Abstract
Background:
There is currently a mandate globally to incorporate patient’s perceptions of their illness into outcome measures, in order to provide a deeper insight into medical practice. Facial nerve palsy (FNP) is a devastating condition that can significantly impact quality of life. However, no measure currently exists that comprehensively assesses outcome in FNP using patient perception. The aim of this study is to explore patients’ experiences of FNP with the aim of informing the development of a patient-reported outcome measure.
Methods:
Presented is a qualitative study, using in-depth semi-structured interviews with FNP patients. An interview guide was developed using expert opinion and a literature review. Interpretative description was used as the qualitative approach. Interviews were audio-recorded, transcribed, and coded line-by-line. Codes were refined using the constant comparison approach. Interviews continued until data saturation was reached. The data were used to develop a conceptual framework of patient perceived issues relating to FNP.
Results:
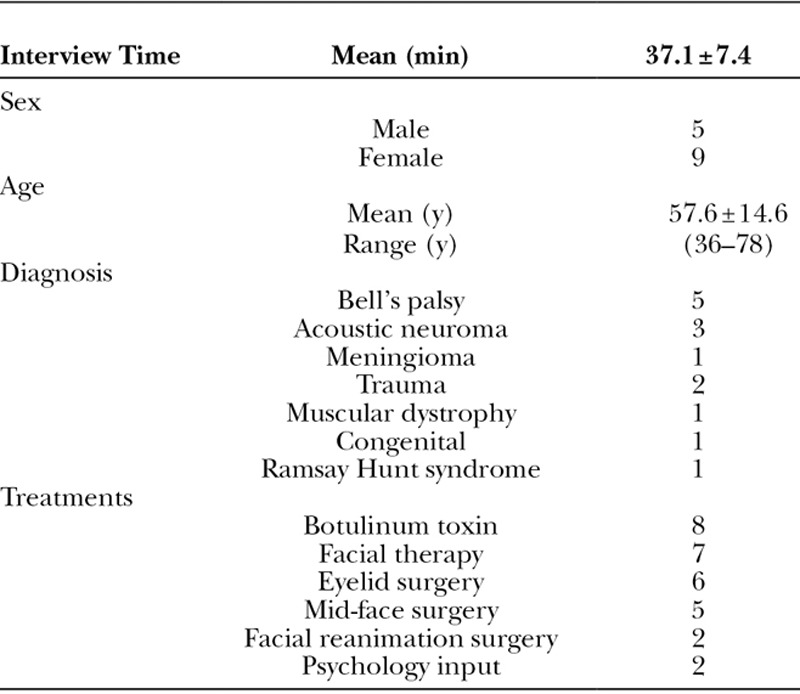
The sample included 5 men and 9 women aged 57.7 years (range, 36–78) with a range of causes of FNP, including Bell’s palsy (n = 5), acoustic neuroma (n = 3), trauma (n = 2), meningioma (n = 1), muscular dystrophy (n = 1), congenital (n = 1), and Ramsay Hunt syndrome (n = 1). Analysis of the 14 participant interviews led to identification of 5 major domains including “facial function concerns,” “appearance concerns,” “psychological function,” “social function,” and “experience of care.”
Conclusion:
This study provides a conceptual framework covering outcomes that matter to patients with FNP, which can be used to inform the development of a new comprehensive FNP-specific patient-reported outcome measure.
INTRODUCTION
Facial nerve palsy (FNP) is a debilitating condition that affects approximately 20,000 patients in the United Kingdom, with an annual incidence of 70 cases per 100,000 population.1 Facial weakness adversely impacts both appearance and function, affecting speech, vision, eating, drinking, hearing, and communication.2–4 This condition has the capacity to severely and detrimentally impact physical and psychosocial well-being.5,6
Outcome data have taken many forms over the years. Over a century ago, Florence Nightingale proposed a simple, 7-point outcome measure for her ward patients. This measure classified patients as: relieved, unrelieved, and dead.7 For many years since, mortality and morbidity data have been used to benchmark healthcare and assess its performance. Objective data of this type are undoubtedly essential to determining outcome; however used in isolation, it may not necessarily confer patient benefit.8 Currently, the term “health” has an accepted broader definition, that is not solely encompassed by mortality and morbidity data. Health is now viewed as complete physical, psychological, and social wellbeing and not merely the absence of disease9 and can be measured using patient-reported outcome measures (PROMs). PROMs measure outcomes that matter to patients [eg, symptoms, health-related quality of life (HR-QOL)] from their perspective.10 PROMs have been adopted in many healthcare sectors, particularly high volume services such as hip and knee replacement, varicose vein, and hernia surgery.11 PROMs are also increasingly used in patient-care, quality improvement activities, and comparative effectiveness research.11–15
Although the use of an evidence-based approach is generally accepted by the medical community, there is a paucity of evidence-based outcomes data to substantiate any benefit, and to highlight best practice for management of facial palsy. Importantly, there is a fundamental lack of understanding as to the effect of facial weakness on a patient’s well-being. If the key issues in facial palsy from the patient’s perspective are not fully conceptualized, any PROM developed for FNP will lack content validity.10 FNP services often use a clinician-based, subjective grading measure to ascertain surgical and nonsurgical outcomes. A systematic review by Ho et al.16 identified only 2 published disease-specific PROMs that displayed any degree of formal development; the Facial Disability Index (FDI) and Facial Clinimetric Evaluation (FacE) scales. These 2 outcome measures are the most commonly used in current practice (Fattah et al.,17 2014). The FDI scale measures physical function and social/well-being function.18 The FaCE scale incorporates more domains in its framework, but does not measure patient’s experience of care specifically relating their own treatment or information use.19
What is clear from available PROMs is that the impact of FNP on patient well-being is not fully understood, and there is currently no universally accepted or comprehensive PROM that measures outcomes for treatments that patients with FNP receive. A disease-specific PROM in FNP is needed, as generic PROMs, such as the 36-item Short Form Survey (SF-36)20 or Glasgow Benefit Inventory,21 do not ask any questions about facial appearance or facial function, and therefore lack content validity when used in the context of FNP.
The overall purpose of this study was to explore patient experience of FNP using a qualitative approach to gain a deeper understanding of outcomes from the patient perspective. This study constitutes the first phase in the creation of a PROM with the development of a descriptive conceptual model illustrating the patient perception of their condition. Specifically a robust approach, similar to that used in other studies that examined outcomes from the patient perspective22,23 was applied to ensure the validity, reliability, and usability of the findings.
METHODS
Research ethics approval was obtained from Queens Square Research Ethics Committee before interviewing patients (REC reference: 15/LO/1507, IRAS project ID: 176828). Oxford University Hospitals NHS Foundation Trust reviewed and sponsored the study.
This study employed a qualitative research approach to elicit concepts of interest from participants and form a conceptual framework. We took an applied health services research approach known as Interpretive Description, which assumes there is theoretical, clinical, and scientific knowledge, informing an understanding of the study topic for clinicians and researchers.24
A draft semistructured interview guide composed of open-ended questions (Appendix A) was developed by the research team based on an analysis of the relevant literature16 that reviewed content from HR-QOL scales such as the FDI18 and FaCE scales.19 The use of open-ended questions ensured that participants could describe their experiences of FNP in their own words, as opposed to using closed questions which predetermine domains of concern and may therefore be less sensitive.25 The interview guide was also informed by clinical knowledge from members of a FNP multi-disciplinary team at the Oxford University Hospitals NHS Trust. The draft guide was modified collaboratively by input from clinicians form the FNP clinic (a plastic surgeon, an ophthalmologist, a speech and language therapist, and a qualitative researcher) during a focus group session led by the lead investigator (J.H.N.).
Participants were purposively sampled from a database of patients who had attended the Oxford University Hospitals NHS Trust Facial Palsy Clinic. The sample was chosen to include patients with different types of FNP at different stages of treatment (pre-, during, and posttreatment). Any adult over 18 years of age with FNP was eligible for inclusion in this study. Non-English speaking patients or those with cognitive impairment were not eligible to participate in the study.
Participants were contacted by telephone to introduce the study and its objectives. Those patients who subsequently agreed to participate were provided (by e-mail or post) an information leaflet and consent form to sign and return. Interviews were conducted face-to-face by J.H.N. (a consultant oculoplastic surgeon and member of the facial palsy multidisciplinary team). Each interview was audio-recorded and transcribed verbatim. Data collection and analysis took place concurrently so that modifications could be made to the interview guide after each interview. Theoretical thinking was applied to the interview process to ensure that new concepts emerging from the data were incorporated into the interview guide. This allowed the lead investigator to determine relevance to subsequent participants. Interview sessions lasted between 30 and 60 minutes with the direction and length of the interview led by the participant.
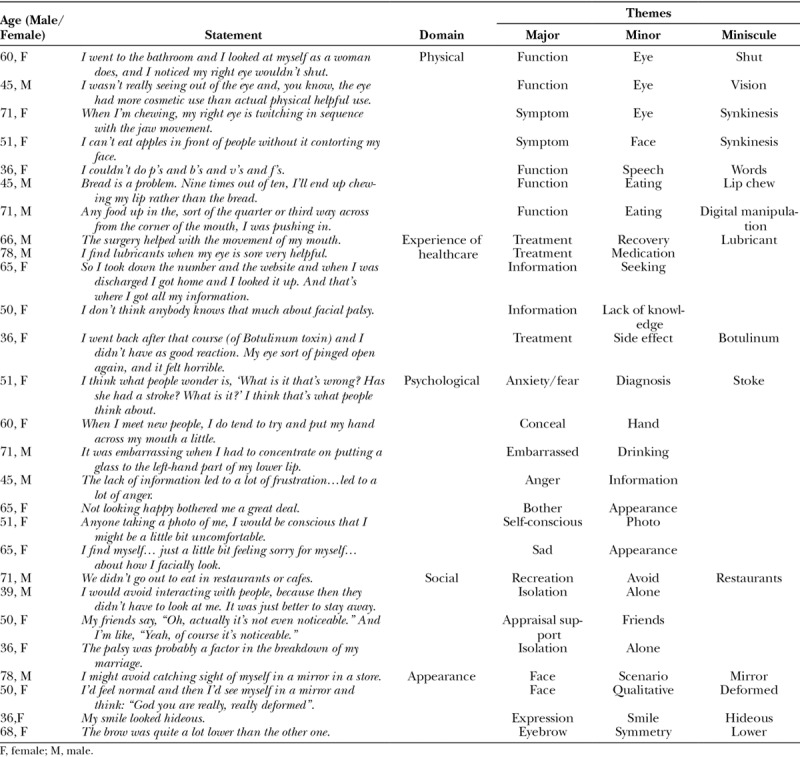
Each interview transcript was coded using a line-by-line approach. Quotes (participant words) that related to any aspect of outcome were transferred from the Word document into Excel along with specific participant characteristics (ie, age, sex, and type of facial paralysis) and coded by assigning them conceptual top-level domains, and major and minor themes. Constant comparison was used to refine the codes and ensure that all codes covering similar concepts were consistently coded. During the process of coding, we ensured that duplicate statements were removed to be able to identify themes important across the sample (rather than themes relating to one participant repeating a specific concern multiple times). Some statements could produce 2 codes, for example: “I get annoyed when I dribble.” This statement was coded as both a physical problem (“….when I dribble”) and also psychological issue (“I get annoyed…”). A codebook was constructed during this process, which assimilated and organized the codes for ease of use. The entire item pool of over 1,700 statements was examined by J.H.N. and items were simplified and generated. After each cycle of refinement, the framework was reviewed by a second observer (N.M.L.). This process of item generation and refinement stopped at the point when both observers agreed that no further modifications could be made. There were 5 cycles of data refinement before agreement was reached between observers. Interviews continued until no new concepts were elicited from additional interviews. Examples of how data were categorized are shown in Table 1. At this point, the conceptual model was complete.
Table 1.
Examples for How the Qualitative Data Were Categorized into Domains and Concepts
RESULTS
From a database of 172 facial palsy patients, a diverse sample of 24 patients were contacted and invited to participate in the study (12 male, 12 female) of which 14 participants agreed to participate and consent to the study (5 male, 9 female). Interviews were conducted over an 8-week period from May 2016 to June 2016. The characteristics of the sample, including diagnosis and treatments received, are shown in Table 2.
Table 2.
Characteristics of Individual Participants Interviewed in the Study
The sample provided a total of 1,623 codes that led to the identification of 5 top-level domains as follows: facial function and symptom (n = 551, 34%), experience of care (n = 334, 21%), psychological (n = 313, 19%), appearance-related (n = 223, 14%) and social function (n = 202, 12%; Fig. 1).
Fig. 1.
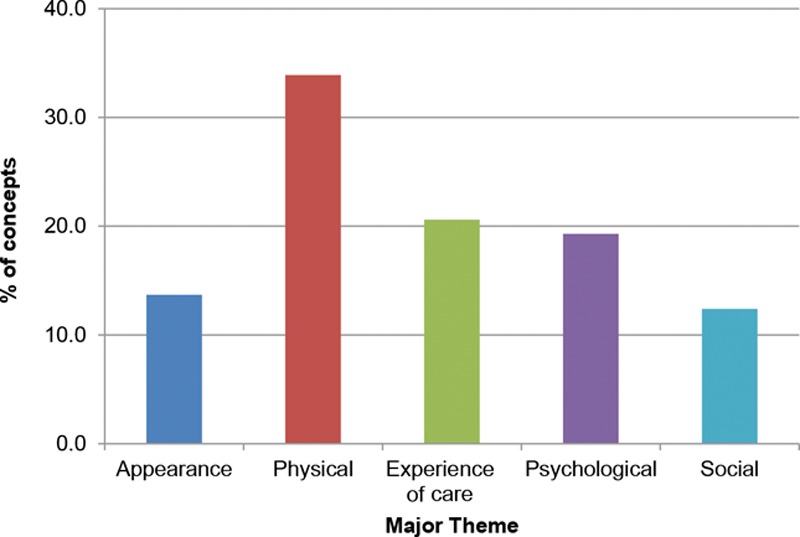
Percentage of major domains reported by participants.
Facial Function and Symptoms
Participants reported multiple issues relating to facial function and symptoms as a result of their FNP. These included problems relating to the jaw (eg, tiredness, tightness, and pain), mouth (eg, drooling, dribbling, dryness, and poor lip seal), breathing (eg, inhaling through the nose and dryness of the throat), sleep quality (often due to breathing problems), facial movement (eg, facial expression, smiling, and raising the eyebrow), and balance The most common facial function concerns related to the eye (37% of physical codes), the face in general (14%), speech (9%) and eating (8%).
With regard to the eye, participants reported both functional and symptom-related issues. The most frequent concern relating to the eye was visual disturbance discussed by 11 of 14 participants. Participants complained that their vision was often blurred as a result of exposure of the eye, watering or secondary to the ointment (which is further discussed in the “experience of care” section). Another functional complaint was involuntary closure of the eye relating to synkinesis. Representative quotes for the main subthemes can be seen in Table 1. The most common ocular symptoms were “watering” and “dryness.” Regarding the face, other adjectives used to describe synkinesis were “twitch,” “flicker,” and “contort.” Synkinesis was reported by 11 of 14 participants with over 40 comments made. Several participants described the face as feeling “tight,” “tense,” or “pulled.”
Seven of the 14 participants felt that their speech was impaired. A few participants (3/14) mentioned “slurring” as being a problem. Participants described difficulties with being understood by others and particularly referenced the difficulty with the pronunciation of certain letters or words.
Eating and drinking were important issues for participants in our sample. The 2 most common concerns were 1-sided eating (only being able to chew food on 1 side of the mouth) and oral incompetence (where food falls out of the mouth resulting in fingering the food back into the mouth). Participants also discussed dribbling when drinking fluids as being a specific problem. A number of participants complained about getting food trapped on the side affected by the palsy and 3 participants mentioned cheek and lip biting (or chewing).
Psychological Concerns
All participants described experiencing some degree of psychological impact following their diagnosis of facial palsy. Psychological concerns were varied and broadly divided into 4 overarching themes (Table 3).
Table 3.
Main Psychological Themes Described by Participants
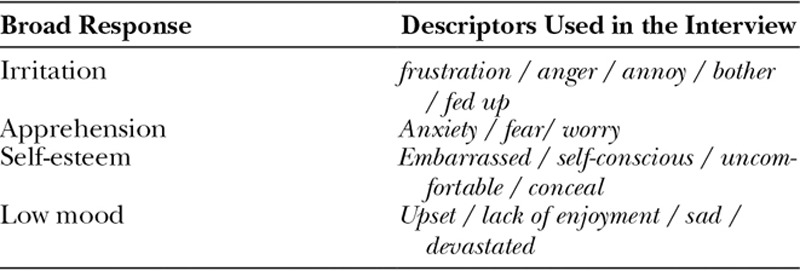
Participants were apprehensive about several aspects in relation to their diagnosis, the change in their appearance and facial function (eg, the appearance of their smile or their ability to eat in public), and concerns about what the future held for them. Participants experienced anxiety when people stared at them or made comments. Three participants worried that strangers may think they had had a stroke. Some form of concealment of the palsy was mentioned by most (10/14) participants who described using their hair (eg, a low fringe), a hand or sunglasses to hide certain aspects of the palsy, such as a difference in the position of their eyebrows. Other forms of concealment behavior included drinking (eg, with eye closed to reduce perceived synkinesis) or smiling (eg, using a limited smile to reduce facial asymmetry). Most participants reported that facial palsy had lowered their self-esteem, and that they felt self-conscious about facial appearance and/or functional disability. Commonly participants reported feeling very embarrassed when eating or drinking. Emotions such as feeling annoyed, bothered, or angry with regard to the changes in appearance were also common (6/14). Feeling sad, upset, or depressed about the change in appearance was frequently reported (5/14).
Social Concerns
A variety of social concerns were mentioned by participants that related to dating, driving, social support, interaction with people, work, and recreational activities. Most participants (13/14) reported avoiding or limiting recreational activities due to their facial palsy. In several cases, this specifically related to eating in public environments such as restaurants.
Social isolation was a common theme and accounted for over a quarter of social concerns. Eight participants described feelings of being isolated or alone, as a result of the palsy. Support from both friendship groups and family were mentioned by most participants and accounted for a quarter of codes within this theme. This took the form of appraisal support: “your smile is looking better,” emotional support: “my friends treat me the same” or instrumental support: “my husband took me to the hospital.” In all, 11 participants described that their condition had an impact on their employment. Specifically, 3 participants changed their job and 7 discussed needing prolonged time off work.
Appearance-related Concerns
The most common concerns about appearance related to overall facial appearance (n = 14), facial expression (n = 13), and the appearance of the eye (n = 10). How the face looked in different scenarios, such as in a mirror or photograph, were common concerns discussed by 12 participants. The most common adjectives used to describe the impact of facial palsy on appearance included “droops,” “looks different,’ down on one side.” After treatment, 8 participants specifically discussed the symmetry of their face for example: “My face had more symmetry after the plastic surgery.”
Many participants talked about the impact of facial palsy on their ability to show expression, including the ability to smile. Participants talked about not being able to smile: “I am not able to smile.” The second most common descriptor related to symmetry, for example: “I could only smile on my left side.” Participants also describe their smile as looking “awful,” “crooked,” “down,” and “uneven.”
In terms of the appearance of the eye, most comments described the eyelid position in terms of them “drooping,” “dropped,” and/or “down,” which accounted for 90% of comments and usually related to lower eyelid position. Participants also described the appearance of their eye using terms such as “drooping,” “bags,” “flickering,” “noticeable,” “closed,” “open,” and “freaky.”
Participant Experience of Healthcare
Over half of “experience of care” domain related to treatment of the FNP (eg, medication, surgery, botulinum toxin injections and facial therapy) as opposed to other aspects of healthcare. The next most common theme related to “information” including the process of receiving, seeking, or processing information. The information theme covered diagnosis, investigations, facial function issues, and/or treatments. Several participants felt that they lacked knowledge about their condition. Nine participants described seeking more information from various sources, including the medical staff, printed information such as leaflets and/or information derived from the internet. Comments were also made that the diagnosing medical team did not necessarily possess the knowledge themselves, nor did they always pass on medical information effectively. Participants often felt frustrated when treatments were not effective in reducing symptoms. Frustrations with the communication with their medical team were commonly reported.
DISCUSSION
Presented is the first qualitative study to formally develop a comprehensive framework of concerns (a conceptual framework) in patients with FNP following international guidance for the development of a PROM.10 This study increases our understanding of the impact of FNP on a patient’s HRQOL and provides the basis for the development of a new PROM. The semistructured interviews used generated an initial item pool of over 1,600 concerns from 14 patients with different causes of facial palsy. Key domains that emerged related to facial function and symptoms, facial appearance, psychological and social function, and experience of healthcare. These major themes are in keeping with similar studies exploring HR-QOL in this area. For example, Brooker et al.25 in a study exploring QOL in acoustic neuroma patient reported very similar themes including “physical symptoms,” “psychosocial wellbeing,” “social wellbeing,” “functional status,” and “psychosocial factors that influenced adjustment.” This model highlights the need for measures that include the patient’s perspective in outcome assessment rather than to simply assess facial palsy objectively in terms of appearance (eg, photos analysis) and facial movement (eg, speech).
A large number of outcome measures in FNP are in use internationally including clinician-based grading scales,26–31 generic PROMs,21,32,33 domain-specific PROMs,34 and global, FNP, multi-domain PROMs.18,19 In most cases, these measures are flawed in terms of developmental rigor. The literature would indicate that no single measure exists that is valid, comprehensive, and universally used.16 The heterogeneity of published outcomes erodes the quality of the evidence-base and affects decision-making both at clinical and commissioning levels, which may impact patient care.
Several concepts in this study have emerged that have not been included in current disease-specific FNP PROMs such as the FDI18 and the FaCE Scale.19 Our data suggest that patients with facial palsy will often experience visual disturbance and synkinesis both of which are not included in current multi-domain disease-specific measures. Speech was another key concern for patients including difficulty with pronunciation, slurring, and reduced understanding by others which is not fully covered with current measures.
Facial palsy is known to detrimentally affect psychosocial well-being, indicating that this patient group would benefit from assessment of psychological impact during their care. A number of current outcome measures fail to assess self-perception of appearance. We observed that patients were particularly critical of their own appearance, which affected their psychological state. Symmetry and facial expression were important issues for patients and are intrinsic to psychological well-being. Many participants reported feeling irritation, anxiety, lower self-esteem, and low mood. Although the psychological impact of FNP is reported in the published literature,6,35 this concept is not specifically measured by commonly used instruments such as the FDI18 or FaCE scales.19 It is recognized that the degree of facial asymmetry or physical difference perceived by a patient does not correlate with the level of distress felt36 and so many patients may not receive the level of psychological support needed. Our sample described a range of tactics used to conceal their palsy, for example, with a hand, eye patch or fringe. To our knowledge, this theme has only been included in a synkinesis-specific QoL instrument34 and has not been included in general, muglolti-domain, FNP PROMs.
Healthcare experience in this study was a real priority for participants and has been observed in similar studies.22 The need for scales measuring experience of care is not disputed and such measures are essential to deliver feedback to service provision. Such information can assist healthcare providers to the understand areas of need and how to improve practice.37 However, the inclusion of experience measures within a PROM has not always been accepted practice and has historically been debated. There are an increasing number of plastic surgery–specific PROMs that adopt the modular approach and include a range of independently functioning scales to measure outcomes as well as experiences of care. The BREAST-Q, for example, includes experience scales to measure satisfaction with information, the surgeon, medical team, and office staff.38 The advantage of using such experience scales is that their content was designed from the same patient population as the outcome scales,39–41 a factor that may influence future PROMS related to FNP.
Some limitations are present in this study that should be acknowledged. This study sought the opinions of those specialists who worked within the FNP multidisciplinary clinic when designing the interview guide. Similar studies have sought the opinion of a wider range of experts (eg, a psychologist or ear, nose and throat [ENT] specialist) who could have potentially generated more relevant interview questions.23 There were no patients in the interview cohort who had developed a facial palsy within the previous 3 months. It would have been interesting to explore the issues of patients in “real time” rather than with retrospective discussion. The U.S. Food and Drug Administration (FDA) advised that content validity may be reduced when asking patients to recall concerns and experiences that can undermine the PROM.10 More females (n = 9) attended the interview than males (n = 5) due to difficulties in recruitment. Several other studies relating to QoL assessment report lower attendance in males in keeping with this study and recognize that men are more difficult to recruit to studies than women.42 Analysis was performed comparing female and male themes. Overall, there were few major differences between men and women for issues in each of the major domains. Males and females for the most part commented on similar issues relating to experience of care as well as physical, psychological, social, and appearance-related concerns.
CONCLUSIONS
Presented is an in-depth account of patient perception when experiencing facial palsy; it conforms to stringent, validated, international development criteria. The data in this study confirm that facial palsy has a significant and detrimental impact on well-being. The conceptual model highlights a number of key themes relevant to this patient group including concepts relating to physical function, psychosocial well-being, perception of appearance, and experience of healthcare. These themes also emerge in the medical literature, reinforcing that facial palsy has a substantial impact on all aspects of QOL. Analysis of current patient-reported outcome instruments in FNP, in the context of the findings from this study, confirms some aspects of patient experience are not currently being captured including psychological distress, eye-related concerns, and synkinesis. This diminishes the validity of the respective outcome measures in use currently.
ACKNOWLEDGMENT
The authors acknowledge the work of Laura Stacey who assisted with the administration of this study.
Footnotes
Published online 9 January 2019.
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Rowlands S, Hooper R, Hughes R, et al. The epidemiology and treatment of Bell’s palsy in the UK. Eur J Neurol. 2002;9:63–67. [DOI] [PubMed] [Google Scholar]
- 2.Benecke JE., Jr. Facial paralysis. Otolaryngol Clin North Am. 2002;35:357–365. [DOI] [PubMed] [Google Scholar]
- 3.Shindo M. Management of facial nerve paralysis. Otolaryngol Clin North Am. 1999;32:945–964. [DOI] [PubMed] [Google Scholar]
- 4.Schrom T, Buchal A, Ganswindt S, et al. Patient satisfaction after lid loading in facial palsy. Eur Arch Otorhinolaryngol. 2009;266:1727–1731. [DOI] [PubMed] [Google Scholar]
- 5.Ciuman RR, Oels W, Jaussi R, et al. Outcome, general, and symptom-specific quality of life after various types of parotid resection. Laryngoscope. 2012;122:1254–1261. [DOI] [PubMed] [Google Scholar]
- 6.VanSwearingen JM, Cohn JF, Turnbull J, et al. Psychological distress: linking impairment with disability in facial neuromotor disorders. Otolaryngol Head Neck Surg. 1998;118:790–796. [DOI] [PubMed] [Google Scholar]
- 7.Nightingale F. Some Notes on Hospitals. 18633rd ed London, United Kingdom: Longmans, Green and Co. [Google Scholar]
- 8.Cano SJ, Klassen A, Pusic AL. The science behind quality-of-life measurement: a primer for plastic surgeons. Plast Reconstr Surg. 2009;123:98e–106e. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization. Basic Documents. 48th ed. [online]. 2014. Available at http://apps.who.int/gb/bd/PDF/bd48/basic-documents-48th-edition-en.pdf#page=7. Accessed August 31, 2016.
- 10.US Food and Drug Administration, Center for Drug Evaluation and Research, Center for Biologics Evaluation and Research, Center for Devices and Radiological Health. Guidance for industry patient-reported outcome measures: use in medical product development to support labeling claims. [online]. 2009. Available at http://www.fda.gov/downloads/Drugs/.../Guidances/UCM193282.pdf. Accessed February 1, 2016.
- 11.Department of Health. Guidance on the routine collection of patient reported outcome measures (PROMs). [online]. 2009. Available at http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_092625.pdf. Accessed May 4, 2016.
- 12.Baumhauer JF, Bozic KJ. Value-based healthcare: PROs in clinical decision-making. Clin Orthop Relat Res. 2016;474:1375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nelson EC, Eftimovska E, Lind C, et al. Patient reported outcome measures in practice. BMJ. 2015;350:g7818. [DOI] [PubMed] [Google Scholar]
- 14.Scientific Advisory Committee of the Medical Trust. Assessing health status and quality-of-life instruments: attributes and review criteria. Qual Life Res 2002;11:193–205. [DOI] [PubMed] [Google Scholar]
- 15.Wu AW, Kharrazi H, Boulware LE, et al. Measure once, cut twice—adding PROs to the electronic health record for comparative effectiveness research. J Clin Epidemiol. 2013;203;66:S12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ho AL, Scott AM, Klassen AF, et al. Measuring quality of life and patient satisfaction in facial paralysis patients: a systematic review of patient-reported outcome measures. Plast Reconstr Surg. 2012;130:91–99. [DOI] [PubMed] [Google Scholar]
- 17.Fattah AY, Gavilan J, Hadlock TA, et al. Survey of methods of facial palsy documentation in use by members of the Sir Charles Bell Society. Laryngoscope. 2014;124:2247–2251. [DOI] [PubMed] [Google Scholar]
- 18.VanSwearingen JM, Brach JS. The facial disability index: reliability and validity of a disability assessment instrument for disorders of the facial neuromuscular system. Phys Ther. 1996;76:1288–1298; discussion 1298. [DOI] [PubMed] [Google Scholar]
- 19.Kahn JB, Gliklich RE, Boyev KP, et al. Validation of a patient-graded instrument for facial nerve paralysis: the FaCE scale. Laryngoscope. 2001;111:387–398. [DOI] [PubMed] [Google Scholar]
- 20.Ware JE, Snow KK, Kosinski M, et al. SF-36 Health Survey Manual and Interpretation Guide. 1993Boston, Mass.: New England Medical Center, The Health Institute. [Google Scholar]
- 21.Robinson K, Gatehouse S, Browning GG. Measuring patient benefit from otorhinolaryngological surgery and therapy. Ann Otol Rhinol Laryngol. 1996;105:415–422. [DOI] [PubMed] [Google Scholar]
- 22.Lee EH, Klassen AF, Lawson JL, et al. Patient experiences and outcomes following facial skin cancer surgery: a qualitative study. Australas J Dermatol. 2016;57:e100–e104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Klassen AF, Cano SJ, Scott A, et al. Measuring patient-reported outcomes in facial aesthetic patients: development of the FACE-Q. Facial Plast Surg. 2010;26:303–309. [DOI] [PubMed] [Google Scholar]
- 24.Thorne SE. Interpretive Description. Developing Qualitative Inquiry. 2008Walnut Creek, Calif.: Left Coast Press. [Google Scholar]
- 25.Brooker J, Burney S, Fletcher J, et al. A qualitative exploration of quality of life among individuals diagnosed with an acoustic neuroma. Br J Health Psychol. 2009;14:563–578. [DOI] [PubMed] [Google Scholar]
- 26.Alicandri-Ciufelli M, Piccinini A, Grammatica A, et al. A step backward: the ‘Rough’ facial nerve grading system. J Craniomaxillofac Surg. 2013;41:e175–e179. [DOI] [PubMed] [Google Scholar]
- 27.Banks CA, Jowett N, Hadlock CR, et al. Weighting of facial grading variables to disfigurement in facial palsy. JAMA Facial Plast Surg. 2016;18:292–298. [DOI] [PubMed] [Google Scholar]
- 28.House JW, Brackmann DE. Facial nerve grading system. Otolaryngol Head Neck Surg. 1985;93:146–147. [DOI] [PubMed] [Google Scholar]
- 29.Katsumi S, Esaki S, Hattori K, et al. Quantitative analysis of facial palsy using a three-dimensional facial motion measurement system. Auris Nasus Larynx. 2015;42:275–283. [DOI] [PubMed] [Google Scholar]
- 30.Kecskés G, Jóri J, O’Reilly BF, et al. Clinical assessment of a new computerised objective method of measuring facial palsy. Clin Otolaryngol. 2011;36:313–319. [DOI] [PubMed] [Google Scholar]
- 31.Lee LN, Susarla SM, H Hohman M, et al. A comparison of facial nerve grading systems. Ann Plast Surg. 2013;70:313–316. [DOI] [PubMed] [Google Scholar]
- 32.Lassaletta L, Alfonso C, Del Rio L, et al. Impact of facial dysfunction on quality of life after vestibular schwannoma surgery. Ann Otol Rhinol Laryngol. 2006;115:694–698. [DOI] [PubMed] [Google Scholar]
- 33.Nicoucar K, Momjian S, Vader JP, et al. Surgery for large vestibular schwannomas: how patients and surgeons perceive quality of life. J Neurosurg. 2006;105:205–212. [DOI] [PubMed] [Google Scholar]
- 34.Borodic G, Bartley M, Slattery W, et al. Botulinum toxin for aberrant facial nerve regeneration: double-blind, placebo-controlled trial using subjective endpoints. Plast Reconstr Surg. 2005;116:36–43. [DOI] [PubMed] [Google Scholar]
- 35.Walker DT, Hallam MJ, Ni Mhurchadha S, et al. The psychosocial impact of facial palsy: our experience in one hundred and twenty six patients. Clin Otolaryngol. 2012;37:474–477. [DOI] [PubMed] [Google Scholar]
- 36.Lansdown R, Rumsey N, Bradbury E, et al. Visibly Different: Coping with Disfigurement. 1997Oxford, United Kingdom: Butterworth-Heinemann. [Google Scholar]
- 37.Department of Health. Transparency in outcomes—a framework for the NHS. [online]. 2010. Available at http://webarchive.nationalarchives.gov.uk/+/www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_122952.pdf. Accessed May 4, 2016.
- 38.Pusic AL, Klassen AF, Scott AM, et al. Development of a new patient-reported outcome measure for breast surgery: the BREAST-Q. Plast Reconstr Surg. 2009;124:345–353. [DOI] [PubMed] [Google Scholar]
- 39.Klassen AF, Cano SJ, Alderman A, et al. The BODY-Q: a patient-reported outcome instrument for weight loss and body contouring treatments. Plast Reconstr Surg Glob Open. 2016;4:e679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Luo Y, Yang J, Zhang Y. Development and validation of a patient-reported outcome measure for stroke patients. Health Qual Life Outcomes. 2015;13:53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Klassen AF, Cano SJ, Schwitzer JA, et al. FACE-Q scales for health-related quality of life, early life impact, satisfaction with outcomes, and decision to have treatment: development and validation. Plast Reconstr Surg. 2015;135:375–386. [DOI] [PubMed] [Google Scholar]
- 42.Oliffe J, Thorne S. Men, masculinities, and prostate cancer: Australian and Canadian patient perspectives of communication with male physicians. Qual Health Res. 2007;17:149–161. [DOI] [PubMed] [Google Scholar]


