Abstract
Purpose
27-hydroxycholesterol (27HC), an endogenous selective estrogen receptor modulator (SERM), drives the growth of estrogen receptor-positive (ER+) breast cancer. 1,25-dihydroxyvitamin D (1,25(OH)2D), the active metabolite of vitamin D, is known to inhibit expression of CYP27B1, which is very similar in structure and function to CYP27A1, the synthesizing enzyme of 27HC. Therefore, we hypothesized that 1,25(OH)2D may also inhibit expression of CYP27A1, thereby reducing 27HC concentrations in the blood and tissues that express CYP27A1, including breast cancer tissue.
Methods
27HC, 25-hydroxyvitamin D (25OHD), and 1,25(OH)2D were measured in sera from 29 breast cancer patients before and after supplementation with low-dose (400 IU/day) or high-dose (10,000 IU/day) vitamin D in the interval between biopsy and surgery.
Results
A significant increase (p = 4.3E−5) in 25OHD and a decrease (p = 1.7E−1) in 27HC was observed in high-dose versus low-dose vitamin D subjects. Excluding two statistical outliers, 25OHD and 27HC levels were inversely correlated (p = 7.0E−3).
Conclusions
Vitamin D supplementation can decrease circulating 27HC of breast cancer patients, likely by CYP27A1 inhibition. This suggests a new and additional modality by which vitamin D can inhibit ER+ breast cancer growth, though a larger study is needed for verification.
Keywords: Vitamin D, Calcitriol, 27-hydroxycholesterol, ER+ breast cancer, CYP27A1
Introduction
Recently, an endogenous selective estrogen receptor modulator (SERM), 27-hydroxycholesterol (27HC) [1, 2], was discovered to have agonist activity on estrogen receptor-positive (ER+) breast cancer [2–4] and to promote tumor growth and metastasis [4]. The concentration of 27HC is elevated in ER+ breast cancer tissue compared to normal breast tissue due to decreased expression of CYP7B1, the degrading enzyme of 27HC [3]. In animal models, knocking down the synthesizing enzyme of 27HC, CYP27A1, reduces cancer rates and ER+ breast cancer tumor sizes in mice [5]. Despite the accumulating evidence for the role of 27HC in ER+ breast cancer stimulation, no therapies have been developed to target specifically the 27HC metabolic pathway, although it has been hypothesized that the presumed benefit of statins on cancer risk may be due to an effect of lowering 27HC production by reducing cholesterol synthesis [5]. In one study, atorvastatin was shown to decrease serum 27HC and increase CYP27A1 protein expression in breast cancer tissue in a small cohort of 42 breast cancer patients, and higher expression of CYP27A1 in ER+ breast cancer tumors was shown to correlate with longer recurrence-free and overall survival [6]. These data demonstrate the importance of targeting the 27HC pathway in the treatment of ER+ breast cancer.
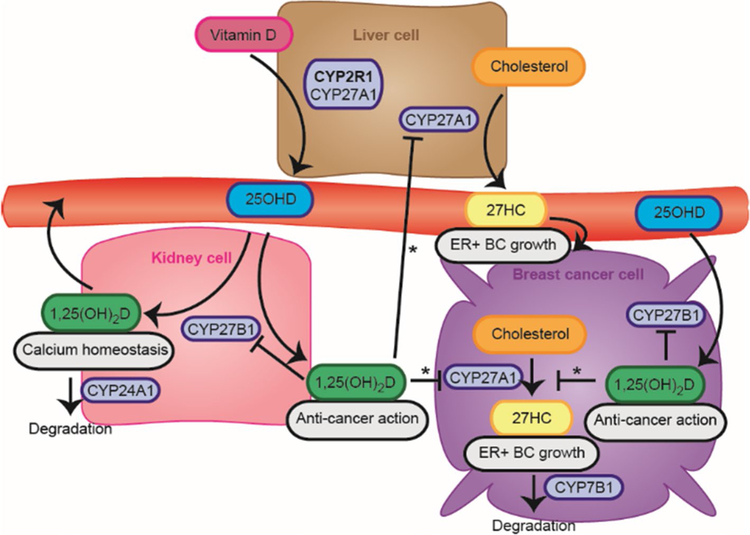
Vitamin D is a prohormone for the steroid hormone calcitriol (1,25-dihydroxyvitamin D3, 1,25(OH)2D3), which is estimated to be responsible for the transcriptional regulation of 0.5–5% of the total human genome [7], including those known to influence pathways associated with cancer growth and progression [8–10]. Calcitriol can reduce its own activation of target genes by inhibiting expression of CYP27B1 [11, 12], the enzyme responsible for 1-α-hydroxylation of 25-hydroxyvitamin D (25OHD) to form calcitriol (Fig. 1), as well as stimulating the calcitriol and 25OHD degrading enzyme CYP24A1 [8, 13]. CYP27A1 has 40% sequence homology with CYP27B1, and CYP27A1 also has 1-α-hydroxylase activity toward 25OHD [13–15]. Given the similarity between CYP27B1 and CYP27A1 [13], we hypothesized that vitamin D might inhibit 27HC production by calcitriol-mediated inhibition of CYP27A1 expression, providing an additional means by which vitamin D inhibits ER+ breast cancer and a novel way to target the 27HC pathway. Previous data on the relationship between vitamin D and 27HC have been ambiguous [16, 17]. Here we show in an interventional trial of 29 women with breast cancer, a sub-study of a larger trial, that raising serum 25OHD levels with vitamin D supplements can lower the concentration of circulating 27HC in most subjects. The findings of this pilot study will require verification in a larger study.
Fig. 1.
Metabolic pathways of 1,25(OH)2D and 27HC synthesis. Vitamin D is converted to 25-hydroxyvitamin D (25OHD) by the cytochrome P450s CYP2R1 and, to a lesser extent, CYP27A1 in the liver. 25OHD is the primary metabolite of vitamin D found in the circulation and is clinically used as the best indicator of vitamin D status. 25OHD can be 1-α-hydroxylated by CYP27B1 to form 1,25(OH)2D in the kidney as part of maintaining blood mineral homeostasis, or locally in many tissues, including breast cancer cells. 1,25(OH)2D acts as an anti-cancer agent via regulation of multiple pathways associated with cancer growth and progression. One such pathway may be that of cholesterol metabolism into 27-hydroxycholesterol (27HC), a selective estrogen receptor modulator that promotes ER+ breast cancer growth and metastasis. 1,25(OH)2 inhibits its synthesizing enzyme, CYP27B1, and we hypothesize that 1,25(OH)2D may also inhibit CYP27A1 (*), the synthesizing enzyme of 27HC, which is similar in structure and function to CYP27B1
Materials and methods
This paper describes an ancillary study of a breast cancer trial (NCT01472445), the full details of which are currently being prepared for publication. Briefly, this trial was a randomized, controlled, and blinded trial in women with core needle biopsies positive for breast cancer, but without the presence of metastatic lesions. Subjects with a history of parathyroid disease, hypercalcemia, kidney stones, SERM or aromatase inhibitor therapy, or renal failure, and patients taking metformin or more than 2000 IU of vitamin D per day were excluded from the trial. The protocol was approved by the Stanford Institutional Review Board for Protection of Human Subjects, and all women provided informed written consent. Serum was collected from 29 women with breast cancer at the time of biopsy and again before surgery prior to any subsequent therapy. This study comprised a subgroup of all subjects in the trial limited by available sera for the required assays. All patients discontinued the use of any vitamin D supplements taken before the start of the trial, and the women were treated with a daily supplement of high-dose (10,000 IU) or similar appearing capsules of low-dose (400 IU) vitamin D3 (Vital Nutrients, Middletown, CT) in a 2:1 ratio in the interval between biopsy and surgery. The low dose was shown to have a negligible effect on 25OHD levels in the short interval of supplementation and functioned as a placebo in our study as well as the full trial. Women who had surgery prior to 7 days were excluded so that capsules were taken for a minimum of 7 days, and the longest interval of supplementation for a subject was 41 days. Remaining capsules were counted to validate compliance. The concentration of total 25OHD (the sum of 25OHD2 and 25OHD3 abundances) was measured at the Stanford Clinical Lab, and the concentration of 1,25(OH)2D (the sum of 1,25(OH)2D2 and 1,25(OH)2D3 (calcitriol) abundances) was measured at Mayo Clinic Labs by liquid chromatography tandem mass spectrometry (LC–MS/MS), both in a blinded fashion.
The concentration of 27HC was measured by LC–MS/MS and selected reaction monitoring (SRM) using an adapted method [18]—please see Supplementary Information for further details. The change in 25OHD (Δ25OHD), 1,25(OH)2D (Δ1,25(OH)2D), and 27HC (Δ27HC) for each patient was calculated as the difference between pre- and post-treatment concentrations. A Wilcoxon unpaired, two-sample t test (Mann–Whitney) was performed to compare changes in metabolite concentrations for the low-dose and high-dose groups.
Results
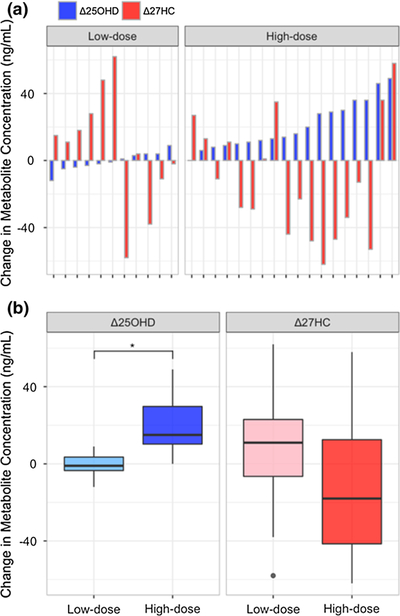
The concentrations of 25OHD, 1,25(OH)2D, and 27HC were measured in serum samples collected from the breast cancer subjects at the time of biopsy and at the time of surgery, corresponding to pre- and post-vitamin D treatment, respectively. Changes in pre- to post-treatment levels of these metabolites (Δ25OHD and Δ27HC) are plotted for each subject in Fig. 2a, and a summary of these data comparing the low-dose (400 IU/day) to the high-dose (10,000 IU/day) Vitamin D group is shown in Fig. 2b. As expected, minimal changes in 25OHD concentration were observed on average in the low-dose group (− 1 ± 6 ng/mL), and there was no correlation between Δ25OHD and the number of capsules taken, indicating that the low-dose, 400 IU/day vitamin D supplement effectively acted as a placebo in the trial. By contrast, serum 25OHD concentrations increased significantly by 21 ± 14 ng/mL on average in the high-dose group, and subjects treated over a longer period of time, who therefore ingested a greater number of high-dose capsules, showed a greater increase in 25OHD. Despite the significant difference between the low-dose and high-dose groups in the observed Δ25OHD (p = 4.3E−5), there was no significant difference in Δ1,25(OH)2D (p = 4.2E−1). This is expected since the rise in 25OHD inhibits a further rise in serum 1,25(OH)2D by stimulation of CYP24A1 and inhibition of CYP27B1, as depicted in Fig. 1.
Fig. 2.
Changes in the concentrations of 27HC and 25OHD for individual patients (a) and in the low-dose and high-dose groups as a whole (b). Significance (p < 0.05) is indicated by *
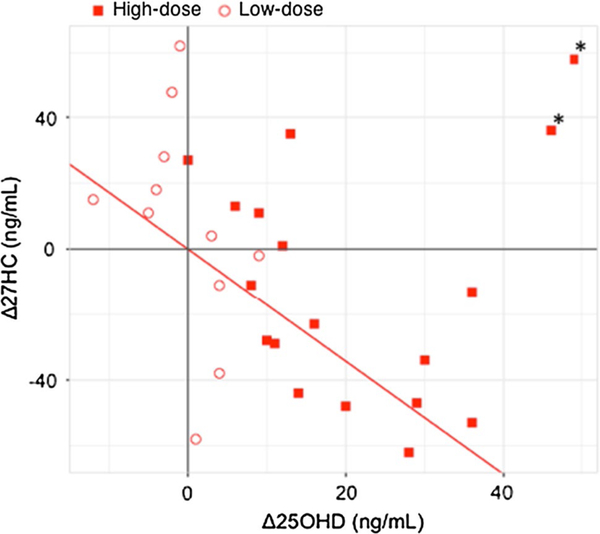
There is a decrease in median 27HC concentration (p = 1.7E−1) in the high-dose group compared to the low-dose group, with a change of 7 ± 35 ng/mL on average for the low-dose group and − 12 ± 35 ng/mL on average for the high-dose group. Although Δ27HC is not as statistically significant when comparing the low-dose to the high-dose group as Δ25OHD, a simple linear regression between Δ27HC and Δ25OHD in the high-dose group yields a coefficient of − 1.7 (p = 7.0E−3), indicating a significant decrease in 27HC with an increase in 25OHD (Fig. 3) when two high leverage outliers (Fig. 3, starred) are excluded. No significant correlation (p < 0.05) was observed between Δ27HC and Δ25OHD in the low-dose group. These data indicate that vitamin D supplements that raise the circulating 25OHD concentration can be used to decrease serum 27HC concentrations. The two high leverage outliers, who were exceptions to the inverse correlation between 27HC and 25OHD, were determined using Cook’s distance metric. For these subjects, a large increase in 27HC concentration was observed (+ 58 and + 36 ng/mL) despite large increases in serum 25OHD concentration (+ 49 and + 46 ng/mL, respectively) (Fig. 2a, far right). No other characteristics were extraordinary for these two patients compared to the rest of the cohort, including cancer phenotype, tumor grade or size, or BMI, a factor that has been associated with altered vitamin D metabolism [19, 20].
Fig. 3.
Change in the concentration of 27HC plotted against change in the concentration of 25OHD for individual patients. A linear regression of patients who received high-dose vitamin D supplements, excluding starred outliers, shows an inverse correlation between Δ25OHD and Δ27HC
Discussion
Whereas minimal changes were observed in 25OHD concentrations in the low-dose vitamin D group, significant increases in 25OHD levels were observed in most subjects in the high-dose group. The increases in 25OHD in the high-dose group correlated with decreases in 27HC, demonstrating that vitamin D supplements can decrease serum 27HC concentrations. The mechanism of this effect is likely inhibition of CYP27A1 by the active metabolite of vitamin D, calcitriol (1,25(OH)2D3), as calcitriol is known to inhibit CYP27B1 [11, 12], which shares high structural and functional similarity with CYP27A1 [13–15]. Although serum levels of 1,25(OH)2D did not increase during the high-dose vitamin D supplementation, 25OHD is converted to 1,25(OH)2D in renal and extra-renal tissues, including the liver as well as breast cancer cells, where it is expected that the elevated circulating 25OHD results in increased conversion to 1,25(OH)2D [21]. Thus, the expected inhibition of CYP27A1 by calcitriol likely occurs locally in tissue after local 25OHD to 1,25(OH)2D conversion, resulting in decreased 27HC concentrations in multiple organs and decreased shedding of 27HC into the circulation and delivery to the breast. However, measurements of 27HC in tissues are necessary to assess this definitively, and there was not enough breast tissue from many subjects in this study to measure this effect directly in the breast tumors.
It is important to note that the changes observed in serum 27HC concentrations due to the high-dose supplements represent contributions from all tissues in the body, with the largest contribution likely deriving from the liver, where CYP27A1 expression is the highest. Although it is unclear to what degree the breast tissue contributes to the decrease in serum 27HC, CYP27B1 and CYP27A1 are both expressed in breast and breast cancer cells, and local conversion of vitamin D or 25OHD into 1,25(OH)2D and cholesterol into 27HC is known to occur in breast tumors [5, 22, 23]. Thus, the effect of high-dose vitamin D supplements to lower serum 27HC is likely reflected in the breast cancer tumors as well. Furthermore, decreasing circulating 27HC has been shown to inhibit tumor growth [5]. Therefore, the data in this work suggest that vitamin D supplementation may be a simple way to suppress 27HC-mediated ER stimulation in ER+ breast cancers by decreasing the 27HC concentration in the circulation. This beneficial action of vitamin D would be in addition to all of the other pathways by which vitamin D has been shown to inhibit the progression of breast cancer [8–10].
Two subjects were exceptions to the inverse correlation between 27HC and 25OHD, suggesting that there may be a more complex interaction between vitamin D and the regulation of the 27HC pathway. It is possible that these patients carry genetic variations affecting the vitamin D or cholesterol metabolic pathways, resulting in an increase in 27HC production despite high doses of vitamin D. A larger study is also needed to investigate the possibility that beyond some threshold serum 25OHD levels, increases rather than decreases in 27HC are observed, negatively impacting ER+ breast cancer patients.
No significant difference in circulating 1,25(OH)2D was observed between the low-dose and high-dose groups even though a significant increase in 25OHD was observed because the concentration of 1,25(OH)2D in the blood is tightly regulated by serum calcium and phosphate levels and parathyroid hormone in order to maintain mineral homeostasis [9]. Because the local synthesis of 1,25(OH)2D in the breast and in breast cancer tumors depends primarily on serum 25OHD levels [24], the effective 1,25(OH)2D concentrations in the breast tumors and other tissues of the high-dose group acting in a paracrine manner were likely increased [20, 24, 25]. It should be noted that the high dose of 10,000 IU of vitamin D was used because of the very short interval of therapy—1 to 6 weeks—between diagnosis and surgery. The optimal dose of vitamin D, or the 25OHD concentration to be targeted to elicit a decrease in 27HC, is not yet established because dose–response studies were not carried out. Furthermore, longer longitudinal studies are necessary to determine the dose and time course of vitamin D therapy required to reduce 27HC and to establish further whether vitamin D supplementation contributes to a clinical outcome benefit in ER+ breast cancer patients.
Although a larger study is needed to verify the findings that vitamin D supplements can be used to reduce 27HC levels in the circulation and that inhibition of 27HC production via CYP27A1 inhibition is the mechanism by which 27HC levels are reduced, the preliminary data presented here give evidence for 27HC regulation by vitamin D. In practice, we envision that vitamin D supplements that raise circulating 25OHD levels can be used preventatively to suppress 27HC-mediated ER+ breast cancer growth in patients who have a high risk of developing ER+ breast cancer, and during cancer treatment to contribute to other therapies to minimize breast cancer growth before and after surgery. This effect to reduce 27HC is in addition to the many previously described actions of vitamin D to inhibit breast cancer growth and progression [8–10, 26, 27]. Vitamin D supplements may be particularly useful for those whose breast cancer treatment includes aromatase inhibitors and who become resistant to that therapy. In long-term estrogen-deprived breast cancer cells, CYP27A1 is upregulated, suggesting that a dominant driver of ER+ breast cancer may be 27HC in the cases of patients who develop resistance to aromatase inhibitors [28].
In conclusion, this work suggests that vitamin D supplementation targeting 27HC might be a useful addition to current therapies for ER+ breast cancer. The finding requires verification in a larger study. Also, we are suggesting only that vitamin D supplementation be an adjunct to other indicated therapies and that vitamin D deficiency be checked for and treated in all breast cancer patients. However, because for two subjects a rise in 27HC was observed during vitamin D supplementation, 27HC levels should be monitored during vitamin D supplementation to ensure that these supplements are benefiting rather than hindering the treatment of breast cancer patients.
Supplementary Material
Acknowledgements
The authors would like to acknowledge funding for this project from the Vincent Coates Foundation Mass Spectrometry Laboratory in the form of a SUMS Seed Grant. We are grateful to Dr. Melinda Telli, Dr. Kristin Jensen, and members of the Feldman Lab that carried out this trial for their generous access to serum specimens of many of the subjects.
Abbreviations
- 1,25(OH)2D
1,25-Dihydroxyvitamin D
- 25OHD
25-Hydroxyvitamin D
- 27HC
27-Hydroxycholesterol
- ER+
Estrogen receptor-positive
- LC–MS/MS
Liquid chromatography tandem mass spectrometry
- SERM
Selective estrogen receptor modulator
- SRM
Selected reaction monitoring
Footnotes
Conflict of interest The authors declare that they have no conflict of interest.
Electronic supplementary material The online version of this article (https://doi.org/10.1007/s10549-017-4562-4) contains supplementary material, which is available to authorized users.
References
- 1.Umetani M, Domoto H, Gormley AK, Yuhanna IS, Cummins CL, Javitt NB, Korach KS, Shaul PW, Mangelsdorf DJ (2007) 27-Hydroxycholesterol is an endogenous SERM that inhibits the cardiovascular effects of estrogen. Nat Med 13:1185–1192 [DOI] [PubMed] [Google Scholar]
- 2.DuSell CD, Umetani M, Shaul PW, Mangelsdorf DJ, McDonnell DP (2008) 27-Hydroxycholesterol is an endogenous selective estrogen receptor modulator. Mol Endocrinol 22:65–77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu Q, Ishikawa T, Sirianni R, Tang H, McDonald JG, Yuhanna IS, Thompson B, Girard L, Mineo C, Brekken RA, Umetani M, Euhus DM, Xie Y, Shaul PW (2013) 27-Hydroxycholesterol promotes cell-autonomous ER-positive breast cancer growth. Cell Rep 5:637–645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nelson ER, Wardell SE, McDonnell DP (2015) Abstract A82: the cholesterol metabolite, 27-hydroxycholesterol, promotes breast cancer metastasis. Cancer Immunol Res 3:A82 [Google Scholar]
- 5.Nelson ER, Wardell SE, Jasper JS, Park S, Suchindran S, Howe MK, Carver NJ, Pillai RV, Sullivan PM, Sondhi V, Umetani M, Geradts J, McDonnell DP (2013) 27-Hydroxycholesterol links hypercholesterolemia and breast cancer pathophysiology. Science 342:1094–1098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kimbung S, Chang C, Bendahl P-O, Dubois L, Thompson WJ, McDonnell DP, Borgquist S (2017) Impact of 27-hydroxylase (CYP27A1) and 27-hydroxycholesterol in breast cancer. Endocr Relat Cancer 24:339–349 [DOI] [PubMed] [Google Scholar]
- 7.Haussler MR, Whitfield GK, Kaneko I, Haussler CA, Hsieh D, Hsieh JC, Jurutka PW (2013) Molecular mechanisms of vitamin D action. Calcif Tissue Int 92:77–98 [DOI] [PubMed] [Google Scholar]
- 8.Krishnan AV, Feldman D (2011) Mechanisms of the anti-cancer and anti-inflammatory actions of vitamin D. Annu Rev Pharmacol Toxicol 51:311–336 [DOI] [PubMed] [Google Scholar]
- 9.Feldman D, Krishnan AV, Swami S, Giovannucci E, Feldman BJ (2014) The role of vitamin D in reducing cancer risk and progression. Nat Rev Cancer 14:342–357 [DOI] [PubMed] [Google Scholar]
- 10.Luo W, Johnson CS, Trump DL (2016) Vitamin D signaling modulators in cancer therapy. Vitam Horm 100:433–472 [DOI] [PubMed] [Google Scholar]
- 11.Takeyama K-i, Kitanaka S, Sato T, Kobori M, Yanagisawa J, Kato S (1997) 25-Hydroxyvitamin D3 1α-hydroxylase and vitamin D synthesis. Science 277:1827–1830 [DOI] [PubMed] [Google Scholar]
- 12.Murayama A, Takeyama K-i, Kitanaka S, Kodera Y, Hosoya T, Kato S (1998) The promoter of the human 25-hydroxyvitamin D3 1 alpha-hydroxylase gene confers positive and negative responsiveness to PTH, calcitonin, and 1 alpha,25(OH)2D3. Biochem Biophys Res Commun 249:11–16 [DOI] [PubMed] [Google Scholar]
- 13.Jones G, Prosser DE, Kaufmann M (2014) Cytochrome P450-mediated metabolism of vitamin D. J Lipid Res 55:13–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Axen E, Postland H, Sioberg H, Wikvall K (1994) Liver mitochondrial cytochrome P450 CYP27 and recombinant-expressed human CYP27 catalyze 1 alpha-hydroxylation of 25-hydroxyvitamin D3. Proc Natl Acad Sci USA 91:10014–10018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sawada N, Sakaki T, Ohta M, Inouye K (2000) Metabolism of vitamin D3 by CYP27A1. Biochem Biophys Res Commun 273:977–984 [DOI] [PubMed] [Google Scholar]
- 16.Yin K, You Y, Swier V, Tang L, Radwan MM, Pandya AN, Agrawal DK (2015) Vitamin D protects against atherosclerosis via regulation of cholesterol efflux and macrophage polarization in hypercholesterolemic swine. Arterioscler Thromb Vasc Biol 35:2432–2442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Barchetta I, Carotti S, Labbadia G, Gentilucci UV, Muda AO, Angelico F, Silecchia G, Leonetti F, Fraioli A, Picardi A, Morini S, Cavallo MG (2012) Liver vitamin D receptor, CYP2R1, and CYP27A1 expression: relationship with liver histology and vita-min D3 levels in patients with nonalcoholic steatohepatitis or hepatitis C virus. Hepatology 56:2180–2187 [DOI] [PubMed] [Google Scholar]
- 18.McDonald JG, Smith DD, Stiles AR, Russell DW (2012) A comprehensive method for extraction and quantitative analysis of sterols and secosteroids from human plasma. J Lipid Res 53:1399–1409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vanlint S (2013) Vitamin D and Obesity. Nutrients 5:949–956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Swami S, Krishnan AV, Williams J, Aggarwal A, Albertelli MA, Horst RL, Feldman BJ, Feldman D (2016) Vitamin D mitigates the adverse effects of obesity on breast cancer in mice. Endocr Relat Cancer 23:251–264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Swami S, Krishnan AV, Wang JY, Jensen K, Horst R, Albertelli MA, Feldman D (2012) Dietary vitamin D(3) and 1,25-dihydroxyvitamin D(3) (calcitriol) exhibit equivalent anticancer activity in mouse xenograft models of breast and prostate cancer. Endocrinology 153:2576–2587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Townsend K, Banwell CM, Guy M, Colston KW, Mansi JL, Stewart PM, Campbell MJ, Hewison M (2005) Autocrine metabolism of vitamin D in normal and malignant breast tissue. Clin Cancer Res 11:3579–3586 [DOI] [PubMed] [Google Scholar]
- 23.Kemmis CM, Salvador SM, Smith KM, Welsh J (2006) Human mammary epithelial cells express CYP27B1 and are growth inhibited by 25-hydroxyvitamin D-3, the major circulating form of vitamin D-3. J Nutr 136:887–892 [DOI] [PubMed] [Google Scholar]
- 24.Krishnan AV, Swami S, Feldman D (2013) Equivalent anticancer activities of dietary vitamin D and calcitriol in an animal model of breast cancer: importance of mammary CYP27B1 for treatment and prevention. J Steroid Biochem Mol Biol 136:289–295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wagner D, Trudel D, Van der Kwast T, Nonn L, Giangreco AA, Li D, Dias A, Cardoza M, Laszlo S, Hersey K, Klotz L, Finelli A, Fleshner N, Vieth R (2013) Randomized clinical trial of vita-min D3 doses on prostatic vitamin D metabolite levels and ki67 labeling in prostate cancer patients. J Clin Endocrinol Metab 98:1498–1507 [DOI] [PubMed] [Google Scholar]
- 26.Aggarwal A, Feldman D, Feldman BJ (2017) Identification of tumor-autonomous and indirect effects of vitamin D action that inhibit breast cancer growth and tumor progression. J Steroid Biochem Mol Biol. 10.1016/j.jsbmb.2017.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Williams JD, Aggarwal A, Swami S, Krishnan AV, Ji L, Albertelli MA, Feldman BJ (2016) Tumor autonomous effects of vitamin D deficiency promote breast cancer metastasis. Endocrinology 157:1341–1347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nguyen VTM, Barozzi I, Faronato M, Lombardo Y, Steel JH, Patel N, Darbre P, Castellano L, Győrffy B, Woodley L, Meira A, Patten DK, Vircillo V, Periyasamy M, Ali S, Frige G, Minucci S, Coombes RC, Magnani L (2015) Differential epigenetic reprogramming in response to specific endocrine therapies promotes cholesterol biosynthesis and cellular invasion. Nat Commun 6:10044. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.