The overall entry mechanism for herpesviruses is not completely known, including those for the human gammaherpesviruses Kaposi’s sarcoma-associated herpesvirus (KSHV) and Epstein-Barr virus (EBV). To fully understand the herpesvirus entry process, functional receptors need to be identified. In the current study, we found that EphA4 can also function for a KSHV entry receptor along with EphA2. Interestingly, we found that EphA4 does not function as an entry receptor for EBV, whereas EphA2 does. The discovery of EphA4 as a KSHV entry receptor has important implications for KSHV pathogenesis in humans, may prove useful in understanding the unique pathogenesis of KSHV infection in humans, and may uncover new potential targets that can be used for the development of novel interventional strategies.
KEYWORDS: Eph receptors, EphA4, Kaposi’s sarcoma-associated herpesvirus, viral entry, gH/gL
ABSTRACT
Kaposi’s sarcoma-associated herpesvirus (KSHV) is a human gammaherpesvirus associated with the development of Kaposi’s sarcoma (KS). KSHV target cells include endothelial cells, B cells, monocytes, epithelial cells, dendritic cells, macrophages, and fibroblasts. KSHV entry into target cells is a complex multistep process and is initiated by the binding and interaction of viral envelope glycoproteins with the cellular receptors. In the current studies, we have found that EphA4 promotes KSHV glycoprotein H/glycoprotein L (gH/gL)-mediated fusion and infection better than does ephrin A2 (EphA2) in HEK293T cells, indicating that EphA4 is a new KSHV entry receptor. To confirm that epithelial cells express EphA2 and EphA4, we analyzed the expression of EphA2 and EphA4 in epithelial cells, endothelial cells, B cells, monocytes, fibroblasts using RNA sequencing (RNA-seq) data analysis of existing data sets. We found that these cell types broadly express both EphA2 and EphA4, with the exception of monocytes and B cells. To confirm EphA4 is important for KSHV fusion and infection, we generated EphA2 and EphA4 single- and double-knockout cells. We found that both EphA2 and EphA4 play a role in KSHV fusion and infection, since EphA2-EphA4 double-knockout cells had the greatest decrease in fusion activity and infection compared to single-knockout cells. Fusion and infection of KSHV were rescued in the EphA2-EphA4 double-knockout cells upon overexpression of EphA2 and/or EphA4. EphA2 binds to both Epstein-Barr virus (EBV) and KSHV gH/gL; however, EphA4 binds only to KSHV gH/gL. Taken together, our results identify EphA4 as a new entry receptor for KSHV.
INTRODUCTION
Herpesviruses are enveloped double-stranded DNA viruses capable of infecting a wide range of hosts and cause a variety of diseases (1). There are nine human herpesviruses that infect humans establishing lifelong latent infections (2). The gammaherpesviruses Kaposi’s sarcoma-associated herpesvirus (KSHV) and Epstein-Barr virus (EBV) are associated with human cancer (1, 3). Kaposi’s sarcoma (KS) is a cancer that develops from the endothelium that lines lymph or blood vessels. It usually appears as tumors on the skin or on mucosal surfaces, such as inside the mouth, lungs, liver, and gastrointestinal tract. Skin lesions usually cause no symptoms; however, KS may become life-threatening if the lesions develop in essential organs such as the lungs, liver, or digestive tract (3).
KSHV infection is essential for the development of KS. The first step of KSHV infection is entry into target cells, which is a complex multistep process. KSHV target cells in humans include endothelial cells, B cells, monocytes, epithelial cells, dendritic cells, macrophages, and fibroblasts (4). Entry of herpesviruses into target cells is initiated by the binding and interaction of viral envelope glycoproteins with cellular receptors, leading to either fusion of the viral envelope with the host cell membrane or endocytosis of viral particles and subsequent fusion of the viral envelope with an endocytic membrane for capsid release (5). Understanding the virus entry process may aide in the development of novel entry inhibitors and vaccines. Multiple KSHV receptors have been identified, including integrins (α3β1, αVβ3, and αVβ5), xCT (cystine/glutamate transporter), intercellular adhesion molecule-3 (ICAM-3), dendritic cell-specific intercellular adhesion molecule-grabbing nonintegrin (DC-SIGN), and ephrin A2 (EphA2) (6–10). The integrin receptors and xCT are likely nonessential for infection and only required for the initial binding of the virus to cells (11), whereas EphA2 is essential because it triggers fusion upon virus binding to epithelial cells (10). The role of EphA2 in EBV entry was only recently identified by us and another group (12, 13). Both EBV and KSHV are associated with epithelial cell cancers, indicating that the engagement of EphA receptors could be a key commonality in the development of these malignancies.
In the current studies, we found that EphA4 functions as an entry receptor for KSHV. It is intriguing that the two human gammaherpesviruses EBV and KSHV use EphA proteins as entry receptors. Both EphA2 and EphA4 belong to the Eph receptor family, a large family of receptor tyrosine kinases (RTKs). The Eph receptor family contains 14 members and is divided into two classes, A and B, based upon sequence similarity and affinity with the 9 ephrin ligands (14). The Eph receptors and their ligands have bidirectional signaling capacity, indicating that they can serve as both receptors and ligands (14). The ephrin receptors transduce signals from the cell exterior to the cell interior by ligand-induced activation of their kinase domain (15). The functions of the Eph family include boundary formation, cell migration, axon guidance, synapse formation, angiogenesis, proliferation, and cell differentiation (15, 16). Eph receptors have been implicated in regulating cell migration, adhesion, proliferation, and differentiation (16). Altered expression patterns of Eph receptors and ephrins (Eph receptor ligands) have been correlated with tumor behavior, such as invasiveness, vascularization, metastatic potential, and patient prognosis (17). Overexpression of EphA2 and EphA4 has been reported in gastric cancer, breast cancer, colon cancer, and prostate cancer (17–24). In the current studies, we investigated and found that EphA4 functions as an entry receptor of KSHV. Overall, the current findings broaden the knowledge of KSHV entry process and herpesvirus entry in general and may facilitate the development of potential entry inhibitors targeting KSHV infection.
RESULTS
EphA4 promotes both KSHV cell-cell fusion activity and infection.
We recently discovered that EBV uses EphA2 but not EphA4 as an epithelial cell entry receptor (12). EphA2 had previously been shown to function as a KSHV entry receptor for endothelial and epithelial cells (10). In the current studies, we investigated if EphA4 may also function in KSHV entry. Key in these studies was the use of EBV glycoprotein B (gB) in the KSHV fusion assay in place of KSHV gB. Our previous work had shown that the KSHV cell-cell fusion assay was not as robust as the EBV fusion assay, making it difficult to obtain reproducible and significant data (25, 26). By replacing KSHV gB with EBV gB, KSHV fusion is greatly enhanced with fusion levels much higher than those mediated by the KSHV glycoproteins (26). The exact nature of this enhancement is unknown but likely is due to differences in the fusion activities of EBV gB and KSHV gB, although a role of glycoprotein H/glycoprotein L (gH/gL) cannot be excluded.
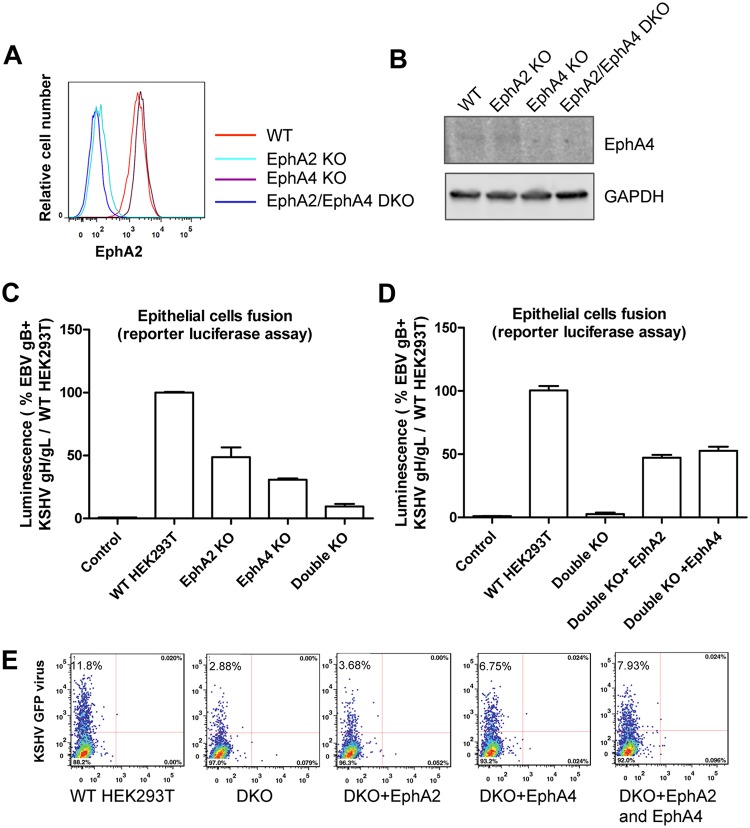
To determine if EphA4 may trigger fusion, we transfected EBV gB with KSHV gH/gL and EBV gH/gL as a control in CHO-K1 cells and quantified fusion with HEK293T target cells overexpressing either EphA2 or EphA4. We found that overexpression of EphA4 induced higher fusion activity for the EBV gB and KSHV gH/gL combination than when EphA2 was tested (Fig. 1A). Our previous data showed that EphA2 but not EphA4 is required for EBV fusion activity (12), similar to the results shown when EBV gB and EBV gH/gL are used (Fig. 1A). These published data combined with the results shown in Fig. 1A suggest a specificity of EphA4 for KSHV gH/gL for fusion function compared to EBV gH/gL. To further examine if EphA4 is sufficient to induce fusion for KSHV gH/gL, we examined fusion activity using a split green fluorescent protein (GFP) fusion assay and readily detected fusion; this was monitored by the appearance of green cells indicative of fusion activity only when KSHV gH/gL- and EBV gB-expressing cells were overlaid with cells that overexpress EphA2 or EphA4 (Fig. 1B). Similarly, EphA4 induced more fusion activity than did EphA2, consistent with our observation of greater fusion in HEK293T cells transfected with EphA4. To examine the effect of EphA4 on KSHV infection of epithelial cells, we transfected HEK293T cells with control plasmid, EphA2, EphA4, and EphA2-EphA4 and then infected the cells with KSHV virus expressing GFP. Flow cytometry showed increased infection of KSHV in the presence of either EphA2 or EphA4 and higher levels of fusion when both EphA2 and EphA4 were transfected (Fig. 1C). We also examined infection by fluorescence microscopy (Fig. 1D), the results of which were consistent with the flow cytometry data (Fig. 1C).
FIG 1.
EphA4 promotes both KSHV infection and virus-free cell-cell fusion. (A) CHO-K1 cells were transfected with T7 luciferase plasmid and either control plasmid or EBV gH/gL, EBV gB, or KSHV gH/gL. Transfected CHO-K1 cells were overlaid with HEK293T cells transfected with pcDNA3.1, EphA2, or EphA4 together with T7 polymerase. Fusion activity was standardized to EBV gB and KSHV gH/gL fusion with HEK293T cells transfected with control pcDNA3.1, which was set to 100%. ***, P < 0.001 (ANOVA followed by post hoc Tukey’s multiple-comparison test), compared to pcDNA 3.1. (B) A total of 2.5 × 105 CHO-K1 cells transfected with Rluc81-7 plasmid together with either control plasmid, EBV gH/gL with EBV gB, or KSHV gH/gL with EBV gB, were overlaid with 2.5 × 105 CHO-K1 cells transfected with pcDNA3.1, EphA2, or EphA4 together with Rluc88-11. Green cells, indicative of fusion, were visualized and captured with an EVOS fluorescence microscope. (C) HEK293T cells were transfected with pcDNA3.1, EphA2, or EphA4. At 24 h posttransfection, 5 × 104 cells were seeded into a 48-well plate. Twenty-four hours later, the cells were infected with concentrated KSHV. After an additional 24 h, the infected cells were analyzed by flow cytometry (C) or visualized by microscopy and images captured with an EVOS fluorescence microscope (D).
EphA2 and EphA4 are expressed in various KSHV target cells, and both function in KSHV entry.
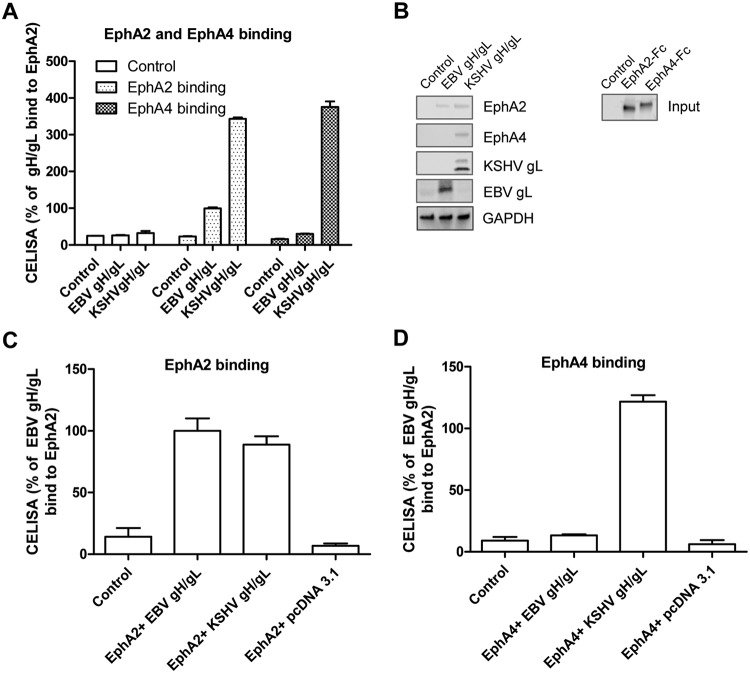
KSHV has broad tropism since its genome and transcripts can be detected in vivo and in vitro in a variety of cell types (27). To confirm that EphA4 is expressed in cells infected by KSHV, we analyzed existing RNA-seq data sets from B cells, monocytes, epithelial cells, fibroblasts, and endothelial cells available from the SRA database (https://www.ncbi.nlm.nih.gov/sra). Neither EphA2 nor EphA4 was expressed abundantly in monocytes, indicating that entry of KSHV into monocytes may use other receptors (Fig. 2A to D), whereas EphA2 and EphA4 were expressed in epithelial cells, fibroblasts, and endothelial cells (https://www.proteinatlas.org/ENSG00000116106-EPHA4/tissue), consistent with KSHV using EphA2 and EphA4 as primary entry receptors in these cell types. To further confirm that EphA4 can serve as a cellular receptor for KSHV infection, we generated EphA2 and EphA4 single- and double-knockout cells using the CRISPR/Cas9 system in HEK293T cells. Following knockout, EphA2 cell surface expression was determined by flow cytometry. As expected, there was a lack of EphA2 expression as analyzed by flow cytometry in the EphA2 single-knockout cells and in the EphA2/EphA4 double-knockout cells but not in the EphA4 knockout cells and wild-type (WT) cells (Fig. 3A). We analyzed EphA4 expression by Western blotting since the available antibodies did not work well for flow cytometry. EphA4 expression was not detected in EphA4 single-knockout cells and in the EphA2-EphA4 double-knockout cells (Fig. 3B). We next examined the effect of EphA2 and EphA4 knockout on KSHV fusion. We found that knockout of EphA2 and EphA4 individually dramatically decreased fusion activity (Fig. 3C). In the EphA2-EphA4 double-knockout cells, fusion activity was further decreased compared to that in single-knockout cells (Fig. 3C). When EphA2 or EphA4 was overexpressed in the double-knockout cells, fusion activity was rescued (Fig. 3D). These data confirmed that both EphA2 and EphA4 are functional for KSHV fusion. Finally, we investigated if EphA2 and EphA4 expression restored KSHV infection in the double-knockout cells. When EphA2 and EphA4 were individually transfected into the double-knockout cells, infection with KSHV was partially rescued compared to levels observed in HEK293T cells (Fig. 3E). The level of infection in EphA2-expressing cells was just above background levels, in contrast to the EphA4-expressing cells, in which the level of infection was higher (Fig. 3E). Overall, the fusion and infection results presented in Fig. 3 indicate that both EphA2 and EphA4 function as receptors, with EphA4 being the better receptor in the assays used in the current studies.
FIG 2.
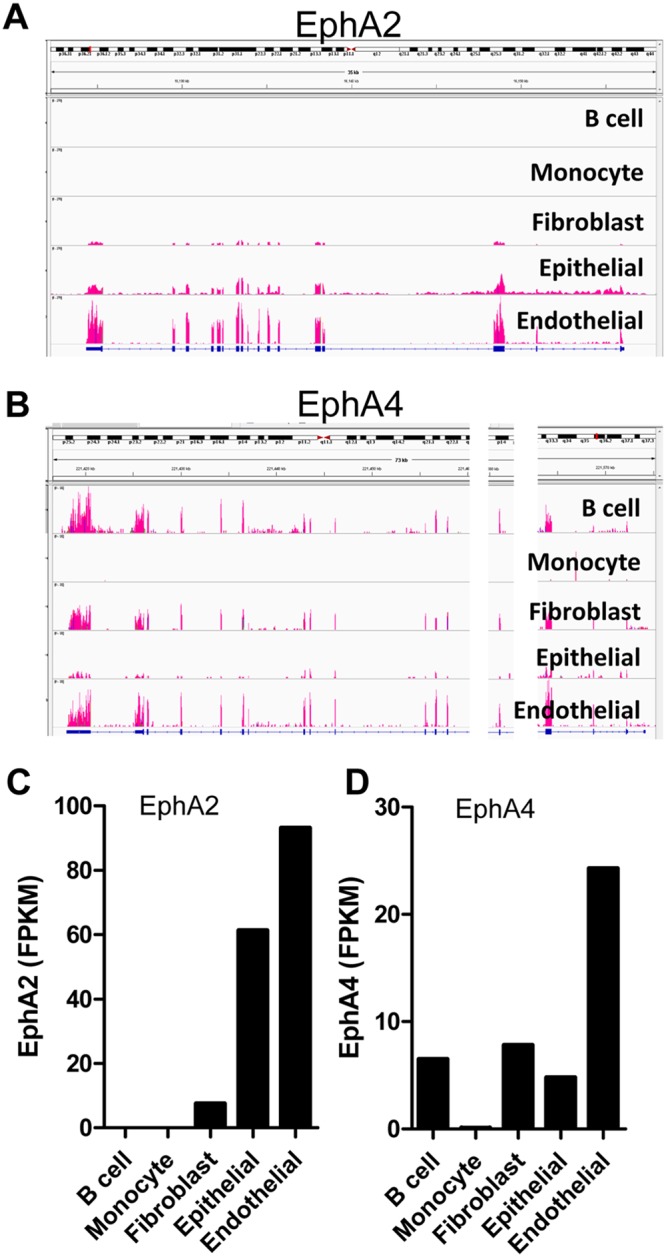
EphA2 and EphA4 expression in KSHV target cells. (A and B) The distribution of EphA2 (A) and EphA4 (B) sequencing reads across EphA2 or EphA4 exons. BAM-formatted files were generated by alignment of RNA-seq data from various cell types infected by KSHV. RNA-seq data were obtained from the Sequence Read Archive database (NIH), and aligned data were then loaded into the Integrative Genomics Viewer (Broad Institute) to acquire the transcript map, with exon reads shown in red. Two chromosomal regions, in which no reads for EphA4 were detected, were removed and are shown as white bars, allowing the transcript map to fit within the figure. (C and D) The mean fragments per kilobase of transcript per million mapped reads (FPKM) of EphA2 (C) and EphA4 (D) in various KSHV target cells. FPKM was determined using the Cuffdiff software (Broad Institute).
FIG 3.
EphA4 is the potential epithelial cell receptor for KSHV. (A) EphA2 cell surface expression in EphA2 and EphA4 single- or double-knockout (DKO) HEK293T cells by flow cytometry. The x axis represents the relative number of cells analyzed by flow cytometry with a particular level of EphA2 expression. The y axis represents the level of expression within the analyzed cell population on a log scale. (B) EphA4 expression in EphA2 and EphA4 single- or double-knockout HEK293T cells by Western blotting. Glyceraldehyde-3-phosphate dehydrogenase (GAPDH) was used as a loading control. For fusion function of knockout cell lines, CHO-K1 cells transfected with T7 luciferase and either a control plasmid or KSHV gH/gL with EBV gB were overlaid with EphA2 and EphA4 single- or double-knockout cells together with T7 polymerase (C), or EphA2-EphA4 double-knockout cells overexpressing EphA2 or EphA4 together with T7 polymerase (D). (E) WT or EphA2 and EphA4 double-knockout cells were transfected with EphA2, EphA4, or EphA2-EphA4 and infected with KSHV as described in Materials and Methods. Twenty-four hours post-infection, cells were analyzed by flow cytometry. Percentage of infected cells, which are GFP positive, are as indicated in panel E.
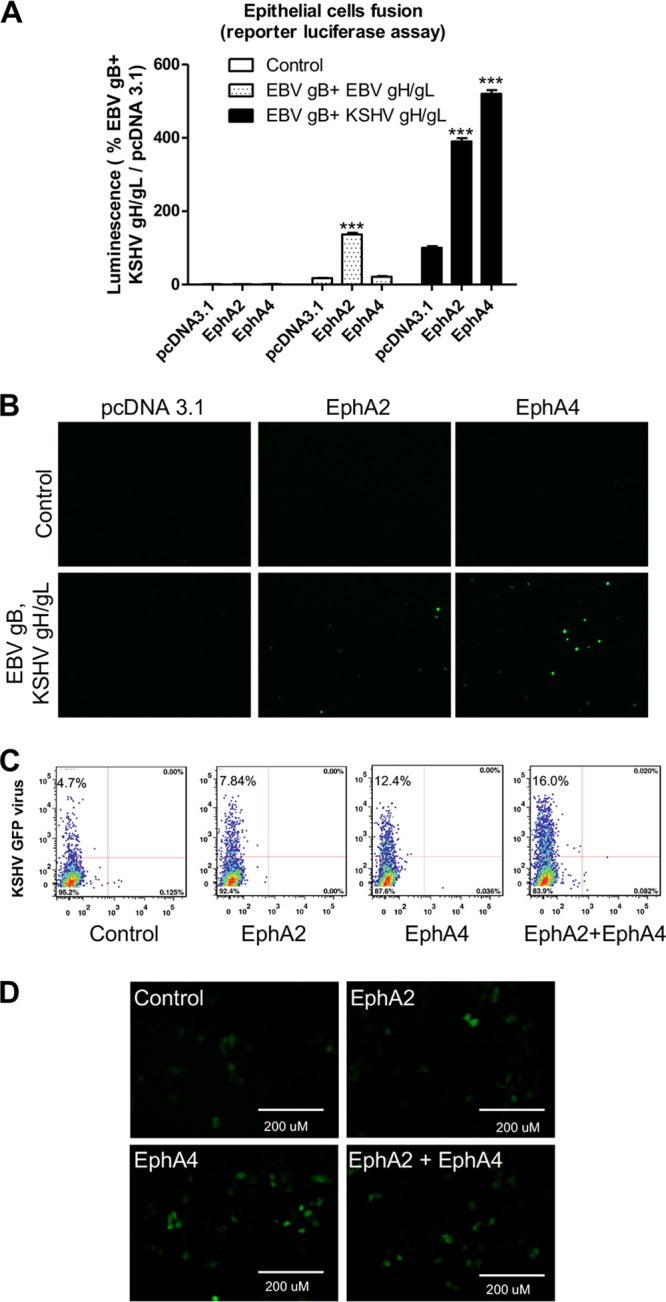
Both EphA2 and EphA4 bind to KSHV gH/gL.
Previous studies indicated that both EphA2 and EphA4 can bind KSHV gH/gL by coimmunoprecipitation, but the function of EphA4 in mediating entry was not studied (28). To confirm the previously observed binding of KSHV gH/gL with EphA2 and EphA4, we used three different methods. We first transfected CHO-K1 cells with control plasmid, EBV gH/gL, or KSHV gH/gL. Twenty-four hours later, the cells were detached and seeded in a 96-well plate in triplicate or in a 6-well plate. Supernatants from cells transfected with the soluble forms of EphA4-Fc and EphA2-Fc were added to cells transfected with KSHV or EBV gH/gL at 4°C. The binding of EphA2 or EphA4 with EBV or KSHV gH/gL was then determined by CELISA or Western blotting (Fig. 4A and B). The cell enzyme-linked immunosorbent assay (CELISA) data showed that EphA2 can bind to both EBV and KSHV gH/gL but with higher levels for KSHV gH/gL (Fig. 4A). However, EphA4 only bound to KSHV gH/gL and not EBV gH/gL (Fig. 4A). This is consistent with the observation that EphA4 expression does not increase EBV fusion. When soluble EphA2-Fc is coexpressed with EBV gH/gL-, KSHV gH/gL-, or control vector-transfected cells, soluble EphA2-Fc can bind to both EBV and KSHV gH/gL, as detected by CELISA (Fig. 4C). However, soluble EphA4-Fc can only be detected when KSHV gH/gL are coexpressed and not with EBV gH/gL (Fig. 4D). These data confirmed that KSHV gH/gL can bind to both EphA2 and EphA4, whereas EBV gH/gL binds better to EphA2 than to EphA4 (Fig. 4A). There was some difference in the efficiency of EphA2 binding to KSHV gH/gL and EBV gH/gL when Fig. 4A and C are compared. This is likely a result of the different methods used to detect binding, as described in the legend for Fig. 4 and Materials and Methods.
FIG 4.
Both EphA2 and EphA4 bind to KSHV gH/gL. (A) CHO-K1 cells were transiently transfected with control pcDNA3.1, EBV gH/gL, or KSHV gH/gL plasmids. Soluble EphA2-Fc or EphA4-Fc was prepared by transfecting CHO-K1 cells with EphA2-Fc or EphA4-Fc plasmid constructs, and medium supernatants containing EphA2-Fc or EphA4-Fc were overlaid on HEK293T cells expressing EBV gH/gL or KSHV gH/gL in 96-well plates in triplicate for 2 h at 4°C; bound protein was detected using anti-human IgG, which recognizes the Fc portion of the Eph2-Fc and EphA4-Fc by CELISA. (B) CHO-K1 cells seeded in 6-well plates were transfected with control plasmid pcDNA3.1, EBV gH/gL, or KSHV gH/gL with gL containing a Hig tag, as indicated. After 24 h, cells were washed twice with ice-cold PBS and incubated with supernatants from pcDNA3.1 (control plasmid), EphA2-Fc-, or EphA4-Fc-transfected cells isolated 24 h posttransfection for 2 h at 4°C. The cells were then washed with ice-cold PBS three times and lysed with 200 μl of 1 × SDS lysis buffer. Proteins bound to the cells expressing EBV gH/gL or KSHV gH/gL were then analyzed using antibodies to the Fc region of the EphA2 and EphA4 fusions by Western blotting. GAPDH was used as a loading control. Expression of the KSHV gH/L or EBV gH/gL complex was monitored by analyzing KSHV gL or EBV gL expression using anti-His antibodies directed against a His tag added to KSHV gL or polyclonal antibodies directed against EBV gL. (C and D) CHO-K1 cells seeded in 6-well plates were transfected with control plasmid pcDNA3.1, EBV gH/gL, or KSHV gH/gL together with EphA2-Fc or EphA4-Fc. Transfected cells were seeded in 96-well plates in triplicate posttransfection. The cells were then washed with ice-cold PBS three times, and gH/gL-associated EphA2 (C) or EphA4 (D) was determined by CELISA using anti-human IgG antibodies.
The ectodomains of EphA2 and EphA4 are interchangeable for KSHV fusion activity, and EphA4 kinase activity is not needed for KSHV fusion activity.
EphA4 is a membrane protein with four different ectodomain regions, including a ligand binding domain (LBD), a cysteine-rich region (CYS), and two fibronectin regions (FBN). EphA4 and EphA2 share about 51% similarity at the amino acid level. The kinase domain is located within the cytoplasmic tail domain. Previous studies by Hahn et al. indicated that the ectodomain of EphA2 is important for binding with KSHV (10). Our previous results with EBV found that the LBD is important in EBV fusion function. We demonstrated this by swapping the LBD of EphA2 and EphA4 to generate EphA2A4 or EphA4A2 LBD chimeras (12). We used the same constructs to investigate if the LBDs of EphA2 and EphA4 are interchangeable for KSHV gH/gL. Overall, all of the chimeras worked well in KSHV fusion (Fig. 5A and B). Interestingly, the EphA4A2 chimera functioned better in fusion than did the EphA2A4 chimera, indicating that the LBD domain may be responsible for the greater fusion activity observed for EphA4 than for EphA2.
FIG 5.
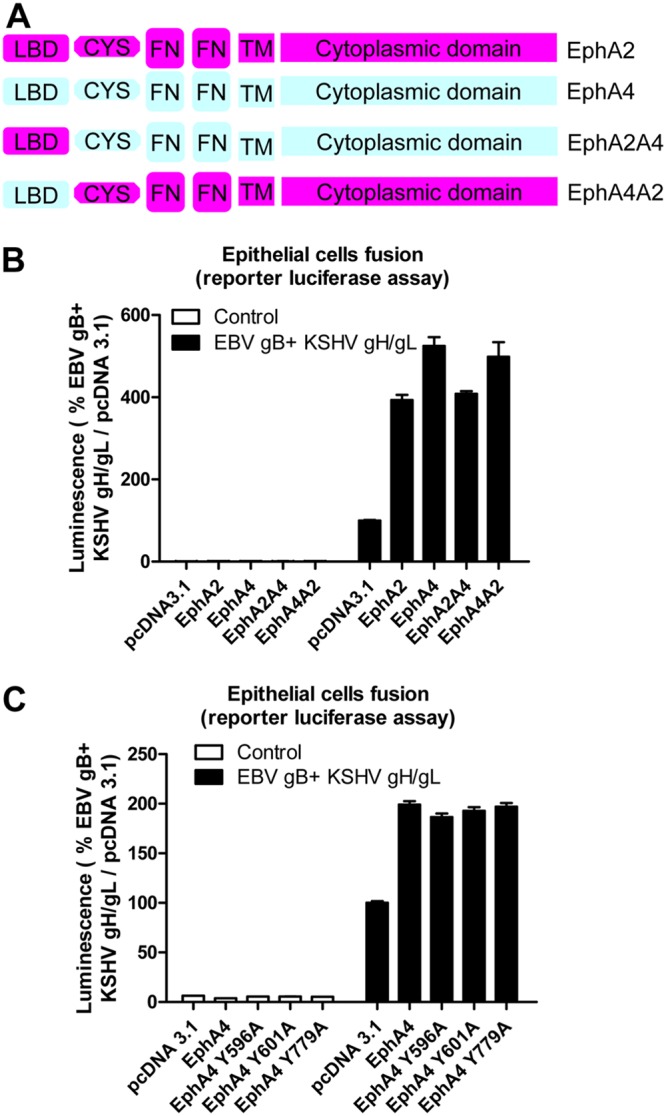
The ectodomain of EphA2 and EphA4 are interchangeable for KSHV fusion activity, and the kinase activity of EphA4 is not needed for KSHV fusion activity. (A) Schematic drawing of the EphA2, EphA4, and, EphA2-EphA4 chimeras, including the ligand binding domain (LBD). (B) KSHV fusion with HEK293T cells transfected with control plasmid pcDNA3.1, EphA2, EphA4, or EphA2 and EphA4 chimeras, as indicated. (C) KSHV fusion with HEK293T cells transfected with control plasmid pcDNA3.1, EphA4, or EphA4 kinase-dead mutants as indicated. (B and C) Fusion activity of HEK293T cells transfected with pcDNA 3.1 was set to 100%.
Previous studies had demonstrated that the kinase region of EphA2 was important for KSHV endocytosis (10) and subsequent entry. Our previous results demonstrated the EphA2 kinase function was not important for EBV mediated cell-cell fusion (12). To investigate if the kinase function was also nonessential for KSHV cell-cell fusion, we constructed three EphA4 kinase-dead mutants based on previous studies (27, 28), similar to the EphA2 constructs that we used in our previous study with EBV (12). In these constructs, tyrosine 596, 602, and 779 were all mutated individually to alanine. These three mutants all lack kinase activity based on prior mutagenesis studies (29, 30). The three EphA4 kinase-dead mutants were transfected into HEK293T cells. The fusion activities of the mutants compared to that of WT EphA4 (Fig. 5C) were similar, indicating that the kinase activity is not important for the fusion function of EphA4. The lower fusion observed in the pcDNA3.1-transfected cells is a result of the existing EphA2 and EphA4 expression in these cells since the EphA2-EphA4 double-knockout cells were not used for this experiment.
DISCUSSION
KSHV infection is essential for the development of KS (3). This study has shown that, similar to EphA2, EphA4 is a receptor that can directly interact with KSHV gH/gL. Moreover, we found that EphA4 functions better than EphA2, since overexpression of EphA4 enhances KSHV fusion by approximately 33% and KSHV infection by 163% compared to EphA2 (Fig. 1). Both EphA2 and EphA4 are expressed in many KSHV target cells, including epithelial cells, fibroblasts, and endothelial cells (Fig. 2). Interestingly, EphA4 but not EphA2 is expressed in B cells, suggesting that EphA4 might play a key role in KSHV B cell infection exclusively compared to EphA2. Knockout of both EphA2 and EphA4 greatly decreased fusion and infection of KSHV, while overexpression of EphA2 and EphA4 alone or together rescued the fusion and infection of EphA2-EphA4 double-knockout cells (Fig. 3). These findings indicate that EphA4 might be a novel factor important for KSHV infection and may play a role in KS pathogenesis.
Recently, EphA2 has been identified as the receptor for several viruses and as an epithelial cell pattern recognition receptor for fungal β-glucans (31). The human blood-brain barrier internalizes Cryptococcus neoformans via EphA2 (32). EphA2 is a receptor for KSHV and EBV and a cellular cofactor for hepatitis C virus entry (33). Additionally, ephrinB2, one ligand of this family, has been identified as a receptor for Nipah virus (34, 35). Thus, the Eph family and its ligands are entry factors for many pathogens.
Cell entry by KSHV is a multistep process involving viral envelope glycoproteins as well as cellular receptors and other cofactors leading to the merger of virus and host membranes (5). The binding receptors for KSHV include surface heparan sulfate (HS), which promotes a charge-based interaction between virus glycoproteins and the cell surface. Integrins such as α3β1, αVβ3, and αVβ5 play a crucial role in KSHV infection (6). xCT, a 12-transmembrane glutamate/cystine exchange transporter protein, and DC-SIGN have also been reported to be entry receptors for KSHV (7–9). More recently, EphA2 was identified as receptor that mediates KSHV infection of epithelial and endothelial cells (10). After the identification of EphA2 as the receptor for KSHV, Hahn and Desrosiers screened the interaction of 14 Eph proteins with KSHV gH/gL. They found that other Eph family members also interact with KSHV gH/gL, including EphA4, EphA5, and EphB8 (28).
Like EBV gH/gL and HSV gH/gL, KSHV gH/gL forms a non-covalently linked complex (36). The function of gH/gL is to provide a key function in herpesvirus fusion to trigger gB activation and subsequent membrane fusion. Our previous results found that compared to EBV gB, KSHV gB is a poor fusogen (26). In the current study, we used this enhanced fusion function of EBV gB with KSHV gH/gL to increase fusion activity to facilitate the current studies. We found that while only EphA2 can enhance the fusion activity of EBV gH/gL, both EphA2 and EphA4 can enhance the fusion activity of KSHV gH/gL (Fig. 1A), indicating the specificity of EphA4 for KSHV gH/gL. Using a split GFP assay, we found that overexpression of EphA2 or EphA4 can induce fusion compared to control cells, indicating that EphA2 or EphA4 alone is sufficient to serve as the receptor for KSHV gH/gL (Fig. 1B). In WT HEK293T cells, overexpression of either EphA2 or EphA4 or both can also enhance KSHV infection (Fig. 1C and D).
EphA4 is widely expressed in different tissues and cell types (3). Using RNA-seq analysis, we found that EphA4 is expressed in B cells, fibroblasts, epithelial cells, and endothelial cells (Fig. 2) suggesting a role for EphA4 in the infection of epithelial cells. To confirm this, we generated EphA2 and EphA4 single- and double-knockout cells. Fusion activity was decreased in both EphA2 (approximate 50% decrease) and EphA4 single-knockout cells (approximate 70% decrease) (Fig. 3C). Fusion activity was drastically decreased in the EphA2-EphA4 double-knockout cells (90% decrease) (Fig. 3C). Transfection of the double-knockout cells with EphA2 or EphA4, and especially both EphA2 and EphA4, rescued infection (Fig. 3E and F). These results together indicate that both EphA2 and EphA4 play a role in KSHV fusion. A recent paper published by TerBush et al. reveals an integrin-independent route of KSHV infection and suggests that multiple Eph receptors besides EphA2 can promote and regulate infection, consistent with our findings (11).
As a KSHV receptor, EphA2 binds to KSHV gH/gL at a nanomolar level (12, 37). Previous coimmunoprecipitation (co-IP) data also showed that KSHV gH/gL can bind to EphA2, EphA4, EphA5, and EphB8 (28). We confirmed that EphA4 can bind to KSHV gH/gL. Using three different methods, we showed that EphA2 can bind to both EBV gH/gL and KSHV gH/gL independent of gB (Fig. 4) and that only EphA4 can bind to KSHV gH/gL, as previously shown (12, 28). Recently, Großkopf et al. found a conserved motif, ELEFN, within gH of KSHV and rhesus monkey rhadinovirus (RRV) which is important for the EphA2 and EphB3 binding (38). Mutation of the ELEFN motif in RRV and KSHV is sufficient for detargeting of KSHV from Eph family receptors and reduces infection of susceptible cells (38). The corresponding motif in EBV gH is DIEGH. Interestingly, the first three amino acids in this motif, DIE, have structural and biochemical characteristics similar to those of the ELE found in KSHV gH. In contrast, the last two amino acids in the ELEFN motif, F and N, are structurally and biochemically quite different from the G and H found in EBV gH, suggesting that these two regions may be critical for KSHV to use EphA2 and EphA4 as receptors.
Our results showed that EphA4 promotes KSHV fusion approximately 33% better than does EphA2 (Fig. 1A and 5B) for KSHV fusion. Both KSHV gH/gL and EBV gH/gL binds to the EphA2 LBD domain, and the interaction can be competed with ephrins (12, 13, 37). In the current study, we tested EphA2 and EphA4 LBD chimeras and found that the LBD of EphA2 and EphA4 is interchangeable for KSHV fusion. Interestingly, it is the LBD that determines fusion activity since the chimera containing the EphA4 LBD (EphA4A2) behaves more like WT EphA4, and this is also true for the EphA2A4 chimera (Fig. 5B).
Previously, we examined if the kinase activity of EphA2 is important for the fusion of EBV gH/gL and did not observe any loss of fusion function for the kinase-dead EphA2 mutants (12). In the current study, we examined the kinase activity of EphA4 in the context of KSHV gH/gL fusion. Similarly, we did not observe any changes between WT EphA4 and the EphA4 kinase-dead mutants for fusion function. Previous work indicated that binding of KSHV gH/gL to EphA2 triggered EphA2 phosphorylation and endocytosis (10). Since fusion levels are not altered in the EphA2 and EphA4 kinase-dead mutants, it is likely that the kinase function is important for infection by functioning in endocytosis following virus binding (10).
Both EphA2 and EphA4 are overexpressed in numerous malignancies, including gastric cancer, breast cancer, colon cancer, and prostate cancer (17–24). Since both EBV and KSHV infections are associated with multiple malignancies, along with the observation that both EBV and KSHV use EphA family receptors, it will be of interest to determine if EphA2 and EphA4 play a role in the development of KSHV- and/or EBV-associated cancers not only as entry receptors. The identification of EphA4 as a KSHV entry receptor provides new opportunities to understand the tissue tropism of KSHV and strategies to limit KSHV infection in the human host.
MATERIALS AND METHODS
Cell culture.
Chinese hamster ovary (CHO-K1) cells (ATCC CCL-61) were grown in Ham’s F-12 medium (Corning) containing 10% heat-inactivated fetal bovine serum (FBS; Corning) and 1% penicillin-streptomycin (100 U penicillin/ml, 100 µg streptomycin/ml; Sigma). Human embryonic kidney 293T (HEK293T) cells (ATCC CRL-3216) or HEK293-T14 cells derived from HEK293T stably expressing T7 RNA polymerase (39) were grown in Dulbecco’s modified Eagle medium (DMEM; Corning) with 100 µg/ml zeocin (Invitrogen, for HEK293T cells expressing T7 RNA polymerase only), containing 10% heat-inactivated FBS and 1% penicillin-streptomycin, respectively. iSLK.219 KSHV cells (40) were kindly provided by Eva Gottwein and were grown in DMEM (Corning) containing 10% tetracycline-free fetal bovine serum complex (Clontech) and 1% penicillin-streptomycin (100 U penicillin/ml, 100 µg streptomycin/ml; Sigma).
Constructs.
The EphA2 and EphA4 constructs (12) were a gift from Spiro Getsios (Northwestern University). The construction of the EphA2 and EphA4 LBD chimeras (EphA2A4 or EphA4A2) was previously described (12). Soluble EphA2-Fc and EphA4-Fc were cloned in an Fc construct a gift from Qing Fan (41). The EphA2-Fc (lowercase letters indicate the His tag sequence) constructs used were oligonucleotides EphA2-Fc F, GACTCGAGATGCAGGGCAAGGAAGTGGTACTG; and EphA2-Fc R, GACTCGAGgtggtgatggtgatgatgGTTGCCAGATCCCTCCGGGGA. The EphA4-Fc (lowercase letters indicate the His tag sequence) constructs used were oligonucleotides EphA4-Fc F, GACTCGAGATGGCTGGGATTTTCTATTTC; and EphA4-Fc R, GACTCGAGgtggtgatggtgatgatgTGTGGAGTTAGCCCCATCTCC (lowercase letters indicate the His tag sequence).
His-tagged KSHV gL was subcloned into the pSG5 vector using the following primers: KSHV gL EcoRI F, GCGAATTCCATGGGGATCTTTGCGCTATTT; and KSHV His gL BglII R, TAAGATCTGTTTAGTGGTGATGGTGATGATGTTTTCCCTTTTGACCTGCGTG.
The EphA2 single guide RNA (sgRNA) constructs used were oligonucleotides, 5′-AAACGTGTGCGCTACTCGGAGCCTC-3′ and 5′-CACCGGAAGCGCGGCATGGAGCTCC-3′, which were annealed and ligated into a lentiGuide-Puro plasmid (Addgene #52963). EphA4 sgRNA constructs used were oligonucleotides 5′-AAACCACAGTACATTTTTGGCACAC-3′ and 5′-CACCGTGTGCCAAAAATGTACTGTG-3′, which were annealed and ligated into a lentiGuide-Puro plasmid (Addgene #52963). Sequencing was performed for all constructs to confirm the correct sequence.
RNA-seq data assay.
The RNA-seq data assay was performed as described in our previous paper (12). Briefly, the Sequence Read Archive (SRA) data from RNA-seq for B cells (SRA accession numbers SRR5048157 and SRR5048162), monocytes (SRA accession numbers SRR5048180 and SRR5048177), fibroblasts (SRA accession numbers SRR3192540 and SRR3192539), epithelial cells (SRA accession numbers SRR3192374 and SRR3192375), and endothelial cells (SRA accession numbers SRR3192370 and SRR3192369) were downloaded from the SRA database (https://www.ncbi.nlm.nih.gov/sra). The SRA data were transformed into the original FASTQ documents using NCBI SRA Toolkit fastq-dump. The original documents were further trimmed using FASTX and aligned to the reference genome using TopHat2. The differential expression analysis was performed using Cuffdiff software.
Generation of EphA2 and EphA4 single- and double-KO cells.
For EphA2 and EphA4 single- and double-KO cells, Cas9-expressing stable HEK293-T14 cells were established by infecting with lentivirus containing Cas9 for 24 h. Twenty-four hours later, the cells were changed to fresh medium with 5 μg/ml blasticidin for selection. After 1 week, single colonies were picked as previously described and expanded for 2 to 3 weeks (12). The Cas9 expression in these single-cell colonies was analyzed using Western blotting using the Flag tag fused to Cas9. A total of 2.5 × 105 HEK293-T14-Cas9 cells per well in a 12-well plate were infected with lentivirus, including control sgRNA, EphA2 sgRNA, or EphA4 sgRNA, either individually or combined. The cells were selected with 2 μg/ml puromycin and cloned as single cells as previously described (12). After 2 to 3 weeks of expansion, knockout of EphA2 was confirmed by flow cytometry, and the knockout of EphA4 was confirmed by Western blotting.
Fusion assay.
The virus-free cell-based fusion assay was performed as described previously (42). Briefly, CHO-K1 cells grown to approximately 80% confluence in a 6-well plate and were transiently transfected with T7 luciferase reporter plasmid with a T7 promoter (1.5 µg) and the essential glycoproteins for EBV fusion, EBV gB (0.8 µg), EBV gH (0.5 µg), and EBV gL (0.5 µg) or, for KSHV fusion, EBV gB (0.8 µg), KSHV gH (0.5 µg), and KSHV gL (0.5 µg) by using Lipofectamine 2000 transfection reagent (Invitrogen) in Opti-MEM medium (Gibco-Life Technologies), as previously described (26). HEK293T cells or EphA2-single, EphA4-single, or EphA2-EphA4 double-knockout (DKO) cells were transfected with T7 polymerase (1.5 μg) plus 1.5 μg pcDNA 3.1, EphA2, or EphA4 for the fusion assay. After 24 h posttransfection, the transfected CHO-K1 cells were detached, counted, and mixed in a 1:1 ratio with target cells (HEK293T cells, 2.0 × 105 per sample) into a 48-well plate in 0.5 ml Ham’s F-12 medium with 10% heat-inactivated FBS. Twenty-four hours later, the cells were washed once with phosphate-buffered saline (PBS) and lysed with 50 µl of passive lysis buffer (Promega). Luciferase activity was quantified by transferring 20 µl of lysed cells to a 96-well plate and adding 50 µl of luciferase assay reagent (Promega). Luminescence was measured on a PerkinElmer Victor II plate reader. For the split GFP fusion assay, T7 polymerase was replaced with RLuc88-11 (encode half of the GFP protein), and T7 luciferase was replaced with RLuc81-7 (encode the other half of the GFP protein). The plasmids used were kindly provided by Gary Cohen and constructed by Matsuda and colleagues (43, 44). Images monitoring fusion were taken using an EVOS cell imaging system at ×10 magnification.
Cell surface expression.
Surface expression of EphA2 was determined by flow cytometry analysis. A total of 1 × 106 WT HEK293T cells, EphA2- or EphA4 single-knockout, or double-knockout cells were harvested, washed with PBS containing 1% bovine serum albumin (BSA), and incubated with 5 μl of phycoerythrin (PE)-conjugated EphA2 antibody (BioLegend, SHM16) in 50 μl PBS containing 1% BSA for 30 min at 4°C. Cells were then washed and diluted in 300 μl PBS containing 1% BSA. Data were acquired using a BD LSRFortessa instrument, and the FlowJo software was used for analysis.
KSHV infection.
iSLK.219 cells (40) were cultured in DMEM supplemented with 10% fetal bovine serum (tetracycline [Tet]-free FBS), 1% penicillin-streptomycin, 1 μg/ml puromycin, 250 μg/ml G418, and 1 mg/ml hygromycin B. KSHV producing cells (2.0 × 105/well iSLK219 cells) were seeded in a 24-well plate in DMEM supplemented with 10% FBS and 1% penicillin-streptomycin. Twenty-four hours later, the cells were induced with 1 μg/ml doxycycline. After 4 days, the supernatant was collected, and cells were pelleted at 1,500 rpm for 10 min; the supernatant was aliquoted in 1 ml and then frozen at −80°C or centrifuged at 13,000 rpm for 30 min at 4°C. The pellets were resuspended in 100 μl of 10% FBS-DMEM. A total of 7.5 × 104 HEK293T cells/well were seeded on a 48-well plate and infected on the second day with 100 μl KSHV in 10% FBS-DMEM. The percentage of infected cells was determined by flow cytometry or microscopic imaging.
Western blotting.
Expression of EphA4 was examined by Western blotting. WT HEK293T cells and EphA2 or EphA4 single- or double-knockout cells in 6-well plates were collected and resuspended in 50 μl PBS and then mixed with 50 µl 2 × SDS loading buffer (60 mM Tris-HCl [pH 6.8], 0.2% SDS, 25% glycerol, 0.01% bromophenol blue). Samples were boiled for 3 min and loaded onto a Bio-Rad 4 to 20% Mini-PROTEAN TGX gel for Western blotting. After electrophoresis, proteins were transferred to nitrocellulose membranes (Schleicher & Schuell, Keene, NH). The blots were blocked with 5% nonfat dry milk in buffer (20 mM Tris-HCl [pH 7.6], 137 mM NaCl) for 2 h at room temperature (RT). The blots were washed with PBS and incubated with primary antibodies (anti-EBV gH/gL [a rabbit polyclonal antiserum; 1:200]) (45) and anti-His tag antibody (for His-tagged KSHV gL, OB05, 1:1,000; Calbiochem) overnight at 4°C. Anti-rabbit IRDye800 or anti-mouse IRDye680 secondary antibodies (LI-COR Biosciences, Lincoln, NE) were added to the membranes at a dilution of 1:10,000 and incubated for 1 h at RT. For detection of EphA2-Fc and EphA4-Fc, the membrane with transferred proteins was incubated with anti-human IgG (H&L) (horseradish peroxidase [HRP]) (ab6759, 1:1,000; Abcam) against the Fc region. The membrane was then incubated with 1 ml SuperSignal chemiluminescent substrate (Thermo Fisher Scientific) prior to imaging. Protein bands on the membrane were visualized with the Odyssey Fc Western blotting imager using Image studio version 2.0 (LI-COR Biosciences).
Cell enzyme-linked immunosorbent assay.
The EphA2-Fc and EphA4-Fc bound to the transfected cells was determined by cell enzyme-linked immunosorbent assay (CELISA). CHO-K1 cells were transiently transfected with control plasmid pcDNA 3.1, EBV gH/gL, and KSHV gH/gL. Soluble EphA2-Fc and EphA4-Fc were prepared by transfecting the CHO-K1 cells with EphA2-Fc and EphA4-Fc constructs and used to overlay epithelial cells (5 × 104 cells/well) in 96-well plates in triplicate. After incubation for 2 h at 4°C, the cells were incubated with anti-human IgG (H&L) (HRP) (ab6759, 1:1,000; Abcam) against the Fc region for 30 min and fixed with 2% formaldehyde and 0.2% glutaraldehyde in PBS for 15 min, followed by three PBS washes. 3,3′,5,5′,-Tetramethylbenzidine (TMB) one-component HRP microwell substrate was added, and the amounts of bound EphA2-Fc and EphA4-Fc were determined by measuring the absorbance at 380 nm with a PerkinElmer Victor plate reader. Binding activity was standardized in comparison to EphA2-Fc binding to EBV gB, which was set to 100%.
Statistical analysis.
Data were collected from three independent experiments. Statistical differences between multiple groups were determined by one-way ANOVA with post hoc Tukey’s multiple-comparison test. Two-group comparisons were analyzed by the two-tailed unpaired Student t test. A P value of <0.05 denotes the presence of a statistically significant difference. Data are expressed as mean ± standard error (SE). The analysis was performed using GraphPad Prism version 6.0c for Mac (GraphPad Software, San Diego, CA, USA). Flow cytometry histograms and microscopy images are representative of at least two independent experiments.
Data availability.
The data that support the findings of this study are available within this article and its supplemental information files or, upon request, the relevant information from the corresponding author.
ACKNOWLEDGMENTS
We appreciate the help and advice from members of the Longnecker and Jardetzky laboratories, especially Nanette Susmarski. We thank Gary Cohen for kindly providing the RLuc8 plasmids that were originally constructed by Z. Matsuda.
This research was supported by grant AI076183 (to R.L. and T.S.J.) and grant AI137267 (to R.L. and T.S.J.) from the National Institute of Allergy and Infectious Diseases, grant IRG-15-173-21 (to J.C.) from the American Cancer Society, and the Third Coast Center for AIDS Research pilot award (to J.C.).
J.C. and R.L. designed the overall study with input from the coauthors. J.C. performed the key experiments. X.Z. performed the RNA-seq analysis, aided in the design of the sgRNA, EphA2-Fc, and EphA4-Fc constructs, and helped with statistical analysis. S.S. helped with cell cultures and fusion assays and the generation of EphA2/EphA4 chimeras. J.C. and R.L. wrote the manuscript. S.S., X.Z., and T.S.J. contributed expertise and helped write the paper. All authors analyzed the results, read, and approved the manuscript for submission.
We declare no competing financial interests.
Footnotes
Citation Chen J, Zhang X, Schaller S, Jardetzky TS, Longnecker R. 2019. Ephrin receptor A4 is a new Kaposi’s sarcoma-associated herpesvirus virus entry receptor. mBio 10:e02892-18. https://doi.org/10.1128/mBio.02892-18.
Contributor Information
Thomas Shenk, Princeton University.
Gary Cohen, University of Pennsylvania.
Erle Robertson, University of Pennyslvannia.
REFERENCES
- 1.Longnecker R, Kieff E, Cohen JI. 2013. Epstein-Barr virus, p 1898–1959. In Knipe DM, Howley PM, Cohen JI, Griffin DE, Lamb RA, Martin MA, Roizman B (ed), Fields virology, 6th ed Lippincott Williams & Wilkins, Philadelphia, PA. [Google Scholar]
- 2.Pellett PE, Roizman B. 2013. Herpesviridae, p 1802–1822. In Knipe DM, Howley PM, Cohen JI, Griffin DE, Lamb RA, Martin MA, Roizman B (ed), Fields virology, 6th ed Lippincott Williams & Wilkins, Philadelphia, PA. [Google Scholar]
- 3.Damania BA, Cesarman E. 2013. Kaposi's sarcoma-associated herpesvirus, p 2080–2128. In Knipe DM, Howley PM, Cohen JI, Griffin DE, Lamb RA, Martin MA, Roizman B (ed), Fields virology, 6th ed Lippincott Williams & Wilkins, Philadelphia, PA. [Google Scholar]
- 4.Kumar B, Chandran B. 2016. KSHV entry and trafficking in target cells-hijacking of cell signal pathways, actin and membrane dynamics. Viruses 8:305. doi: 10.3390/v8110305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Connolly SA, Jackson JO, Jardetzky TS, Longnecker R. 2011. Fusing structure and function: a structural view of the herpesvirus entry machinery. Nat Rev Microbiol 9:369–381. doi: 10.1038/nrmicro2548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Veettil MV, Sadagopan S, Sharma-Walia N, Wang FZ, Raghu H, Varga L, Chandran B. 2008. Kaposi’s sarcoma-associated herpesvirus forms a multimolecular complex of integrins (alphaVbeta5, alphaVbeta3, and alpha3beta1) and CD98-xCT during infection of human dermal microvascular endothelial cells, and CD98-xCT is essential for the postentry stage of infection. J Virol 82:12126–12144. doi: 10.1128/JVI.01146-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rappocciolo G, Hensler HR, Jais M, Reinhart TA, Pegu A, Jenkins FJ, Rinaldo CR. 2008. Human herpesvirus 8 infects and replicates in primary cultures of activated B lymphocytes through DC-SIGN. J Virol 82:4793–4806. doi: 10.1128/JVI.01587-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rappocciolo G, Jenkins FJ, Hensler HR, Piazza P, Jais M, Borowski L, Watkins SC, Rinaldo CR Jr.. 2006. DC-SIGN is a receptor for human herpesvirus 8 on dendritic cells and macrophages. J Immunol 176:1741–1749. doi: 10.4049/jimmunol.176.3.1741. [DOI] [PubMed] [Google Scholar]
- 9.Kaleeba JA, Berger EA. 2006. Kaposi’s sarcoma-associated herpesvirus fusion-entry receptor: cystine transporter xCT. Science 311:1921–1924. doi: 10.1126/science.1120878. [DOI] [PubMed] [Google Scholar]
- 10.Hahn AS, Kaufmann JK, Wies E, Naschberger E, Panteleev-Ivlev J, Schmidt K, Holzer A, Schmidt M, Chen J, Konig S, Ensser A, Myoung J, Brockmeyer NH, Sturzl M, Fleckenstein B, Neipel F. 2012. The ephrin receptor tyrosine kinase A2 is a cellular receptor for Kaposi’s sarcoma-associated herpesvirus. Nat Med 18:961–966. doi: 10.1038/nm.2805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.TerBush AA, Hafkamp F, Lee HJ, Coscoy L. 2018. A Kaposi’s sarcoma-associated herpesvirus infection mechanism is independent of integrins alpha3beta1, alphaVbeta3, and alphaVbeta5. J Virol 92:e00803-18. doi: 10.1128/JVI.00803-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen J, Sathiyamoorthy K, Zhang X, Schaller S, Perez White BE, Jardetzky TS, Longnecker R. 2018. Ephrin receptor A2 is a functional entry receptor for Epstein-Barr virus. Nat Microbiol 3:172–180. doi: 10.1038/s41564-017-0081-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang H, Li Y, Wang HB, Zhang A, Chen ML, Fang ZX, Dong XD, Li SB, Du Y, Xiong D, He JY, Li MZ, Liu YM, Zhou AJ, Zhong Q, Zeng YX, Kieff E, Zhang Z, Gewurz BE, Zhao B, Zeng MS. 2018. Ephrin receptor A2 is an epithelial cell receptor for Epstein-Barr virus entry. Nat Microbiol 3:164–171. doi: 10.1038/s41564-017-0080-8. [DOI] [PubMed] [Google Scholar]
- 14.Kania A, Klein R. 2016. Mechanisms of ephrin-Eph signalling in development, physiology and disease. Nat Rev Mol Cell Biol 17:240–256. doi: 10.1038/nrm.2015.16. [DOI] [PubMed] [Google Scholar]
- 15.Lisabeth EM, Falivelli G, Pasquale EB. 2013. Eph receptor signaling and ephrins. Cold Spring Harb Perspect Biol 5:a009159. doi: 10.1101/cshperspect.a009159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pasquale EB. 2010. Eph receptors and ephrins in cancer: bidirectional signalling and beyond. Nat Rev Cancer 10:165–180. doi: 10.1038/nrc2806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Oki M, Yamamoto H, Taniguchi H, Adachi Y, Imai K, Shinomura Y. 2008. Overexpression of the receptor tyrosine kinase EphA4 in human gastric cancers. World J Gastroenterol 14:5650–5656. doi: 10.3748/wjg.14.5650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee HY, Mohammed KA, Kaye F, Moudgil BM, Nasreen N. 2017. EphA2 targeted intratumoral therapy for non-small cell lung cancer using albumin mesospheres. Am J Transl Res 9:3293–3303. [PMC free article] [PubMed] [Google Scholar]
- 19.Hou F, Yuan W, Huang J, Qian L, Chen Z, Ge J, Wu S, Chen J, Wang J, Chen Z. 2012. Overexpression of EphA2 correlates with epithelial-mesenchymal transition-related proteins in gastric cancer and their prognostic importance for postoperative patients. Med Oncol 29:2691–2700. doi: 10.1007/s12032-011-0127-2. [DOI] [PubMed] [Google Scholar]
- 20.Saintigny P, Peng S, Zhang L, Sen B, Wistuba II, Lippman SM, Girard L, Minna JD, Heymach JV, Johnson FM. 2012. Global evaluation of Eph receptors and ephrins in lung adenocarcinomas identifies EphA4 as an inhibitor of cell migration and invasion. Mol Cancer Ther 11:2021–2032. doi: 10.1158/1535-7163.MCT-12-0030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yamaguchi S, Tatsumi T, Takehara T, Sakamori R, Uemura A, Mizushima T, Ohkawa K, Storkus WJ, Hayashi N. 2007. Immunotherapy of murine colon cancer using receptor tyrosine kinase EphA2-derived peptide-pulsed dendritic cell vaccines. Cancer 110:1469–1477. doi: 10.1002/cncr.22958. [DOI] [PubMed] [Google Scholar]
- 22.de Marcondes PG, Bastos LG, de-Freitas-Junior JC, Rocha MR, Morgado-Diaz JA. 2016. EphA4-mediated signaling regulates the aggressive phenotype of irradiation survivor colorectal cancer cells. Tumor Biol 37:12411–12422. doi: 10.1007/s13277-016-5120-0. [DOI] [PubMed] [Google Scholar]
- 23.Brantley-Sieders DM, Jiang A, Sarma K, Badu-Nkansah A, Walter DL, Shyr Y, Chen J. 2011. Eph/ephrin profiling in human breast cancer reveals significant associations between expression level and clinical outcome. PLoS One 6:e24426. doi: 10.1371/journal.pone.0024426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Batson J, Maccarthy-Morrogh L, Archer A, Tanton H, Nobes CD. 2014. EphA receptors regulate prostate cancer cell dissemination through Vav2-RhoA mediated cell-cell repulsion. Biol Open 3:453–462. doi: 10.1242/bio.20146601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pertel PE. 2002. Human herpesvirus 8 glycoprotein B (gB), gH, and gL can mediate cell fusion. J Virol 76:4390–4400. doi: 10.1128/JVI.76.9.4390-4400.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Omerović J, Longnecker R. 2007. Functional homology of gHs and gLs from EBV-related gamma-herpesviruses for EBV-induced membrane fusion. Virology 365:157–165. doi: 10.1016/j.virol.2007.03.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chakraborty S, Veettil MV, Chandran B. 2012. Kaposi’s sarcoma associated herpesvirus entry into target cells. Front Microbiol 3:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hahn AS, Desrosiers RC. 2013. Rhesus monkey rhadinovirus uses eph family receptors for entry into B cells and endothelial cells but not fibroblasts. PLoS Pathog 9:e1003360. doi: 10.1371/journal.ppat.1003360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Binns KL, Taylor PP, Sicheri F, Pawson T, Holland SJ. 2000. Phosphorylation of tyrosine residues in the kinase domain and juxtamembrane region regulates the biological and catalytic activities of Eph receptors. Mol Cell Biol 20:4791–4805. doi: 10.1128/MCB.20.13.4791-4805.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kullander K, Mather NK, Diella F, Dottori M, Boyd AW, Klein R. 2001. Kinase-dependent and kinase-independent functions of EphA4 receptors in major axon tract formation in vivo. Neuron 29:73–84. doi: 10.1016/S0896-6273(01)00181-7. [DOI] [PubMed] [Google Scholar]
- 31.Swidergall M, Solis NV, Lionakis MS, Filler SG. 2018. EphA2 is an epithelial cell pattern recognition receptor for fungal beta-glucans. Nat Microbiol 3:53–61. doi: 10.1038/s41564-017-0059-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Aaron PA, Jamklang M, Uhrig JP, Gelli A. 2018. The blood-brain barrier internalises Cryptococcus neoformans via the EphA2-tyrosine kinase receptor. Cell Microbiol 20:e12811. doi: 10.1111/cmi.12811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lupberger J, Zeisel MB, Xiao F, Thumann C, Fofana I, Zona L, Davis C, Mee CJ, Turek M, Gorke S, Royer C, Fischer B, Zahid MN, Lavillette D, Fresquet J, Cosset FL, Rothenberg SM, Pietschmann T, Patel AH, Pessaux P, Doffoel M, Raffelsberger W, Poch O, McKeating JA, Brino L, Baumert TF. 2011. EGFR and EphA2 are host factors for hepatitis C virus entry and possible targets for antiviral therapy. Nat Med 17:589–595. doi: 10.1038/nm.2341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bonaparte MI, Dimitrov AS, Bossart KN, Crameri G, Mungall BA, Bishop KA, Choudhry V, Dimitrov DS, Wang LF, Eaton BT, Broder CC. 2005. Ephrin-B2 ligand is a functional receptor for Hendra virus and Nipah virus. Proc Natl Acad Sci U S A 102:10652–10657. doi: 10.1073/pnas.0504887102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Negrete OA, Levroney EL, Aguilar HC, Bertolotti-Ciarlet A, Nazarian R, Tajyar S, Lee B. 2005. EphrinB2 is the entry receptor for Nipah virus, an emergent deadly paramyxovirus. Nature 436:401–405. doi: 10.1038/nature03838. [DOI] [PubMed] [Google Scholar]
- 36.Naranatt PP, Akula SM, Chandran B. 2002. Characterization of gamma2-human herpesvirus-8 glycoproteins gH and gL. Arch Virol 147:1349–1370. doi: 10.1007/s00705-002-0813-7. [DOI] [PubMed] [Google Scholar]
- 37.Hahn AS, Desrosiers RC. 2014. Binding of the Kaposi’s sarcoma-associated herpesvirus to the ephrin binding surface of the EphA2 receptor and its inhibition by a small molecule. J Virol 88:8724–8734. doi: 10.1128/JVI.01392-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Großkopf AK, Ensser A, Neipel F, Jungnickl D, Schlagowski S, Desrosiers RC, Hahn AS. 2018. A conserved Eph family receptor-binding motif on the gH/gL complex of Kaposi’s sarcoma-associated herpesvirus and rhesus monkey rhadinovirus. PLoS Pathog 14:e1006912. doi: 10.1371/journal.ppat.1006912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McShane MP, Longnecker R. 2004. Cell-surface expression of a mutated Epstein-Barr virus glycoprotein B allows fusion independent of other viral proteins. Proc Natl Acad Sci U S A 101:17474–17479. doi: 10.1073/pnas.0404535101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Myoung J, Ganem D. 2011. Generation of a doxycycline-inducible KSHV producer cell line of endothelial origin: maintenance of tight latency with efficient reactivation upon induction. J Virol Methods 174:12–21. doi: 10.1016/j.jviromet.2011.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fan Q, Longnecker R. 2010. The Ig-like v-type domain of paired Ig-like type 2 receptor alpha is critical for herpes simplex virus type 1-mediated membrane fusion. J Virol 84:8664–8672. doi: 10.1128/JVI.01039-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.McShane MP, Longnecker R. 2005. Analysis of fusion using a virus-free cell fusion assay. Methods Mol Biol 292:187–196. [DOI] [PubMed] [Google Scholar]
- 43.Atanasiu D, Saw WT, Gallagher JR, Hannah BP, Matsuda Z, Whitbeck JC, Cohen GH, Eisenberg RJ. 2013. Dual split protein-based fusion assay reveals that mutations to herpes simplex virus (HSV) glycoprotein gB alter the kinetics of cell-cell fusion induced by HSV entry glycoproteins. J Virol 87:11332–11345. doi: 10.1128/JVI.01700-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ishikawa H, Meng F, Kondo N, Iwamoto A, Matsuda Z. 2012. Generation of a dual-functional split-reporter protein for monitoring membrane fusion using self-associating split GFP. Protein Eng Des Sel 25:813–820. doi: 10.1093/protein/gzs051. [DOI] [PubMed] [Google Scholar]
- 45.Möhl BS, Sathiyamoorthy K, Jardetzky TS, Longnecker R. 2014. The conserved disulfide bond within domain II of Epstein-Barr virus gH has divergent roles in membrane fusion with epithelial cells and B cells. J Virol 88:13570–13579. doi: 10.1128/JVI.02272-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available within this article and its supplemental information files or, upon request, the relevant information from the corresponding author.