Summary:
Nipple-sparing mastectomy (NSM) places greater stress on the breast-skin envelope compared with traditional mastectomy techniques. Precise mastectomy flap dissection is critical to optimize breast skin flap thickness and minimize complication risk. This study evaluated patient-specific factors associated with mastectomy flap quality to improve technical success in NSM. Ideal NSM flap thickness was determined for all NSMs from 2006 to 2016 with available preoperative breast magnetic resonance imaging (MRIs). Demographic, operative variables, and flap thickness were compared for NSMs as stratified by body mass index (BMI) and mastectomy weight. Of the 1,037 NSMs, 420 cases (40.5%; 243 patients) had MRI data available, which included 379 (36.5%) preoperative breast MRIs. Average BMI was 24.08 kg/m2, whereas average mastectomy weight was 442.28 g. NSMs were classified according to BMI <25 kg/m2, 25–30 kg/m2, and >30 kg/m2. Average ideal overall NSM flap thicknesses in these groups were 10.43, 12.54, and 14.91 mm, respectively. Each incremental increase in average overall NSM flap thickness per BMI category was statistically significant (P < 0.0001; P < 0.0001; P = 0.0002). NSMs were also classified into mastectomy weight categories: <400 g, 400–799 g, and ≥800 g. Average overall NSM flap thicknesses in these groups were 9.97, 12.21, and 14.50 mm, respectively. Each incremental increase in average overall NSM flap thickness per mastectomy weight category was similarly statistically significant (P < 0.0001; P < 0.0001; P < 0.0001). NSM flap thickness and quality is related to BMI and breast size. Characterizing these anatomic variations preoperatively will help surgeons optimize mastectomy flap dissections and minimize ischemic complications in breast reconstruction after NSM.
INTRODUCTION
Nipple-sparing mastectomy (NSM) is a technically challenging procedure that places greater ischemic stress on the breast-skin envelope compared with traditional mastectomy techniques.1–6 Mastectomy flap quality is perhaps the most important factor in successful immediate breast reconstruction after NSM.3,7 After NSM, the perfusion of the breast-skin flap and nipple-areola complex is dependent on the superficial vasculature in the subcutaneous and subdermal levels.8–14 Therefore, precise mastectomy flap dissection at the level of the breast capsule is critical to optimize breast skin flap thickness, minimizing ischemic complications while maximizing oncologic resection. The variable nature of the breast subcutaneous and skin thickness superficial to the fascia has been previously discussed as absolute mastectomy flap thickness will vary by patient.8,15–17 However, if mastectomy dissection is precise at the superficial breast fascia level, an ideal and individualized mastectomy flap thickness will be produced.
The influence of patient-specific factors on mastectomy flap quality and thickness, most notably body mass index (BMI) and breast size, have not been completely elucidated.15 We therefore seek to evaluate these important patient-specific factors in relation to mastectomy flap quality.
METHODS
All NSMs undergoing immediate breast reconstruction performed from 2006 to June 2016 were reviewed. A blinded reviewer measured ideal flap thicknesses for NSMs with available preoperative magnetic resonance imaging (MRI) data at 12 different locations on each breast as measured from the skin to the breast capsule level. This distance was defined as the “ideal” flap thickness as there was no physical flap dissected in these preoperative MRIs. Three measurements were taken on superior and inferior flaps each, in the sagittal plane as well as on medial and lateral flaps in the axial plane. These 3 measurements corresponded with anterior, middle, and posterior locations taken at one-quarter, one-half, and three-quarters the length of the total anteroposterior distance of each breast. Although thickness varies throughout the breast, these averaged measurements best represented ideal mastectomy flap thicknesses that were independent of the actual mastectomy flap thickness produced in the operating room. All images acquired were using a dedicated breast coil on 1.5-Tesla and 3-Tesla magnets with T1-weighted nonfat suppressed volumetric scans and high-resolution postcontrast scans. A full description of the method of measurement is included in our previous article.7
NSMs were then stratified according to BMI (<25 kg/m2, 25–30 kg/m2, and >30 kg/m2) and mastectomy weight (<400 g, 400–799 g, and ≥800 g). NSM flap thicknesses in the overall, anterior, middle, and posterior dimensions were compared among these various groups. Descriptive statistics, measures of central tendency, and Student’s t tests were used as appropriate. All statistical analysis was performed using GraphPad Software, Inc. (La Jolla, Calif.).
RESULTS
Of 1,037 NSM reconstructions, 379 (36.5%) had preoperative breast MRIs. Average BMI was 24.08 kg/m2, whereas average mastectomy weight was 442.28 g.
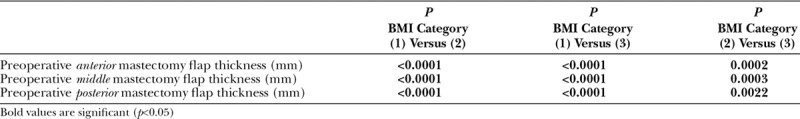
Average overall ideal NSM flap thicknesses per BMI subcategories were 10.43 in patients with BMI <25 kg/m2, 12.54 in BMIs of 25–30 kg/m2, and 14.91 mm in BMIs and >30 kg/m2. Each incremental increase in average overall NSM flap thickness per BMI category was statistically significant (P < 0.0001; P < 0.0001; P = 0.0002). The R2 correlation value of flap thickness with increasing BMI was 0.26. Each category increase in BMI was also associated with a significant increase in NSM flap thickness in the anterior, middle, and posterior dimensions.
Average overall ideal NSM flap thicknesses in NSMs classified by mastectomy weight categories were 9.97 for weight <400 g, 12.21 for 400–799 g, and 14.50 mm for ≥800 g. Each incremental increase in average overall NSM flap thickness per mastectomy weight category was statistically significant (P < 0.0001; P < 0.0001; P < 0.0001). The R2 correlation value of flap thickness with increasing BMI was 0.23. Each category increase in mastectomy weight was also associated with a significant increase in NSM flap thickness in the anterior, middle, and posterior dimensions (Tables 1–3).
Table 1.
Average Overall NSM Flap Thickness as Measured on Preoperative MRI Stratified by Body Mass Index and Mastectomy Weight
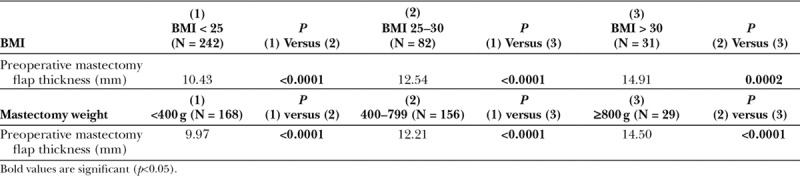
Table 3.
P Values in Comparing Average Anterior, Middle, and Posterior NSM Flap Thicknesses as Measured on Preoperative MRI Stratified by Mastectomy Weight Categories
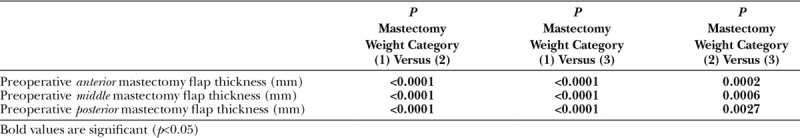
Table 2.
P Values in Comparing Average Anterior, Middle, and Posterior NSM Flap Thicknesses as Measured on Preoperative MRI Stratified by Body Mass Index Categories
DISCUSSION
Ischemic complications after nipple-sparing mastectomy (NSM) can be devastating and risk reconstructive failure.3,18,19 Mastectomy flap perfusion and quality is a critical determinant of ability to achieve a successful immediate breast reconstruction after NSM.3,7,16,17 Mastectomy flap thickness appears to be a suitable proxy for mastectomy flap quality in predicting ischemic complications in NSM. It has previously been demonstrated that thinner postoperative mastectomy flaps and lower preoperative/postoperative NSM flap thickness ratios are associated with increased ischemic complications in NSM.7 This underscores the importance of maximizing oncologic resection while minimizing trauma to the breast-skin envelope.
The ideal NSM flap includes the entire skin and subcutaneous fat thickness of the breast superficial to the breast fascia. The absolute value of this thickness is variable by patient and technical execution. Patient-specific factors, such as BMI and breast size, seem most likely to influence the nature of these specific breast tissue layers. The identification of this variability in mastectomy flap thickness is important to guide understanding and execution of proper anatomic dissection in NSM. However, prior studies are lacking in terms of intraoperative or pathologic tissue assessment and generalizability to NSM.15–17 Specifically, Larson et al.20 utilized breast reduction specimens to estimate mastectomy flap thickness and found a median thickness of approximately 1 cm with no dependence on patient-specific factors.17 However, breast reduction specimens have an inherently smaller skin component for analysis, limiting generalizability to NSM.17 Therefore, we utilized preoperative MRI as a modality to evaluate patient’s individualized, intrinsic, and ideal mastectomy flap thickness as a composite average from 12 points on the breast.
Our findings reveal that increasing ideal mastectomy flap thickness is significantly associated with increasing patient BMI and mastectomy weight, which served as surrogate for breast size. As patients were grouped into increasing BMI and mastectomy weight categories, average overall as well as anterior, middle, and posterior flap thicknesses increased significantly with BMI > 30 kg/m2 and mastectomy weight ≥800 g having the thickest flaps. Moreover, correlation values were similarly positive for BMI and mastectomy weight, suggesting a near equal effect of these patient-specific factors on NSM flap thickness.
As NSM places greater stress on the breast skin envelope, especially in the setting of immediate breast reconstruction,3,4 these findings are important as surgeons strive to optimize outcomes in breast reconstruction overall.20,21 We demonstrate that ideal mastectomy flap thickness is not a one-size-fits-all and varies significantly by patient-specific factors including BMI and breast size. Therefore, it is imperative that NSM flap dissection be performed precisely and in a patient-specific manner at the level of the superficial breast fascia to maximize success.
Footnotes
Published online 11 January 2019.
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Bailey CR, Ogbuagu O, Baltodano PA, et al. Quality-of-life outcomes improve with nipple-sparing mastectomy and breast reconstruction. Plast Reconstr Surg. 2017;140:219–226. [DOI] [PubMed] [Google Scholar]
- 2.Rodriguez-Feliz J, Codner MA. Embrace the change: incorporating single-stage implant breast reconstruction into your practice. Plast Reconstr Surg. 2015;136:221–231. [DOI] [PubMed] [Google Scholar]
- 3.Frey JD, Choi M, Salibian AA, et al. Comparison of outcomes with tissue expander, immediate implant, and autologous breast reconstruction in greater than 1000 nipple-sparing mastectomies. Plast Reconstr Surg. 2017;139:1300–1310. [DOI] [PubMed] [Google Scholar]
- 4.Choi M, Frey JD, Alperovich M, et al. “Breast in a Day”: examining single-stage immediate, permanent implant reconstruction in nipple-sparing mastectomy. Plast Reconstr Surg. 2016;138:184e–191e. [DOI] [PubMed] [Google Scholar]
- 5.Murthy V, Chamberlain RS. Defining a place for nipple sparing mastectomy in modern breast care: an evidence based review. Breast J. 2013;19:571–581. [DOI] [PubMed] [Google Scholar]
- 6.Galimberti V, Vicini E, Corso G, et al. Nipple-sparing and skin-sparing mastectomy: review of aims, oncological safety and contraindications. Breast. 2017;34:S82–S84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Frey JD, Salibian AA, Choi M, et al. Mastectomy flap thickness and complications in nipple-sparing mastectomy: objective evaluation using magnetic resonance imaging. Plast Reconstr Surg Glob Open. 2017;5:e1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Robertson SA, Rusby JE, Cutress RI. Determinants of optimal mastectomy skin flap thickness. Br J Surg. 2014;101:899–911. [DOI] [PubMed] [Google Scholar]
- 9.Seitz IA, Nixon AT, Friedewald SM, et al. “NACsomes”: a new classification system of the blood supply to the nipple areola complex (NAC) based on diagnostic breast MRI exams. J Plast Reconstr Aesthet Surg. 2015;68:792–799. [DOI] [PubMed] [Google Scholar]
- 10.Cunningham L. The anatomy of the arteries and veins of the breast. J Surg Oncol. 1977;9:71–85. [DOI] [PubMed] [Google Scholar]
- 11.van Deventer PV. The blood supply to the nipple-areola complex of the human mammary gland. Aesthetic Plast Surg. 2004;28:393–398. [DOI] [PubMed] [Google Scholar]
- 12.O’Dey Dm, Prescher A, Pallua N. Vascular reliability of nipple-areola complex-bearing pedicles: an anatomical microdissection study. Plast Reconstr Surg. 2007;119:1167–1177. [DOI] [PubMed] [Google Scholar]
- 13.Başaran K, Ucar A, Guven E, et al. Ultrasonographically determined pedicled breast reduction in severe gigantomastia. Plast Reconstr Surg. 2011;128:252e–259e. [DOI] [PubMed] [Google Scholar]
- 14.Hall-Findlay EJ, Shestak KC. Breast reduction. Plast Reconstr Surg. 2015;136:531e–544e. [DOI] [PubMed] [Google Scholar]
- 15.Larson DL, Basir Z, Bruce T. Is oncologic safety compatible with a predictably viable mastectomy skin flap? Plast Reconstr Surg. 2011;127:27–33. [DOI] [PubMed] [Google Scholar]
- 16.Algaithy ZK, Petit JY, Lohsiriwat V, et al. Nipple sparing mastectomy: can we predict the factors predisposing to necrosis? Eur J Surg Oncol. 2012;38:125–129. [DOI] [PubMed] [Google Scholar]
- 17.De Vita R, Zoccali G, Buccheri EM, et al. Outcome evaluation after 2023 nipple-sparing mastectomies: our experience. Plast Reconstr Surg. 2017;139:335e–347e. [DOI] [PubMed] [Google Scholar]
- 18.Colwell AS, Tessler O, Lin AM, et al. Breast reconstruction following nipple-sparing mastectomy: predictors of complications, reconstruction outcomes, and 5-year trends. Plast Reconstr Surg. 2014;133:496–506. [DOI] [PubMed] [Google Scholar]
- 19.Reish RG, Lin A, Phillips NA, et al. Breast reconstruction outcomes after nipple-sparing mastectomy and radiation therapy. Plast Reconstr Surg. 2015;135:959–966. [DOI] [PubMed] [Google Scholar]
- 20.Larson DL, Basir Z, Bruce T. Is oncologic safety compatible with a predictably viable mastectomy skin flap? Plast Reconstr Surg. 2011;127:27–33. [DOI] [PubMed] [Google Scholar]
- 21.Gfrerer L, Mattos D, Mastroianni M, et al. Assessment of patient factors, surgeons, and surgeon teams in immediate implant-based breast reconstruction outcomes. Plast Reconstr Surg. 2015;135:245e–252e. [DOI] [PubMed] [Google Scholar]
- 22.Albornoz CR, Bach PB, Mehrara BJ, et al. A paradigm shift in U.S. Breast reconstruction: increasing implant rates. Plast Reconstr Surg. 2013;131:15–23. [DOI] [PubMed] [Google Scholar]


