Short abstract
Objectives
This study aimed to evaluate the effects of periodontal therapy on the efficacy of Helicobacter pylori eradication and on the recurrence of infection after eradication.
Methods
We conducted a prospective randomized trial on 698 gastric H. pylori-infected patients, of whom 347 received gastric H. pylori treatment alone and 342 received gastric H. pylori treatment plus periodontal therapy. The presence of H. pylori and associated virulence genes were detected by real-time polymerase chain reaction.
Results
After eradication of gastric H. pylori infection, the recurrence of gastric H. pylori was significantly lower in the gastric H. pylori treatment plus periodontal therapy group than in the group receiving gastric H. pylori treatment alone (OR 0.67; 95% CI 0.45 to 0.99), whereas the eradication rate was not significantly different (OR 0.87; 95% CI 0.68 to 0.98). There was a close relationship between the presence of H. pylori in saliva and its presence in the stomach.
Conclusions
The oral cavity is an important reservoir for gastric H. pylori infection. Adjunctive periodontal therapy could enhance the efficiency of H. pylori treatment and reduce the recurrence of gastric H. pylori infection.
Keywords: Periodontal therapy, gastric eradication, Helicobacter pylori, oral cavity, recurrent infection, virulence, adjunctive therapy, gastrointestinal disease
Introduction
Helicobacter pylori infection is an important gastrointestinal disease associated with the onset of gastritis, as well as gastric or duodenal ulcer disease and gastric cancer. Chronic gastritis-associated H. pylori infection has been found in approximately 50% of the global population and is etiologically linked to gastric cancers, comprising 25% of cancers related to this etiology of infection; therefore, it constitutes a primary public health problem.1–4 In Thailand, the infection rate ranges from 54.1% to 76.1%;5 however, the age-standardized incidence rate of gastric cancer is relatively low in Asian countries.6 The progression of disease depends on multiple factors, which contribute to the onset of associated gastric diseases.7
Cytotoxin-associated antigen (cagA) and vacuolating cytotoxin (vacA) are the major virulence factors of H. pylori,8 and are most closely associated with clinical outcomes of H. pylori infection.9 The cag pathogenicity island (cag PAI) is a cluster of genes found in strains exhibiting enhanced interactions with gastric tissue.9 This cluster encodes a bacterial type IV secretion system that translocates cagA into host gastric epithelial cells, and has been associated with the production of vacA, which causes cytoplasmic vacuolization in gastric epithelial cells;9,10 moreover, it has been associated with delayed healing of gastric ulcers, inhibition of re-epithelialization, and worsening of the quality of mucosal scarring.11 H. pylori strains harboring cagA and vacA are more frequent among patients with peptic ulcers, gastric mucosa-associated lymphoid tissue (MALT) lymphoma, and gastric cancers.12–14
Although standard triple therapy regimens achieve successful eradication in H. pylori-positive gastritis patients, the recurrence rate is relatively high (13%).16–18 Causes of gastric H. pylori recurrence-associated gastrointestinal diseases are not clear. There is a high prevalence of H. pylori DNA in dental plaque and saliva; notably, the oral cavity may constitute a reservoir for gastric infection and transmission.18–22 Therefore, failed H. pylori eradication may be linked to the presence of oral H. pylori.
To determine whether eradication therapy alone or eradication therapy plus periodontal therapy contribute to reduced recurrence, it is necessary to identify factors involved in the recurrence of H. pylori in gastric mucosa. This study evaluated the association between the presence of H. pylori in saliva and its presence in the stomach, and investigated possible H. pylori treatment in Thailand. The findings of this study may improve treatment efficacy and reduce the risk of H. pylori recurrence in this region.
Patients and methods
Patients and sampling
Samples were obtained from patients diagnosed with H. pylori-associated gastric diseases who underwent esophagogastroduodenoscopy (EGD) at Suranaree University of Technology Hospital in the northeast region of Thailand from March 2017 to December 2017. Full-mouth periodontal examination was performed in all cases. The plaque index (PI) score was classified as follows: 0 = no plaque; 1 = a film of plaque adheres to the gingival margin, assessed by passing a probe across the tooth surface; 2 = moderate accumulation of plaque visible to the naked eye within the gingival pocket, and/or at the gingival margin and tooth surface; and 3 = abundant accumulation (1- to 2-mm thick) of plaque visible to the naked eye within the gingival pocket, and/or at the gingival margin and tooth surface. The gingival index (GI) score was recorded as follows: 0 = normal gingiva; 1 = mild inflammation, slight change in color, slight edema, and no bleeding on probing (BOP); 2 = moderate inflammation, edema, redness and glazing, and BOP present; and 3 = severe inflammation, marked redness and ulceration, spontaneous bleeding, and edema. Probing depth (PD) and relative attachment level (RAL) were measured at six locations per tooth (mesial, distal, lingual/palatal, and buccal/labial) using a periodontal probe.23–25 After baseline recording of clinical parameters, saliva was collected into a polypropylene tube, via the passive drool technique, until 2 mL of saliva was collected per patient; this saliva (2 mL) was mixed with DNAgard saliva stabilizer (1.5 mL; Biomatrica, San Diego, CA, USA), in accordance with the manufacturers’ instructions. After oral clinical examination in accordance with the World Health Organization criteria, the patients were subjected to esophagogastroduodenoscopy (EGD), which was performed using an upper GI video endoscope (Olympus EVIS EXERA III, CV-190). First, the whole stomach was examined by conventional endoscopy; then, biopsies were conducted using the site-specific biopsy technique.26 Gastric biopsy specimens for histological determinations were subsequently examined by the pathologist. Hematoxylin and eosin (H&E) and giemsa stains were used for H. pylori identification. All samples were stored at −20°C until further processing by molecular methods.
H. pylori-associated gastritis patients, as determined by stool antigen, rapid urease test, or histological examination, were included in the study. The exclusion criteria were as follows: treatment for H. pylori infection during the previous 2 months; presence of metabolic disorders; immunosuppression; use of antibiotics or gastrointestinal medications, such as proton pomp inhibitors, within the previous 2 months; previous gastric surgery; and a history of professional tooth cleaning or any other periodontal treatment within the past 6 months. We recruited a total of 689 H. pylori-associated gastritis patients who underwent EGD at Suranaree University of Technology Hospital (Figure 1). Demographic and clinical data, including sex, age, oral health status (dental caries, dental plaque, aphthous stomatitis, periodontitis, and dental caries + periodontitis) were collected for the enrolled patients. Written informed consent was obtained from all patients, and the study protocol was approved by the Ethics Committee for Research Involving Human Subjects, Suranaree University of Technology (EC 13-2560) and Thai Clinical Trials Registry (Study ID: TCTR20170324001). The methods were performed in accordance with the principles of good clinical practice and the Declaration of Helsinki guidelines.
Figure 1.
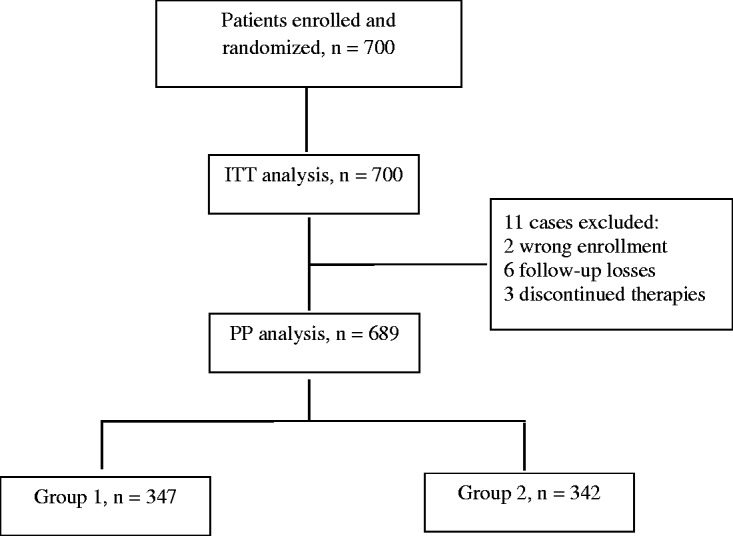
Flow diagram showing numbers of patients enrolled and missed for per-protocol and intention-to-treat analyses. ITT: intention-to-treat; PP: per-protocol; ATB: antibiotic. Group 1: ATB alone, group 2: ATB plus periodontal therapy.
Study groups
Six hundred eighty-nine H. pylori-associated gastritis patients were randomly divided into two groups using a random number generator from SPSS for Windows (version 16.0; SPSS Inc., Chicago, IL, USA) (Figure 1). Among these patients, 347 (168 female and 179 male; mean age of 46 ± 2 years; range, 17–80 years) were randomized to 1-week triple therapy (esomeprazole 20 mg twice per day, clarithromycin 500 mg twice per day, or metronidazole 400 mg three times per day (if clarithromycin-resistant), and amoxicillin 1000 mg twice per day (group 1)), and 342 patients (173 female and 169 male; mean age of 49 ± 3 years; range, 17–80 years) were randomized to triple therapy plus periodontal therapy (group 2). There were no significant differences between group 1 and group 2 in terms of numbers of patients, age, sex, or periodontal diseases.
Follow-up statement
Patient follow-up was scheduled 4 weeks after the completion of therapy. Stool antigen tests, rapid urease tests, and histopathological examinations were performed as per routine practice, with polymerase chain reaction (PCR) for validation. Those who were negative for H. pylori underwent further examination after 1 year to establish the recurrence rate. Both invasive tests (gastric biopsy and PCR) and non-invasive tests (rapid urease test and histopathological examination) were used for diagnosis of reinfection with H. pylori.
Periodontal therapy
Scaling and root planning (SRP) is the gold standard in periodontal therapy. Treatment included hand instrumentation of the teeth to remove dental plaque and calculus from affected enamel and cementum, ultrasonic scaling therapy, flossing, irrigation with 0.12% chlorhexidine mouth rinse for 45 seconds, and oral hygiene instruction.27 All patients were examined at 3 months following SRP to confirm the therapeutic results.
DNA extraction
Genomic DNA was extracted from saliva and fresh frozen gastric biopsies using the QIAamp® DNA Microme Kit (Qiagen, Duesseldorf, Germany) and QIamp DNA mini kit (Qiagen), respectively, in accordance with the manufacturer's protocol. The extracted DNA concentration and purity were evaluated using a DS-11+ spectrophotometer (Denovix, Wilmington, DE, USA) and stored at −20°C.
Real-time polymerase chain reaction (PCR)
To determine the presence of H. pylori and its virulence genes, real-time PCR was performed. DNA extracted from saliva and gastric biopsies samples was used as template in the amplification reactions. Real-time PCR was performed in accordance with the manufacturer's protocol in a final volume of 20 µl, containing cDNA template, 2X SYBR Green PCR Master Mix (Roche Applied Science, Mannheim, Germany), and 5 pmol of each primer using a LightCycler® 480 Instrument (Roche Diagnostics, Neuilly sur Seine, France). The PCR primers for 16s RNA, cagA, vacA, and ureA (Integrated DNA Technologies, Coralville, IA, USA) are shown in Table 1. The PCR conditions were as follows: 95°C for 10 minutes, then 40 cycles of 95°C for 15 s and 60°C for 1 minute. All data were analyzed using LightCycler 480 software, version 1.5 (Roche Diagnostics).
Table 1.
Primer sequences used for real-time polymerase chain reaction.
| Gene | Forward | Reverse |
|---|---|---|
| CagA | 5′-GAGTCATAATGGCATAGAACCTGAA-3′ | 5′-TTGTGCAAGAAATTCCATGAAA-3′ |
| VacA | 5′-CTCCAGAAGGCACACCAATAA-3′ | 5′-TGGCTTCCACTTCCCCATTAA-3′ |
| UreA | 5′-CGTGGCAAGCATGATCCAT-3′ | 5′-GGGTATGCACGGTTACGAGTTT-3′ |
| 16s | 5′-GGAGTACGGTCGCAAGATTAAA-3′ | 5′-CTAGCGGATTCTCTCAATGTCAA-3′ |
Statistical analysis
All statistical analyses were performed using SPSS for Windows, version 16.0 (SPSS Inc., Chicago, IL, USA). Comparisons between groups were performed using ANOVA for patient demographic data. Statistical significance of the correlations of the presence of H. pylori between saliva and gastric biopsies was evaluated using the χ2 and Pearson’s correlation tests. The eradication rates of H. pylori were evaluated by intention-to-treat (ITT) and per-protocol (PP) analysis. All patients were subjected to the ITT analysis; however, patients with incorrect enrollment, or who were lost to follow-up, were subjected to PP analysis. The association between treatment with H. pylori eradication therapy alone and H. pylori eradication therapy plus periodontal therapy was analyzed using a logistic regression model, with significance set at p < 0.05.
Results
Presence of H. pylori and virulence genes in saliva and stomach and their associations
Two H. pylori-specific genes, the 16S rRNA and ureA genes, were included for H. pylori detection; these genes were detected in all 689 (100%) gastric biopsy samples, and were detected in 549/689 (79.7%) saliva samples. An association was observed between saliva H. pylori and gastric biopsy H. pylori (p = 0.007). Among the 549 H. pylori-positive cases, 231 were positive for the cagA gene (42%) and 223 were positive for the vacA gene (41%) in saliva. On gastric biopsy, 605 H. pylori-positive cases were positive for the cagA gene (87.8%) and 532 cases were positive for the vacA gene (77.2%). There were no significant associations between the virulence genes of H. pylori in saliva and gastric biopsy samples.
H. pylori eradication
We subsequently examined the potential therapy for gastric H. pylori eradication and its recurrence in patients with gastric H. pylori treatment alone and in those with gastric H. pylori treatment plus periodontal therapy. We found that gastric H. pylori treatment plus periodontal therapy produced a significantly lower recurrence rate of H. pylori infection than did gastric H. pylori treatment alone (OR 0.69; 95% CI 0.52 to 0.99; p = 0.001) by PP analysis; however, the eradication rates were not significantly different (OR 0.77; 95% CI 0.58 to 0.97) (Table 2). ITT analysis showed that the recurrence rates were significantly different between the groups (OR 0.67; 95% CI 0.45 to 0.99; p = 0.001), while the eradication rates were not significantly different (OR 0.87; 95% CI 0.68 to 0.98) (Table 2).
Table 2.
Outcomes of treatment with triple therapy alone and treatment with triple therapy plus periodontal therapy.
| Variable | Treatment |
OR (95% CI) | p-value | |
|---|---|---|---|---|
| ATB alone | ATB + periodontal therapy | |||
| ITT | ||||
| Cure rate | 304/350 (86.85) | 331/350 (94.57) | 0.87 (0.68–0.98) | 0.076 |
| Recurrence | 53/350 (15.14) | 7/350 (2) | 0.67 (0.45–0.99) | 0.001* |
| PP | ||||
| Cure rate | 304/347 (87.60) | 331/342 (96.78) | 0.77 (0.58–0.97) | 0.078 |
| Recurrence | 53/347 (15.27) | 7/342 (2.04) | 0.69 (0.52–0.99) | 0.001* |
ATB: antibiotic OR: odds ratio; CI: confidence interval; ITT: intention-to-treat; PP: per-protocol.
Discussion
H. pylori infection has been associated with chronic gastritis, peptic ulcers, gastric MALT lymphomas, and gastric adenocarcinomas.28 Reported annual H. pylori recurrence rates after eradication therapy in developed and developing countries were 2.67% and 13.00%, respectively;18 notably, the organism has been observed in various niches in the oral cavity, including the tongue, saliva, and dental plaque.9,29 In Thailand, the reported annual recurrence rate of H. pylori infection after successful eradication was 2.9%.30 To the best of our knowledge, this study is the first to determine the effect of periodontal therapy on gastric H. pylori eradication, as well as to evaluate the association between the presence of H. pylori in saliva and in the stomach in Thailand. We found that periodontal therapy plus gastric H. pylori treatment reduced the recurrence of gastric H. pylori infections. This result suggests a promising approach for reducing the risk of recurrent H. pylori infection. Moreover, we observed a significant association between H. pylori in saliva and gastric biopsy.
Avcu et al.31 found that the recurrence of gastric H. pylori infection after triple therapy was more frequent among patients with poor oral hygiene than among patients with good oral hygiene. Furthermore, Adler et al.32 demonstrated that the oral cavity was an initial extra-gastric reservoir for H. pylori; they found a strong relationship between H. pylori infections in the mouth and stomach. This observation may explain the consistently high recurrence rates of H. pylori infection in the stomach. Several studies have demonstrated that bacterial eradication in the oral cavity should be considered as an important aspect in the elimination of H. pylori-associated diseases, because the oral cavity may serve as a potential reservoir.3,28,33–37 Our results agree with these observations, in that, after treatment for H pylori infection, patients treated with periodontal therapy plus triple therapy had a significantly lower recurrence rate of H. pylori infection, relative to the rate observed in patients who received only triple therapy. There was no significant difference in the eradication rates between the groups. Nevertheless, periodontal therapy plus triple therapy appears to have a better effect on H. pylori eradication. We suspect that periodontal treatments may be useful adjuncts to triple therapy for H. pylori eradication.
Some authors have proposed that no living H. pylori can be found in the oral cavity and that the positive response on PCR may therefore result from regurgitation, vomiting, or reflux from the stomach; however, in the present study, we found H. pylori in the saliva and stomach of 79.7% and 100% of enrolled patients, respectively (p = 0.007). We speculate that the oral cavity is a potential reservoir for H. pylori and may be the source of gastric infection (and re-infection) and bacterial transmission. Currently, it remains unclear whether H. pylori strains in the oral cavity are the same strains that cause gastritis. Nevertheless, genotyping of H. pylori strains isolated from the stomach and the oral cavity have demonstrated that strains from these two sites appear to be identical, although different strains are harbored by different individuals.9,38 Additionally, some studies have shown 98% agreement between DNA sequences of H. pylori in the stomach and corresponding strains in dental plaque or saliva,9 suggesting that at least some individuals harbor the same strain in both the stomach and the mouth.9,28 There have been many reports that H. pylori strains carrying cagA and vacA are closely associated with the incidence of severe gastroduodenal diseases.12–14 Therefore, H. pylori strains in the oral cavity that produce cagA and vacA may be considered highly virulent. We observed a high rate of detection of H. pylori cagA-producing virulent strains in saliva (42% positive), while 41% of strains produced vacA in saliva. This finding suggests that salivary H. pylori might be a risk factor for gastrointestinal reinfection. Interestingly, we observed no significant association between the virulence genes of H. pylori in saliva and those in gastric biopsy. It is possible that H. pylori from two different places may comprise the same strains. Therefore, genotyping of H. pylori strains isolated from stomach and saliva should be prioritized in future research.
Although our findings revealed an association between the presence of H. pylori in saliva and that in the stomach, the complete genomes of H. pylori strains in both sites should be sequenced, because this is the only method to assess genetic identity. Furthermore, additional multicenter studies and large-scale randomized controlled trials are required to provide a better representation of the actual data and evaluate the hypothesis.
Conclusions
To the best of our knowledge, this is the first study to assess the prevalence of saliva H. pylori strains in the northeast region of Thailand, where there is a high prevalence of H. pylori infection. An association was observed between H. pylori in saliva and in gastric biopsies, suggesting that the oral cavity might constitute a reservoir for gastric H. pylori infection and re-infection. We further observed that H. pylori eradication plus periodontal therapy reduced the recurrence of gastric H. pylori infection in both PP and ITT analyses. Therefore, periodontal therapy should be applied to reduce the risk of recurrence of H. pylori re-infection-associated gastritis.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This research was supported by a grant from Suranaree University of Technology and by the Office of the Higher Education Commission under the NRU project of Thailand.
References
- 1.Mbulaiteye SM, Hisada M, El-Omar EM. Helicobacter pylori associated global gastric cancer burden. Front Biosci (Landmark Ed) 2009; 14: 1490–1504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Plummer M, Franceschi S, Vignat J, et al. Global burden of gastric cancer attributable to Helicobacterpylori. Int. J. Cancer 2015; 136: 487–490. [DOI] [PubMed] [Google Scholar]
- 3.Burucoa C, Axon A. Epidemiology of Helicobacter pylori infection. Helicobacter 2017; 22: e12403. [DOI] [PubMed] [Google Scholar]
- 4.Peleteiro B, Bastos A, Ferro A, et al. Prevalence of Helicobacter pylori infection worldwide: a systematic review of studies with national coverage. Dig Dis Sci 2014; 59: 1698–1709. [DOI] [PubMed] [Google Scholar]
- 5.Sahara S, Sugimoto M, Vilaichone RK, et al. Role of Helicobacter pylori cagA EPIYA motif and vacA genotypes for the development of gastrointestinal diseases in Southeast Asian countries: a meta-analysis. BMC Infect Dis 2012; 12: 223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mitacek EJ, Brunnemann KD, Suttajit M, et al. Geographic distribution of liver and stomach cancers in Thailand in relation to estimated dietary intake of nitrate, nitrite, and nitrosodimethylamine. Nutr Cancer 2008; 60: 196–203. [DOI] [PubMed] [Google Scholar]
- 7.Trang TT, Shiota S, Matsuda M, et al. The prevalence of Helicobacter pylori virulence factors in Bhutan, Vietnam, and Myanmar is related to gastric cancer incidence. Biomed Res Int 2015; 2015: 830813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McClain MS, Beckett AC, Cover TL. Helicobacter pylori vacuolating toxin and gastric cancer. Toxins 2017; 9: 316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Silva DG, Stevens RH, Macedo JM, et al. Detection of cytotoxin genotypes of Helicobacter pylori in stomach, saliva and dental plaque. Arch Oral Biol 2009; 54: 684–688. [DOI] [PubMed] [Google Scholar]
- 10.Ali A, Naz A, Soares SC, et al. Pan-genome analysis of human gastric pathogen H. pylori: comparative genomics and pathogenomics approaches to identify regions associated with pathogenicity and prediction of potential core therapeutic targets. Biomed Res Int 2015; 2015: 139580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chang K, Fujiwara Y, Wyle F, et al. Helicobacter pylori toxin inhibits growth and proliferation of cultured gastric cells-Kato III. J Physiol Pharmacol 1993; 44: 17–22. [PubMed] [Google Scholar]
- 12.Oliveira AG, Santos A, Guerra JB, et al. babA2- and cagA-positive Helicobacter pylori strains are associated with duodenal ulcer and gastric carcinoma in Brazil. J Clin Microbiol 2003; 4: 3964–3966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dabiri H, Jafari F, Baghaei, et al. Prevalence of Helicobacter pylori vacA, cagA, cagE, oipA, iceA, babA2 and babB genotypes in Iranian dyspeptic patients. Microb Pathog 2017; 105: 226–230. [DOI] [PubMed] [Google Scholar]
- 14.Amieva M, Richard M, Peek RM., Jr. Pathobiology of Helicobacter pylori–induced gastric cancer. Gastroenterology 2016; 150: 64–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rimbara E, Fischbach LA, Graham DY. Optimal therapy for Helicobacter pylori infections. Nat Rev Gastroenterol Hepatol 2011; 8: 79–88. [DOI] [PubMed] [Google Scholar]
- 16.Hu Y, Wan JH, Zhu Y, et al. Systematic review with meta‐analysis: the global recurrence rate of Helicobacter pylori. Aliment Pharmacol Ther 2017; 48: 773–779. [DOI] [PubMed] [Google Scholar]
- 17.Hooshmand B, Monsef A, Amirmadglesi M, et al. Oral fluid antibody detection in the diagnosis of gastric Helicobacter pylori infection. Iran J Allergy Asthma Immunol 2004; 3: 127–131. [PubMed] [Google Scholar]
- 18.Niv Y. H. pylori recurrence after successful eradication. World J Gastroenterol 2008; 14: 1477–1478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Adler I, Denninghoff VC, Alvarez MI, et al. Helicobacter pylori associated with glossitis and halitosis. Helicobacter 2005; 10: 312–317. [DOI] [PubMed] [Google Scholar]
- 20.Rasmussen LT, Labio RW, Gatti LL, et al. Helicobacter pylori detection in gastric biopsies, saliva and dental plaque of Brazilian dyspeptic patients. Mem Inst Oswaldo Cruz 2010; 105: 326–330. [DOI] [PubMed] [Google Scholar]
- 21.Umeda M, Kobayashi H, Takeuchi Y, et al. High prevalence of Helicobacter pylori detected by PCR in the oral cavities of periodontitis patients. J Periodontol 2003; 74: 129–134. [DOI] [PubMed] [Google Scholar]
- 22.Burgers R, Schneider-Brachert W, Reischl U, et al. Helicobacter pylori in human oral cavity and stomach. Eur J Oral Sci 2008; 116: 297–304. [DOI] [PubMed] [Google Scholar]
- 23.Eickholz P. Clinical periodontal diagnosis: probing pocket depth, vertical attachment level and bleeding on probing. Perio Quintessenz 2004; 1: 75–80. [Google Scholar]
- 24.Vandana KL, Gupta I. The location of cemento enamel junction for CAL measurement: a clinical crisis. J Indian Soc Periodontol 2009; 13: 12–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Löe H. The gingival index, the plaque index and the retention index systems. J Periodontol 1967; 38: 610–616. [DOI] [PubMed] [Google Scholar]
- 26.Tongtawee T, Dechsukhum C, Leeanansaksiri W, et al. Improved detection of Helicobacter pylori infection and premalignant gastric mucosa using “site specific biopsy”: a randomized control clinical tria. Asian Pac J Cancer Prev 2015; 16: 8487–8490. [DOI] [PubMed] [Google Scholar]
- 27.Quirynen M, Mongardini C, de Soete M, et al. The role of chlorhexidine in the one-stage full-mouth disinfection treatment of patients with advanced adult periodontitis. Long-term clinical and microbiological observations. J Clin Periodontol 2000, 27:578–589. [DOI] [PubMed] [Google Scholar]
- 28.Silva DG, Stevens RH, Macedo JM, et al. Presence of Helicobacter pylori in supragingival dental plaque of individuals with periodontal disease and upper gastric diseases. Arch Oral Biol 2010; 55: 896–901. [DOI] [PubMed] [Google Scholar]
- 29.Jia CL, Jiang GS, Li CH, et al. Effect of dental plaque control on infection of Helicobacter pylori in gastric mucosa. J Periodontol 2009; 80: 1606–1609. [DOI] [PubMed] [Google Scholar]
- 30.Vilaichone RK, Wongcha UA, Chotivitayatarakorn P. Low re-infection rate of Helicobacter pylori after successful eradication in Thailand: a 2 years study. Asian Pac J Cancer Prev 2017; 18: 695–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Avcu N, Avcu F, Beyan C, et al. The relationship between gastric–oral Helicobacter pylori and oral hygiene in patients with vitamin B-12 deficiency anemia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001; 92: 166–169. [DOI] [PubMed] [Google Scholar]
- 32.Adler I, Muino A, Aguas S, et al. Helicobacter pylori and oral pathology: relationship with the gastric infection. World J Gastroenterol 2014; 20: 9922–9935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Anand PS, Nandakumar K, Shenoy KT. Are dental plaque, poor oral hygiene, and periodontal disease associated with Helicobacter pylori infection? J Periodontol 2006; 77: 692–698. [DOI] [PubMed] [Google Scholar]
- 34.Anand PS, Kamath KP, Anil S. Role of dental plaque, saliva and periodontal disease in Helicobacter pylori infection. World J Gastroenterol 2014; 20: 5639–5653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Colombo AP, Gonçalves C, Maria R, et al. Microbiological evaluation of adjunctive systemic and local tetracycline administration combined with scaling and root planing in the treatment of chronic periodontitis. Braz J Oral Sci 2003; 2: 370–377. [Google Scholar]
- 36.Bouziane A, Ahid S, Abouqal R, et al. Effect of periodontal therapy on prevention of gastric Helicobacter pylori recurrence: a systematic review and meta-analysis. J Clin Periodontol 2012; 39: 1166–1173. [DOI] [PubMed] [Google Scholar]
- 37.Zaric S, Bojic B, Jankovic LJ, et al. Periodontal therapy improves gastric Helicobacter pylori eradication. J Dent Res 2009; 88: 946–950. [DOI] [PubMed] [Google Scholar]
- 38.Shames B, Krajden S, Fuksa M, et al. Evidence for the occurrence of the same strain of Campylobacter pylori in the stomach and dental plaque. J Clin Microbiol 1989; 27: 2849–2850. [DOI] [PMC free article] [PubMed] [Google Scholar]


