Abstract
Context. Pediatricians working toward health equity require health care delivery mechanisms that take on dual roles: mitigating the health effects of a maladaptive social ecosystem while simultaneously working to improve the ecosystem itself. School-based health centers (SBHCs) perform these dual roles by providing medical, mental/behavioral, dental, and vision care directly in schools where young people spend the majority of their time, maximizing their opportunity to learn and grow. Evidence Acquisition. Databases were searched extensively for research studies published between January 2000 and December 2018. Evidence Synthesis. The authors began with 3 recent high-impact reviews that covered SBHC history, health outcomes, cost-benefit, and impact on health equity. Informed by these articles, the authors organized the evidence into 4 broad categories of impact: Financial, Physical Health (including medical, vision, and dental), Mental Health, and Educational Outcomes. Using these 4 categories, the authors then performed a robust literature search using PubMed for studies that fit into these themes. Conclusions. SBHCs increase access to health services for children, families, and communities, which ultimately leads to positive short- and long-term outcomes in service of a broad range of stakeholders. Educational impact requires further attention on both outcomes and methodological approaches. Three current public health topics of importance were identified that SBHCs might be well-suited to address: Youth Gun Violence, Adverse Childhood Experiences, and the Health of American Indian/Alaskan Native communities in the United States.
Keywords: school based health, mental health, behavioral health, adverse childhood experiences, gun violence, American Indian and Alaskan native health
Pediatricians working toward health equity require health care delivery mechanisms that take on dual roles: mitigating the health effects of a maladaptive social ecosystem while simultaneously working to improve the ecosystem itself.1 School-based health centers (SBHCs) sustainably perform these dual roles. SBHCs place critically needed services like medical, mental, dental, and vision care directly in schools where young people spend the majority of their time, maximizing their opportunity to learn and grow. SBHCs collaborate with the school nurse and augment the health care services a child may already have access to. If a child lacks access to care, SBHCs can serve as a primary medical home.2 Being located in schools, factors such as transportation issues, parent availability, and missed appointments are greatly reduced.3
SBHCs operate within two of the most heavily regulated sectors in the United States—education and health. Thus, SBHCs have to display superior health and educational outcomes, while also being as financially sustainable as traditional pediatric primary care services.4 This narrative review begins with a summary of the structure and latest policy initiatives related to SBHCs. Next the evidence pertaining to financial, physical, mental, and educational impact of SBHCs is evaluated. Finally, the authors explore the impact SBHCs might have on 3 current public health challenges that are closely tied to both education and health care sectors in the United States. These are gun violence in schools, adverse childhood experiences (ACE), and the rising premature death rates of young people in the American Indian and Alaskan Native (AI/AN) community.
Methods
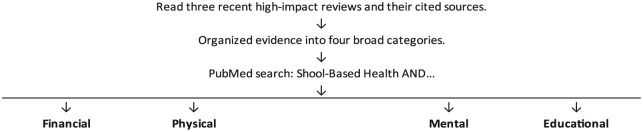
The authors conducted a literature search to review the current evidence pertaining to SBHCs (Figure 1). The authors began with 3 recent high-impact reviews that covered SBHC history, health outcomes, cost-benefit, and impact on health equity.3,5,6 Informed by these articles, the authors organized evidence according to 4 broad categories (financial, physical, mental, and educational outcomes). Using these 4 categories, the authors then performed a robust search using PubMed for literature that would fit into these themes. The PubMed search began by reviewing abstracts of sources cited in the 3 above-mentioned review articles. In addition, keyword and MESH search in PubMed was conducted using the following: (“SBHC” OR “school based health”) AND (“financial OR economic OR cost OR “Delivery of Health Care/economics”[Mesh] OR “Health Care Costs”[Mesh]”), (“medical OR “Diseases Category”[Majr] OR “Diagnosis”[Majr]”), (“mental OR behavioral OR “Mental Health”[Mesh] OR “Psychiatry and Psychology Category”[Majr]) OR “Behavioral Medicine”[Majr]”), and (“Education[Majr]”).
Figure 1.
Literature review process.
In total, more than 300 articles were examined for this review. Inclusion criteria included peer-review articles whose main findings related to financial, physical, mental, or educational outcomes (Table 1). A study was excluded if it was written prior to year 2000 or did not relate to categories of interest. When possible, the authors highlighted evidence that had not been incorporated into prior reviews of SBHCs. Each author was given 1 of the 4 categories to research and draft their review. The initial decision to include an article from a given category required only one author. The first author was then responsible for reviewing the evidence, collating each section, and ensuring studies were cited appropriately.
Table 1.
Inclusion and Exclusion criteria.
| Inclusion | Exclusion |
|---|---|
| Article was cited in review articles by Keeton et al5 (2012), Knopf et al3 (2016), or Ran et al6 (2016). | Published prior to January 1, 2000 |
| Article discussed financial, medical, mental/behavioral, or educational impact of SBHCs. | |
| Article discussed 3 public health concerns: gun violence, ACEs, and AI/AN populations. |
Abbreviations: SBHC, school-based health center; ACEs, adverse childhood experiences; AI/AN, American Indian/Alaskan Native.
For the purposes of identifying future directions, 3 current topics were identified by the authors as having particular public health importance that SBHCs might be well-suited to address: youth gun violence, adverse childhood experiences (ACEs), and the health of American Indian/Alaskan Native (AI/AN) communities in the United States. The terms used to identify literature on these 3 topics were (“Adverse Childhood Experiences OR toxic stress OR child trauma”), (“American Indian OR Alaskan native OR native American”), and (“gun violence OR firearm”). For this second literature search, the decision to include an article or not was left to the first author. Literature review began in October 2017 and concluded in December 2018.
Ethical Approval and Informed Consent
Ethics approval was not required for this systematic review. Informed consent was not required for this systematic review.
Purpose and Structure of SBHCs
In order to increase access to health care, SBHCs were started in the 1960s in Massachusetts, Dallas, and Minneapolis as a part of the American Academy of Pediatrics Community Access to Child Health (CATCH) program. In 1978, funding through the Robert Wood Johnson Foundation spurred an increase in the numbers SBHCs throughout the United States. Despite initial controversy focusing on issues of reproductive health care and parental rights, the efforts to establish SBHCs grew rapidly in the 1990s. Over time, SBHCs’ fiscal sustainability have improved through a diverse portfolio of funding sources including state and federal governments, private foundations, partner organizations, and school or school districts.5
Today, the mission of SBHCs is to contribute to the health of children by providing access to primary health care and preventive health care services.7 Often SBHCs provide services to an underserved population of children and adolescents. SBHCs are staffed by a multidisciplinary team of nurse practitioners or physician’s assistants, physicians, mental health providers, and other support staff. This support staff may include nurses, health educators, outreach workers, medical assistants, substance abuse counselors, dental hygienists, nutritionists, and school staff, among others.
SBHCs are steadily expanding across the United States as they demonstrate increased access to health care and prevent downstream health care–associated costs to society. There are currently 2315 SBHCs in the United States, distributed among urban, suburban, and rural locations.8 This represents a roughly 20% increase in SBHCs since 2011.9 Expansion of SBHCs are in part driven by the broad support garnered from major legislative and policymaking bodies. The American Academy of Pediatrics recommends SBHCs as a safety-net health care delivery model for pediatric populations that are uninsured, underinsured, or represent special populations who do not have regular access health care.2 In 2010, the Patient Protection and Affordable Care Act initially provided funding of $200 million toward expanding SBHCs in medically underserved communities or those experiencing a shortage of health professionals.10 Most recently, the Centers for Disease Control and Prevention’s (CDC) Community Preventive Services Task Force strongly recommended the “implementation and maintenance of SBHCs in low-income communities, based on sufficient evidence of effectiveness in improving educational and health outcomes.”11
The services SBHCs provide are far-reaching and often reflect the unique needs of the communities in which they are embedded. Prevention and early intervention are key initiatives. SBHCs are established in Kindergarten through 12th grade settings. They provide the basics of primary health care, including but not limited to, health assessments, anticipatory guidance, screenings for vision and hearing, immunizations, acute illness care, and treatment and laboratory services. They also provide mental health care, social services, dentistry, and health education. SBHCs are often established in schools that serve low-income youth and other populations that experience disparities in health care access and outcomes.5,9 In elementary school, SBHCs provide opportunities for preventive care, health maintenance, and the treatment of acute illnesses and injuries.5,12
The SBHC may provide a medical home for students who would not otherwise have access to care.13,14 For those students that already have a regular source of care, SBHCs do not appear to fragment a child’s health care. Instead, SBHCs link with other sources of care through health information technology and refer to community care providers for after-hours care.3 Generally, student participation requires parental consent. Services provided for individual students are sometimes restricted either due to lack of resources or, in the case of reproductive health, prohibitive policies. The latter, most commonly at the school-district level, limited half of SBHCs from dispensing contraception as of 2014.8 However, the percentage of SBHCs that dispense contraceptives has been increasing for the last decade. Services can be expanded to other people in the community including school staff, student family members, or even the community at large. Services are often provided by a medical center or provider independent of the school system, such as a federally qualified health center or academic institution.11
SBHCs address several challenges faced by more traditional models of care.15,16 SBHCs improve access to health care for children in rural areas, increase time spent learning in school by reducing travel to regular health appointments, improve follow-up compliance, and better serve adolescents.2,5 They also prevent major causes of youth mortality (eg, suicide, homicide, and accidental injury) through increased access to health and mental health services as well as enhanced behavioral surveillance and clinical management.15 For these reasons, in particular, SBHCs might be particularly well-suited to serve hard-to-reach populations such as the AI/AN in the United States, where there is an urgent need for better mental health care quality and access to care for young people. Although research in this population is limited, one study has found American-Indian youth rely on SBHCs for behavioral health and checkups more than their peers.17 This indicates that AI/AN communities might be open to utilizing SBHCs.
SBHCs have the potential to address sequelae of health disparities and poverty. Poverty and mental health outcomes for children are clearly linked.1,18 Impoverished children are more likely to have parents with substance abuse or mental health disorders, more likely to be abused or neglected, be placed in foster care, have a parent who is absent or incarcerated, or to be exposed to violence, trauma, and/or the death of a parent.19-23 They are also at higher risk for teenage pregnancy, depression, obesity, unintentional injuries, homicide, suicide, or diabetes, and are more likely to be hungry, have problems with vision, oral health, or hearing.1,5,23-29 These medical and mental health problems are associated with decreased scholastic performance and educational achievement,3,5,30 which is in turn strongly associated with future risk-taking behavior and higher rates of morbidity and mortality.3 Children growing up in poverty and those experiencing health disparities require models of care that better serve their health care needs. SBHCs integrate with the education system to improve access, quality, and cost for these disadvantaged pediatric populations.
Financial Benefits
Public sector grants (ie, local, state, and federal) offset losses to SBHCs associated with non-reimbursable services and uninsured patients. For example, 7 in 10 SBHCs report receiving state dollars for operations. Eighteen states report dedicating nearly $85 million to SBHCs. And as of 2014, sixty-five local health departments from across the country administer approximately 135 SBHCs as part of their public health mission. In addition to government contributions, SBHC partners (eg, hospitals and schools) often provide both cash and in-kind support to underwrite operations. For example, as of 2014 in the United States, more than 100 hospital systems sponsored 330 SBHCs. Private sector support (eg, foundations, private insurers, and corporations) is less common than public grants and partnerships. Nevertheless, more than 40% of SBHCs receive funds from private foundations.
SBHCs provide financial savings to children and their families. Health care provided by SBHCs prevents secondary losses of time and productivity for parents who would otherwise have to leave work to bring their children to appointments. SBHCs prevent unnecessary ED visits and unintended pregnancies.6 For example, Guo et al found that when they demonstrated financial savings to stakeholders after children with access to a SBHC showed decreased emergency room utilization in comparison with those from non-SBHC schools.31,32 SBHCs also provide services to patients and their families at reduced costs or for free by leveraging favorable state and federal policies, a diverse array of sponsorships (grants and in-kind donations), as well as employing traditional funding mechanisms such as third-party insurance payments.6,8 For example, for students enrolled in Medicaid, total health care costs and costs for mental health services were lower for students in schools with SBHCs compared with students in schools without SBHCs.33
SBHCs have also demonstrated a cost-benefit to society.6,7,33-35 According to a review by Ran et al,6 after adjusting to the 2013 consumer price index, each SBHC provided a total social benefit ranging from US$15 028 to US$912 878, with cost-benefit ratios from 1.38:1 to 3.05:1.6,35-37 Estimates vary based on geography, school characteristics, and categories of health benefits considered as social benefits, with avoided emergency department visits and delayed or avoided teen pregnancies providing the most benefit.6 Medicaid especially benefits from the cost savings associated with SBHCs, with estimated savings ranging from $30 to $969 per visit and between $46 to $1166 per Medicaid enrolled student in schools with SBHCs.6,31,35,38
SBHCs have continued to invest in sustainability.8 Nine in 10 SBHCs seek reimbursement for services from public and private health insurers. On average, SBHCs bill 4 different patient revenue sources, which cover one third (33.6%) of program costs. While fee-for-service remains the standard payment method for SBHCs (78.3%), some sites receive monthly or annual capitated payments for primary care (34.8%), “pay for performance” supplements (26.7%), or monthly or annual capitated payments for care coordination (18.8%). As a result of these diverse sponsorships and sustainability efforts, SBHCs provide financial benefits to both children and families that lack access to affordable health care. Children and adolescents who lack health insurance, are underinsured, come from low-income backgrounds, or those with special health care needs are at particular high risk for substandard access to health maintenance, well-child care, mental health services, and dental disease. The majority of SBHCs in the United States currently provide these necessary services.9
Physical Health Outcomes
Physical health includes medical, vision, and dental health. SBHCs are defined first by their ability to provide medical care.5,9 SBHC services that improve physical health include preventive care (eg, administering immunizations), managing and coordinating care of chronic illnesses (eg, asthma and obesity), and decrease health-risk behaviors (eg, tobacco, drug, and alcohol use). More than 83% of SBHCs provide treatment and management of chronic health conditions. Students with chronic health conditions may suffer academic setbacks, increased disability, fewer job opportunities, and limited community interactions as they enter adulthood.39 SBHCs have had success treating many pediatric chronic conditions including asthma, obesity, children with special health care needs, and substance abuse (eg, alcohol, tobacco, and other drugs).5
SBHCs have also improved prenatal care.3,5 For example, Barnet et al showed that teens who received prenatal care at an SBHC comprehensive adolescent pregnancy prevention program (CAPP) had lower odds of delivering a low-birth weight baby than those who received CAPP at a hospital-based setting.40 They also provide reproductive health services that address issues such as teen pregnancy and sexually transmitted infections. For example, SBHCs have been credited for a major decline in black teen pregnancy rates in adolescents in Denver, CO.41 The biggest strength of on-site reproductive health is being able to provide care when students decide they want or need a service.
Vision screening is provided by 84% of SBHCs.8 Some offer full vision services, including provision of eyeglasses. In addition, nearly 18% of SBHCs have oral health providers as a member of staff, and 20% provide oral health exams by a dentist or dental hygienist on-site. Poor access to oral health care remains one of the most persistent health disparities in the United States and is one of the largest causes of chronic disease and absenteeism.42 SBHCs solve this problem by bringing dental services to children in school.43
Mental Health Outcomes
Confronted with the large and persistent unmet mental health needs of children and youth, schools in the United States have become the most common provider of children’s mental health care.44 However, they have neither the resources nor the expertise to do so. Nearly 1 in 5 US children have a mental, emotional, or behavioral disorder, such as anxiety, depression, or attention-deficit/hyperactivity disorder.45 Early diagnosis and treatment are critical, but access to mental health care can be a challenge due to shortages in the availability and affordability of child psychiatrists, psychologists, or behavior therapists. Minority racial/ethnic pediatric populations, as well as those living in poverty, are more likely to lack access to mental health resources.46
SBHCs are in a unique position not only to identify mental health problems among children and adolescents but also to provide treatment or links to appropriate services. Evidence shows students with either public or no health insurance are more likely to access SBHC mental health services.47 Nearly 70% of SBHCs offer mental health care services through licensed clinical social workers, psychologists, and/or substance abuse counselors.9,30,48 Services most often provided include substance use counseling, violence prevention, suicide prevention, dating violence, mental health diagnoses, grief and loss therapy, crisis intervention, and medication management or administration.9 In addition, they often treat depression, anxiety, social conflict, sequelae of toxic stress, and attention disorders.8 Females seek mental health services more often; however, evidence shows that SBHCs are successful in reaching males as well.
Increasing availability of SBHC mental health services has been shown to reduce depressive episodes and suicide risk among adolescents. For example, in one study of 168 Oregon public schools, students with increased access to mental health through SBHCs at 14 different schools were less likely to report depressive episodes (odds ratio [OR] = 0.88, P < .01), suicidal ideation (OR = 0.84, P < .01), and suicide attempts (OR = 0.82, P < .01) from 2013 to 2015 compared with all other schools in the study. Students who exhibit high-risk behaviors or had more complex mental health difficulties such as suicide, depression, and difficultly with sleep are more likely to seek services at an SBHC.49
Limited research on mental health delivery models in SBHCs exist. One qualitative study of 43 key stakeholders in a network of 14 SBHCs describes various types and levels of integration between health and mental health services.50 Specifically, the authors identified 3 mental health delivery models: (1) coordinated care, where medical and mental health is provided in separate locations and coordinate care from a distance; (2) co-located care, where medical and mental health services are provided in the same location but have separate operational systems; and (3) integrated care, where medical and mental health providers share treatment plans. The latter “integrated care” model within an SBHC appears related to greater screening and detection of mental health problems. Nevertheless, the various types of mental health care delivery models reflect the heterogeneity of the communities that SBHCs serve. In caring for highly underserved populations, key determinants of the depth of mental health integration into SBHCs include staffing and operations, partnerships, and community engagement. As SBHCs expand and move toward interconnected systems of care, further research is needed to study these systems’ effects on children’s health, mental health, and academic achievement.50
Ultimately there remains a large need for school-based mental health that effectively partners with families, schools, and other community systems.51 For example, mental health has been implicated as a top risk factor for mass school shootings (ie, “rampage shootings”).52 The American Public Health Association (APHA) has endorsed SBHCs as a key mechanism through which gun violence prevention, intervention, and emergency preparedness can occur.53 Early identification of suicidal youth in schools and other settings could be a target of intervention for school shooters. In addition, preventing the more common urban “street” (ie, non-rampage) youth gun violence involves making mental health resources available in schools at all times.52
In addition, children exposed to ACEs have a greater risk for mental health disorders and school failure. ACEs are gaining increasing research priority across the country and are defined as childhood abuse, neglect, or dysfunction in the household (eg, domestic violence, parental mental illness, or parental substance abuse). Intervening early in a child experiencing chronic trauma is critical but mental health services are often inaccessible, especially for children and adolescents of minority racial/ethnic groups and those living in poverty. SBHCs may have a unique role to play in improving screening, treatment, and prevention.30,54
Education Outcomes
The CDC considers academic success both a strong indicator and outcome of the overall health and well-being of a child. Children must learn how to be healthy and must be healthy to learn. Academic success is a social determinant of pediatric and adult health. For example, it has been shown that chronic health conditions decrease academic achievement, and safe school environments improve health behaviors and academic performance.55 As emphasis on school accountability grows, increasingly fewer resources at the federal, state, and local levels create a need to understand whether SBHCs have an impact on academic achievement.
The evidence linking SBHC presence to educational outcomes, however, is limited and mixed. The link between SBHC services and academic performance is indirect and intangible. As such, it is methodologically more challenging to study (challenges discussed below in Future Directions). For example, in a 2011 study, the authors reported that SBHC use decreased dropout rates. However, after the methodological concern of time-dependent bias was brought to their attention, the authors reanalyzed their data and retracted their results, finding no statistical relationship between SBHC use and dropout rates.56 It was unclear whether SBHC use affected graduation or simply attending school through graduation had an effect on measured SBHC use.
Nevertheless, SBHC utilization has been associated with improved academic outcomes, such as improved GPAs, attendance, grade promotion, college preparation, and reduced rates of suspensions.3,57 The APHA53 supports SBHCs because they “[create] school-wide programs that address bullying, violence, anger, depression and other social and emotional issues that impede academic achievement.” Additionally, a growing body of evidence suggests that SBHCs improve academic performance indirectly by increasing school connectedness, particularly in lower income youth populations.58,59 The CDC defines school connectedness as “the belief held by students that adults and peers in the school care about their learning as well as about them as individuals.”60 In one study, SBHC usage was significantly associated with school connection (bonding, attachment, and commitment), which was positively related to GPA and promotion to the next grade level.58
The close relationship between schooling and health have become the focus of significant philanthropy efforts.34 Organizations such as The Primary School (established by Priscilla Chan, a pediatrician, and her husband Mark Zuckerberg, founder of Facebook), Communities in Schools, and the Children’s Aid Society believe that at-risk children’s health and learning can improve when students, teachers, and families have access to health experts and services in schools.
Future Directions
Many questions remain regarding the effects of SBHCs on their student populations. Gaps in the evidence base of SBHCs’ impact may reflect methodologic challenges in evaluating SBHCs. These challenges include selection bias, sample size and statistical power, heterogeneity in services delivered or received, displacement effects (ie, when students replace SBHC with other sources of health care such as ED visits), historical effects (eg, child maturation), and clustering effects (eg, students at the same schools are usually more similar to each other than students at a different school).57 Bersamin and colleagues discuss 5 promising approaches that can improve the rigor of SBHC evaluation that address these challenges.57
Many opportunities remain where further research is needed. Most important issues are related to mental health integration and educational impact of SBHCs. Regarding the latter, the link between SBHCs and educational outcomes remains tenuous. More methodologically robust design and analysis is required by, for example, linking educational data to health records. However, there remain large legal barriers to negotiating exchange of information about students. Finally, most studies on the benefits of SBHCs have focused on on-site SBHCS in minority populations, low-income schools, urban settings, and older groups of students. Further research must also focus on the sustainability of SBHCs in different environments including off-site clinics, rural settings, schools in mid- to high-income communities, and with younger children. Experimenting with telemedicine, as well, could provide SBHCs additional utility and save costs to the health care system, as it has been shown to do with asthma in young people.61
Targets for research that have not yet been discussed much in the literature pertain to harmful societal issues such as youth gun violence, ACEs, and the rising premature death rates of young people in the AI/AN community. Regarding the first, US youth perpetrate and experience very high rates of violence compared with youth from many other developed nations. Over 17 000 American children and teens are injured or killed each year due to gun violence. This translates to nearly 46 youth shot each day leading to 7 fatalities.62 Gun violence cost the US$229 billion in 2015, or an average of $700 per gun in America.53 The societal costs of firearm assault injury include work loss, medical/mental health care, emergency transportation, police/criminal justice activities, insurance claims processing, costs to employers, and decreased quality of life. Gun violence is a prime example of an issue situated at the intersection of clinical medicine and population health, as well as a driver of children and teen’s maladaptive social ecosystems. In a scoping review of youth violence, Bushman et al call for research that establishes how mental health services can be effectively harnessed to support youth experiencing serious social and emotional difficulties.52 Future research should investigate whether SBHCs prevent youth gun violence, possibly by way of providing mental health care to those youth most at risk.
Another potential area of research is ACE. The effects of ACEs exposure extend well beyond the immediate act of harm and include severe mental, physical, and behavioral health disorders across the life course.63,64 These include increased risk for sexually transmitted diseases, self-inflicted injury, substance abuse, and violence. Ultimately, the annual US economic burden for childhood maltreatment (ie, ACEs) is $124 billion.64 Associated downstream costs to society include health care costs, productivity losses, child welfare costs, violence/crime costs, special education costs, and suicide death costs. Recently, a 4-year national effort culminated during which stakeholders engaged in creating a comprehensive national research and action agenda on ACEs. Research now prioritizes relationship-centered health care as well as family and community engagement in order to mitigate the effect of ACEs-related stress and trauma, establish resilience, promote positive health skills, and improve child health and well-being.65 While SBHCs have engaged in trauma-informed care, research that has measured or evaluated their effectiveness is lacking. Future research ought to focus on whether young people with high ACE scores receiving trauma-informed care experience better outcomes in schools with SBHCS compared with those without.
Finally, despite being particularly well-suited to serve the AI/AN population in the United States, evidence on the use of SBHC in this community is lacking. Between 2011 and 2014, AI/ANs had the highest premature mortality rates in the United States, driven mainly by suicide, accidental deaths (primarily drug overdoses), and chronic liver disease and cirrhosis.66 The largest reported mortality increases were in young people. From 1999 to 2014, mortality in 25-year-old AI/ANs increased 2.7% for men and 5% for women each year. This likely underestimates the mortality burden, however, since nearly 40% of AI/ANs are recorded as the wrong race (usually white) on their death certificates according to a 2016 CDC report.66 Given this epidemic among young people and the quality and access barriers they face, SBHC services align well with necessary efforts to address health equity issues among the AI/AN community.
Conclusions
SBHCs may promote social mobility and improve health equity by meeting the needs of disadvantaged populations and removing barriers to health care services.3 Their financial and physical benefits are well documented but more research is needed on their impact on mental health and educational outcomes. Further research opportunities exist related to the impact of SBHCs on pressing health-related societal concerns in vulnerable populations.
Footnotes
Author Contributions: All authors contributed equally to the first draft. The first author took on the responsibility of editing and submitting all subsequent manuscripts drafts. The last author provided mentorship throughout the writing process.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Research time for this article was partially supported by National Science Foundation grant #1634234 and the National Institute of Mental Health (1R03MH113849-01).
ORCID iD: Michael Arenson  https://orcid.org/0000-0002-2007-7799
https://orcid.org/0000-0002-2007-7799
References
- 1. Komro KA, Tobler AL, Delisle AL, O’Mara RJ, Wagenaar AC. Beyond the clinic: improving child health through evidence-based community development. BMC Pediatr. 2013;13:172. doi: 10.1186/1471-2431-13-172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Council on School Health. School-based health centers and pediatric practice. Pediatrics. 2012;129:387-393. doi: 10.1542/peds.2011-3443 [DOI] [PubMed] [Google Scholar]
- 3. Knopf JA, Finnie RKC, Peng Y, et al. School-based health centers to advance health equity: a community guide systematic review. Am J Prev Med. 2016;51:114-126. doi: 10.1016/j.amepre.2016.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Brindis CD. The “State of the State” of school-based health centers: achieving health and educational outcomes. Am J Prev Med. 2016;51:139-140. doi: 10.1016/j.amepre.2016.03.004 [DOI] [PubMed] [Google Scholar]
- 5. Keeton V, Soleimanpour S, Brindis CD. School-based health centers in an era of health care reform: building on history. Curr Probl Pediatr Adolesc Health Care. 2012;42:132-156. doi: 10.1016/j.cppeds.2012.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ran T, Chattopadhyay SK, Hahn RA; Community Preventive Services Task Force. Economic evaluation of school-based health centers: a community guide systematic review. Am J Prev Med. 2016;51:129-138. doi: 10.1016/J.AMEPRE.2016.01.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gustafson EM. History and overview of school-based health centers in the US. Nurs Clin North Am. 2005;40:595-606. doi: 10.1016/j.cnur.2005.08.001 [DOI] [PubMed] [Google Scholar]
- 8. School Based Health Alliance. 2013-14 Census of school-based health centers: methodology, key report data details, and acknowledgements. http://www.sbh4all.org/wp-content/uploads/2015/02/2013-14-Census-Data-and-Methods.pdf. Accessed October 31, 2017.
- 9. School-Based Health Alliance. National School-Based Health Care Census. http://www.sbh4all.org/school-health-care/national-census-of-school-based-health-centers/. Published 2015. Accessed December 4, 2017.
- 10. The Patient Protection and Affordable Care Act. One Hundred Eleventh Congress of the United States of America; 2010:Sbu-Section 4101. http://www.ncsl.org/documents/health/ppaca-consolidated.pdf. Accessed December 4, 2017.
- 11. Community Preventive Services Task Force. School-based health centers to promote health equity: recommendation of the Community Preventive Services Task Force. Am J Prev Med. 2016;51:127-128. doi: 10.1016/j.amepre.2016.01.008 [DOI] [PubMed] [Google Scholar]
- 12. Johnson V, Hutcherson V. A study of the utilization patterns of an elementary school-based health clinic over a 5-year period. J Sch Health. 2006;76:373-378. doi: 10.1111/j.1746-1561.2006.00128.x [DOI] [PubMed] [Google Scholar]
- 13. Albright K, Barnard J, O’Leary S, et al. School-based health centers as medical homes: parents’ and adolescents’ perspectives. Acad Pediatr. 2016;16:381-386. doi: 10.1016/j.acap.2015.06.004 [DOI] [PubMed] [Google Scholar]
- 14. O’Leary ST, Lee M, Federico S, et al. School-based health centers as patient-centered medical homes. Pediatrics. 2014;134:957-964. doi: 10.1542/peds.2014-0296 [DOI] [PubMed] [Google Scholar]
- 15. American Academy of Pediatrics. Committee on School Health. School health centers and other integrated school health services. Pediatrics. 2001;107:198-201. [DOI] [PubMed] [Google Scholar]
- 16. Bloom B, Jones LI, Freeman G. Summary health statistics for US children: National Health Interview Survey, 2012. Vital Health Stat 10. 2013;(258):1-81. [PubMed] [Google Scholar]
- 17. Koenig KT, Ramos MM, Fowler TT, Oreskovich K, McGrath J, Fairbrother G. A statewide profile of frequent users of school-based health centers: implications for adolescent health care. J Sch Health. 2016;86:250-257. doi: 10.1111/josh.12374 [DOI] [PubMed] [Google Scholar]
- 18. Schor EL, Billingsley MM, Golden AL, et al. Report of the task force on the family. Pediatrics. 2003;111(6 pt 2):1541-1571. [PubMed] [Google Scholar]
- 19. Berger LM. Income, family characteristics, and physical violence toward children. Child Abuse Negl. 2005;29:107-133. doi: 10.1016/j.chiabu.2004.02.006 [DOI] [PubMed] [Google Scholar]
- 20. Smith VC, Wilson CR; Committee on Substance Use and Prevention Cosua. Families affected by parental substance use. Pediatrics. 2016;138:e20161575. doi: 10.1542/peds.2016-1575 [DOI] [PubMed] [Google Scholar]
- 21. Berdahl T, Owens PL, Dougherty D, McCormick MC, Pylypchuk Y, Simpson LA. Annual report on health care for children and youth in the United States: racial/ethnic and socioeconomic disparities in children’s health care quality. Acad Pediatr. 2010;10:95-118. doi: 10.1016/j.acap.2009.12.005 [DOI] [PubMed] [Google Scholar]
- 22. Oral R, Ramirez M, Coohey C, et al. Adverse childhood experiences and trauma informed care: the future of health care. Pediatr Res. 2016;79:227-233. doi: 10.1038/pr.2015.197 [DOI] [PubMed] [Google Scholar]
- 23. Federal Interagency Forum on Child and Family Statistics. America’s children: key national indicators of well-being, 2017. https://www.childstats.gov/pdf/ac2017/ac_17.pdf. Accessed January 22, 2019.
- 24. Health Resources | Services Administration Maternal | Child Health Bureau. The Health and Well-Being of Children: A Portrait of States and the Nation. Rockville, MD: Health Resources and Services Administration Maternal and Child Health Bureau; 2014. https://mchb.hrsa.gov/nsch/2011-12/health/index.html. Accessed January 22, 2019. [Google Scholar]
- 25. Thomas JF, Temple JR, Perez N, Rupp R. Ethnic and gender disparities in needed adolescent mental health care. J Health Care Poor Underserved. 2011;22:101-110. doi: 10.1353/hpu.2011.0029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lyon AR, Ludwig KA, Stoep AV, Gudmundsen G, Mccauley E. Patterns and predictors of mental healthcare utilization in schools and other service sectors among adolescents at risk for depression. School Ment Health. 2013;5:77-97. doi: 10.1007/s12310-012-9097-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Flaherty EG, Thompson R, Dubowitz H, et al. Adverse childhood experiences and child health in early adolescence. JAMA Pediatr. 2013;167:622-629. doi: 10.1001/jamapediatrics.2013.22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Mason-Jones AJ, Crisp C, Momberg M, Koech J, De Koker P, Mathews C. A systematic review of the role of school-based healthcare in adolescent sexual, reproductive, and mental health. Syst Rev. 2012;1:49. doi: 10.1186/2046-4053-1-49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Paschall MJ, Bersamin M. School-based health centers, depression, and suicide risk among adolescents. Am J Prev Med. 2018;54:44-50. doi: 10.1016/j.amepre.2017.08.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Larson S, Chapman S, Spetz J, Brindis CD. Chronic childhood trauma, mental health, academic achievement, and school-based health center mental health services. J Sch Health. 2017;87:675-686. doi: 10.1111/josh.12541 [DOI] [PubMed] [Google Scholar]
- 31. Guo JJ, Jang R, Keller KN, McCracken AL, Pan W, Cluxton RJ. Impact of school-based health centers on children with asthma. J Adolesc Health. 2005;37:266-274. doi: 10.1016/j.jadohealth.2004.09.006 [DOI] [PubMed] [Google Scholar]
- 32. Webber MP, Carpiniello KE, Oruwariye T, Lo Y, Burton WB, Appel DK. Burden of asthma in inner-city elementary schoolchildren: do school-based health centers make a difference? Arch Pediatr Adolesc Med. 2003;157:125-129. doi: 10.1001/archpedi.157.2.125 [DOI] [PubMed] [Google Scholar]
- 33. Guo JJ, Wade TJ, Keller KN. Impact of school-based health centers on students with mental health problems. Public Health Rep. 2008;123:768-780. doi: 10.1177/003335490812300613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kottke TE, Pronk N, Zinkel AR, Isham GJ. Philanthropy and beyond: creating shared value to promote well-being for individuals in their communities. Perm J. 2017;21. doi: 10.7812/TPP/16-188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Guo JJ, Wade TJ, Pan W, Keller KN. School-based health centers: cost-benefit analysis and impact on health care disparities. Am J Public Health. 2010;100:1617-1623. doi: 10.2105/AJPH.2009.185181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Horton JM, Lima-Negron J. School-based health centers: expanding the knowledge and vision. https://hfwcny.org/hfwcny-content/uploads/School_Based_Health_Centers_July_2009.pdf. Published July 2009. Accessed January 22, 2019.
- 37. Brindis CD. An Evaluation Study of School-Based Clinics in California : Major Findings, 1986-1991. San Francisco, CA: University of California, San Francisco, Center for Reproductive Health Policy Research; 1993. [Google Scholar]
- 38. Adams EK, Johnson V. An elementary school-based health clinic: can it reduce Medicaid costs? Pediatrics. 2000;105(4 pt 1):780-788. doi: 10.1542/PEDS.105.4.780 [DOI] [PubMed] [Google Scholar]
- 39. Leroy ZC, Wallin R, Lee S. The role of school health services in addressing the needs of students with chronic health conditions. J Sch Nurs. 2017;33:64-72. doi: 10.1177/1059840516678909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Barnet B, Duggan AK, Devoe M. Reduced low birth weight for teenagers receiving prenatal care at a school-based health center: effect of access and comprehensive care. J Adolesc Health. 2003;33:349-358. [DOI] [PubMed] [Google Scholar]
- 41. Ricketts SA, Guernsey BP. School-based health centers and the decline in black teen fertility during the 1990s in Denver, Colorado. Am J Public Health. 2006;96:1588-1592. doi: 10.2105/AJPH.2004.059816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. da Fonseca MA, Avenetti D. Social determinants of pediatric oral health. Dent Clin North Am. 2017;61:519-532. doi: 10.1016/j.cden.2017.02.002 [DOI] [PubMed] [Google Scholar]
- 43. Larsen CD, Larsen MD, Handwerker LB, Kim MS, Rosenthal M. A comparison of urban school- and community-based dental clinics. J Sch Health. 2009;79:116-122. doi: 10.1111/j.1746-1561.2008.00395.x [DOI] [PubMed] [Google Scholar]
- 44. Atkins MS, Cappella E, Shernoff ES, Mehta TG, Gustafson EL. Schooling and children’s mental health: realigning resources to reduce disparities and advance public health. Annu Rev Clin Psychol. 2017;13:123-147. doi: 10.1146/annurev-clinpsy-032816-045234 [DOI] [PubMed] [Google Scholar]
- 45. Perou R, Bitsko RH, Blumberg SJ, et al. Mental health surveillance among children—United States, 2005-2011. MMWR Suppl. 2013;62:1-35. https://www.cdc.gov/mmwr/preview/mmwrhtml/su6202a1.htm?s_cid=su6202a1_w. Accessed January 9, 2018. [PubMed] [Google Scholar]
- 46. Centers for Disease Control and Prevention. Children’s mental health. https://www.cdc.gov/childrensmentalhealth/index.html. Published 2017. Accessed January 22, 2019.
- 47. Bains RM, Diallo AF. Mental health services in school-based health centers: systematic review. J Sch Nurs. 2016;32:8-19. doi: 10.1177/1059840515590607 [DOI] [PubMed] [Google Scholar]
- 48. Larson S, Spetz J, Brindis CD, Chapman S. Characteristic differences between school-based health centers with and without mental health providers: a review of national trends. J Pediatr Health Care. 2017;31:484-492. doi: 10.1016/j.pedhc.2016.12.007 [DOI] [PubMed] [Google Scholar]
- 49. Bains RM, Cusson R, White-Frese J, Walsh S. Utilization of mental health services in school-based health centers. J Sch Health. 2017;87:584-592. doi: 10.1111/josh.12528 [DOI] [PubMed] [Google Scholar]
- 50. Lai K, Guo S, Ijadi-Maghsoodi R, Puffer M, Kataoka SH. Bringing wellness to schools: opportunities for and challenges to mental health integration in school-based health centers. Psychiatr Serv. 2016;67:1328-1333. doi: 10.1176/appi.ps.201500401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Brener ND, Wheeler L, Wolfe LC, Vernon-Smiley M, Caldart-Olson L. Health services: results from the School Health Policies and Programs Study 2006. J Sch Health. 2007;77:464-485. doi: 10.1111/j.1746-1561.2007.00230.x [DOI] [PubMed] [Google Scholar]
- 52. Bushman BJ, Newman K, Calvert SL, et al. Youth violence: what we know and what we need to know. Am Psychol. 2016;71:17-39. doi: 10.1037/a0039687 [DOI] [PubMed] [Google Scholar]
- 53. American Public Health Association. Preventing gun violence. https://www.apha.org/~/media/files/pdf/factsheets/160317_gunviolencefs.ashx. Accessed February 11, 2018. [DOI] [PubMed]
- 54. Soleimanpour S, Geierstanger SP, Kaller S, McCarter V, Brindis CD. The role of school health centers in health care access and client outcomes. Am J Public Health. 2010;100:1597-1603. doi: 10.2105/AJPH.2009.186833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Michael SL, Merlo CL, Basch CE, Wentzel KR, Wechsler H. Critical connections: health and academics. J Sch Health. 2015;85:740-758. doi: 10.1111/josh.12309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Kerns SE, Pullmann MD, Walker SC, Lyon AR, Cosgrove TJ, Bruns EJ. School-based health center use and high school dropout rates—reply. Arch Pediatr Adolesc Med. 2012;166:675-677. doi: 10.1001/archpediatrics.2012.553 [DOI] [PubMed] [Google Scholar]
- 57. Bersamin M, Garbers S, Gold MA, et al. Measuring success: evaluation designs and approaches to assessing the impact of school-based health centers. J Adolesc Health. 2016;58:3-10. doi: 10.1016/j.jadohealth.2015.09.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Strolin-Goltzman J, Sisselman A, Melekis K, Auerbach C. Understanding the relationship between school-based health center use, school connection, and academic performance. Health Soc Work. 2014;39:83-91. doi: 10.1093/hsw/hlu018 [DOI] [PubMed] [Google Scholar]
- 59. Bersamin M, Coulter RWS, Gaarde J, Garbers S, Mair C, Santelli J. School-based health centers and school connectedness. J Sch Health. 2019;89:11-19. doi: 10.1111/josh.12707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Centers for Disease Control and Prevention. School Connectedness: Strategies for Increasing Protective Factors Among Youth. Atlanta, GA: US Department of Health and Human Services; 2009. https://www.cdc.gov/healthyyouth/protective/pdf/connectedness.pdf. Accessed January 18, 2018. [Google Scholar]
- 61. Halterman JS, Fagnano M, Tajon RS, et al. Effect of the School-Based Telemedicine Enhanced Asthma Management (SB-TEAM) Program on Asthma Morbidity: a randomized clinical trial. JAMA Pediatr. 2018;172:e174938. doi: 10.1001/jamapediatrics.2017.4938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Brady Campaign. Children and gun violence. https://www.bradycampaign.org/gun-violence/topics/children-and-gun-violence. Published 2017. Accessed February 11, 2018.
- 63. Letourneau EJ, Brown DS, Fang X, Hassan A, Mercy JA. The economic burden of child sexual abuse in the United States. Child Abuse Negl. 2018;79:413-422. doi: 10.1016/j.chiabu.2018.02.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Peterson C, Florence C, Klevens J. The economic burden of child maltreatment in the United States, 2015. Child Abuse Negl. 2018;86:178-183. doi: 10.1016/j.chiabu.2018.09.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Bethell CD, Simpson LA, Solloway MR. Child well-being and adverse childhood experiences in the United States. Acad Pediatr. 2017;17(7 supple):S1-S3. doi: 10.1016/j.acap.2017.06.011 [DOI] [PubMed] [Google Scholar]
- 66. Abbasi J. Why are American Indians dying young? JAMA. 2018;319:109-111. doi: 10.1001/jama.2017.10122 [DOI] [PubMed] [Google Scholar]