,34). Substance use, such as cocaine and marijuana, was not abstracted from the medical record but is a known risk factor that is prevalent among young patients presenting with AMI (35). Mortality in this young population was modest, limiting the statistical power of comparisons between women and men. Other clinically-relevant endpoints, such as hospital readmissions or major adverse cardiovascular events, may prove to differ by sex for young patients with AMI; however, these outcomes were not available for analysis. Finally, specific troponin assays and their associated sensitivities varied across hospital systems and over time, potentially influencing trends in AMI detection. Our study also has several noteworthy strengths. The ARIC Study provides a large, multi-year surveillance of 4 diverse US communities, allowing an analysis of contemporary trends spanning several decades. Clinical and laboratory values were meticulously collected by certified abstractors following standardized protocols. AMI was classified and adjudicated by physician review of the medical records, and mortality outcomes verified by the National Death Index.
Conclusion
Young patients presenting with AMI are becoming increasingly common, have high prevalence of cardiometabolic comorbidities, and face 1-year mortality rates that approach 10%. Relative to young men, young women presenting with AMI have a higher comorbidity burden and a lower likelihood of undergoing an invasive strategy or receiving guideline-based AMI therapies. These observations from the ARIC Community Surveillance study have important health implications considering the increased disability-adjusted life years associated with AMI at a younger age. There is an enduring need for effective preventive strategies to reduce the burden of cardiovascular disease in the young population, especially among young women. Ongoing primordial, primary, and secondary prevention efforts are urgently needed to promote uniform and guideline-based care targeting AMI, associated cardiometabolic comorbidities, and adverse health behaviors in the young population.
Supplementary Material
Clinical Perspectives.
What is new?
In this community-based surveillance spanning 2 decades, the proportion of AMI hospitalizations attributable to young patients increased and was most pronounced among women.
This trend parallels an increase in cardiovascular risk factors, including hypertension and diabetes mellitus, among young patients hospitalized with AMI.
Relative to young men, young women had a higher comorbidity burden, and a lesser likelihood of undergoing an invasive strategy or being managed with guideline-based ACS medications.
What are the clinical implications?
An integrated, multifaceted approach is needed to promote effective primordial, primary, and secondary prevention strategies among at-risk women
Clinical trials designed specifically for women are required to understand further the distinct cardiovascular risk profile and to define treatment pathways in women.
Expanding initiatives such as the American Heart Association Go Red for Women campaign to increase awareness about cardiovascular disease risk in women through media and other outlets should also be encouraged
Acknowledgments
The authors thank the staff and participants of the ARIC study for their important contributions.
Funding
The Atherosclerosis Risk in Communities Study is carried out as a collaborative study supported by National Heart, Lung, and Blood Institute contracts (HHSN268201700001I, HHSN268201700002I, HHSN268201700003I, HHSN268201700004I, HHSN268201700005I).
Footnotes
Disclosures: Dr. Arman Qamar is supported by the NHLBI T32 postdoctoral training grant (T32HL007604). Dr. Muthiah Vaduganathan is supported by the KL2/Catalyst Medical Research Investigator Training award from Harvard Catalyst | The Harvard Clinical and Translational Science Center (National Center for Advancing Translational Sciences, National Institutes of Health Award KL2 TR002542), and serves on advisory boards for Bayer AG and Baxter Healthcare. Dr. Deepak L. Bhatt discloses the following relationships - Advisory Board: Cardax, Elsevier Practice Update Cardiology, Medscape Cardiology, Regado Biosciences; Board of Directors: Boston VA Research Institute, Society of Cardiovascular Patient Care, TobeSoft; Chair: American Heart Association Quality Oversight Committee; Data Monitoring Committees: Baim Institute for Clinical Research (formerly Harvard Clinical Research Institute, for the PORTICO trial, funded by St. Jude Medical, now Abbott), Cleveland Clinic, Duke Clinical Research Institute, Mayo Clinic, Mount Sinai School of Medicine (for the ENVISAGE trial, funded by Daiichi Sankyo), Population Health Research Institute; Honoraria: American College of Cardiology (Senior Associate Editor, Clinical Trials and News, ACC.org; Vice-Chair, ACC Accreditation Committee), Baim Institute for Clinical Research (formerly Harvard Clinical Research Institute; RE-DUAL PCI clinical trial steering committee funded by Boehringer Ingelheim), Belvoir Publications (Editor in Chief, Harvard Heart Letter), Duke Clinical Research Institute (clinical trial steering committees), HMP Global (Editor in Chief, Journal of Invasive Cardiology), Journal of the American College of Cardiology (Guest Editor; Associate Editor), Population Health Research Institute (for the COMPASS operations committee, publications committee, steering committee, and USA national co-leader, funded by Bayer), Slack Publications (Chief Medical Editor, Cardiology Today’s Intervention), Society of Cardiovascular Patient Care (Secretary/Treasurer), WebMD (CME steering committees); Other: Clinical Cardiology (Deputy Editor), NCDR-ACTION Registry Steering Committee (Chair), VA CART Research and Publications Committee (Chair); Research Funding: Abbott, Amarin, Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Chiesi, Eisai, Ethicon, Forest Laboratories, Idorsia, Ironwood, Ischemix, Lilly, Medtronic, PhaseBio, Pfizer, Regeneron, Roche, Sanofi Aventis, Synaptic, The Medicines Company; Royalties: Elsevier (Editor, Cardiovascular Intervention: A Companion to Braunwald’s Heart Disease); Site Co-Investigator: Biotronik, Boston Scientific, St. Jude Medical (now Abbott), Svelte; Trustee: American College of Cardiology; Unfunded Research: FlowCo, Merck, Novo Nordisk, PLx Pharma, Takeda. The other authors have no relevant conflicts of interest to disclose.
Bibliography
- 1.Wilmot KA, O’Flaherty M, Capewell S, Ford ES and Vaccarino V. Coronary Heart Disease Mortality Declines in the United States From 1979 Through 2011: Evidence for Stagnation in Young Adults, Especially Women. Circulation. 2015;132:997–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gupta A, Wang Y, Spertus JA, Geda M, Lorenze N, Nkonde-Price C, D’Onofrio G, Lichtman JH and Krumholz HM. Trends in acute myocardial infarction in young patients and differences by sex and race, 2001 to 2010. J Am Coll Cardiol. 2014;64:337–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Olshansky SJ, Passaro DJ, Hershow RC, Layden J, Carnes BA, Brody J, Hayflick L, Butler RN, Allison DB and Ludwig DS. A potential decline in life expectancy in the United States in the 21st century. N Engl J Med. 2005;352:1138–45. [DOI] [PubMed] [Google Scholar]
- 4.Bilal U and Diez-Roux AV. Troubling Trends in Health Disparities. N Engl J Med. 2018;378:1557–1558. [DOI] [PubMed] [Google Scholar]
- 5.Izadnegahdar M, Singer J, Lee MK, Gao M, Thompson CR, Kopec J, Humphries KH. Do younger women fare worse? Sex differences in acute myocardial infarction hospitalization and early mortality rates over ten years. J Womens Health (Larchmt). 2014;23:10–17. [DOI] [PubMed] [Google Scholar]
- 6.Rosamond WD, Chambless LE, Heiss G, Mosley TH, Coresh J, Whitsel E, Wagenknecht L, Ni H, Folsom AR. Twenty-two-year trends in incidence of myocardial infarction, coronary heart disease mortality, and case fatality in 4 US communities, 1987–2008. Circulation. 2012; 125: 1848–1857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Udell JA, Fonarow GC, Maddox TM, Cannon CP, Frank Peacock W, Laskey WK, Grau-Sepulveda MV, Smith EE, Hernandez AF, Peterson ED, Bhatt DL, Get With The Guidelines Steering C and Investigators. Sustained sex-based treatment differences in acute coronary syndrome care: Insights from the American Heart Association Get With The Guidelines Coronary Artery Disease Registry. Clin Cardiol. 2018;41:758–768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jneid H, Fonarow GC, Cannon CP, Hernandez AF, Palacios IF, Maree AO, Wells Q, Bozkurt B, Labresh KA, Liang L, Hong Y, Newby LK, Fletcher G, Peterson E, Wexler L, Get With the Guidelines Steering C and Investigators. Sex differences in medical care and early death after acute myocardial infarction. Circulation. 2008;118:2803–10. [DOI] [PubMed] [Google Scholar]
- 9.National Heart Lung and Blood Institute. https://biolincc.nhlbi.nih.gov/home/,
- 10.White AD, Folsom AR, Chambless LE, Sharret AR, Yang K, Conwill D, Higgins M, Williams OD, Tyroler HA. Community surveillance of coronary heart disease in the Atherosclerosis Risk in Communities (ARIC) Study: methods and initial two years’ experience. J Clin Epidemiol. 1996; 49: 223–233. [DOI] [PubMed] [Google Scholar]
- 11.Myerson M, Coady S, Taylor H, Rosamond WD, Goff DC Jr, ARIC Investigators. Declining severity of myocardial infarction from 1987 to 2002: the Atherosclerosis Risk in Communities (ARIC) Study. Circulation. 2009; 119: 503–514. [DOI] [PubMed] [Google Scholar]
- 12.Atherosclerosis Risk in Communities Study. https://www2.cscc.unc.edu/aric/sites/default/files/public/manuals/Updates%20Manual3_20151112.pdf,
- 13.Mansournia MA, Altman DG. Inverse probability weighting. BMJ. 2016; 352: i189. [DOI] [PubMed] [Google Scholar]
- 14.Zhang J, Yu KF. What’s the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA. 1998;280(19):1690–1691. [DOI] [PubMed] [Google Scholar]
- 15.Ortman J, Velkoff V. An aging nation: The older population in the United States. United States Census Bureau; 2014. https://www.census.gov/prod/2014pubs/p25-1140.pdf, [Google Scholar]
- 16.Gooding HC, Ning H, Gillman MW, Shay C, Allen N, Goff DC Jr.,, Lloyd-Jones D and Chiuve S Application of a Lifestyle-Based Tool to Estimate Premature Cardiovascular Disease Events in Young Adults: The Coronary Artery Risk Development in Young Adults (CARDIA) Study. JAMA Intern Med. 2017;177:1354–1360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Singh A, Collins BL, Gupta A, Fatima A, Qamar A, Biery D, Baez J, Cawley M, Klein J, Hainer J, Plutzky J, Cannon CP, Nasir K, Di Carli MF, Bhatt DL and Blankstein R. Cardiovascular Risk and Statin Eligibility of Young Adults After an MI: Partners YOUNG-MI Registry. J Am Coll Cardiol. 2018;71:292–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leifheit-Limson EC, D’Onofrio G, Daneshvar M, Geda M, Bueno H, Spertus JA, Krumholz HM and Lichtman JH. Sex Differences in Cardiac Risk Factors, Perceived Risk, and Health Care Provider Discussion of Risk and Risk Modification Among Young Patients With Acute Myocardial Infarction: The VIRGO Study. J Am Coll Cardiol. 2015;66:1949–1957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bucholz EM, Strait KM, Dreyer RP et al. Sex differences in young patients with acute myocardial infarction: A VIRGO study analysis. Eur Heart J Acute Cardiovasc Care 2017. 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Towfighi A, Markovic D and Ovbiagele B. National gender-specific trends in myocardial infarction hospitalization rates among patients aged 35 to 64 years. Am J Cardiol. 2011;108:1102–7. [DOI] [PubMed] [Google Scholar]
- 21.Towfighi A, Zheng L and Ovbiagele B. Sex-specific trends in midlife coronary heart disease risk and prevalence. Arch Intern Med. 2009;169:1762–6. [DOI] [PubMed] [Google Scholar]
- 22.Smolderen KG, Spertus JA, Nallamothu BK, Krumhold HM, Tang F, Ross JS, Ting HH, Alexander KP, Rathore SS, Chan PS. Health Care Insurance, Financial Concerns in Accessing Care, and Delays to Hospital Presentation in Acute Myocardial Infarction.JAMA. 2010;303(14):1392–1400. doi: 10.1001/jama.2010.409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Trivedi AN, Nsa W, Hausmann LR, Lee JS, Ma A, Bratzler DW, Mor MK, Baus K, Larbi F and Fine MJ. Quality and equity of care in U.S. hospitals. N Engl J Med. 2014;371:2298–308. [DOI] [PubMed] [Google Scholar]
- 24.Sonel AF, Good CB, Mulgund J, Roe MT, Gibler WB, Smith SC Jr.,, Cohen MG, Pollack CV Jr., Ohman EM, Peterson ED and Investigators C. Racial variations in treatment and outcomes of black and white patients with high-risk non-ST-elevation acute coronary syndromes: insights from CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the ACC/AHA Guidelines?). Circulation. 2005;111:1225–32. [DOI] [PubMed] [Google Scholar]
- 25.Bhatt DL, Roe MT, Peterson ED, Li Y, Chen AY, Harrington RA, Greenbaum AB, Berger PB, Cannon CP, Cohen DJ, Gibson CM, Saucedo JF, Kleiman NS, Hochman JS, Boden WE, Brindis RG, Peacock WF, Smith SC Jr.,, Pollack CV Jr., Gibler WB, Ohman EM and Investigators C Utilization of early invasive management strategies for high-risk patients with non-ST-segment elevation acute coronary syndromes: results from the CRUSADE Quality Improvement Initiative. JAMA. 2004;292:2096–104. [DOI] [PubMed] [Google Scholar]
- 26.Bucholz EM, Strait KM, Dreyer RP, Lindau ST, D’Onofrio G, Geda M, Spatz ES, Beltrame JF, Lichtman JH, Lorenze NP, Bueno H and Krumholz HM. Editor’s Choice-Sex differences in young patients with acute myocardial infarction: A VIRGO study analysis. Eur Heart J Acute Cardiovasc Care. 2017;6:610–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bangalore S, Fonarow GC, Peterson ED, Hellkamp AS, Hernandez AF, Laskey W, Peacock WF, Cannon CP, Schwamm LH, Bhatt DL, Get with the Guidelines Steering C and Investigators. Age and gender differences in quality of care and outcomes for patients with ST-segment elevation myocardial infarction. Am J Med. 2012;125:1000–9. [DOI] [PubMed] [Google Scholar]
- 28.Lee SK, Khambhati J, Varghese T, Stahl EP, Kumar S, Sandesara PB, Wender NK, Sperling LS. Comprehensive primary prevention of cardiovascular disease in women. Clin Cardiol. 2017;40:832–838. 10.1002/clc.22767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tobias DK, Stuart JJ, Li S, Chavarro J, Rimm EB, Rich-Edwards J, Hu FB, Manson JE and Zhang C. Association of History of Gestational Diabetes With Long-term Cardiovascular Disease Risk in a Large Prospective Cohort of US Women. JAMA Intern Med. 2017;177:1735–1742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lubiszewska B, Kruk M, Broda G, Ksiezycka E, Piotrowski W, Kurjata P, Zielinski T and Ploski R. The impact of early menopause on risk of coronary artery disease (PREmature Coronary Artery Disease In Women--PRECADIW case-control study). Eur J Prev Cardiol. 2012;19:95–101. [DOI] [PubMed] [Google Scholar]
- 31.Yusuf S, Hawken S, Ôunpuu S, Dans T, Avezum A, Lanas F, McQueen M, Budaj A, Pais P, Varigos J, Lisheng L; INTERHEART Study Investigators. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–952. [DOI] [PubMed] [Google Scholar]
- 32.Mosca L, Benjamin EJ, Berra K, Bezanson JL, Dolor RJ, Lloyd-Jones DM, Newby LK, Pin˜a IL, Roger VL, Shaw LJ, Zhao D; Beckie TM, Bushnell C, D’Armiento J, Kris-Etherton PM, Fang J, Ganiats TG, Gomes AS, Gracia CR, Haan CK, Jackson EA, Judelson DR, Kelepouris E, Lavie CJ, Moore A, Nussmeier NA, Ofili E, Oparil S, Ouyang P, Pinn VW, Sherif K, Smith SC Jr, Sopko G, Chandra-Strobos N, Urbina EM, Vaccarino V, Wenger NK. Effectiveness-based guidelines for the prevention of cardiovascular disease in women—2011 update: a guideline from the American Heart Association. Circulation. 2011;123:1243–1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ford ES, Williamson DF, Liu S. Weight change and diabetes incidence: findings from a national cohort of US adults. Am J Epidemiol.1997;146:214–222. [DOI] [PubMed] [Google Scholar]
- 34.Resnick HE, Valsania P, Halter JB, Lin X. Relation of weight gain and weight loss on subsequent diabetes risk in overweight adults. J Epidemiol Community Health.2000;54:596–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.DeFilippis EM, Singh A, Divakaran S, Gupta A, Collins BL, Biery D, Qamar A, Fatima A, Ramsis M, Pipilas D, Rajabi R, Eng M, Hainer J, Klein J, Januzzi JL, Nasir K, Di Carli MF, Bhatt DL, Blankstein R. Cocaine and Marijuana Use among Young Adults Presenting with Myocardial Infarction: The Partners YOUNG-MI Registry. J Am Coll Cardiol. 2018;71:2540–2551. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.