Abstract
Background
Since 2011, hundreds of thousands of Syrians have been displaced and injured due to the ongoing Syrian civil war. In this study, we report the prevalence of neurologic injuries in a major rehabilitation center on the Turkish–Syrian border where death and injury tolls continue to rise.
Method
Based on several on-site visits from 2013 to 2016, medical practitioners collected data from patients in the major rehabilitation center on the border of Turkey and Syria. The clinical data, which included the type and cause of injury, laterality, paralysis, areas injured, and treatment offered, were analyzed.
Results
A total of 230 patients were identified as having sustained a neurologic injury, 221/230 (96.1%) male and 9/230 (3.91%) female, ranging from ages 2–52 years. A total of 305 total injuries were documented over the course of a 4-year analysis due to several patients having multiple injuries. Gunshot wounds were the dominant mechanism of injury in 125/230 (54.3%) patients. Patients more frequently sustained single injuries 152/230 (66.1%) than multiple injuries 78/230 (33.9%). Peripheral nerve injuries were the most prevalent injuries, at 92.5% of all neurologic injuries (282/305), specifically injury to the radial nerve, at 19.1% (54/282) of peripheral injuries. Patients with spinal cord injuries made up 20/230 (8.7%) of all patients, with thoracic spine injuries composing 50% (10/20). Traumatic brain injuries were the least prevalent, 3/230 (1.3%), with an equal distribution of subtypes.
Conclusion
This study and critical analysis of the devastation in Syria suggests the desperate need for emergency aid.
The Syrian war, which started in 2011, represents one of the most devastating crises of the 21st century,1,2 resulting in over 470,000 deaths as of February 20161 and displacement of 12.2 million Syrians (5.6 million refugees, 6.6 million internally displaced people).3 Widespread attacks on health facilities have been documented1,2 and there are few facilities capable of providing rehabilitative services.
In order to provide rehabilitative services to the large number of patients injured in the war, our medical relief team, led by Union of Medical Care and Relief Organizations, with support from other Syrian expatriate relief agencies, solicited responses by offering expertise and time in clinical camps on the Syrian–Turkish border. Due to the siege and constant attacks on the Syrian side of the border, the rehabilitation facility was established in the Turkish border town of Reyhanli. This article presents a retrospective analysis of neurotrauma cases documented through serial medical missions to this facility.
Method
From 2013 to 2016, a team of 2 neurologists and 1 physiotherapist conducted 5 medical missions to the Reyhanli facility, treating a total of 2,500 patients over a course of five 5-day visits. Patients at the facility sustained injuries inside Syria and were referred to the rehabilitation center from hospitals inside Syria and transported via personal transportation or by ambulance, taking anywhere between a few hours to a week to reach the rehabilitation facilities. Patients remained in the facility for at least 2 months after treatment for socioeconomic reasons. The rehabilitation facility provided diagnostic imaging including plain radiographs and EMG, and utilized CT scanning from surrounding facilities. Patients requiring additional clinical services were referred to nearby Turkish hospitals for continued definitive care.
The aim of the study was to estimate the prevalence of neurologic injuries in the largest facility providing rehabilitation services to Syrian war injured. Detailed clinical notes were maintained by the study team. Clinical and demographic data of each patient were collected by the medical team. Demographic data included sex and age. Clinical data included type of injury, mechanism of injury, laterality, paralysis, areas injured, and treatment offered. This data was handwritten on neurologic examination papers and subsequently deidentified by the clinical team prior to analysis. Retrospective analysis of neurotrauma cases was conducted and descriptive statistics were calculated. Ethical review was conducted by the Ethical Research Committee of Yale University.
Standard protocol approvals, registrations, and patient consents
Ethics approval was obtained from Yale University. Verbal consent was collected from all patients (or guardians of patients) included in this study.
Data availability
Data available upon request.
Results
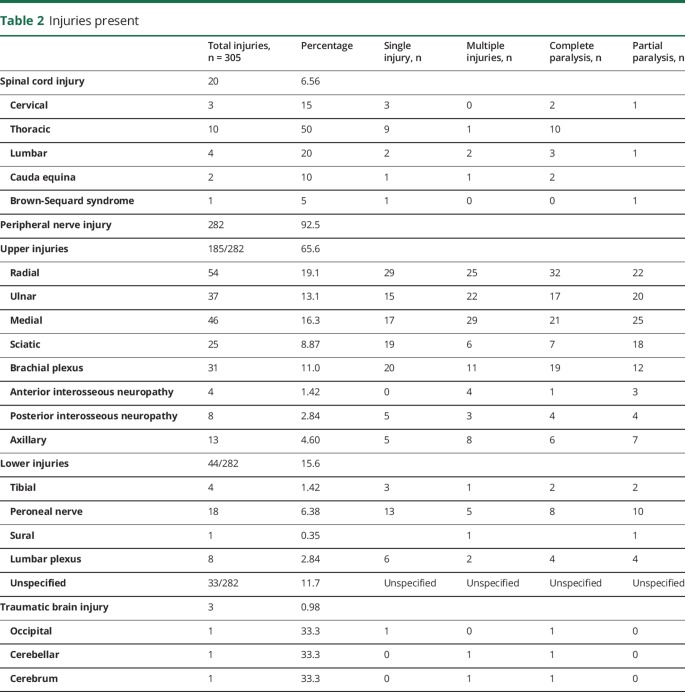
A total of 230 patients with neurologic injuries, treated from 2013 to 2016, were included in the analysis. Neurotrauma patients were predominately male (221 adult men, 19–40 years; 9 women, 27–47 years; and 5 pediatric cases, 2–18 years) with a mean age of 25.45 years. The youngest patient was a 2-year-old boy and the oldest a 52-year-old man (table 1).
Table 1.
Baseline characteristics of 230 patients
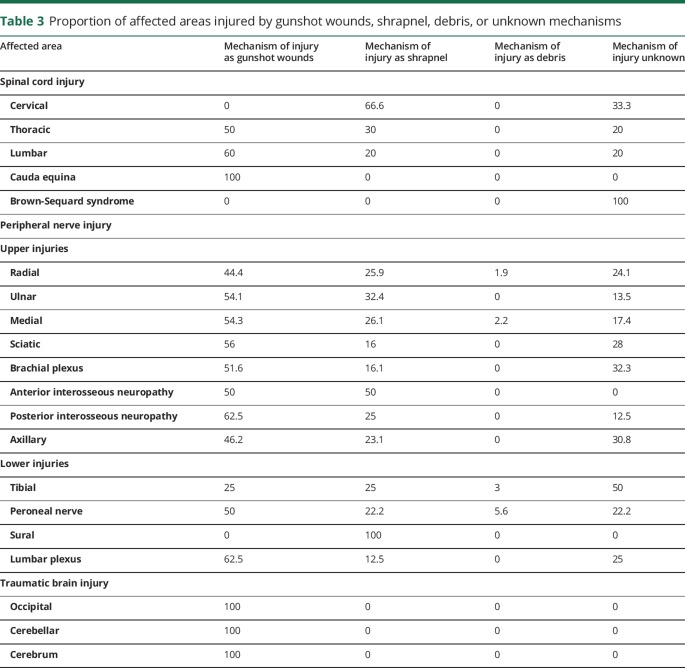
There were a total of 305 neurologic injuries with approximately 1/3 of patients sustaining more than one neurotrauma (table 2). The mechanisms of injury were consistent with those sustained in a war zone, with gunshot wounds (53.9%), shrapnel wounds (22.2%), debris (1.30%), or an unknown source (23.5%). The majority of patients at the rehabilitation facility sustained peripheral neurotrauma (282 peripheral nerve injuries [PNI] [92.5%], 20 spinal cord injuries [SCI] [6.56%], and 3 traumatic brain injuries [TBI] [0.98%]).
Table 2.
Injuries present
Peripheral nerve injuries
There were 282 PNI, many associated with non-neurologic injuries. PNI diagnosis was based upon clinical examinations and EMG findings (table 2). The majority, 137 (48.6%), were localized to the forearm (radial nerve injury, 54 [19.1%]; median nerve injury, 46 [16.3%]; and ulnar nerve injury, 37 [13.1%]). The most prevalent lower extremity PNI was to the common peroneal nerve. However, this injury pattern was seen far less frequently, comprising 18 of the 282 injuries (6.38%). Brachial plexus injuries comprised 23 (8.16%). Two out of 23 cases of brachial plexus injuries were upper trunk injuries, 2 cases were lower trunk injuries, and 4 out of 23 cases were suprascapular injuries. Thirty-three (11.7%) PNI were unspecified in diagnosis as well as region of injury and were therefore labeled unspecified PNI.
Most of the PNI were sustained in the context of multiple associated neurologic and non-neurologic injuries and resulted in complete functional loss of motor activity associated with the injured nerve (table 2).
Spinal cord injuries
Due to the given location and social climate of the hospital, American Spinal Injury Association status of the SCI was unable to be documented (table 2). There was a total of 20 SCI cases, making up 6.56% of total injuries (3 cervical, 10 thoracic, 4 lumbar, 2 cauda equine, and 1 Brown-Sequard). Three out of 20 (15%) were injuries to the cervical spinal cord. The most predominant SCI location was in the thoracic spine, making up 50% of SCIs sustained, particularly at the T7–T12 level. Four out of 20 injuries (20%) were lumbar SCI; 2 out of 20 (10%) cases were cauda equina; and 1 (5%) was Brown-Sequard syndrome. Seventeen of 20 (85%) SCIs resulted in complete paralysis and 3 (15%) resulted in partial paralysis. All SCI cases underwent surgical intervention except one case, based on the clinical judgment of the attending physician.
Traumatic brain injuries
Only 3 cases of TBI (0.98%) were recorded—1 occipital fracture, 1 skull base fracture, and 1 cerebellar injury (table 2). The injuries were diagnosed based on clinical assessment and confirmed via CT scan. Surgical intervention was performed for the occipital and skull base injuries, but was deemed clinically inappropriate for the cerebellar injury. Of the 3 TBIs, only the occipital TBI was sustained as an isolated injury.
Discussion
The Syrian war has resulted in widespread morbidity from war trauma. Neurotrauma patients surviving to referral for rehabilitation services were predominately male with PNI. This finding is consistent with the disproportionate role of males injured in Syrian war trauma overall.4 This is likely due to men being more actively involved in the warfare, protests, and resistance, and therefore more vulnerable to injury. Furthermore, it is possible that women and children are geographically removed from the most intense combat areas and thus sustained fewer injuries. Conversely, as they are not directly involved in active combat, they are more likely to sustain mortal injuries due to lack of protective armor when combat does encroach on their respective domestic and educational domains. It was not possible to differentiate these patients into military personnel and civilian groups due to the large influx and quick turnover in the facility.
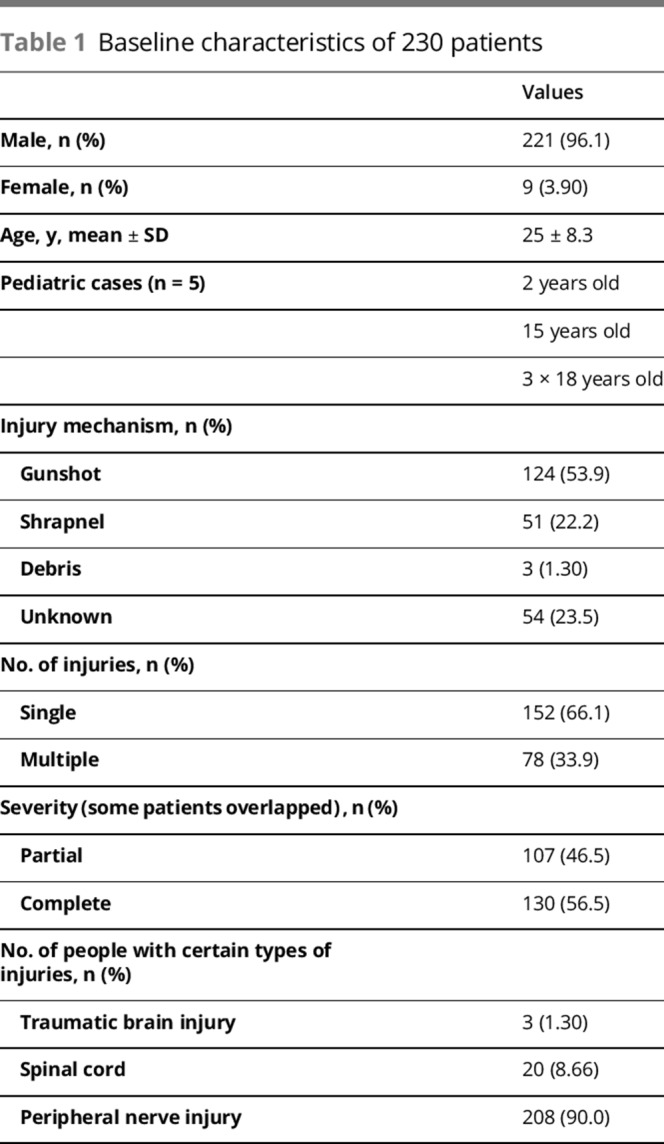
The weaponry used in the Syria war are typically high-velocity, penetrating projectiles (bullets, missiles, shrapnel) with an explosive component, as well as barrel bombs, which result in building collapse and crush injuries. The result is that the majority of patients in our study sustained complete transection injuries. Furthermore, radial and median nerve injuries were the most common (table 2). This may also be due to the mechanism of injury, as most injuries are due to blunt impact from shrapnel and gunshot wounds (table 3). This is likely exacerbated by the insufficient protective gear and nonspecific firing of weaponry that is rampant in the Syrian war zone.
Table 3.
Proportion of affected areas injured by gunshot wounds, shrapnel, debris, or unknown mechanisms
Our findings differed from findings from previous military studies (no previous studies have been documented in civilian populations). Birch et al.5 investigated the epidemiology and outcomes of PNI in service men and women injured in Iraq and Afghanistan. This group observed that the PNI were distributed as follows: 45% of cases were neurapraxia, 35% were axonotmesis, 20% were neurotmesis.5 The PNI in military personnel were evenly distributed between the upper and the lower limbs.5 Explosions accounted for 63% of PNI.5 This contrasts the results we observed in the injured population in Syria, where 65.4% of the PNI were in the upper extremity, and the majority (53.9%) of injuries were gunshot wounds. A similar study done in Vietnam documented the prevalence of neurologic injuries of civilians and military personnel during the Vietnam War.6 It was found that approximately 21% of the nerve-injured patients had injuries due to gunshot wounds; this was notably less than our findings. In contrast to Birch et al. who solely studied injuries in military personnel, Daroff6 found that upper extremity nerve injuries were more frequent than spinal injuries, which parallels our results. Birch et al.5 also detailed the outcomes of the PNI over a mean follow-up of 27.4 months. Since Syria is a combat zone with limited resources, we were unable to follow our patient population over time once they left the rehabilitation center.
SCI were the next most prevalent neurologic injury type. The clear majority of SCIs occurred in the thoracic spine region via gunshot wounds and shrapnel (tables 2 and 3). These patients with thoracic SCI resulted in total paralysis despite spinal surgery. The poor outcomes of SCI may be explained by the mechanism of injury and prehospitalization factors, which include lack of formal prehospital emergency care, prolonged transport times, and insufficient specialty care at initial receiving hospitals.
Proper prehospital care in a combat zone is complex. Prehospital efforts in Syria were often ad hoc by providers who lack formal training. Lack of proper equipment to extract patients from collapsed structures and nonadherence to spinal immobilization may have resulted in worse SCI prior to presentation to treatment facilities.
Moreover, hospitals providing injury care in Syria during the war rarely had spinal surgical specialists available.7 Even when surgical interventions were possible, a survey of hospital facilities in Syria revealed that only 16% of hospitals have the capacity to care for patients after surgery due to limited health care personnel and inpatient capacity.8 The hostile environment in which these hospitals are located is demonstrated by the fact that 26% of facilities rely on smuggling routes to refer patients to other hospitals and 50% of hospitals report domestic supply lines that were never open or open a few hours a day.8
Furthermore, the weaponry used in the Syrian conflict likely affected the type and extent of SCI. High-velocity projectiles and improvised explosive devices (IED), most specifically barrel bombs—oil drums packed with explosives, fuel, and shrapnel—were commonly used in the Syrian war. IEDs have a characteristic injury pattern in that they are typically localized to the thoracic and lumbar spine and classically burst fractures.9 In the Iraq War, it was estimated that IEDs produced approximately 75%–80% of all military personnel combat casualties.10 In Iraq, thoracolumbar injury classification and severity score was substantially higher in combat burst fractures than all other mechanisms of injury.9
The least common neurologic injury documented at our facility was TBI. The small number of patients presenting to the center with TBIs is most likely secondary to the severity of the brain injuries sustained during conflict, resulting in poor overall survival rates. Furthermore, the ambulance system was not well-developed during the period studied, resulting in delayed transport for definitive treatment, another potential reason why only a very small number of TBIs were observed in the context of this study.
Given the devastating nature of these injuries sustained in the context of penetrating war trauma, it is likely that our sample from the rehabilitation facility is not representative of Syrian war neurotrauma patients generally as the majority of such cases were unlikely to survive their initial management and transfer to rehabilitation.
While this study represents only a sampling of the neurotrauma cases at the high-volume rehabilitation center at Reyhanli, the methodology used was similar to other recent published studies, including an analysis of neurologic disease in Operation Iraqi Freedom to document injury and illness of military troops.11 However, in that study, the conditions documented more closely resembled those documented by Daroff6 in a study of Vietnam War neurotrauma (headaches, seizures, and psychiatric disorders) more than the weapon-inflicted injuries of our studies. It is difficult to directly compare our data to those presented in those articles as those focused on military personnel with protective armor and military prehospital transport, whereas our patient sample represents a diverse population of civilians and informal combatants without protective gear.
Limitations
A major limitation of this study is that of survival bias, where the cases analyzed represent only those who survived their initial injuries and survived their initial treatments at field hospitals and transport to the Reyhanli rehabilitation facility. Furthermore, the patients included in this study were only those treated during a short visitation period of 5 days. It is likely that only patients with less life-threatening injuries survive to be evaluated at our rehabilitation center. If the study included hospitals of initial presentation, the distribution of injuries would likely have described a higher percentage of patients with CNS trauma. The patient population mostly came from Central and Northern Syria and likely disproportionately represented patients with easier access to the border crossing, further limiting generalizability since neurotrauma patients from more distant or isolated regions within Syria may not have been able to access the facility.
In addition, the high rate of presentation and lack of communications limited the ability to document factors such as transport times from receiving hospitals and hampered efforts to follow up patients after their discharge from the rehabilitation center.
We focused on traumatic central and PNI only and did not collect data characterizing mild TBI and concussions or neuropsychiatric illnesses due to mechanisms such as IED blasts. However, some of these conditions have been previously reported in the Syrian context by Al-Nuaimi et al.4 as well as in other war zones, as presented in studies by Daroff6 and Hartmann.11 Despite being located on the fringe of the conflict zone, the facility studied has a severe lack of human and medical resources. Thus, the exact evacuation patterns of the patients were not documented, as the limited resources are devoted to clinical treatment. Characterization of central and PNI in Syria is the first step in facilitating the ability to formulate more effective interventions in hospital and prehospital settings.
Our small sample from the rehabilitation center likely underrepresents the overall breadth of neurologic injuries in the Syrian war but represents an important estimate of the unmet need for neurotrauma care for injured Syrians. The rehabilitation center treated patients without surveying whether they were civilians or military personnel. Although this may have added merit to the study, it was not possible to differentiate as the clinic is nonspecific and in accordance with a neutral medical mandate treats whoever is brought in for rehabilitation. These limitations attenuate the generalizability of the study. However, the value of this study should not be underestimated as it presents a valuable portrait of what is occurring in present-day Syria.
As of the writing of this manuscript, conflict continues in Syria. The results of this study call for several important interventions including the training of prehospital personnel in the proper extraction and immobilization of neurotrauma patients. We further suggest that organizations supporting hospitals in Syria implement a system for neurologic emergency triage in the field to ensure that TBI patients are treated appropriately in the prehospital setting. Given the lack of specialists, just-in-time training needs to be provided to general and orthopedic surgeons who provide stabilization of neurotrauma patients to increase their capacity to stabilize these injuries. Moreover, a rapid referral system is needed to quickly transport patients with neurotrauma to facilities with capability to provide stabilization and onward referral for rehabilitative services. As well, we recommend implementing early intervention and education for first responders regarding the immobilization of potential SCI patients in aims to improve prognosis. Finally, given the prevalence of upper extremity peripheral nerve, we would suggest implementing a surgical program focused on reconstructing brachial plexus as well as lower extremity PNI to reduce morbidity of these injuries.
Our study revealed that the conflict in Syria is one that is greatly overlooked. The prevalence of neurologic injuries is increasing as the conflict continues, placing a great strain on the few resources available to alleviate it. Most cases of neurologic injury were treated with surgery, which demonstrated a need for increased time and resource allocation to surgical and postsurgical care. The timing of surgery was often delayed due to postponement of patient presentation and lack of resources, which presents the necessity of an increased need for surgeons, physicians, and allied health professionals with the ability to care for this particular patient population. This delay in appropriate care could influence the morbidity and mortality of injuries sustained. The focal outcome from this epidemiologic study highlighted the intense need for prehospital care, organized transport systems, as well as the overall importance that physicians have in early prevention of unnecessary morbidity and mortality in a population that is suffering acutely from the effects of war.
Footnotes
Podcast: NPub.org/NCP/podcast9-1a
Editorial page 5
Author contributions
Y. El Hajj Abdallah: data analysis and interpretation. M. Saqqur: study concept and design, supervision of study, data acquisition. M. Chan: critical revision of the manuscript for important intellectual content. J. Beveridge: critical revision of the manuscript for important intellectual content. T. Deeb: critical revision of the manuscript for important intellectual content, acquisition of data, contribution in case discourse. A. Saed Easa: acquisition of data, contribution in case discourse. S. Al-Nuaimi: acquisition of data, contribution in case discourse. H. Mowafi: critical revision of the manuscript, acquisition of ethical review.
Study funding
No targeted funding reported.
Disclosure
Y. El Hajj Abdallah is a pharmacy student at Shoppers Drugmart Pharmacy. M. Chan serves as an Associate Editor for Muscle and Nerve and on the editorial board of Canadian Journal of Neurologic Sciences and receives research support from Edmonton Civic Employees Fund, University Hospital Foundation, and Glenrose Foundation. A. Saed Easa, J. Beveridge, S. Al-Nuaimi, and T. Deeb report no disclosures. H. Mowafi serves as an Associate Editor for Trauma BMC Emergency Medicine. M. Saqqur reports no disclosures. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
References
- 1.Syrian Crisis Report. Syria Confronting Fragmentation! Impact of Syrian Crisis Report. Syrian Center for Policy Research; 2015;67. [Google Scholar]
- 2.World Health Organization. Syrian Arab Republic. Annual Report 2017. 2017. Available at: applications.emro.who.int/docs/COPub_SYR_2018_EN_20156.pdf?ua=1. Accessed August 1, 2018. [Google Scholar]
- 3.UNHCR. Situation Syria Regional Refugee Response. 2018. Available at: data2.unhcr.org/en/situations/syria#_ga=2.34003617.1610024342.1534814593-1676494769.1534814593. Accessed August 1, 2018. [Google Scholar]
- 4.Al-Nuaimi S, Aldandashi S, Easa AKS, Saqqur M. Psychiatric morbidity among physically injured Syrian refugees in Turkey. Compr Psychiatry 2018;80:34–38. [DOI] [PubMed] [Google Scholar]
- 5.Birch R, Misra P, Stewart MP, et al. Nerve injuries sustained during warfare: part I: epidemiology. 2012;94:523–528. [DOI] [PubMed] [Google Scholar]
- 6.Daroff R. Neurology in a combat zone: Viet Nam 1966. J Neurol Sci 1999;170:131–137. [DOI] [PubMed] [Google Scholar]
- 7.Kherallah M, Alahfez T, Sahloul Z, Dia Eddin K, Jamil G. Heath care in Syria before and during the crisis. 2012;2:51–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mowafi H, Hariri M, Al nahhas H. Results of a nationwide capacity survey of hospitals providing trauma care in war-affected Syria. JAMA Surg 2016;151:815–822. [DOI] [PubMed] [Google Scholar]
- 9.Freedman B, Serrano JA, Belmont PJ Jr, et al. The combat burst fracture study: results of a cohort analysis of the most prevalent combat specific mechanism of major thoracolumbar spinal injury. Arch Orthop Trauma Surg 2014;134:1353–1359. [DOI] [PubMed] [Google Scholar]
- 10.Schoenfeld A, Goodman GP, Belmont P. Characterization of combat-related spinal injuries sustained by a US army brigade combat team during operation Iraqi freedom. Spine J 2012;12:771–776. [DOI] [PubMed] [Google Scholar]
- 11.Hartmann JE. Neurology in operation Iraqi freedom: risk factors for referral, clinical presentations and incidence of disease. J Neurol Sci 2006;241:83–90. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data available upon request.