Abstract
Pigmented villonodular synovitis is a rare, disabling disease that usually presents in young adults. Here, the authors present a unique case of pigmented villonodular synovitis in a 60-year-old female diagnosed 20 years after the initial presentation. The patient presented with a complaint of knee pain consistent with osteoarthritis. Radiological investigations, including magnetic resonance imaging, only showed degenerative changes and were inconclusive to diagnose pigmented villonodular synovitis. Intraoperative macroscopic features of the synovium suggested pigmented villonodular synovitis, which was confirmed by histopathological examination. Histopathological examination, despite being the gold standard, was performed late in this case. The authors recommend histopathological confirmation of pigmented villonodular synovitis in all suspected cases, even with inconclusive radiological manifestations.
Keywords: Histopathology, knee pain, osteoarthritis, pigmented villonodular synovitis
INTRODUCTION
Pigmented villonodular synovitis (PVNS) is a rare yet debilitating disease that usually presents in young adults and mainly affects the knee (in ~70% of cases) and hip joints (in ~20% of cases).[1,2,3] According to a 17-year study, in the United States, the annual incidence of PVNS is estimated as 1.8 per million, with a male preponderance.[4] In contrast, in China, a retrospective study of 237 cases found a female preponderance.[3] There are no large-scale studies from the Middle East to indicate the preponderance in the region.
PVNS is characterized by synovial proliferation and hemosiderin deposition inside the joints, tendon sheaths and bursae.[1] Although the exact etiology remains unclear, trauma, intra-articular hemorrhage and inflammation have been reported to be associated with the disease.[5] Some authors consider chronic inflammation to be its cause, while others consider it to be a neoplastic disorder.[2] Magnetic resonance imaging (MRI) is the imaging of choice for clinically suspected patients; however, histopathology remains the gold standard tool for the diagnosis.[2] Here, the authors present the case of an atypical presentation confirmed by late histopathological examination.
CASE REPORT
A 60-year-old female with a history of diabetes mellitus and hypertension presented to the Orthopedic Clinic at King Khalid National Guard Hospital, Jeddah, Saudi Arabia, complaining of bilateral knee pain, primarily affecting the right knee, for the past 20 years. She had only been on pain medication and there was no surgical intervention. She described the pain as constant and nonradiating that got aggravated by activities and relieved by rest. The patient had a history of knee trauma, while her systemic review was unremarkable, except for a positive first-degree family history of breast cancer.
On examination, she walked without assistance and showed a full range of motion without the signs of effusion. She had previously been diagnosed with osteoarthritis, and weight-bearing X-ray showed severe bilateral osteoarthritic changes, positive bilateral findings of osteopenia, small effusion and genu varus deformity. Later, an MRI of the right knee showed high-signal intensity in the anteromedial fibers of the anterior cruciate ligaments. Moreover, the posterior horn of the medial meniscus had a complex tear and displacement consistent with a bucket handle tear. The lateral meniscus showed a mild increase in signal intensity, representing intrameniscal degeneration. The MRI also showed old injuries and trauma-related findings in collateral ligaments and medial retinaculum, respectively. Furthermore, a small Baker's cyst was noted [Figure 1]. Accordingly, the right knee arthroscopy was done, and partial synovectomy was performed. After arthroscopy, and because of advanced osteoarthritic changes, the patient underwent total knee replacement.
Figure 1.
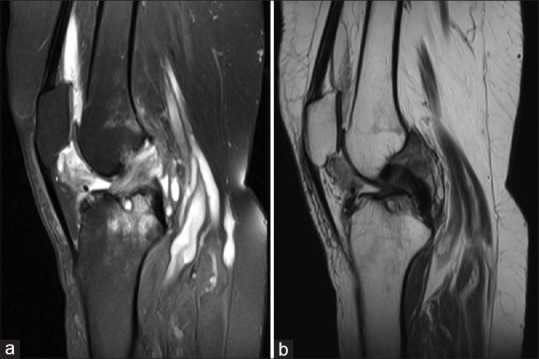
Sagittal view of the right knee magnetic resonance imaging; T2 view showing high-signal intensity in the anterior cruciate ligaments, Baker's cyst and absence of pigmented villonodular synovitis features (a and b)
Intraoperatively, a bright brown inflamed synovium was seen. A decision was made to obtain synovial biopsy from the right femoral notch, which confirmed the diagnosis of PVNS. Macroscopically, a single piece of irregular, gray-tan, rubbery tissue with a lobulated outer surface was observed. Microscopically, a circumscribed lesion consisting of sheets of mononuclear synoviocytes mixed with multinucleated giant cells and foamy histiocytes along with focal hemosiderin pigmentation was noted [Figure 2]. The patient tolerated the operation well, without any postoperative complications. She was discharged and seen at the clinic after 2 weeks for suture removal. At her 2-month follow-up, clinical and radiological examinations were unremarkable.
Figure 2.
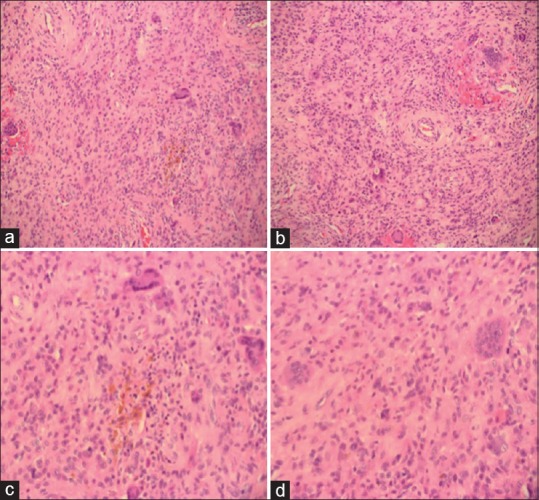
(a and b) Cellular proliferation of mononucleated synoviocyte, macrophages and multinucleated giant cells (H and E); (c and d) Multinucleated giant cells and brown hemosiderin pigments (H and E)
DISCUSSION
This is only the second reported case of PVNS in Saudi Arabia; the first reported case was of a 12-month-old girl with PVNS affecting the knee.[6] In the current case report, the patient had a relatively late-onset PVNS that affected the knee. The mean age of PVNS presentation is 33 (±13.1) years;[2] the patient in this report was likely in her forties when PVNS occurred.
The mean delay from the first appearance of PVNS symptoms until diagnosis is 2.9 years.[2] However, in this report, PVNS was only diagnosed in her early sixties, about 20 years after the first symptom. Although higher than in general, this delay in diagnosis is much lower than one patient who reported a delay of 600 months from symptom onset to diagnosis.[3] It has been noted that the older the patient, the more the delay in diagnosis, thereby indicating that clinical presentations at older ages could cause difficulties in differential diagnosis.[5] Further, gender could also play a role in delay in diagnosis, especially when the knee is affected in females, as they are more susceptible to knee osteoarthritis.[2,3,5]
MRI is the most commonly used tool for diagnosing PVNS, with the most common findings being changes due to gadolinium deposition, synovial hypertrophy, nodules and bone lesions.[2] However, in the current report, MRI did not show any signs of PVNS. Interestingly, we found the Baker's cyst on the MRI, which can easily lead to misdiagnosis. Similarly, Gokhale et al.[7] found the Baker's cyst on MRI that was later histopathologically confirmed as PVNS.[7] It is unclear if this presence of Baker's cyst in PVNS patients is an incidental association or if it could be a risk factor, and thus further research is required.
When confirmed, arthroscopic synovectomy is the most commonly performed procedure for treating PVNS. However, recurrence of PVNS with this procedure is relatively high (about 20%), differing depending on location and gender.[3] In our case, given the advanced osteoarthritic changes in the knee, total knee replacement was the preferred method. Xie et al.[3] reported that only about 17% of PVNS patients have trauma history; our patient had a history of trauma.
CONCLUSION
This unique case adds to the literature of PVNS by highlighting that MRI findings can be misleading and that synovial biopsy is the gold standard for diagnosis. The authors recommend that clinicians should have a high degree of suspicion for PVNS in patients with long-term knee pain as well as include atypical PVNS presentation into considerations.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the Journal. The patient understands that her name and initials will not be published and due efforts will be made to conceal her identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Shah SH, Porrino JA, Green JR, 3rd, Chew FS. Bilateral pigmented villonodular synovitis of the knee. Radiol Case Rep. 2015;10:56–60. doi: 10.1016/j.radcr.2015.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ottaviani S, Ayral X, Dougados M, Gossec L. Pigmented villonodular synovitis: A retrospective single-center study of 122 cases and review of the literature. Semin Arthritis Rheum. 2011;40:539–46. doi: 10.1016/j.semarthrit.2010.07.005. [DOI] [PubMed] [Google Scholar]
- 3.Xie GP, Jiang N, Liang CX, Zeng JC, Chen ZY, Xu Q, et al. Pigmented villonodular synovitis: A retrospective multicenter study of 237 cases. PLoS One. 2015;10:e0121451. doi: 10.1371/journal.pone.0121451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Myers BW, Masi AT. Pigmented villonodular synovitis and tenosynovitis: A clinical epidemiologic study of 166 cases and literature review. Medicine (Baltimore) 1980;59:223–38. [PubMed] [Google Scholar]
- 5.Bassetti E, Candreva R, Santucci E. Pigmented villonodular synovitis of the knee: A case report. J Ultrasound. 2011;14:167–9. doi: 10.1016/j.jus.2011.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jawadi AH. Pigmented villonodular synovitis of the knee in a 12-month-old girl. J Taibah Univ Med Sci. 2014;9:335–7. [Google Scholar]
- 7.Gokhale N, Purohit S, Bhosale PB. Pigmented villonodular synovitis presenting as a popliteal cyst. J Orthop Case Rep. 2015;5:63–5. doi: 10.13107/jocr.2250-0685.311. [DOI] [PMC free article] [PubMed] [Google Scholar]


