Summary:
Autologous fat injection is becoming a more and more widely accepted procedure in plastic surgery nowadays. Concomitantly, there are many complications. The most serious one is arterial fat embolism, for which there is only poor prognosis and no effective treatment. Here, we report the first case of successful treatment of cerebral fat embolization with the help of mechanical lipectomy. Our patient was found unconscious with left-sided hemiparesis after a facial fat injection surgery 4 hours before. Cerebral artery computed tomography angiography indicated it was multiple fat embolism. Then Solitaire stent (4 × 20 mm) and Solumbra (continuously negative pressure attraction) were utilized for the mechanical extraction of fat emboli. The patient recovered from left-side hemiparesis to muscle strength of Medical Research Council scale grade 4, and National Institutes of Health Stroke Scale score was 0 after 3 months visit. In the cerebral infarction after fat transplantation, mechanical lipectomy can be a novel and significant treatment.
Autologous fat transplantation is a process aimed at eliminating depression regions in skin by subcutaneous injection of the patient’s own fatty tissue.1 In previous studies, complications like blindness, septicemia, infection, local necrosis, and hemiplegia did occur.2–4 Among them, fat embolism of the middle cerebral artery is rare but the most devastating. The results of trials for treating fat-induced cerebral infarction with hormone therapy, craniotomy decompression, drug thrombolysis and so on are not satisfactory at all.5,6 Herein the first successfully treated case that experienced unilateral cerebral infarction of fat embolism with enough auxiliary examinations is reported. The good treatment outcome is satisfactory after our timely intravascular intervention in this condition.
CASE
A 22-year-old Chinese woman came to the Emergency Department in our hospital with a sudden onset of unconsciousness and left-sided hemiparesis after a cosmetic surgery 4 hours before. Bilateral liposuction of the thighs and autologous fat injection into the temporal territory under local anesthesia were conducted on the patient. According to the operative note, a blunt cannula measuring 2.5 mm in diameter had been attached to a 10-ml syringe previously washed with sterile saline, and fat was injected into each temporal (25 ml each) region. Cerebrovascular risk factors or recent trauma were denied.
On arrival, her neurological examination revealed as follows: both pupils were fixed to the right side but were reactive to light, and her left lateral limbs showed Medical Research Council scale (MRC) grade 0, while right limbs showed MRC grade 5. Besides, Babinski sign of the left side was positive and her total National Institutes of Health Stroke Scale (NIHSS) score was 18.
As soon as the result of the patient’s computed tomography angiography came out: multiple fat embolisms in right internal carotid artery and middle cerebral artery with basal ganglia ischemia (Fig. 1); she was transferred to our tertiary stroke center for endovascular treatment. The operation time was 6 hours and 45 minutes after the symptom occurred.
Fig. 1.
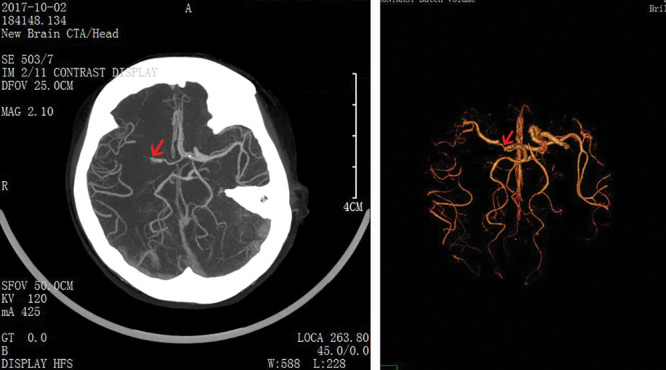
Magnetic resonance angiography showed occlusion of the right internal carotid artery and middle cerebral artery.
First, induced general anesthesia with midazolam (3 mg) and fentanyl (0.1 mg) was applied to the patent. Then an 8F catheter sheath was placed after puncturing the patient’s right femoral artery by using Seldinger’s method. The head of the guide tube was placed at the end of the right carotid artery under the guidance of the guide wire. Next, with the combination of micro-guide wire and Rebar 18 catheter/6F Navien catheter, the middle catheter tip was put to C1, and extended to proximal M2. Later, the size of Solitaire stent (4 × 20 mm) was matched and deployed for 3 minutes to allow full expansion. Afterward, Solumbra technology (Solumbra technology refers to the mechanical thrombectomy combined with thrombus aspiration technique, using guide catheter at the proximal artery, and microcatheter at the distal end with the aid of the microwire and the intermediate catheter, and finally opening the stent after confirming the position by angiography) was used for continuous negative pressure suction with 60 ml syringe. Under negative pressure suction of 6F intermediate catheter, partial fat embolus was aspirated. After that, angiography demonstrated that M1/M2 segments of the right internal carotid were still not developed. Later, the microcatheter was sent to distal M2, and the same method was applied again. Finally, arteries recovered unobstructed with thrombolysis in cerebral infarction grade 3, as shown by the subsequent angiography (Fig. 2).
Fig. 2.
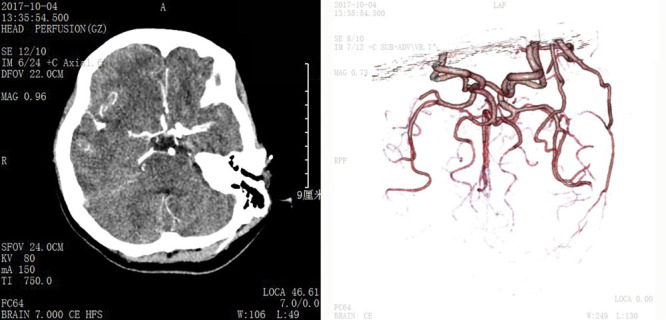
Posttreatment computed tomography scan images demonstrated the patency of the previously obstructed arteries.
The patient’s NIHSS score ranked 17 just 2 hours after the lipectomy operation. Furthermore, at the 3-month follow-up visit, the patient was able to walk without assistance. The left limb was MRC grade 4 and the NIHSS score turned to 0.
DISCUSSION
At present, with the increase in the amount of autologous fat transplantation surgery, complications after such surgery have increased as well. Previous literature suggests that most of the complication following autologous fat transplantation is local skin deformation.7 Another study investigating complications of 1,000 patients after autologous fat transplantation shows that local deformity accounts for 83 cases (8.3%), and infection 4 cases (0.4%). There are also 2 cases of hematoma (0.2%) in the donor site, and meanwhile the implant ruptured (0.1%) in 1 month after the transplantation of fat, though ophthalmic artery and cerebral artery embolism did not happen.2 This indicated that the incidence rate of arterial embolism was extremely low. A review of the recent English-language literature revealed 98 cases of vision change due to filler injections, 47 of which were due to autologous fat injection, and only 1 patient got sensorimotor hemiparesis after infarction of the middle cerebral artery.8
However, since carotid artery has its ophthalmic and facial branches such as superficial temporal artery, and fat particles are composed of various sizes, they may block both large and small arteries. For example, there are some sporadic cases of ocular artery and cerebral arterial embolism. Of course, the size of the injection cannula could be a risk factor of fat embolism since it decides the size of fat particles injecting into artery.
Our case is the first treatment about quickly vascular recanalization via mechanical lipectomy devices on the cerebral infarction patient caused by fat transplantation surgery. As muscle strength of the patient in our case has been restoring gradually, we believe that recovering to normal MRC grade is quite hopeful with subsequent functional exercise.
When it comes to the exact span of appropriate intervention for better prognosis, it still remains unknown. As far as our case is concerned, the patient had the intravascular operation after 6 hours and 45 minutes of her symptoms. We could observe from the above imaging data that hemorrhagic transformation in the right-side cerebral area occurred, and this might suggest intervention to save the brain cells was still not early enough.
CONCLUSIONS
What can be learned from our case is that cerebral artery occlusion of fat granule can be removed successfully by mechanical lipectomy, which might be of great value to cosmetic surgeons. However, as this patient doesn’t have sight problem, we’ve no idea about safe and reliable treatment for reversal of iatrogenic ophthalmic artery occlusion. Thus, we are expecting additional studies and data, which might be a breakthrough for obtaining better clinical outcomes.
Footnotes
Published online 7 January 2019.
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Gir P, Brown SA, Oni G, et al. Fat grafting: evidence-based review on autologous fat harvesting, processing, reinjection, and storage. Plast Reconstr Surg. 2012;130:249–258. [DOI] [PubMed] [Google Scholar]
- 2.Maione L, Vinci V, Klinger M, et al. Autologous fat graft by needle: analysis of complications after 1000 patients. Ann Plast Surg. 2015;74:277–280. [DOI] [PubMed] [Google Scholar]
- 3.Yu NZ, Huang JZ, Zhang H, et al. A systemic review of autologous fat grafting survival rate and related severe complications. Chin Med J (Engl). 2015;128:1245–1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roshandel D, Soheilian M, Pakravan M, et al. Middle cerebral artery, ophthalmic artery, and multibranch retinal vessel occlusion after cosmetic autologous fat transfer to forehead. Ophthalmic Surg Lasers Imaging Retina. 2015;46:593–596. [DOI] [PubMed] [Google Scholar]
- 5.Lee CM, Hong IH, Park SP. Ophthalmic artery obstruction and cerebral infarction following periocular injection of autologous fat. Korean J Ophthalmol. 2011;25:358–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yoon SS, Chang DI, Chung KC. Acute fatal stroke immediately following autologous fat injection into the face. Neurology. 2003;61:1151–1152. [DOI] [PubMed] [Google Scholar]
- 7.Pereira LH, Nicaretta B, Sterodimas A. Correction of liposuction sequelae by autologous fat transplantation. Aesthetic Plast Surg. 2011;35:1000–1008. [DOI] [PubMed] [Google Scholar]
- 8.Haneke E. Managing complications of fillers: rare and not-so-rare. J Cutan Aesthet Surg. 2015;8:198–210. [DOI] [PMC free article] [PubMed] [Google Scholar]


