Summary
Objective
Despite the myriad negative effects of weight self‐stigma, its role in weight loss intervention has not been thoroughly examined. The aim of this study was to examine the association between weight self‐stigma and weight loss.
Methods
This longitudinal study examined the association between weight loss and changes in self‐stigma, assessed by the Weight Self‐Stigma Questionnaire, which distinguished between self‐devaluation and fear of enacted stigma. Participants were adults with overweight or obesity enrolled in a 24‐month weight loss intervention trial (groups were collapsed for this post hoc analysis) who were assessed at baseline, 6, 12, 18 and 24 months.
Results
Baseline levels of self‐stigma were not associated with weight loss outcomes. However, mixed models analysis showed that reductions in one aspect of weight self‐stigma, self‐devaluation, was associated with greater weight loss (p = 0.01). Cross products mediation analysis showed that increases in use of weight control strategies mediated the association between reductions in self‐devaluation and greater weight loss (F = 14.86, p < 0.001; CI 0.09–0.37).
Conclusions
Results suggest that there may be potential for incorporating intervention methods targeting the reduction of self‐stigma in order to improve weight loss outcomes.
Keywords: Obesity, Overweight, Stigma, Weight loss
Introduction
People with obesity are frequently exposed to bias, discrimination and ridicule 1, 2, 3, 4, 5, 6 and are almost universally ascribed negative characteristics 7, 8, 9. The direct experience of weight‐related stigma is associated with a myriad of poor psychosocial outcomes 1, 5, 10 as well as reduced engagement in health behaviours 11. The effects of weight‐based stigma can become more severe when they are internalized (referred to hereafter as ‘weight self‐stigma’) 12, 13, 14, and thus, researchers have called for intervention development to address weight self‐stigma in treatment settings 5, 15.
Currently, there is little known about whether baseline levels of self‐stigma are related to weight loss success and/or about interrelations among change in self‐stigma, weight control behaviours and weight. Weight loss is associated with modest improvements in psychological outcomes 16, 17 and thus could also potentially reduce weight self‐stigma, perhaps in part due to positive feedback from others for successful weight loss efforts. Alternatively, participating in weight loss intervention could reinforce weight loss stereotypes (e.g. that weight is entirely within an individual's control) which could exacerbate stigma.
Researchers have distinguished between two types of self‐stigma – self‐devaluation and fear of enacted stigma – that result from one's identification with a stigmatized group 18, 19. Specifically, self‐devaluation is the internalization of negative beliefs about oneself and association with negative characteristics due to the stigmatization. Fear of enacted stigma is the fear that others will have unfavourable attitudes and engage in ridicule, bias or discrimination towards the individual. In short, self‐stigma is when individuals come to associate themselves with negative characteristics and fear that others will too.
Studies on the self‐devaluation component of weight self‐stigma have been mixed. Some studies have shown small reductions in self‐devaluation following completion of short‐term healthy eating or weight management programmes 20, 21, whereas another found no significant association between changes in weight and self‐devaluation 22. The role of baseline self‐devaluation in weight loss success has yet to be established, with one cross‐sectional study suggesting that higher baseline self‐devaluation predicted poorer weight maintenance 15 and another study finding no relationship between baseline self‐devaluation and weight loss 23. Only one study examined fear of enacted stigma in the context of weight loss and found that baseline fear of enacted stigma predicted less weight loss 3 months later after controlling for demographics, eating problems and psychological symptoms 23. No studies have examined the effect of participation in a weight loss programme on fear of enacted stigma.
The current observational study is a set of exploratory analyses that examine the relationship between weight self‐stigma and weight change in a recently published randomized trial evaluating two different weight loss treatments. This trial compared a 12‐month acceptance‐based behavioural intervention (ABBI) to a standard behavioural treatment (SBT) for weight loss among 162 adults with overweight and obesity who reported high internal disinhibition. Overall weight change (baseline to 24 months, reported previously) was −4.2% for ABBI and −2.4% for SBT, a non‐significant difference. However, during the post‐treatment phase (12–24 months), the ABBI group regained significantly less weight than SBT (4.6 kg for ABBI vs. 7.1 kg for SBT, p = 0.005) 24.
The current study aims were to (a) examine baseline weight self‐stigma means in the context of demographic variables and previously published norms, (b) test whether weight self‐stigma was reduced or increased in the course of exposure to weight loss intervention, (c) examine whether there were associations between weight self‐stigma variables and weight change and (d) explore adherence to weight control strategies as a potential pathway by which weight self‐stigma might influence weight change in the context of a weight loss intervention.
Methods
Design
The current study was a longitudinal examination of weight self‐stigma, weight control behaviours and weight change in the context of weight loss interventions with assessments occurring at baseline, 6, 12, 18 and 24 months. The original study compared two behavioural weight loss intervention across 32 sessions over 12 months in a faded contact design 24, 25. The full details of the study procedures and primary results can be found elsewhere 24, 25; however, relevant aspects are reviewed here. For the purpose of the current study, data were collapsed across treatment conditions because there were no significant differences between groups on weight self‐stigma at any time point.
Participants
Participants (N = 162) were 18–70 years of age, had a baseline body mass index (BMI) between 30 and 50 kg m−2 and reported elevated levels of internal disinhibition (defined as a score of 5 or higher for women or 4 or higher for men on the internal disinhibition subscale of the eating inventory). A detailed description of the screening process and establishment of the internal disinhibition cut‐off can be found in the study protocol 25. All participants from the original trial were used in the current study.
Measures
Anthropometric
Weight was measured to the nearest 0.1 kg using a digital scale, and height was measured to the nearest millimetre with a stadiometer, using standardized procedures, and used to calculate BMI (kg m−2). Percent weight loss was used as the measure of change while baseline BMI was used as a covariate where appropriate in the analyses.
Weight Self‐Stigma Questionnaire (WSSQ)
The WSSQ is a 12‐item measure of weight self‐stigma using a 5‐point Likert‐type rating that ranges from ‘completely disagree’ to ‘completely agree’ 19. It contains two subscales: self‐devaluation and fear of enacted stigma. The self‐devaluation subscale contains six items that pertain to ascribing personal blame and endorsing negative characteristics because of one's weight. For example, one question reads, ‘I became overweight because I am a weak person’. The fear of enacted stigma subscale contains six items that assess the degree to which someone is concerned with the possibility of being the target of ridicule, bias or discrimination because of one's weight. For example, one question reads, ‘Others will think I lack self‐control because of my weight problems’. Total weight self‐stigma and its subcomponents have demonstrated adequate internal consistency and construct validity 19. In the current study, the full scale WSSQ Cronbach's Alpha was 0.86, the self‐devaluation subscale was 0.80 and the fear of enacted subscale was 0.86.
Weight Control Strategies Scale (WCSS)
The WCSS is a 30‐item self‐report measure used to assess the use of specific strategies for losing or maintaining weight loss 26. The WCSS contains four subscales: dietary choices, self‐monitoring strategies, physical activity and psychological coping. Higher scores indicate greater use of weight control strategies. The WCSS has been shown to have good reliability and validity for use in overweight and obese weight loss treatment‐seeking samples 26. In the current study, the full scale WCSS Cronbach's Alpha was 0.89.
Statistical analysis
All analyses were completed using IBM SPSS Statistics software version 24 for PC in 2018. Differences in baseline characteristics between groups were examined using independent samples t‐test and chi square analysis. Chi square and Pearson correlations were used to examine associations of gender and age on baseline levels of both self‐devaluation and fear of enacted stigma.
Change in weight, weight self‐stigma and use of weight control strategies were analysed with linear and nonlinear mixed effects models. Unconditional models were used to determine whether a linear or nonlinear trend best fit the longitudinal trajectory of the outcomes (non‐linear was the best fit for weight loss; linear was better for all other analyses), and to evaluate the variance components associated with the slope of time to determine assignment as fixed versus random effects (intercepts and slopes were treated as random effects in all models). The unit of time was represented as months from baseline. All significance tests were two‐tailed, with alpha set to 0.05. Overall estimated marginal means were calculated using the linear mixed modelling procedure described earlier. The analytic approach accommodated missing data by making use of all available data from all randomized participants.
The impact of change in weight self‐stigma on change in weight was examined in a similar manner using the linear and non‐linear mixed effects models described previously; however, percent weight change was used as the dependent variable (DV) with change in weight self‐stigma and the use of weight control strategies as the predictor variables.
Finally, an examination of possible pathways for the impact of weight self‐stigma on weight change was conducted. The use of weight control strategies was proposed as a potential mediator as it represents the degree to which individuals use the common strategies taught in behaviour weight loss. Mediation analyses were performed for any weight self‐stigma variable that showed a significant association with weight change (only self‐devaluation) using post‐treatment (12 months) change in weight self‐stigma as the independent variable (IV), post‐treatment change in the use of weight control strategies as the mediator and 24‐month percent weight change as the DV. Mediation was tested by assessing the significance of the cross product of the coefficients for the IV to mediator relation (the a path), and the mediator to outcome relation controlling for treatment (the b path), using a well‐validated and widely utilized bootstrapped procedure 27, 28, 29. Parameter estimates were based on 5,000 bootstrap samples. The point estimate of the indirect cross product is the mean for these 5,000 samples which ensures stability of the analyses; the bias corrected and accelerated 95% confidence intervals are similar to the 2.5 and 97.5 percentile scores of the obtained distribution over the samples, but with z‐score based corrections for bias due to the underlying distribution 28, 29. Thus, if the confidence intervals do not contain zero, the point estimate is significant at the level indicated.
Results
Baseline characteristics
As shown in Table 1, the sample was primarily female, non‐Hispanic White and middle aged. Baseline weight self‐stigma levels were consistent with published norms for weight loss treatment‐seeking adults with overweight and obesity (treatment‐seeking full scale norm M = 35.98; self‐devaluation M = 19.32; fear of enacted M = 16.66) 19. There were no significant differences between genders on mean baseline score for self‐devaluation (Men = 19.75 vs. Women = 20.53; p = 0.452) or fear of enacted stigma (Men = 15.58 vs. Women = 17.51; p = 0.116). There were no significant differences when comparing White participants to participants from racial or ethnic minority groups for self‐devaluation (White = 20.46 vs. non‐White = 19.94; p = 0.659) or fear of enacted stigma (White = 17.34 vs. non‐White = 16.23; p = 0.437). Pearson correlations between age and self‐devaluation (r = −0.07) and fear of enacted stigma (r = −0.12) were not significant. BMI was significantly correlated with fear of enacted stigma (r = 0.25; p = 0.001) but not self‐devaluation (r = 0.02; p = 0.801).
Table 1.
Baseline characteristics of participants
| Characteristics | (N = 162) |
|---|---|
| Sex, N (%) | |
| Female | 138 (85) |
| Male | 24 (12) |
| Race/ethnicity, N (%) | |
| Black/African American | 8 (5) |
| Hispanic White | 10 (6) |
| Asian | 2 (1) |
| White (non‐Hispanic) | 142 (88) |
| Education, N (%) | |
| High school/G.E.D. | 12 (7.5) |
| Some college/vocational | 44 (28) |
| Bachelor's degree | 58 (36.5) |
| Graduate or professional | 45 (28) |
| Age (year) | 50.2 ± 10.9 |
| Weight (kg) | 102.3 ± 17.4 |
| BMI (kg m−2) | 37.6 ± 5.3 |
| Weight Self‐Stigma Total | 37.6 ± 8.7 |
| Self‐devaluation | 20.4 ± 4.7 |
| Fear of enacted stigma | 17.2 ± 5.5 |
| Weight control strategies | 1.3 ± 0.5 |
Values shown are mean ± standard deviation.
Changes over time
Table 2 shows the results of the mixed effects models analysis. Overall change in weight was significant, with participants losing the most weight at 6 months and then gradually regaining over time. Reductions in self‐devaluation and increased in the use of weight control strategies followed a similar pattern. Change in WSSQ full scale and fear of enacted stigma over time was not significant.
Table 2.
Mean changes in study variables from baseline and overall estimated marginal mean and p value from multi‐level modeling (MLM) analysis
| 6M | 12M | 18M | 24M | MLM overall EM mean | MLM time p values | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | M | SD | |||
| Percent weight loss | −9.87 | 6.08 | −9.16 | 8.54 | −6.23 | 7.90 | −4.29 | 7.32 | −7.74 | <0.001 |
| Weight self‐stigma full scale | −6.45 | 8.36 | −7.64 | 9.82 | −6.66 | 9.21 | −5.39 | 8.64 | −6.45 | 0.099 |
| Self‐devaluation | −3.94 | 4.88 | −4.02 | 5.70 | −3.02 | 5.18 | −2.32 | 4.79 | −3.29 | <0.001 |
| Fear of enacted stigma | −2.52 | 4.72 | −3.62 | 5.33 | −3.64 | 5.52 | −3.08 | 4.96 | −3.16 | 0.127 |
| Weight control strategies | 2.65 | 0.65 | 2.21 | 0.72 | 1.95 | 0.66 | 1.95 | 0.66 | 0.89 | <0.001 |
Variables associated with weight change
Losing weight was significantly associated with reduction in self‐devaluation and increased use of weight control strategies. There were no significant effects for baseline BMI, baseline self‐devaluation and baseline weight control strategies. See Table 3 for results.
Table 3.
Mixed models results for changes in weight
| Source | Estimate | SE | t | p |
|---|---|---|---|---|
| Intercept | −9.67 | 4.09 | −2.37 | 0.022 |
| Time | 0.01 | 0.00 | 3.01 | 0.003 |
| Baseline BMI | 0.08 | 0.07 | 1.08 | 0.286 |
| Baseline self‐devaluation | 0.17 | 0.10 | 1.74 | 0.088 |
| Self‐devaluation Δ | 0.13 | 0.05 | 2.59 | 0.011 |
| Baseline weight control strategies | −1.18 | 0.85 | −1.39 | 0.173 |
| Weight control strategies Δ | −3.15 | 0.35 | −8.97 | <0.001 |
Mediation model for the impact of self‐devaluation on percent change in weight
Given that the only weight self‐stigma variable significantly associated with weight change was change in self‐devaluation, one mediation analysis was performed using change in self‐devaluation as the IV, change in the use of weight control strategies as the mediator and percent weight change as the DV. Bias‐corrected 95% confidence intervals showed that changes in use of weight control strategies mediated changes in weight (F = 14.86, p < 0.001; CI 0.09–0.37). Figure 1 shows the path analysis betas and p values. Both self‐devaluation to mediator paths (a) were significant, the mediator to weight change path (b) was significant and the effect of the self‐devaluation to weight change (c path) was significantly altered when taking into account the mediator (c' or mediated intervention path), indicating that mediation was observed. Given that self‐devaluation and weight control strategies were measured at the same time, an examination was conducted to determine the possibility that self‐devaluation, rather than use of weight control strategies, was the mediator. The reverse mediation model was tested using change in the use of weight control strategies as the IV and change in self‐devaluation as the mediator. Bias‐corrected 95% confidence intervals showed that changes in self‐devaluation did not mediate changes in weight in this model (CI −0.94–0.39; the c path was not significantly altered when taking into account the mediator).
Figure 1.
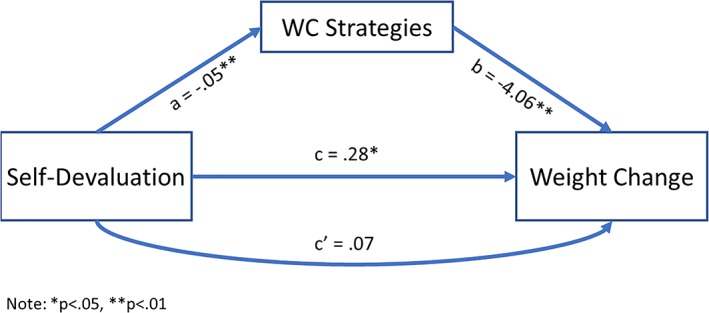
Results of mediation analysis.
Discussion
The currents study is the first to examine the relationship between both aspects of weight self‐stigma, self‐devaluation and fear of enacted stigma, with weight loss in the context of a behavioural weight loss intervention study. Decreases in self‐devaluation were associated with reductions in weight, and greater increases in the use of weight control strategies mediated the relationship between change in self‐devaluation and change in weight. Importantly, participation in the weight loss programme did not exacerbated self‐stigma in the current study.
Self‐devaluation decreased significantly over time, despite the fact that it was not targeted in treatment, and decreases in self‐devaluation were associated with reductions in weight. Although contrary findings exist, the observed association between self‐devaluation and weight change adds support to previous studies with similar results. However, it is unclear how to account for the observed change given that self‐devaluation was not explicitly targeted in either intervention. One possibility is that self‐devaluation decreases as a function of the non‐specific factors involved in group treatment, such as social support and therapist contact. Additionally, participants might improve in competence and confidence as they make significant behavioural changes as part of behavioural weight loss, and thus experience improvements in self‐devaluation as a result. A third possibility is that losing weight leads to reduced self‐devaluation, due at least in part to the change in one's body shape. This study is post hoc and exploratory in nature, precluding a strong interpretation; however, these possibilities can be tested empirically in future studies.
The mediation analysis found that increases in the use of weight control strategies mediated the effect of change in self‐devaluation on weight change. In other words, the data suggest that as individuals adopt a less stigmatizing stance towards themselves, they may engage in more weight control behaviours, which in turn improves weight loss. Importantly, a second mediation analysis found no evidence to support the reverse model (that as individuals use more weight control strategies they take a less stigmatizing stance, thus improving weight loss). Nonetheless, it is important to note that these findings are preliminary given the IV and mediator were measured contiguously.
If we assume the validity of the mediation analysis findings, it would have important implications as it suggests that stigma reduction could be a new target to address in treatment to potentially improve weight loss outcomes. Stigma reduction interventions currently exist and have been applied to weight stigma, and thus, harnessing existing intervention methods would not be particularly difficult. For example, a recent intervention taught mindfulness and acceptance skills to increase the awareness and reduce the believability of stigmatizing thoughts in order to reduce the impact of self‐stigma on health behaviour with positive results 30. Given the wide‐ranging impact of stigma on mental health, there could be additional benefits to targeting it in behavioural weight loss in improving overall mental health functioning. This could be important as even successful participants often remain overweight or obese, keeping them at high risk for stigma. Future studies also need to examine whether targeting self‐devaluation directly in treatment could lead to greater changes in self‐devaluation than observed in the current study, and whether greater reductions in self‐devaluation could lead to greater weight loss.
Baseline levels of weight self‐stigma in this study were consistent with previous research using weight loss treatment‐seeking adults with overweight or obesity, which is about a half standard deviation above non‐treatment seeking adults. Baseline levels of self‐devaluation and fear of enacted stigma were not associated with weight loss, suggesting that weight self‐stigma is not a limiting factor in regard to behavioural weight loss treatment success. Baseline BMI was associated with fear of enacted stigma, which makes sense given that individuals with a higher BMI become more likely targets of bias, discrimination and ridicule. Also of note, no associations were found for age, gender or racial or ethnic minority status and weight self‐stigma.
Fear of enacted stigma did not change significantly over the course of treatment and no relationship was observed between fear of enacted stigma and weight loss. This suggests that one's assumptions about how they will be treated by others may be resistant to change despite the fact that improvements in self‐concept may be attainable through intervention. Individuals may need to experience substantial changes in body shape coupled with repeated exposure to previously stigmatizing contexts before meaningful changes in fear of enacted stigma can be observed given how pervasive weight‐based stigmatization is.
This study has strengths including a relatively large sample, a 2‐year timeline and multiple assessments to allow for some testing of sequence of change. The study is limited by a relatively homogenous sample consisting mostly of White middle‐aged women. Another major limitation of the study is the infrequent measurement of change in self‐stigma and change in the use of weight control strategies.
The current analysis was a post hoc longitudinal examination of the association between change in weight self‐stigma, weight control behaviours and weight loss. Reductions in one aspect of weight self‐stigma, self‐devaluation, was associated with improved weight loss and increases in the use of weight control strategies mediated the association between reductions in self‐devaluation and greater weight loss. Thus, there may be potential for incorporating intervention methods targeting the reduction of self‐stigma in order to improve obesity outcomes via improved adherence to the use of recommended weight control strategies.
Funding
This study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases (R01DK087704; K23DK097143).
Conflict of Interest statement
The authors declare that they have no conflict of interest.
Registration
Clinicaltrials.org #NCT01461421; https://www.clinicaltrials.gov/ct2/show/NCT01461421
Lillis, J. , Thomas, J. G. , Olson, K. , and Wing, R. R. (2019) Weight self‐stigma and weight loss during behavioural weight loss intervention. Obesity Science & Practice, 5: 21–27. 10.1002/osp4.314.
References
- 1. Puhl R, Heuer CA. The stigma of obesity: a review and update. Obesity 2009; 17: 941–964. [DOI] [PubMed] [Google Scholar]
- 2. Carr D, Friedman MA. Is obesity stigmatizing? Body weight, perceived discrimination, and psychological well‐being in the United States. J Health Soc Behav 2005; 46: 244–259. [DOI] [PubMed] [Google Scholar]
- 3. Maranto CL, Stencien AF. Weight discrimination: a multidisciplinary analysis. Employee Responsibilities Rights J 2000; 12: 9–24. [Google Scholar]
- 4. Karnehed N, Rasmussen F, Hemmingsson T, Tylnelius P. Obesity and attained education: cohort study of more than 700,000 Swedish men. Obesity 2006; 14: 1421–1428. [DOI] [PubMed] [Google Scholar]
- 5. Puhl RM, Heuer CA. Obesity stigma: important considerations for public health. Am J Public Health 2010; 100: 1019–1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Schwartz MB, Chambliss HO, Brownell KD, Blair SN, Billington C. Weight bias among health professionals specializing in obesity. Obes Res 2003; 11: 1033–1039. [DOI] [PubMed] [Google Scholar]
- 7. Allon N. The stigma of overweight in everyday life In: Woldman BB. (ed.). Psychological Aspects of Obesity. Van Nostrand Reinhold: New York, 1982, pp. 130–174. [Google Scholar]
- 8. Allison DB, Basile VC, Yuker HE. The measurement of attitudes toward and beliefs about obese persons. Int J Eat Disord 1991; 10: 599–607. [Google Scholar]
- 9. Weiner B. Judgments of Responsibility: A Theory of Social Conduct. Guilford: New York, 1995. [Google Scholar]
- 10. Puhl R, Brownell KD. Bias, discrimination, and obesity. Obes Res 2001; 9: 788–805. [DOI] [PubMed] [Google Scholar]
- 11. Tomiyama AJ. Weight stigma is stressful. A review of evidence for the cyclic obesity/weight‐based stigma model. Appetite 2014; 82: 8–15. [DOI] [PubMed] [Google Scholar]
- 12. Lillis J, Levin ME, Hayes SC. Exploring the relationship between body mass index and health‐related quality of life: a pilot study of the impact of weight self‐stigma and experiential avoidance. J Health Psychol 2011; 16: 722–727. [DOI] [PubMed] [Google Scholar]
- 13. Friedman KE, Reichmann SK, Costanzo PR, Zelli A, Ashmore JA, Musante GJ. Weight stigmatization and ideological beliefs: relation to psychological functioning in obese adults. Obes Res 2005; 13: 907–916. [DOI] [PubMed] [Google Scholar]
- 14. Puhl R, Brownell KD. Confronting and coping with weight stigma: an investigation of overweight and obese adults. Obesity 2006; 14: 1802–1815. [DOI] [PubMed] [Google Scholar]
- 15. Puhl RM, Quinn DM, Weisz BM, Suh YJ. The role of stigma in weight loss maintenance among US adults. Ann Behav Med 2017; 51: 754–763. [DOI] [PubMed] [Google Scholar]
- 16. Kolotkin RL, Crosby RD, Williams GR, Hartley GG, Nicol S. The relationship between health‐related quality of life and weight loss. Obes Res 2001; 9: 564–571. [DOI] [PubMed] [Google Scholar]
- 17. Sarwer DB, Moore RH, Diewald LK, et al. The impact of a primary care‐based weight loss intervention on the quality of life. Int J Obes (Lond) 2013; 37: S25–S30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Link BG, Phelan JC. Conceptualizing stigma. Annu Rev Sociol 2001; 27: 363–385. [Google Scholar]
- 19. Lillis J, Luoma J, Levin M, Hayes SC. Measuring weight self stigma: the Weight Stigma Questionnaire. Obesity 2010; 18: 971–976. [DOI] [PubMed] [Google Scholar]
- 20. Carels RA, Burmeister JM, Koball AM, et al. A randomized trial comparing two approaches to weight loss: differences in weight loss maintenance. J Health Psychol 2014; 19: 296–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Mensinger JL, Calogero RM, Tylka TL. Internalized weight stigma moderates eating behavior outcomes in women with high BMI participating in a healthy living program. Appetite 2016; 102: 32–43. [DOI] [PubMed] [Google Scholar]
- 22. Carels RA, Wott CB, Young KM, Gumble A, Koball A, Oehlhof MW. Implicit, explicit, and internalized weight bias and psychosocial maladjustment among treatment‐seeking adults. Eat Behav 2010; 11: 180–185. [DOI] [PubMed] [Google Scholar]
- 23. Lillis J, Thomas JG, Levin ME, Wing RR. Self‐stigma and weight loss: the impact of being stigmatized. J Health Psychol 2017. 10.1177/1359105317739101, 135910531773910. [DOI] [PubMed] [Google Scholar]
- 24. Lillis J, Niemeier HM, Thomas JG, et al. A randomized trial of an acceptance‐based behavioral intervention for weight loss in people with high internal disinhibition. Obesity 2016; 24: 2509–2514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lillis J, Niemeier HM, Ross KM, et al. Weight loss intervention for individuals with high internal disinhibition: design of the acceptance based behavioral intervention (ABBI) randomized controlled trial. BMC Psychol 2015; 3: 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Pinto AM, Fava JL, Raynor HA, LaRose JG, Wing RR. Development and validation of the Weight Control Strategies Scale. Obesity 2013; 21: 2429–2436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods 2002; 7: 83–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instrum Comput 2004; 36: 717–731. [DOI] [PubMed] [Google Scholar]
- 29. Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods 2008; 40: 879–891. [DOI] [PubMed] [Google Scholar]
- 30. Levin ME, Potts S, Haeger J, Lillis J. Delivering acceptance and commitment therapy for weight self‐stigma through guided self‐help: results from an open pilot trial. Cogn Behav Pract 2018; 25: 87–104. [Google Scholar]


