Abstract
Chronic pain during childhood is prevalent and costly but access to interdisciplinary pain care is limited. Studies investigating adults waiting for pain clinic evaluation found that symptoms and quality of life deteriorate over the waiting period, but little is known about the experience of adolescents. Therefore, we aimed to determine waitlist times and longitudinal trends of pain, physical, mental and social health over a 12-week period. Ninety-seven adolescents, ages 10-18 years (M age= 14.7 years; 82% female) waiting for evaluation at an interdisciplinary pediatric pain clinic completed assessments at enrollment, four, eight, and 12-week follow-up. We performed a medical record review of attendance patterns twelve months later. Twelve adolescents and their parents also completed qualitative interviews describing their experience waiting for evaluation. Wait times averaged 197.5 days (range 69-758 days) from time of referral to first-attended appointment, and 86.6% of youth completed appointments. Longitudinal repeated measures analyses demonstrated little improvement in pain or other domains of functioning over the 12-week period. In qualitative interviews, families described anxious anticipation for the upcoming appointment combined with frustration in waiting. Findings highlight the need to consider approaches to reduce wait times and provide early intervention for youth awaiting pain clinic evaluation.
Keywords: chronic pain, pediatric, evaluation, waiting list
Introduction
Epidemiological studies indicate that chronic pain is common in children and adolescents with median prevalence rates of 11% to 38% depending upon the condition [14]. Chronic pain negatively affects multiple domains of functioning for children and adolescents including school attendance, social, physical, and athletic activities, and emotional functioning [16]. Because longitudinal data demonstrates that childhood chronic pain places individuals at significant risk for developing or continuing with chronic pain, physical symptoms, and psychiatric complaints into adulthood [22], effective treatment of pain in childhood is critical for preventing or lessening the enormous societal impact of adult chronic pain. Indeed, costs of childhood pain are higher than costs of other common childhood conditions, estimated at $19.5 billion annually in the United States [8], with potential to increase substantially as youth age into adulthood.
Interdisciplinary pain treatment is the gold standard recommendation for children and adolescents with complex chronic pain [1]. However, interdisciplinary evaluations are both staff and time intensive and systems of care (e.g., fee for service) create barriers to access and receipt of timely care. Moreover, geographic distance to clinics, which are typically in large metropolitan areas, creates personal barriers for families [19]. In the United States, there are approximately 45 interdisciplinary pediatric chronic pain programs, and typically each program serves a very wide catchment area [18]. Due to the small number of pain clinics and limited staff, wait times for evaluation at interdisciplinary tertiary care pain clinics are highly variable. In adult pain clinics, a median wait time of six months was reported in several countries [6].
A number of international efforts address access to treatment. In particular, the International Association for the Study of Pain (IASP) established a Task Force on Wait Times in 2009 to provide a consensus on appropriate wait-times benchmarks for treatment of chronic pain [12]. This group reviewed available data from systematic reviews of studies of adults waiting for pain clinic appointments, which demonstrated either no improvement or deterioration of symptoms including worsening depression, anxiety, and quality of life, e.g.,[4, 15], Therefore, the Task Force recommended that people with chronic pain should be seen within 8 weeks based on data that lengthy wait lists have potential negative impact on patient symptoms and quality of life.
Similar attention has not been devoted to access for pediatric chronic pain services; data are not available for wait times in pediatric pain clinics but the limited overall access to clinics has been noted. For example in a review of 102 multidisciplinary pain treatment facilities in Canada only five were specifically devoted to children [20], It is critically important to address this gap in knowledge and understand the experience of youth and families waiting to be seen for pain clinic evaluation. This has potential to fuel advocacy for access to appropriate pediatric resources, to improve referral and triage, and innovate services that might be offered during the waiting period.
Thus, we conducted a mixed methods study to 1) determine wait times and attendance patterns in one interdisciplinary pediatric pain clinic located in the U.S., 2) examine longitudinal patterns of pain intensity, physical, mental and social health (i.e., physical mobility, anxiety and depressive symptoms, fatigue, peer relationships, and pain interference) over a 12-week period of the wait list, and 3) obtain qualitative data on child and parent perspectives on their experience waiting to attend pain clinic evaluation. We hypothesized, similar to adults on waiting lists, adolescent’s symptoms would either not improve or deteriorate over the 12-week period.
Methods
Participants and Sampling Approach
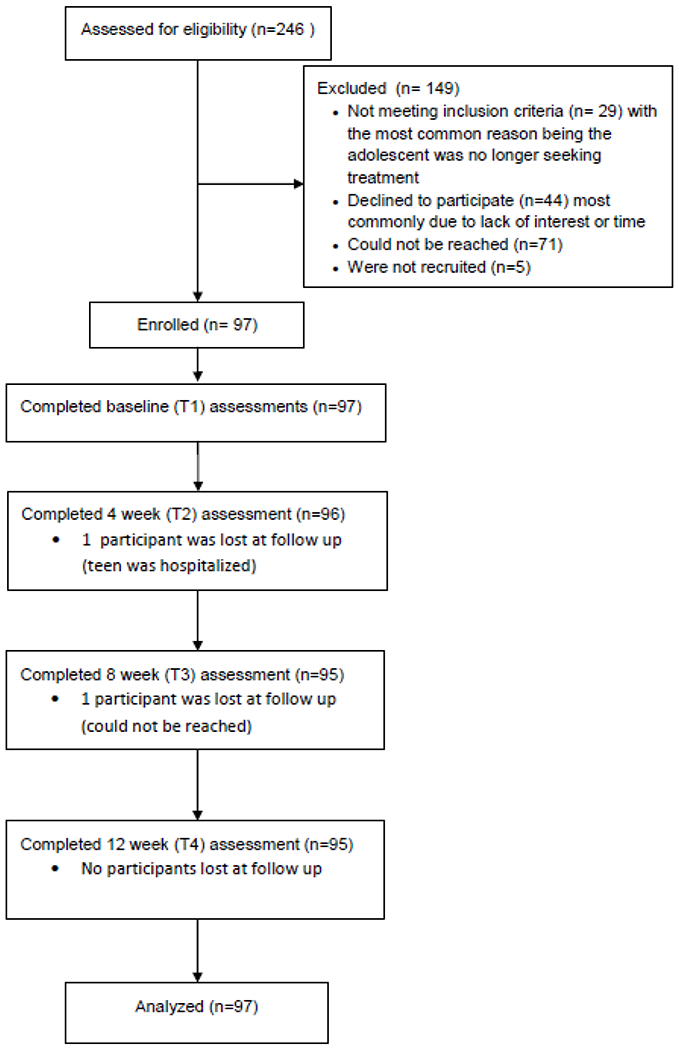
Our sample size was determined by the number of youth on the wait list and we aimed to enroll as many as could be reached who met inclusion criteria. Eligibility requirements included (a) adolescent referred to the tertiary pediatric pain clinic at Seattle Children’s Hospital; (b) adolescent aged 10-18 years, (c) on the waitlist to schedule a pain clinic appointment or have an existing scheduled appointment at least 12 weeks from study enrollment; (d) fluency in English; and (e) no reported developmental delay. There were 246 youth on the wait list and we sent letters about the study to all of these families. After repeated phone attempts, we were able to make contact with 171 of them. Twenty-nine youth did not meet inclusion criteria, with the most common reason being the adolescent was no longer seeking a pain clinic evaluation; 43 families declined to participate most commonly due to lack of interest or time. These youth did not differ from enrolled youth on demographic characteristics. We enrolled 97 families; there was minimal loss to follow up over the 12 week study period (1 family dropped out at T2 due to teen’s hospitalization and 1 family dropped out at T3 who could not be reached).
Description of Interdisciplinary Pain Clinic
Study participants were on the waitlist to be clinic located in a tertiary medical center in the Northwestern United States. The pain program was started in 1985. Current providers include two physicians (MD), three pediatric pain psychologists, and three physical or occupational therapists (PT/OT). The pain clinic operates three days a week and conducts between three to 12 new patient intakes weekly. Over 400 annual visits are conducted each year for new patients. The waitlist is ordered in general by referral date, but patients are prioritized who had a recent hospital discharge or have high acuity. In addition, patients with a complex regional pain syndrome diagnosis are prioritized on the basis of evidence that intensive physical therapy is the cornerstone of treatment, and that patients with CRPS can suffer from significantly rapid decline in function without proper treatment.
Procedures
All study procedures were approved by the local institutional review board. We identified adolescents from the queue of referrals to the pain clinic. Study staff screened families for eligibility and consented families into the study over the phone. Enrolled parents and adolescents received separate links to online questionnaires administered via REDCap. They completed questionnaires at baseline (T1) and four weeks (T2), eight weeks (T3), and 12 weeks (T4) post-enrollment. Families were reimbursed with gift cards for their participation at each time point.
Of the families enrolled in the study, a random number generator was used to select 15 families to complete a semi-structured interview after the T4 assessment to discuss their experience waiting for a pain clinic appointment. Five families declined the opportunity to complete the interview. We reached data saturation at n = 12 interviews and chose to stop collecting these data. Parents and teens were interviewed individually and were asked to be in separate rooms during the interview to avoid influencing the other’s responses. These interviews were recorded and transcribed. For the purpose of the present analysis, we coded responses to one question, “What was the waiting period like for you?”
Measures
Demographics:
Parents reported their own household income, education level, work experience, race, and ethnicity. Parents also provided their teen’s age, sex, race, and ethnicity.
Review of medical record:
In order to fully capture appointment history, we waited until 12 months after the last participant was enrolled to review each adolescent’s electronic health record to obtain the date of their pain clinic appointment including the status of the appointment (completed, cancelled, missed, rescheduled).
Pain Characteristics:
At baseline, adolescents reported on their pain intensity on a 10-point NRS (0 = “no pain”, 10 = “worst pain you can think of”). Adolescents reported primary pain location in a multiple choice format, and pain onset using open-ended questions. Parents reported their child’s current medications and health services used for pain over 6 months.
PROMIS 25:
Adolescents completed the PROMIS-25 Profile (v1.1 )[13] at all four time\ points. This measure is a Pediatric Profile instrument developed as part of the Patient-Reported Outcomes Measurement Information System (PROMIS) to assess various domains of physical, mental and social health in children. This particular profile uses 4-item short forms to measure six domains including physical function-mobility, anxiety/fear, depressive symptoms, fatigue, peer relationships, and pain interference. Adolescents reported the extent to which they experienced particular areas of difficulty within each domain in the past seven days on a five point Likert scale. Subscales were summed and converted to a standardized T-score, with a mean of 50 and a SD of 10.
Scores are considered clinically elevated when they are greater than one SD above the mean (in the case of negatively-worded concepts including anxiety, depressive symptoms, fatigue) or below the mean (in the case of positive-worded concepts including pain interference and peer relationships). For the purposes of our longitudinal analyses we were interested in individual change in these domains over the course of the 12-week period.
Data Analysis
We summarized sample characteristics by examining means and frequencies on variables of interest. Based on our medical record review of pain clinic attendance, we calculated the number of days from referral until the appointment in the pain clinic. We were able to capture appointment status for all enrolled participants. However, because we found that some families were seen in the pain clinic for appointments during the 12-week study period, we created an indicator variable recording whether an adolescent completed a pain clinic visit during this period to add to our analysis. This included whether or not an appointment was completed by the time of the 4 week, 8 week, or 12-week follow-up assessments, or if it occurred following the 12-week follow-up. In an exploratory manner, we examined associations between baseline characteristics and time to complete pain clinic visit using ANOVA for continuous variables and chi-squared test for categorical variables. We also examined pain level preceding the pain clinic visit and performed comparisons between those who completed pain clinic visits and who had not during the study period using two-sample t-test at different time points.
Our primary analysis included examining changes in pain and physical, mental and social health over time using linear mixed effects regression models, in which time was modelled as a discrete variable and covariates adjusted for included adolescent age, sex, race/ethnicity, parental education and timing of pain clinic visit. A subject specific random intercept was included in each model to account for within-subject correlations. The time specific coefficients capture the averaged changes from baseline at each time point. All available data were used in analyses.
All analyses were conducted using the R version 3.4.3 statistical software and Ime4 package[21].
Qualitative Coding.
We applied semantic the analysis using an inductive approach, such that themes were not pre-determined, but rather generated from the data in a bottom-up manner. We followed Braun and Clarke’s [2] guidelines for using this approach, and Wu et al’s [23] guidelines for ensuring rigor in the qualitative analysis. First, two primary coders familiarized themselves with the data by reading interview transcripts. Interview data were then broken up into “codes,” isolating meaningful units of text within each transcript: parent and child transcripts were analysed together, but the source of each code (i.e., parent or child) was preserved. Codes that were semantically similar (i.e., two codes convey the same sentiment using different language) were then collapsed. Next, the two coders worked together to group similar codes into categories. Finally, we grouped these categories into overarching themes. At each stage of coding, we recorded in a codebook with detailed definitions and representative quotes the codes, categories and themes were recorded, as well as notable decisions made throughout the coding process. Working from this codebook, the two primary coders worked together to achieve consensus. When there was disagreement, a third member of the author team arbitrated. Through this process, 100% agreement was achieved at every stage. To increase credibility of final themes, a fourth member of the author group read through original transcripts and ensured quotes were well reflected through codes, categories and final themes.
Results
Sample characteristics.
As shown in Table 1, we enrolled 97 adolescents between 10-18 years (mean age= 14.7 years, (SD = 1.8; 82% female) waiting for pain clinic evaluation. The majority of adolescents were Caucasian (81%), non-Hispanic (90%) and from households with incomes greater than $50K (74%). At enrollment, adolescents reported moderate pain intensity (M= 5.8, SD = 1.8) with abdomen (24%), head (18%), and back (14%) representing the most common primary pain locations. Duration of pain ranged from 3 months to 16 years with a mean of 3.3 years. 65 youth were taking a prescription medication at baseline including antidepressants/anxiolytics/antipsychotics (24%), antiepileptics (7%), and opioids (8%). Youth used a range of health services in the prior 6 months to treat pain or symptoms relating to pain (61% primary care physician, 71% specialists, 17% psychiatrist, 22% psychologist or mental health counselor, 39% physical therapist, 26% massage therapist, 17% acupuncture, 21% chiropractor, 19% naturopath). Families came from a large catchment area with distance to medical center ranging from 2.5 to 1800 miles (M = 111.3 miles).
Table 1.
Sample characteristics (N=97)
| Characteristics | Summary Statistics |
|---|---|
| Child age in years, M(SD) | 14.7 (1.8) |
| Child sex, N (%) | |
| Male | 17 (17.5%) |
| Female | 80 (82.5%) |
| Child race, N (%) | |
| Caucasian | 78 (80.4%) |
| African American | 3 (3.1%) |
| Asian American | 3 (3.1%) |
| American Indian or Alaska Native | 1 (1.05%) |
| Other | 11 (11.3%) |
| Missing/Unknown | 1 (1.05%) |
| Child ethnicity, N (%) | |
| Hispanic or Latino | 5 (5.15%) |
| Not Hispanic or Latino | 86 (88.7%) |
| Missing/Unknown | 6 (6.15%) |
| Parent education, N (%) | |
| High school or less | 12 (12.4%) |
| Vocational school/some college | 28 (28.9%) |
| College | 35 (36%) |
| Graduate/Professional school | 19 (19.6%) |
| Missing/Unknown | 3 (3.1%) |
| Household income, N (%) | |
| Less than $10,000 | 5 (5.15%) |
| $10,000 - $29,999 | 7 (7.2%) |
| $30,000 - $49,999 | 12 (12.4%) |
| $50,000 - $79,999 | 11 (11.3%) |
| $80,000 - $119,999 | 22 (22.7%) |
| $120,000 - $149,999 | 12 (12.4%) |
| More than $150,000 | 22 (22.7%) |
| Missing/Unknown | 6 (6.15%) |
| Pain location, N (%) | |
| Head | 17 (17.5%) |
| Neck | 2 (2.1%) |
| Chest | 3 (3.1%) |
| Hand/Arm/Shoulder | 10 (10.3%) |
| Back | 14 (14.4%) |
| Legs | 12 (12.4%) |
| Abdominal | 23 (23.7%) |
| Feet | 5 (5.15%) |
| Other | 11 (11.3%) |
| Baseline Medications, N (%) | |
| Any Prescription | 65 (67%) |
| No Prescription | 32 (33%) |
| Antidepressant/Anxiolytic/Antipsychotic* | 23 (23.7%) |
| Antiepileptic* | 7 (7.2%) |
| Opioids* | 8 (8.2%) |
| Other* | 32 (33% ) |
| Referral Source | |
| Adolescent Medicine | 4 (4%) |
| PCP | 31 (32%) |
| Gastroenterology | 5 (5.15%) |
| Orthopedics | 5 (5.15%) |
| Rheumatology | 31 (32%) |
| Neurology | 12 (12.4%) |
| Other | 9 (9.3%) |
| Timing of pain clinic visit, N | |
| By T2 | 13 (13.4%) |
| By T3 | 12 (12.4%) |
| By T4 | 11 (11.3%) |
| After T4 | 61 (62.9%) |
not mutually exclusive categories
Referrals to the pain clinic came from PCPs (32%), and subspecialists including adolescent medicine (4%), gastroenterology (5.15%), orthopaedics (5.15%), rheumatology (32%), neurology (12.4%), and other (e.g., naturopathic providers, psychiatry; 9.3%). Twenty-one youth received a second referral from another provider during the wait period.
As shown in Table 2, baseline mean scores on PROMIS scales were in the clinically elevated range for pain interference and for mobility; the others were in the average range compared to normative data. However, at the individual level, 82.5% of the sample had T scores in the clinically elevated range on at least one subscale at baseline, and 76.8% continued to have scores in the clinically elevated range at 12 week follow-up.
Table 2.
Summary statistics of pain and PROMIS outcomes across time points
| Outcome | T1 (N=97) Mean (SD) | T2 (N=96) Mean (SD) | T3 (N=95) Mean (SD) | T4 (N=95) Mean (SD) |
|---|---|---|---|---|
| Average pain intensity | 5.8 (1.7) | 5.4 (1.8) | 5.7 (1.9) | 5.5 (2.0) |
| PROMIS Anxiety/Fear T-Score | 56 (11) | 56 (12) | 55 (11) | 55 (13) |
| PROMIS Depression/Sadness T-Score | 53 (11) | 54 (11) | 54 (11) | 54 (11) |
| PROMIS Fatigue T-Score | 58 (11) | 59 (10) | 59 (10) | 58 (12) |
| PROMIS Mobility T-Score | 39.3 (7.6) | 38.4 (7.1) | 38.3 (7.5) | 39.3 (7.4) |
| PROMIS Pain Interference T-Score | 60.7 (7.4) | 59.9 (7.8) | 60.0 (7.5) | 58.1 (8.3) |
| PROMIS Peer Relationship T-Score | 47.7 (9.4) | 46.6 (10.7) | 47.6 (10.1) | 47.8 (9.7) |
Wait times
We were able to capture appointment status for all 97 enrolled participants. Eighty-four (86.6%) youth attended a new patient evaluation in pain clinic according to review of medical records one year later. Two of these patients had cancelled and rescheduled appointments. Eleven patients did not schedule or attend an appointment. One patient with a scheduled appointment failed to show and did not reschedule. Wait times averaged 197.5 days (range 69758 days) from time of first referral to the new patient appointment.
Thirty-six adolescents had their pain clinic evaluation during the 12-week study period (see Table 1): 13 were seen by T2 (4 weeks), 12 were seen by T3 (8 weeks), and 11 were seen by T4 (12 weeks). The remaining 61 adolescents were not seen until after the study period was complete (after 12 weeks).
As an exploratory analysis of factors that may relate to timing of pain clinic visits, we examined whether baseline demographic variables, baseline pain level or PROMIS measures were associated with the timing of pain clinic visits. When comparing pain levels and other PROMIS measures preceding the pain clinic visits with the corresponding measures from those who had not made the clinic visit, no statistically significant differences were detected between the two groups (seen vs not seen).
Symptom trajectories over the waiting period.
We fitted separate linear mixed effects regression models to pain intensity and to each domain of physical, mental and social health assessed by the PROMIS-25 profile. Time was modelled as a discrete predictor. Covariates included age, sex, race/ethnicity, parental education and timing of pain clinic visits. The estimated regression coefficients are listed in Table 3. Adolescent pain intensity trajectory showed large variation during the waiting period with significant drops at T2 and T4, but large rebound (i.e., higher pain intensity) at T3. There was a trend for depression to increase at T4. No significant changes in other PROMIS measures over time were detected in this cohort, except that by T4 youth demonstrated significant improvement from baseline to T4 in pain interference PROMIS T-scores.
Table 3.
Comparison of outcomes across time using linear mixed effects regression models
| T2 β (95% CI) | T3 β (95% CI) | T4 β (95% CI) | |
|---|---|---|---|
| Pain intensity | −0.38 (−0.72, −0.05)** | −0.12 (−0.46, 0.22) | −0.38 (−0.71, 0.04)** |
| PROMIS Anxiety/Fear | −0.24 (−2.08, 1.60) | −0.23 (−2.06, 1.60) | −0.49 (−2.32, 1.35) |
| PROMIS Depression/Sadness | 0.92 (−0.53, 2.37) | 0.70 (−0.75, 2.14) | 1.29 (−0.16, 2.73)* |
| PROMIS Fatigue | 0.27 (−1.30, 1.84) | 1.31 (−0.25, 2.87) | −0.22 (−1.78, 1.35) |
| PROMIS Mobility | −1.02 (−2.43, 0.39) | −1.10 (−2.50, 0.31) | −0.10 (−1.51, 1.30) |
| PROMIS Pain Interference | −0.82 (−2.14, 0.49) | 0.60 (−1.91, 0.71) | −2.31 (−3.62, −1.00)*** |
| PROMIS Peer Relationship | −1.11 (−2.85, 0.63) | −0.77 (−2.51, 0.96) | −0.44 (−2.17, 1.29) |
Baseline (T1) is the reference point. The coefficients are corresponding to T2 vs. T1, T3 vs. T1, and T4 vs. T1.Additional covariates controlled for included adolescent age, sex, race (White/Non-White), ethnicity (Hispanic/Non-Hispanic), parental education and timing of pain clinic visit.
p<0.10;
p<0.05;
p<0.01
Qualitative Interviews: Child and parent perspectives on waiting for pain clinic evaluation
Semantic analysis of 12 parent-teen dyad interviews revealed one overarching family theme describing frustration and anxious anticipation in being on the wait list for a pain clinic appointment.
Frustration/anxiety.
One of the families completing interviews had removed their adolescent’s name from the wait list because they were tired of waiting. Parents described the challenge of witnessing their teen’s ongoing pain. The wait period itself was full of anticipation; the appointment was often on parent’s minds.
“[Waiting] was really hard. It was very frustrating” (Parent 4)
“Any time she would have any pain it was just like, we would just look at the calendar like... we’re having to check days off and kind of get through it” (Parent 11)
It was hard for youth to wait for their appointment. Like their parents, they described frustration with the waiting period as well as anticipation for its arrival. In addition, they described ongoing pain during the wait period that interfered with their functioning.
“But I was kind of like... should I like keep the appointment? I wasn’t sure if I should keep it or if I should just say like you know maybe it’s not worth it to like wait this long. ” (Adolescent 10)
“I was really anticipating the appointment. It was hard to wait.” (Teen 9)
“The longer I’ve had the pain it’s gradually just gotten worse and worse so [the waiting period] was really frustrating” (Teen 9)
Anticipation/hopefulness.
Though waiting was frustrating, parents described anticipation and hopefulness for the appointment. Parents looked forward to the appointment and wished it would come sooner. They were elated when scheduling changes allowed them to be seen earlier than expected in clinic.
“There was a lot of let’s see anticipation and looking forward to the appointment.” (Parent 7)
“At least there’s a light at the end of the tunnel” (Parent 11)
“We were told it was going to be six to eight months so four months was nothing. It was pretty amazing to get the call as early as we did.” (Parent 6)
Adapting.
Departing from family themes, adolescents also described a process of adapting to the waiting period. Youth noted that they felt the same during the wait period, reported actively using coping skills, and even described forgetting about their upcoming appointment.
“[The waiting period] wasn’t really different for me. I’ve had this like my entire life. So it didn’t matter much.” (Teen 6)
“She can have good days as well as bad days, so it’s not, it’s not like she’s been in constant agony the whole time” (Parent 5)
Discussion
We conducted a mixed methods study about the experience of 97 youth waiting to be seen for an interdisciplinary pediatric pain clinic evaluation to determine waitlist times, longitudinal trends of pain, physical, mental and social functioning over a 12-week period, and to obtain individual perspectives from a subset of youth and their parents. Our findings confirmed a lengthy wait period with an average time to be seen for evaluation of 6.5 months. There were no demographic or clinical predictors (i.e., worse pain) of the length of the wait period. Most families (86.6%) followed through with appointments although a subgroup of families removed themselves from the wait list and did not schedule appointments. Over a 12-week measurement period, we evaluated pain intensity, pain interference, mobility, fatigue, anxiety, depression, and peer relationships, finding relative stability in youth’s functioning over time. Pain interference did significantly improve at the 12-week assessment in comparison to baseline. On one hand, it is encouraging that youth’s symptoms did not deteriorate over time as has been found in adults on waiting lists for pain clinic [4,14], but on the other hand, youth are maintaining a high symptom burden for a number of months while waiting for evaluation. A subgroup of youth are also on medications for pain (i.e., opioids) at the time of referral to a lengthy wait list, which is also a concern if they are not being closely monitored.
Wait times have been described in a recent systematic review evaluating multidisciplinary chronic pain treatment facilities for adults in Australia, Canada, Italy, United Kingdom and the United States [6], This review found significant limitations in available resources and lengthy average wait times of 6 months for adults with chronic pain [6], The only study to report wait times for multidisciplinary pain treatment facilities for children was conducted in Canada [20] in five pediatric facilities where the median wait time was 4 weeks but with a wide range of up to 9 months. Nevertheless, our findings from this study and other data from adult interdisciplinary pain clinics suggests that the IASP recommendation of 8 weeks as a maximum wait time for chronic pain evaluation is rarely accomplished [12].
Qualitative interviews offered a glimpse into the experience of children and their parents during the waiting period. As expected, children and parents experienced frustration and anxious anticipation for the appointment. Parents shouldered much of the burden of the timing of the appointment given their role in managing their child’s health care. But, there was hopefulness present in these families as well and some children described adapting to the waiting period. Indeed more research is needed to understand patient and family reactions to referral and the wait period to understand possible resiliency factors that could be targeted in interventions. These data complement the questionnaire data on symptom trajectories by highlighting the experience of children and parents while waiting for pain clinic evaluation. Qualitative results also offer some insight for providers to better understand thoughts and feelings of frustration and anxiety of parents/children while on the waitlist that may help them to build rapport and forge a connection with these families at the time of the initial contact.
The present study has several limitations that should be considered in interpreting the study findings. Our sample included youth waiting to be seen in a single tertiary care pediatric pain treatment facility and may not be representative of wait times or patient characteristics of those seen in other pediatric chronic pain treatment facilities, especially those with differing volumes and staffing. It also represents only one subset of the population with chronic pain - those referred to tertiary pain care. We cannot speak broadly to the issue of regional accessibility and wait times to first appointment in other specialty clinics or community settings for youth with chronic pain. The study did not include patients who were seen promptly due to their disease condition, such as cancer, and thus the sample may not be fully representative of patients with chronic pain. Furthermore, the sample was predominantly non-Hispanic White. It is possible that patients and families experienced reactivity to measurement of symptoms during the wait time and experienced some benefit from their study participation due to being asked about symptoms. However, our study has several strengths including the high response and retention rates, repeat symptom measurement at four time points over three months using well-standardized measures, and use of complementary qualitative data to obtain child and family perspective.
There are a number of future research directions. The undertreatment of pain is considered a societal problem and concerns about access and models of care delivery have been identified in the IOM report on chronic pain [11], and in the recently released Federal Pain Research Strategy. Research is critically needed to understand effective models of care for pediatric chronic pain treatment facilities. Similar to what has been done in adult multidisciplinary treatment facilities in Canada [4] a first step might be to conduct a comprehensive survey to collect data about the volume of patients, referral sources, services offered, and wait times for pediatric chronic pain clinics in the U.S. Moreover, evaluating the cost of care is needed; future studies should document health services used including medications by children waiting to be seen for pain clinic evaluation. It would also be important to understand perspectives of referring physicians to understand whether waiting lists may deter providers from referring their patients. The Canadian STOP-PAIN Project [4] was important for demonstrating the impact of pain on adult patients during the wait time and describing the high economic burden of pain in patients on waitlists [9]. Similar studies are needed to understand the societal impact of children on waitlists for interdisciplinary pain treatment. Addressing these gaps may alert policy makers and health administrators of the access and impact on providing optimal care to youth suffering from chronic pain.
To have the greatest impact with limited resources, studies are needed to test a range of different strategies. For example, studies are needed on approaches to referral and triage such as testing the impact of priority scheduling for certain patient groups (e.g., those most likely to benefit), the role of nurses in triage, or the impact of changing the extent and nature of patient follow-up (e.g., greater use of nurses for follow up care) on wait times, resource allocation, and quality of care provided. Waitlist alternatives have been implemented successfully for other health services [10].
System redesign has also been suggested. One approach evaluated in a few studies in adults conducted in Australia is to implement pre-clinic educational sessions after referral to the wait list. In one study in public pain medicine units in Australia [5], a 2 day pre-clinic group educational program (6 sessions) was found to reduce wait times and costs and increase use of pain management strategies by patients. Burke, Denson, & Mathias [3] tested a single brief pre-clinic educational session delivered to individuals entering the wait-list for a tertiary chronic pain service in Australia. They found all study participants reported significant improvements in pain acceptance (willingness, overall acceptance), health care utilization (frequency) and quality of life (physical), which were maintained/enhanced at 6 months while they were on the wait list.
Another viable strategy to address patient needs during the waiting time is to use low-cost and easily disseminated interventions such as through the internet and smartphone applications. An emerging evidence base now exists for technology-delivered psychological interventions in both adult and pediatric populations; a recent systematic review of the pediatric literature identified eight RCTs, which all delivered cognitive-behavioral therapy, and patients showed improvements in pain and disability [7]. As one recent example, in a large multicenter RCT with 273 adolescents with chronic abdominal, headache, or musculoskeletal pain, Palermo et al. [17] found improvements in daily physical functioning, depressive symptoms, and parent-perceived impact of pain in families receiving an 8-week Internet pain self-management program, compared to an Internet pain education control group. Treatments delivered remotely overcome many barriers of access to health care professionals, which is particularly relevant in pediatric chronic pain, where limited resources exist to provide interdisciplinary pain care for children. Future research is needed to test the timing of such interventions to understand possible benefits during the waiting period.
In conclusion, our findings add to the existing literature demonstrating that children and adolescents have a high burden of symptoms throughout long waiting periods to be seen for interdisciplinary pain clinic evaluation. Lengthy wait periods suggest a pressing need for improved access to pain treatment facilities for children and adolescents with chronic pain. Access is a global problem as the demand for pain services has always been greater than supply of services. Further, novel strategies of referral and triage need to be tested for youth with chronic pain referred for interdisciplinary pain care. The findings are important for characterizing the experience of children with chronic pain waiting for pain clinic evaluation, and highlighting the psychosocial needs of children and their families during this period.
Figure 1.
Highlights:
Access to interdisciplinary pain care is limited for adolescents with chronic pain
Unknown impact of the wait list period on adolescent pain and function
Little improvement was found in pain, physical, mental and social health
Qualitative data revealed anxious anticipation and frustration in waiting
Opportunities exist to provide early intervention for youth waiting for evaluation
Perspective:
This study extends the literature on characteristics and symptom trajectories of adolescents during the wait period for interdisciplinary pain clinic evaluation, previously described only in adults with chronic pain. Findings demonstrated an average wait time of 6.5 months during which youth’s pain, physical, and social health remained impaired.
Acknowledgements
We thank Dr. Gary Walco, Director of Pain Medicine at Seattle Children’s Hospital for his support of the study, Megan Lounds for providing study coordination, and especially the children and families who participated.
Funding: This work was supported by a Center for Child Health, Behavior and Development stimulus grant (TP) and by the National Institutes of Health (grant number K24HD060068) to TP.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures.
None of the authors have any conflicts of interest.
References
- 1.American Pain Society: Assessment and Management of Children with Chronic Pain: a Position Statement (2012). Available at: http://americanpainsociety.org/uploads/get-involved/pediatric-chronic-painstatement.pdf. Accessed May 5, 2018.
- 2.Braun V, Clarke V: Using thematic analysis in psychology. Qual Res Psychol 3: 77–101, 2006 [Google Scholar]
- 3.Burke AL, Denson LA, Mathias JL: Does a brief educational session produce positive change for individuals waiting for tertiary chronic pain services? Pain Med 17:2203–2217, 2016 [DOI] [PubMed] [Google Scholar]
- 4.Choiniere M, Dion D, Peng P, Banner R, Barton PM, Boulanger A, Clark AJ, Gordon AS, Guerriere DN, Guertin MC, Intrater HM, Lefort SM, Lynch ME, Moulin DE, Ong-Lam M, Racine M, Rashiq S, Shir Y, Taenzer P, Ware M: The Canadian STOP-PAIN project - Part 1: Who are the patients on the waitlists of multidisciplinary pain treatment facilities? Can J Anaesth 57:539–48, 2010 [DOI] [PubMed] [Google Scholar]
- 5.Davies S, Quintner J, Parsons R, Parkitny L, Knight P, Forrester E, Roberts M, Graham C, Visser E, Antill T, Packer T, Schug SA: Preclinic group education sessions reduce waiting times and costs at public pain medicine units. Pain Med 12:59–71, 2011 [DOI] [PubMed] [Google Scholar]
- 6.Fashler SR, Cooper LK, Oosenbrug ED, Burns LC, Razavi S, Goldberg L, Katz J: Systematic review of multidisciplinary chronic pain treatment facilities. Pain Res Manag 2016: 5960987, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fisher E, Law E, Palermo TM, Eccleston C: Psychological therapies (remotely delivered) for the management of chronic and recurrent pain in children and adolescents. Cochrane Database Syst Rev 3: CD011118, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Groenewald CB, Wright DR, Palermo TM: Health care expenditures associated with pediatric pain-related conditions in the United States. Pain 156:951–957, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Guerriere DN, Choiniere M, Dion D, Peng P, Stafford-Coyte E, Zagorski B, Banner R, Barton PM, Boulanger A, Clark AJ, Gordon AS, Guertin MC, Intrater HM, Lefort SM, Lynch ME, Moulin DE, Ong-Lam M, Racine M, Rashiq S, Shir Y, Taenzer P, Ware M: The Canadian STOP-PAIN project - Part 2: What is the cost of pain for patients on waitlists of multidisciplinary pain treatment facilities? Can J Anaesth 57:549–58, 2010 [DOI] [PubMed] [Google Scholar]
- 10.Harding KE, Leggat SG, Bowers B, Stafford M, Taylor NF: Reducing waiting time for community rehabilitation services: a controlled before-and-after trial. Arch Phys Med Rehabil 94:23–31, 2013 [DOI] [PubMed] [Google Scholar]
- 11.Institute of Medicine. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research, Washington D.C.,The National Academic Press, 2011 [PubMed] [Google Scholar]
- 12.International Association for the Study of Pain Task Force on Wait-Times. Available at: https://www.dgss.org/fileadmin/pdf/Task_Force_on_Wait-Times.pdf. Accessed July 25, 2018.
- 13.Irwin DE, Stucky BD, Thissen D, Dewitt EM, Lai JS, Yeatts K, Varni JW, DeWalt DA: Sampling plan and patient characteristics of the PROMIS pediatrics large-scale survey. Qual Life Res 19:585–94, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.King S, Chambers CT, Huguet A, MacNevin RC, McGrath PJ, Parker L, MacDonald AJ: The epidemiology of chronic pain in children and adolescents revisited: a systematic review. Pain 152:2729–2738, 2011 [DOI] [PubMed] [Google Scholar]
- 15.Lynch ME, Campbell F, Clark AJ, Dunbar MJ, Goldstein D, Peng P, Stinson J, Tupper H: A systematic review of the effect of waiting for treatment for chronic pain. Pain 136:97–116, 2008 [DOI] [PubMed] [Google Scholar]
- 16.Palermo TM: Impact of recurrent and chronic pain on child and family daily functioning: a critical review of the literature. J Dev Behav Pediatr 21:58–69, 2000 [DOI] [PubMed] [Google Scholar]
- 17.Palermo TM, Law EF, Fales J, Bromberg MH, Jessen-Fiddick T, Tai G: Internet-delivered cognitive-behavioral treatment for adolescents with chronic pain and their parents: a randomized controlled multicenter trial. Pain 157:174–85, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pediatric chronic pain programs in North America. Available at: http://americanpainsociety.org/uploads/get-involved/Pain%20clinic%20list%20-%202018%20update%20Final%20as%20of%2002-06-18.pdf. Accessed May 5, 2018.
- 19.Peng P, Choiniere M, Dion D, Intrater H, Lefort S, Lynch M, Ong M, Rashiq S, Tkachuk G, Veillette Y, Group SI: Challenges in accessing multidisciplinary pain treatment facilities in Canada. Can J Anaesth 54:977–84, 2007 [DOI] [PubMed] [Google Scholar]
- 20.Peng P, Stinson JN, Choiniere M, Dion D, Intrater H, Lefort S, Lynch M, Ong M, Rashiq S, Tkachuk G, Veillette Y: Dedicated multidisciplinary pain management centres for children in Canada: the current status. Can J Anaesth 54:985–91, 2007 [DOI] [PubMed] [Google Scholar]
- 21.Team RC: R: A language and environment for statistical computing R Foundation for Statistical Computing, Vienna, Austria, 2012 [Google Scholar]
- 22.Walker LS, Dengler-Crish CM, Rippel S, Bruehl S: Functional abdominal pain in childhood and adolescence increases risk for chronic pain in adulthood. Pain 150:568–72, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wu YP, Thompson D, Aroian KJ, McQuaid EL, Deatrick JA: Commentary: writing and evaluating qualitative research reports. J Pediatr Psychol 41:493–505, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]


