Description
A 59-year-old woman with a medical history of personality disorder (cluster B disorders: borderline and histrionic) and drug misuse was admitted to our hospital with increasing pain in the left buttock and thigh for the last 3 weeks. She was presenting a body temperature of 38.5°C. She reported self-injected doses of metamizole (2 mg two times per day), although this information was confirmed several days after admission.
On physical examination, she presented with a large, tender, fluctuant lump on the left buttock and upper half of the left thigh. The overlying skin was warm and red. Laboratory tests showed a white cell count of 16 300 leucocytes/mm3 (82% neutrophils and 10% bands), haemoglobin of 113 g/L and platelet count of 401×109/L. C reactive protein was 194 mg/dL (normal level: <5 mg/dL). Kidney, liver, lipids and urine panels were normal. Blood cultures were negatives.
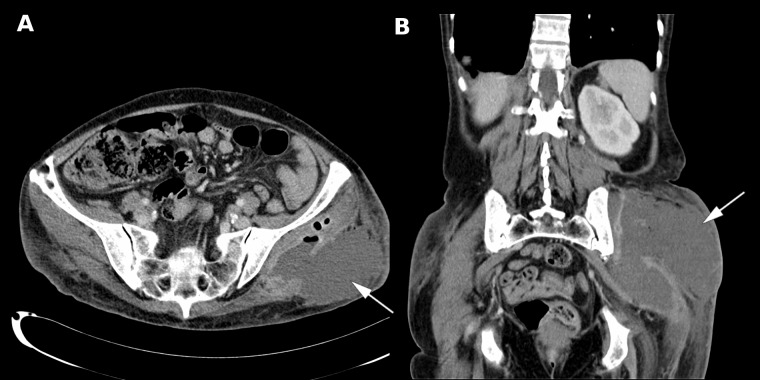
A CT scan confirmed a huge multilobulated abscess in the left buttock (measuring 15×11×8 cm), involving the left gluteal muscles, and containing gas bubbles (figure 1). The abscess had spread into the adjacent tissue and the left iliac crest.
Figure 1.
Abdominal CT scan showing how the abscess had replaced the three gluteal muscles and spread into the panniculus adiposus of the left buttock (slide A: transverse plane; slide B: coronal plane). Arrows are indicating the large abscess. Slide A also shows air bubbles inside the abscess.
We decided to initiate meropenem 1 g every 8 hours and linezolid 600 mg two times per day. She was then referred to the Department of Trauma and Orthopaedic Surgery, where she underwent drainage and surgical debridement of the infected, necrotic tissue. Muscle tissue samples revealed pure growth of Clostridium perfringens, sensitive to metronidazole, amoxicillin-clavulanate, piperacillin-tazobactam and meropenem. The patient was on meropenem for 4 weeks and on amoxicillin-clavulanate for 1 week. She improved rapidly, fever disappeared and C reactive protein was back in the normal range in the following 5 days. In a follow-up, 2 months after discharge, the patient was well, with no pain or functional impairment. A repeat CT scan was then performed, which showed a residual lesion measuring 1×0.8×0.8 cm.
Necrotising soft-tissue infections are rare, but severe, infections associated with high morbidity and mortality.1 Treatment should be aggressive, both surgical and antibiotic, and the outcome depends on the location, micro-organisms involved and patients’ prognostic factors, such as diabetes, immunosuppression, drug abuse and age. The microbiological profile is primarily polymicrobial, with both Gram-negative and Gram-positive bacteria. Streptococcus and Staphylococcus are the most commonly isolated bacteria in monomicrobial infections.2
Clostridium is a Gram-positive, anaerobic micro-organism, which is usually saprophytic, that can cause several syndromes, including soft-tissue infections.3 Several cases have been reported on severe C. perfringens infections and gas-forming abscesses, highlighting the mortality and the difficulty in establishing a diagnosis in the early stages.4
C. perfringens can release histotoxins (alpha, beta, epsilon and iota), some of which are able to cause gas gangrene and widespread necrotising soft-tissue infection.5 In our patient, gas inside the abscess led us to consider that an anaerobic micro-organism was responsible for the infection.
The patient was self-injecting doses of metamizole. Although she admitted this, she gave us no valid reason for doing so. It is worth noting that some studies have established a relationship between factitious disorder (Munchausen syndrome) and borderline disorder (cluster B personality disorder).6
Learning points.
Necrotising soft-tissue infections after intramuscular injections are not frequent, but may be associated with high morbidity and mortality.
Clostridium perfringens infections are not frequent micro-organisms causing necrotising soft-tissue infections, but gas-forming abscesses may lead us to suspect clostridial infections.
When suspected, early implementation of broad-spectrum antibiotic therapy, and surgical drainage and debridement are the key to manage this kind of abscess.
Footnotes
Patient consent for publication: Obtained.
Contributors: RGC wrote the first draft. MG-M and BR-M revised the draft. EI-A edited the CT slides.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Friederichs J, Torka S, Militz M, et al. . Necrotizing soft tissue infections after injection therapy: higher mortality and worse outcome compared to other entry mechanisms. J Infect 2015;71:312–6. 10.1016/j.jinf.2015.05.013 [DOI] [PubMed] [Google Scholar]
- 2. Stevens DL, Bisno AL, Chambers HF, et al. . Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the infectious diseases society of America. Clin Infect Dis 2014;59:147–59. 10.1093/cid/ciu444 [DOI] [PubMed] [Google Scholar]
- 3. Yang CC, Hsu PC, Chang HJ, et al. . Clinical significance and outcomes of Clostridium perfringens bacteremia-a 10-year experience at a tertiary care hospital. Int J Infect Dis 2013;17:e955–60. 10.1016/j.ijid.2013.03.001 [DOI] [PubMed] [Google Scholar]
- 4. van Bunderen CC, Bomers MK, Wesdorp E, et al. . Clostridium perfringens septicaemia with massive intravascular haemolysis: a case report and review of the literature. Neth J Med 2010;68:343–6. [PubMed] [Google Scholar]
- 5. Shindo Y, Dobashi Y, Sakai T, et al. . Epidemiological and pathobiological profiles of Clostridium perfringens infections: review of consecutive series of 33 cases over a 13-year period. Int J Clin Exp Pathol 2015;8:569–77. [PMC free article] [PubMed] [Google Scholar]
- 6. Gordon DK, Sansone RA. A relationship between factitious disorder and borderline personality disorder. Innov Clin Neurosci 2013;10:11–13. [PMC free article] [PubMed] [Google Scholar]