Abstract
Background:
The eyelid crease plays a very important role in determining eyelid symmetry. This study was performed to compare the cosmetic results post silicone rod frontalis suspension surgery, performed with and without eyelid crease formation, for correction of unilateral, congenital ptosis.
Methods:
Prospective, interventional study. One hundred patients with unilateral, congenital ptosis, with poor levator muscle action, operated on by a single facial plastic surgeon, over 5-year duration (2011–2016). Group I had 50 patients, who underwent silicone sling (Bvi Visitec) frontalis suspension surgery. Group II had 50 patients, who underwent frontalis suspension silicone sling (Bvi Visitec) surgery, in combination with eyelid crease formation and levator muscle excision (when required). The cosmetic outcomes were evaluated by the patients themselves and by 3 blinded physician observers and recorded objectively via a 5-point questionnaire, after a 1-year follow-up.
Results:
Patients in group II were much more satisfied than the patients in group I, as confirmed by the subjective and objective evaluations.
Conclusion:
The silicone sling frontalis suspension surgery, when combined with eyelid crease creation and levator excision procedure (when required), provides better symmetry, superior cosmesis, and excellent patient satisfaction.
INTRODUCTION
The main etiologic categories for blepharoptosis are myogenic, aponeurotic, neurogenic, mechanical, and traumatic.1–3 Treatment options for eyelid ptosis correction mainly depend upon levator palpebrae superioris muscle (LPS) action.4–6 Frontalis suspension is the recommended surgery, indicated in patients with severe, congenital ptosis, with poor LPS action (≤4 mm).4–6 The basic surgical technique has remained unchanged since its inception, except for the incorporation of newer sling materials. Various sling materials can be used and silicone rod slings are among the latest options, associated with multiple advantages.7–9 Although the functional outcomes of clearing of the visual axes are important, especially in children with the possibility of developing amblyopia, acceptable cosmetic results achieved by creating an upper eyelid crease and eyelid symmetry with the other eyelid are equally important.10,11
The frontalis suspension surgery using the silicone rod gives decent cosmetic results, with the margin reflex distance (MRD) of the eye that has been operated on being equal to that of the normal eye in multiple studies.12–14 However, patients are still unhappy. On questioning our patients, it was determined that patient dissatisfaction was mainly driven by the absence of the eyelid crease in the operated eye. Besides, in this traditional frontalis suspension surgery, the atonicity of the nonfunctioning LPS, the bunching up of the levator muscle, and the overlying lax eyelid skin on tightening the sling lead to the formation of multiple nonaesthetic eyelid folds. This absence of the eyelid crease and the formation of eyelid folds impair symmetry with the normal eye and hamper patient satisfaction.
To treat these problems better, the traditional silicone sling frontalis suspension surgery technique was combined with eyelid crease formation and levator muscle excision (when required). In this article, the results with this modified silicone sling frontalis suspension procedure are compared with the traditional frontalis sling procedure.
METHODS
This was a prospective, interventional study, which was conducted from January 2011 to August 2016 at a tertiary care, facial plastic surgery center (The Esthetic Clinics) in Mumbai, India. Institutional review board approval was obtained. A written informed consent for surgery, and to publish the relevant clinical photographs, was obtained from all concerned patients. The patient written consent for surgery mentioned that we were performing this study to evaluate and to compare the cosmetic results post silicone rod frontalis suspension surgery, performed with and without eyelid crease formation, for correction of unilateral, congenital ptosis.
All consecutive, unilateral, congenital blepharoptosis patients, associated with poor LPS action, coming to the facility, were included in the study. Exclusion criteria were presence of Marcus Gunn jaw winking, strabismus, previous eyelid surgery, history of trauma and lid laceration, weak Bell’s phenomenon (less than 2+), dry eye and other ocular surface abnormalities, and systemic disorder associated with ptosis, such as myasthenia gravis, myotonic dystrophy, dysthyroid ophthalmopathy, blepharophimosis, and chronic progressive external ophthalmoplegia.
The 2 groups were matched in terms of age and LPS action. The patients were randomly allocated to group I and group II, using a random number enumerator. There were no relevant demographic differences between these 2 groups. All patients were operated on by a single facial plastic surgeon. In group I (50 eyelids), a pentagonal approach was used, with 3 stab incisions above the brow and 2 supra-lash eyelid skin incisions. The silicone sling material was threaded through the forehead incisions and along the tarsal surface. In group II (50 eyelids), the eyelid crease of the normal eye was measured and an eyelid crease incision (at the same level as the other eye) was created in the eye being operated on, in addition to the earlier incisions. The levator muscle was extirpated through the eyelid crease incision, when required. The eyelid crease was created via the incision. The rest of the steps were the same as in group I. Preoperative and postoperative photographs, along with the medical sheets of all 100 patients (100 eyelids), who underwent surgical procedures, were maintained.
Data collected and analyzed included age, sex, follow-up, LPS function, pre and postoperative upper lid MRD-1, palpebral fissure height, margin crease distance (MCD), tarsal show, and subjective satisfaction scores (SSS) and objective assessment scores (OAS). Statistical analysis was performed using software SPSS 17.
Preoperative Evaluation
All patients underwent a complete eye examination, in addition to the detailed ptosis examination. Ptosis examination included measurement of eyelid crease height or the MCD, lid fissure height in primary gaze, LPS muscle function, MRD-1, MRD-2, lagophthalmos, scleral show, and Bell’s phenomenon, ranging from 4+ (implying complete disappearance of the cornea underneath the upper lid) to zero (corresponding to complete absence of Bell’s phenomenon).
In all the cases, the eyelid crease could only be imagined preoperatively, as being represented by very few thin skin lines. Because the eyelid crease was not well defined, hence the preoperative MCD was taken as 0 mm, in the ptosis affected eye.
Operative Technique
Group I
Marking of the points for frontalis suspension was done in all the cases. After placing a lid plate for protection of the globe and using a #15 scalpel blade, 2 horizontal incisions 2 mm in length were made in the upper lid, 2 mm above the lash line through the skin and pretarsal muscle down to the tarsus. The temporal incision was placed over the 3 o’clock position of the limbus, and the nasal incision was placed over the 9 o’clock position of the limbus (Fig. 1).
Fig. 1.
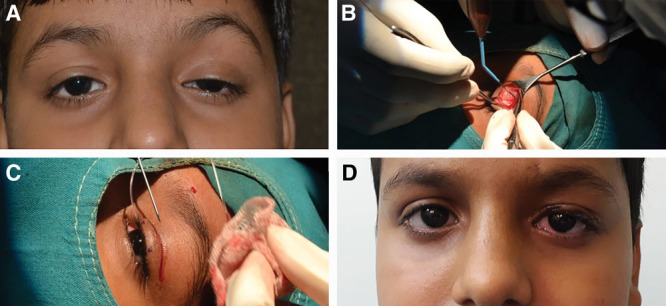
Steps of our modified technique. A, 11-year-old boy with left eye congenital ptosis with poor LPS function. B, Lid crease incision given and levator muscle is seen being dissected and extirpated. C, Silicone sling is then passed in the usual manner. D, 1 week postoperative photograph of the same boy showing symmetric lid crease and the supra tarsal show. There is still surgical edema seen in the lid tissues.
Three incisions, 2 mm in length each, were made above the upper border of the eyebrow in the skin and subcutaneous tissues to reach the frontal periosteum. The middle incision was placed 10 mm above the eyebrow. The medial and lateral incisions were placed at the upper border of the eyebrow, in line with the medial and lateral canthi, respectively, so as to form an isosceles triangle above the brow. A pocket was created above the central supra brow incision to bury the silicone sling knots, at the end of the procedure. Silicone sling (Bvi Visitec, Beaver Visitec International Ltd, United Kingdom) was passed from the central supra brow incision to the nasal supra brow incision, down to the supra lash incisions and back to the temporal supra brow incision and then finally coming out through the central supra brow incision (Fig. 1). The 2 ends of the silicone rod were passed through a silicone sleeve, to prevent slippage of the rod, postsurgery. An additional polypropylene 5-0 suture was used to tie the rod, below the sleeve, to prevent slippage. The silicone rod ends were buried deep in the frontalis muscle pocket. The brow incisions were sutured with 6-0 polypropylene. After completion of the procedure, antibiotic ointment was applied, and a Frost suture was placed using 6-0 silk suture material.
Group II
The marking and incisions were made as in group I. Following which, the eyelid crease incision was marked, corresponding exactly to the eyelid crease of the other normal eye. The orbital septum was opened up and the LPS muscle examined. If the LPS muscle was seen to be bunching up, on mechanically raising the eyelid, the excess LPS muscle was transected and extirpated, leaving just enough muscle stump till the upper tarsal edge (with the eyelid in raised position), without any bunching. The silicone sling was then passed in the same fashion as described above for group I. The orbicularis muscle at the edges of the eyelid crease incision was sutured to the cut edges of the levator muscle, with 6-0 polyglactin interrupted stitches, to deepen and accentuate the crease. Closure was achieved in 2 layers ie orbicularis oculi with 6-0 polyglactin and skin using a running 6-0 polypropylene suture, before closing the brow incisions as described above. After completion of the procedure, antibiotic ointment was applied, and a Frost suture was placed using 6-0 silk suture material (Fig. 2).
Fig. 2.
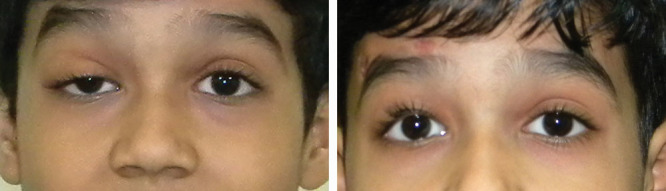
Results of patient in group I. Preoperative and postoperative photographs of patient, with right eye ptosis, with poor levator action. The patient underwent frontalis sling surgery in group I. Postoperative photograph of the patient shows asymmetric lid crease and fullness in the area above the lid crease, after frontalis sling surgery.
Mild compressive dressings were applied for corneal protection for 1 day, in both the groups. Oral antibiotic and analgesics were prescribed for 5 days. The Frost suture was removed the next morning, if no corneal epithelial defect was present. Removal of the Frost suture was deferred, until the corneal epithelial defect had healed completely.
Postoperative Follow-up
Postoperative eyelid creases, tarsal show, symmetry, and eyelid height were graded by 3 blinded, independent, physician observers as unacceptable, poor, fair, good and excellent result (1–5 grading, respectively). The physician observers were all more than 5 years post their residency/highest fellowship trainings, in surgery and dermatology. This OAS was assessed at the last follow-up, which was at 12 months postsurgery. Patient satisfaction grading was done similarly at 12 months postoperatively by a 5-point SSS as unacceptable, poor, fair, good, and excellent result (1–5 grading, respectively). Both OAS and SSS were based upon the following 2 questions:
1) How is the cosmesis postsurgery?
2) Is the operated eye symmetric with the other eye postsurgery?
Parents answered these questions on behalf of children aged less than 12 years of age. Testing field of vision was not possible in children less than 10 years of age. In other patients, confrontation method was used to assess the superior field of vision. Measurements of MRD-1, lid fissure height and eyelid crease height, were performed at 1, 3, and 12 months postoperatively. We considered MCD to be zero in our study in all the cases preoperatively. Hence, the complete distance from the upper eyelid margin to the lower border of brow becomes the effective tarsal show. However, once the lid crease is created and lid fold develops, the tarsal show became measurable from the upper eyelid margin till the lid fold. Thus, an effective “decrease” in the show of the skin on the upper eyelid (the tarsal show) was measured. We agree that using a pretarsal show may have been a better way to evaluate the patients, but would have made postoperative calculations extremely difficult.
Photography was performed, both in primary gaze and down gaze, preoperatively and repeated at 1, 3, and 12 months, for evaluation of upper lid contour and symmetry. Eyelid contour was evaluated using objective assessment of photographs. Paired preoperative and postoperative photographs were reviewed by all the 3 masked observers. Observers graded eyelid contour on a subjective scale: 0 = poor, 1 = fair, 2 = good. Triangular peaking, medial or lateral displacement of the high point, and flattening of the eyelid contour were assessed in the photographs. Postoperative complications, such as corneal surface disorders, overcorrection, under correction, and granuloma formation were also evaluated. Acceptable results consisted of crease and eyelid fissures that were symmetrical (≤1 mm difference) and of appropriate height. For patients with no complications, follow-up visits were performed at 1 and 4 weeks, 3 and 12 months after the operation. If necessary, the patients were examined more frequently.
RESULTS
A total of 100 eyelids of 100 patients, with 56 males and 44 females and mean age of 18.90 ± 14.56 (range, 2–53) years, underwent either one of the procedures. In group I, the mean age was 17.20 ± 14.96 (range, 2–51 years); in group II, the mean age was 20.60 ± 12.16 (range, 2–53 years).
Twenty-six eyelids from group II underwent levator resections.
In group I, OAS reported satisfactory results in terms of symmetrical lid fissure and lid crease, and less than 1 mm of under-correction or overcorrection was achieved in 48% of the cases. In group II, satisfactory results in terms of symmetrical lid fissure and lid crease, and less than 1 mm of under-correction or overcorrection, were achieved in 95% of cases. Eyelid contour was good in all patients, in both groups.
The mean OAS for question 1 in group I were 2.2, 2.7, and 2.1 for observer 1, 2, and 3, respectively. The mean OAS for question 2 in group I were 1.0, 1.6, and 1.1 for observer 1, 2, and 3, respectively. The mean OAS for question 1 in group II were 4.4, 3.9, and 4.5 for observer 1, 2, and 3, respectively. The mean OAS for question 2 in group II were 4.2, 3.8, and 3.9 for observer 1, 2, and 3, respectively. All the 3 examiners gave statistically similar results for both the questions with good agreement (kappa value = 0.615). OAS were better in group II as compared with group I, for both the questions, as analyzed by any of the 3 examiners (Pearson chi-square coefficient = 2.000, df = 3, P = 0.000). Intraobserver variability was calculated by reevaluation of 20 patients, 10 in each group, to confirm the scoring. The scores were found reliable on repeatability (kappa value = 0.810, very good agreement). The mean SSS in group I were 2.3 and 1.4 for question 1 and 2, respectively. The mean SSS in group II were 4.5 and 4.1 for question 1 and 2, respectively. Thus, SSS were better in group II, as compared with group I (Pearson’s chi-square coefficient = 1.700, df = 4, P = 0.000).
All subjects had congenital ptosis, associated with poor levator function. MRD-1 was increased by a mean of 3.05 ± 0.98 mm postoperatively (P = 0.001). MRD-1 in group I improved significantly from 0.25 ± 1.29 to 3.38 ± 0.56 [P value 0.000, analysis of variance (ANOVA); Fig. 3]. MRD-1 in group II improved significantly from 0.25 ± 1.23 to 3.00 ± 0.33 (P value 0.000, ANOVA; Fig. 4]. Intergroup comparison of MRD-1 (Mann Whitney test) showed no significant difference with P value of 0.07. Thus, the eyelid margin was raised similarly in both groups and functional ptosis correction was comparable in both the groups. In both the groups, patients were able to gain a clear, unrestricted, field of vision.
Fig. 3.

Results of patient in group II. Preoperative and postoperative photographs of a patient with symmetric lid crease and tarsal show, after modified frontalis sling surgery performed along with excision of the levator muscle.
Fig. 4.

Results of patient in group II. Preoperative and postoperative photographs of patient, showing symmetric lid crease and tarsal show, after modified frontalis sling surgery performed along with excision of the levator muscle.
MCD in group II improved significantly from 0 to 8.44 ± 0.86 mm (P value 0.000, ANOVA), as compared with no change in group I (Fig. 4). There was no significant statistical improvement in MCD in group I, as the eyelid crease was not formed in these patients. Rather, an eyelid fold formed overhanging the tarsal plate, rendering the tarsal show difficult to be appreciated (Fig. 3). Tarsal show improvement (decrease in tarsal show) occurred in all the patients in group I (P value = 0.358, ANOVA) and group II (P value = 0.000, ANOVA). However, it was statistically significant only in group II (P value = 0.000).
All the patients, in both groups, were able to close their eyes adequately, for corneal protection.
DISCUSSION
Symmetry between the eyelids is of utmost importance in achieving excellent cosmesis and superior patient satisfaction in unilateral ptosis. Even though frontalis sling suspension surgery performed in ptosis with poor LPS action can give patients an exactly matching palpebral aperture height and eliminate the ptosis completely,11–13,15 the patients are still not aesthetically completely satisfied.16
In literature, many modifications and suggestions are suggested to improve the eyelid crease formation, after frontalis sling surgery. Yagci and Egrilmez,16 in a retrospective review of 27 patients, reported better cosmetic outcomes, via a lid crease approach. They suggested passage of the sling through the tarsus, under direct visualization, which is made possible via a lid crease incision.16 Another study defined a refined fascial sling procedure, in which the fascial strip is anchored simultaneously to the upper margin of the tarsal plate and incision margin of the pre-tarsal lid, to produce a proper lid crease.17 Other surgeons prefer to refine the cosmetic appearance by reforming the lid crease as a second-stage procedure, a few months after the primary sling surgery.18,19
In our experience, an asymmetrical eye lid crease, post unilateral ptosis surgery, significantly hampers symmetry between the 2 eyelids (Fig. 3). Even though the MRD is exactly the same as in the other, normal eye this asymmetry leads to the perception of “still-a-ptotic upper eyelid” by the patient, thereby decreasing patient satisfaction.
In complex congenital ptosis, where patients have associated Marcus Gunn jaw winking phenomenon, ablation of a portion of the LPS muscle via an eyelid crease incision and resuspension of the eyelid to the brow are necessary, to abolish the associated synkinetic wink.20 This incision also leads to the development of a well-defined eyelid crease, leading to superior patient satisfaction. The difference clearly lies in the presence of the eyelid crease and the upper eyelid tarsal show, post silicone sling frontalis suspension ptosis surgery, in these patients.
A majority of ptosis patients with poor LPS action have a congenitally weak LPS muscle, which is thin, dystrophic and atonic.20 After conventional frontalis sling suspension surgery, this nonfunctional muscle bunches up and forms a fullness in the preseptal upper lid area. The absence of the tarsal show leads to further dissatisfaction in female patients, who complain that they have no place to apply eye mascara and/or eye shadow, in the eye that has been operated on, post ptosis surgery. We performed excision of the excess LPS muscle, on seeing a bunched up appearance. Closure of orbicularis and skin in layers helps to form a scar and further defines the eyelid crease (Fig. 4). It should be clearly noted, however, that the only role of the LPS excision is to improve the appearance of the supra-tarsal crease by removing the bunched up appearance created by an excess, atonic LPS muscle. The authors do not attribute a higher eyelid height to levator muscle excision. This technique of adding an eyelid crease incision has the added advantage of allowing excess skin removal through the eyelid crease incision (when required) and thus allowing a blepharoplasty, symmetrizing the eyelids even more.
In both the groups, patients were able to gain a clear unrestricted field of vision, because of comparable improvements in MRD-1. Cosmetic satisfaction quotient postsurgery was higher in group II.
CONCLUSIONS
Upper eyelid margin position (MRD-1) has been an obvious measure to grade the success of ptosis surgery since times immemorial. By incorporation of an additional lid crease incision and excision of the atonic levator muscle (when required), our modified frontalis sling surgery technique can better address symmetry between the eyelid creases and tarsal show in both the eyes. By using 2 groups, over a long follow-up, our study compares and clearly demonstrates the benefits that the modified surgical approach has in addressing these issues, thereby leading to greater patient satisfaction. The strength of this study is that this is a prospective study with blinded observers and involves a large number of patients.
In summary, we found statistically significant improvement in the surgical outcomes, using the modified surgical approach of frontalis suspension. Therefore, we recommend that creation of an eyelid crease and excision of the LPS muscle through the upper eyelid crease incision (when required) should be performed in all frontalis sling procedures performed in unilateral ptosis associated with poor LPS action.
ACKNOWLEDGMENT
The authors acknowledge the work of Dr. Ritesh Bansal who was instrumental in the statistical analysis of this study.
Footnotes
Published online 9 January 2019.
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Beard C. Ptosis. 1969:St. Louis, Miss.: Mosby; 39. [Google Scholar]
- 2.Frueh BR. The mechanistic classification of ptosis. Ophthalmology. 1980;87:1019–1021. [DOI] [PubMed] [Google Scholar]
- 3.Beard C. A new classification of blepharoptosis. Int Ophthalmol Clin. 1989;29:214–216. [DOI] [PubMed] [Google Scholar]
- 4.Beard C. A new treatment for severe unilateral congenital ptosis and for ptosis with jaw-winking. Am J Ophthalmol. 1965;59:252–258. [PubMed] [Google Scholar]
- 5.Beard C. The surgical treatment of blepharoptosis: a quantitative approach. Trans Am Ophthalmol Soc. 1966;64:401–487. [PMC free article] [PubMed] [Google Scholar]
- 6.Beard C. Ptosis. 1981:3rd ed St. Louis, Miss.: CV Mosby; 191–192. [Google Scholar]
- 7.Goldberger S, Conn H, Lemor M. Double rhomboid silicone rod frontalis suspension. Ophthalmic Plast Reconstr Surg. 1991;7:48–53. [DOI] [PubMed] [Google Scholar]
- 8.Carter SR, Meecham WJ, Seiff SR. Silicone frontalis slings for the correction of blepharoptosis: indications and efficacy. Ophthalmology. 1996;103:623–630. [DOI] [PubMed] [Google Scholar]
- 9.Tillett CW, Tillett GM. Silicone sling in the correction of ptosis. Am J Ophthalmol. 1966;62:521–523. [DOI] [PubMed] [Google Scholar]
- 10.Taherian K, Atkinson PL, Shekarchian M, et al. Comparative study of the subjective and objective grading of ptosis surgery outcomes. Eye (Lond). 2007;21:639–642. [DOI] [PubMed] [Google Scholar]
- 11.Goldberg RA, Lew H. Cosmetic outcome of posterior approach ptosis surgery (an American Ophthalmological Society thesis). Trans Am Ophthalmol Soc. 2011;109:157–167. [PMC free article] [PubMed] [Google Scholar]
- 12.Yoon JS, Lee SY. Long-term functional and cosmetic outcomes after frontalis suspension using autogenous fascia lata for pediatric congenital ptosis. Ophthalmology. 2009;116:1405–1414. [DOI] [PubMed] [Google Scholar]
- 13.Bernardini FP, Cetinkaya A, Zambelli A. Treatment of unilateral congenital ptosis: putting the debate to rest. Curr Opin Ophthalmol. 2013;24:484–487. [DOI] [PubMed] [Google Scholar]
- 14.Kersten RC, Bernardini FP, Khouri L, et al. Unilateral frontalis sling for the surgical correction of unilateral poor-function ptosis. Ophthalmic Plast Reconstr Surg. 2005;21:412–416; discussion 416. [DOI] [PubMed] [Google Scholar]
- 15.Lew H, Goldberg RA. Maximizing symmetry in upper blepharoplasty: the role of microptosis surgery. Plast Reconstr Surg. 2016;137:296e–304e. [DOI] [PubMed] [Google Scholar]
- 16.Yagci A, Egrilmez S. Comparison of cosmetic results in frontalis sling operations: the eyelid crease incision versus the supralash stab incision. J Pediatr Ophthalmol Strabismus. 2003;40:213–216. [DOI] [PubMed] [Google Scholar]
- 17.Chen TH, Yang JY, Chen YR. Refined frontalis fascial sling with proper lid crease formation for blepharoptosis. Plast Reconstr Surg. 1997;99:34–40. [DOI] [PubMed] [Google Scholar]
- 18.Allen RC, Hong ES, Zimmerman MB, et al. Factors affecting eyelid crease formation before and after silicone frontalis suspension for adult-onset myogenic ptosis. Ophthalmic Plast Reconstr Surg. 2015;31:227–232. [DOI] [PubMed] [Google Scholar]
- 19.Allard FD, Durairaj VD. Current techniques in surgical correction of congenital ptosis. Middle East Afr J Ophthalmol. 2010;17:129–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cates CA, Tyers AG. Results of levator excision followed by fascia lata brow suspension in patients with congenital and jaw-winking ptosis. Orbit. 2008;27:83–89. [DOI] [PubMed] [Google Scholar]


