Abstract
Background:
Although sex differences exist in the management of acute coronary syndromes, less is known about the management and outcomes of women and men with suspected coronary artery disease (CAD) being evaluated with non-invasive testing (NIT).
Methods:
We investigated sex-based differences in NIT results and subsequent clinical management in 4720 women and 4246 men randomized to CT angiography vs stress testing in the PROMISE trial. Logistic regression models assessed relationships between sex and referral for catheterization, revascularization, and aspirin or statin use. Cox regression models assessed the relationship between sex and the composite of all-cause death, myocardial infarction, or unstable angina.
Results:
Women more often had normal NITs than men (61.0% vs 49.6%, p<0.001) and less often had mild (29.3% vs 35.4%, p<0.001), moderate (4.0% vs 6.8%, p<0.001), or severe abnormalities (5.7% vs 8.3%, p<0.001) found on NIT. Women were less likely to be referred for catheterization than men (7.6% vs 12.6%, adjusted OR 0.75 [0.62–0.90]; p=0.002). Of those who underwent catheterization within 90 days of randomization (358 women, 534 men), fewer women than men had obstructive CAD (40.8% vs 60.9%, p<0.001). At a 60-day visit, women were significantly less likely than men to report statin usage when indicated (adjusted OR 0.81 [0.73–0.91]; p<0.001), but were similarly likely to report aspirin usage when indicated (adjusted OR 0.78 [0.56–1.08]; p=0.13). Over a median follow-up of 25 months, women had better outcomes than men (adjusted OR 0.73 [0.57–0.94]; p=0.017).
Conclusions:
Although women more frequently had normal NITs compared with men, those with abnormalities on NIT were less likely to be referred for catheterization or to receive statin therapy. The high rates of negative NIT in women, coupled with the better outcomes compared with men, strongly support the need for a sex-specific algorithm to guide NIT and chest pain management.
Keywords: coronary artery disease, women, noninvasive testing, CT angiography
Several studies over the last 4 decades have shown differences in the diagnostic and therapeutic approaches of physicians to women and men with suspected or known ischemic heart disease.1, 2 These reports, which assessed sex-based differences in management after functional stress testing, found disparities in referral for catheterization,3–5 revascularization,1, 2, 4 and subsequent secondary prevention medication treatment.6 These differences were postulated to be due, at least in part, to provider awareness of the high false-positive rate of stress testing in women.7, 8 However, in the current era of medical management of coronary artery disease (CAD) and with the advent of anatomic non-invasive testing (NIT) with CT angiography (CTA), which has lower false-positive rates,8 it is unclear whether sex-based differences in the management of suspected CAD still exist. Further, it is unknown whether any differences in current management translate into disparities in clinical outcomes between women and men.
We sought to address this gap in knowledge using data from the Prospective Multicenter Imaging Study for Evaluation of Chest Pain (PROMISE).9 PROMISE was a pragmatic comparative effectiveness trial of 10,003 outpatients with stable symptoms suggestive of CAD, randomized to a strategy of either functional or anatomic (CTA) testing. Over a median follow-up period of 25 months, there was no difference between testing arms in clinical events overall or by sex.9 Given the high percentage (53%) of women enrolled in this trial and the fact that clinical decision-making was left up to the local providers after the non-invasive test, it is an ideal setting in which to explore sex-based differences in the management and clinical outcomes of patients with stable angina who receive NIT.
Methods
Study Cohort and Design
PROMISE was a pragmatic randomized trial that compared initial anatomic (CTA) vs stress testing in stable symptomatic patients with suspected CAD.9,10 The choice of stress test was left up to the clinician (exercise electrocardiogram, stress echocardiography, or stress nuclear), as were all test interpretations and all subsequent clinical decisions in both testing arms. Randomization was stratified by study site and by the stress test type that was chosen by the provider prior to randomization, if the patient were to be randomized to the stress testing arm.
Categorization of CTA and stress test results into 4 tiers is outlined in Table 1. A catheterization was considered positive if there was ≥70% stenosis in at least one epicardial artery or ≥50% stenosis in the left main artery. Revascularization was defined as percutaneous coronary intervention (PCI) or coronary artery bypass graft (CABG) surgery. Aspirin and statin use were assessed at a 60-day post-randomization visit in individuals with the following indications: a history of stroke, transient ischemic attack, or peripheral arterial disease, or with a positive CTA or positive catheterization. In addition, individuals with a history of dyslipidemia, diabetes, or 10-year atherosclerotic cardiovascular disease risk of at least 7.5% were included in the statin analysis.11
Table 1:
4-Tier test result definitions for CTA and stress testing
| Anatomical | Functional* | |||
|---|---|---|---|---|
| Test Strata | CTA | Exercise Treadmill Test | Stress Nuclear | Stress Echo |
| Severely abnormal | High-risk coronary artery disease • ≥2 vessel disease (≥70%) • OR ≥50% left main stenosis • OR ≥70% proximal left anterior descending stenosis |
Ischemic ECG • ST changes consistent with ischemia during stress + either severe ventricular arrhythmia OR Hypotension |
Large territory inducible ischemia or mixed defect • Septal/anterior/apical territory or other single territory with transient ischemic dilatation or 2 or more coronary territories with ischemia |
Large territory inducible Ischemia or mixed defect • Wall motion abnormality or mixed abnormality (infarct and ischemia) • Isolated Septal/anterior/apical or other single territory +↓EF to <35 % during stress or • 2 or more coronary territories |
| Moderately abnormal | Obstructive coronary artery disease • ≥70% stenosis in 1 major vessel/branch |
Early positive TM • Failure to reach stage 2 (<3:00 min) with ST changes OR symptoms reproduced • OR any arrhythmia or hypotension |
Inducible ischemia or mixed defect • Perfusion abnormality in one coronary territory (Lateral or Inferior/posterior) OR Normal imaging but early positive TM • Failure to reach stage 2 (<3:00 min) with ST changes OR symptoms reproduced • OR any arrhythmia or hypotension |
Inducible ischemia or mixed defect • Wall motion abnormality or mixed abnormality (infarct and ischemia) in one coronary territory (Lateral or Inferior/posterior) OR Normal imaging but Early positive TM • Failure to reach stage 2 (<3:00 min) with ST changes OR symptoms reproduced • OR any arrhythmia or hypotension |
| Mildly abnormal | Nonobstructive coronary artery disease • 1%–69% stenosis in any major • vessels/branch OR <50% • left main stenosis |
Late positive TM • More than stage 2 (>3:00 min) but failure to finish protocol or target heart rate achieved due to ST changes OR symptoms reproduced OR any arrhythmia or hypotension |
Positive ECG • Normal perfusion or fixed perfusion defect (Scar) OR Normal imaging but late positive TM • More than stage 2 (>3:00 min) but failure to finish protocol or target heart rate achieved due to ST changes OR symptoms reproduced OR any arrhythmia or hypotension |
Positive ECG but normal wall motion or resting wall motion abnormality without inducible ischemia OR Normal imaging but late positive TM • More than stage 2 (>3:00 min) but failure to finish protocol or target heart rate achieved due to ST changes OR symptoms reproduced OR any arrhythmia or hypotension |
| Normal | Absence of coronary atherosclerosis | Normal | Normal | Normal |
As defined by Hoffmann U, Ferencik M, Udelson JE, et al., Prognostic value of noninvasive cardiovascular testing in patients with stable chest pain: Insights from the promise trial (prospective multicenter imaging study for evaluation of chest pain). Circulation 2017;135:2320–2332.
CTA, computed tomographic angiography; ECG, electrocardiogram; TM, treadmill test.
The current analysis included all patients who were tested as randomized and who had interpretable results, defined as not missing and not indeterminate. Primary endpoints of the various analyses included invasive catheterization within 90 days of randomization, revascularization within 30 days of invasive catheterization, aspirin and/or statin use at 60-day visit among those with indications, and a composite of death from any cause, myocardial infarction (MI), or unstable angina hospitalization (UAH). Secondary outcomes included a composite of CV death, MI, or UAH, and a composite of CV death and MI alone.
Statistical Analyses
Baseline characteristics were described using frequencies and percentages for categorical variables and mean ± SD for continuous variables. Characteristics were compared between women and men by sex using the Wilcoxon rank sum test for continuous variables and chi-square testing for categorical variables.
A logistic regression model was used to examine the unadjusted and adjusted association between patient sex and referral for catheterization within 90 days of randomization. The adjusted model controlled for clinically relevant covariates including NIT modality; NIT results (4-tier); BMI (kg/m2); age (standardized by sex); chest pain vs other as primary symptom; chest pain typicality (typical, atypical, non-cardiac); and risk factors including smoker (ever/never), diabetes mellitus, hypertension, history of peripheral artery or cerebrovascular disease, sedentary lifestyle, depression, family history of premature CAD, and dyslipidemia. In all models, linearity assumptions were assessed for continuous adjustment variables. A similar model was fit to assess whether the association between patient sex and referral for catheterization within 90 days of randomization was modified by NIT modality. In addition to the adjustment variables specified for the previous model, this model also included a 2-way interaction term between sex and NIT modality.
Among patients who underwent catheterization within 90 days of randomization, a logistic regression model was used to assess the association between sex and revascularization within 30 days of the catheterization. Time zero for this model was set as the day of the catheterization. In addition to the adjustment factors listed for the catheterization model, this model also adjusted for catheterization results (positive/negative). The relationship between sex and self-reported aspirin or statin use at 60-day follow-up was assessed with a logistic regression model among those with an indication for aspirin or statin therapy, as defined above. The adjustment covariates were the same as those in the catheterization model, with the exception of NIT results (4-tier).
Cox proportional hazards models were used to assess the association between patient sex and the primary and secondary composite outcomes. The proportional hazards assumption was assessed in each model. Models were fit in the overall cohort, in those who did not undergo catheterization, in those who underwent catheterization, and in those who underwent revascularization. Adjustment covariates were the same as those for the catheterization model, with the addition of catheterization referral, catheterization results, and referral for revascularization modeled as time-dependent covariates. Similar models were fit in those patients who were referred to catheterization within 90 days of randomization, with the exception that the analysis was landmarked at the time of the catheterization referral. Similar models were fit in those patients who were referred to revascularization within 30 days of catheterization referral, with the exception that those models were landmarked at the time of the referral to revascularization.
Results
Baseline Characteristics
Among the 8966 patients in PROMISE who underwent testing as randomized and who had interpretable results, 4500 (52% female) had CTA and 4466 (53% female) had stress testing (Supplemental Figure 1). As previously reported,12 in both the CTA and stress testing groups, women were older and more likely to have a history of hypertension, peripheral arterial disease or cerebrovascular disease, family history of premature CAD, depression, and a sedentary lifestyle compared with men (Table 2). On the other hand, women had lower Framingham and ASCVD risk scores and were less likely to have a smoking history than men.
Table 2:
Baseline characteristics by NIT type and sex
| CTA (N=4500) | Stress Test (N=4466) | |||||
|---|---|---|---|---|---|---|
| Characteristic | Women (N=2332) | Men (N=2168) | P-value | Women (N=2388) | Men (N=2078) | P-value |
| Demographics | ||||||
| Age, y | 62.2 (7.68) | 58.6 (8.25) | <.001 | 62.6 (7.88) | 59.2 (8.42) | <.001 |
| Racial minority | 398 (17.2) | 315 (14.7) | 0.029 | 358 (15.1) | 285 (13.8) | <.001 |
| Hispanic or Latino ethnicity | 170/2323 (7.3%) | 173/2154 (8.0%) | 0.370 | 156/2370 (6.6%) | 168/2065 (8.1%) | 0.047 |
| Cardiac risk factors | ||||||
| Hypertension | 1534/2332 (65.8%) | 1359/2168 (62.7%) | 0.030 | 1603/2388 (67.1%) | 1314/2078 (63.2%) | 0.006 |
| Diabetes | 500/2332 (21.4%) | 436/2168 (20.1%) | 0.272 | 525/2388 (22.0%) | 447/2078 (21.5%) | 0.702 |
| Metabolic syndrome | 857/2332 (36.7%) | 816/2168 (37.6%) | 0.538 | 904/2388 (37.9%) | 810/2078 (39.0%) | 0.441 |
| Dyslipidemia | 1621/2332 (69.5%) | 1408/2168 (64.9%) | 0.001 | 1637/2388 (68.6%) | 1404/2078 (67.6%) | 0.481 |
| CAD risk equivalent | 598/2332 (25.6%) | 499/2168 (23.0%) | 0.040 | 635/2388 (26.6%) | 522/2078 (25.1%) | 0.263 |
| Peripheral arterial disease or cerebrovascular disease | 134/2332 (5.7%) | 94/2167 (4.3%) | 0.031 | 153/2388 (6.4%) | 103/2078 (5.0%) | 0.038 |
| Family history of premature CAD | 815/2325 (35.1%) | 645/2160 (29.9%) | <.001 | 787/2379 (33.1%) | 592/2073 (28.6%) | 0.001 |
| Depression | 599/2332 (25.7%) | 286/2168 (13.2%) | <.001 | 627/2387 (26.3%) | 339/2078 (16.3%) | <.001 |
| Smoker (ever/never) | 1068/2331 (45.8%) | 1224/2168 (56.5%) | <.001 | 1094/2388 (45.8%) | 1196/2077 (57.6%) | <.001 |
| Sedentary lifestyle | 1227/2328 (52.7%) | 952/2163 (44.0%) | <.001 | 1270/2384 (53.3%) | 892/2074 (43.0%) | <.001 |
| BMI (kg/m2) | 30.4 (6.43) | 30.4 (5.38) | 0.769 | 30.4 (6.59) | 30.5 (5.39) | 0.619 |
| Cardiac risk scores | ||||||
| Framingham Risk Score | 14.7 (9.53) | 28.2 (16.24) | 0.000 | 15.3 (10.15) | 29.2 (16.32) | <.001 |
| ASCVD Pooled Cohort Risk Equation | 12.1 (10.93) | 16.5 (11.40) | 0.000 | 12.9 (11.79) | 17.3 (11.51) | <.001 |
| Presenting symptoms | 0.290 | 0.928 | ||||
| Chest pain | 1744/2332 (74.8%) | 1578/2165 (72.9%) | 1711/2387 (71.7%) | 1489/2076 (71.7%) | ||
| Provider characterization | 0.647 | 0.237 | ||||
| Typical | 261/2332 (11.2%) | 260/2168 (12.0%) | 265/2388 (11.1%) | 241/2078 (11.6%) | ||
| Atypical | 1818/2332 (78.0%) | 1683/2168 (77.6%) | 1853/2388 (77.6%) | 1634/2078 (78.6%) | ||
| Non-cardiac | 253/2332 (10.8%) | 225/2168 (10.4%) | 270/2388 (11.3%) | 203/2078 (9.8%) | ||
| Dyspnea | 322/2332 (13.8%) | 311/2165 (14.4%) | 385/2387 (16.1%) | 328/2076 (15.8%) | ||
| Other | 266/2332 (11.4%) | 276/2165 (12.7%) | 291/2387 (12.2%) | 259/2076 (12.5%) | ||
| Baseline medication use | ||||||
| Aspirin | 967/2273 (42.5%) | 978/2030 (48.2%) | <.001 | 928/2316 (40.1%) | 961/1963 (49.0%) | <.001 |
| Statin | 1028/2273 (45.2%) | 945/2030 (46.6%) | 0.384 | 1026/2316 (44.3%) | 938/1963 (47.8%) | 0.023 |
| Beta-blocker | 614/2273 (27.0%) | 451/2030 (22.2%) | <.001 | 641/2316 (27.7%) | 429/1963 (21.9%) | <.001 |
| ACEi or ARB | 934/2273 (41.1%) | 926/2030 (45.6%) | 0.003 | 1013/2316 (43.7%) | 890/1963 (45.3%) | 0.294 |
Data reported as mean (SD) or n/N (%).
Abbreviations: CAD – coronary artery disease; BMI – body mass index; ASCVD – atherosclerotic cardiovascular disease; ACEi – angiotensin-converting enzyme inhibitor; ARB – angiotensin receptor blocker.
Sex Differences in Noninvasive Test Results
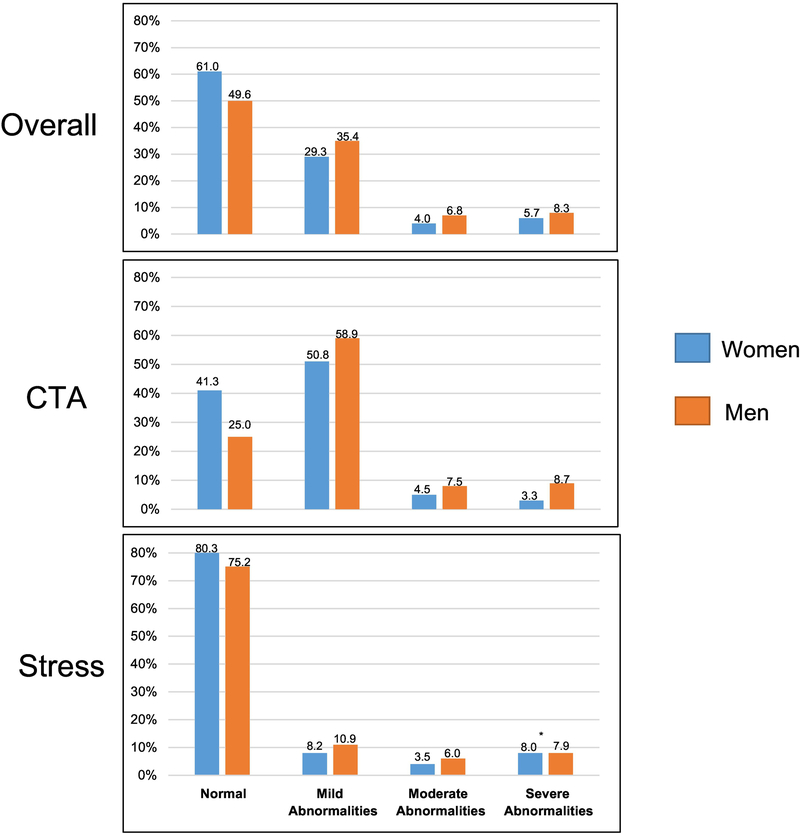
In both testing arms, women had more normal NITs than men (CTA: 41.3% vs 25.0%, p<0.001; stress: 80.3% vs 75.2%, p<0.001), and fewer mildly abnormal (CTA: 50.8% vs 58.9%, p<0.001; stress: 8.2% vs 10.9%, p=0.003) or moderately abnormal (CTA: 4.5% vs 7.5%, p<0.001; stress: 3.5% vs 6.0%, p<0.001) test results. While fewer women had a severe abnormality on CTA compared with men (3.3% vs 8.7%, p<0.001), there was a similar proportion of women and men with a severe abnormality on stress testing (8.0% vs 7.9%, p=0.98) (Table 3; Figure 1).
Table 3:
Test results and processes of care by sex and noninvasive testing arm
| Overall (N=8966) | CTA (N=4500) | Stress Test (N=4466) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Characteristic | Women (N=4720) | Men (N=4246) | P-value | Women (N=2332) | Men (N=2168) | Pvalue | Women (N=2388) | Men (N=2078) | P-value |
| Severe abnormalities | 268/4720 (5.7%) | 353/4246 (8.3%) | <.001 | 78/2332 (3.3%) | 188/2168 (8.7%) | <.001 | 190/2388 (8.0%) | 165/2078 (7.9%) | 0.984 |
| Referral to ICA within 90 days of randomization | 155/268 (57.8%) | 221/353 (62.6%) | 55/78 (70.5%) | 138/188 (73.4%) | 100/190 (52.6%) | 83/165 (50.3%) | |||
| ICA Positive | 73/155 (47.1%) | 159/221 (71.9%) | 40/55 (72.7%) | 103/138 (74.6%) | 33/100 (33.0%) | 56/83 (67.5%) | |||
| Referral for revascularization within 30 days of ICA | 56/73 (76.7%) | 139/159 (87.4%) | 29/40 (72.5%) | 91/103 (88.3%) | 27/33 (81.8%) | 48/56 (85.7%) | |||
| Moderate abnormalities | 190/4720 (4.0%) | 287/4246 (6.8%) | <.001 | 106/2332 (4.5%) | 162/2168 (7.5%) | <.001 | 84/2388 (3.5%) | 125/2078 (6.0%) | <.001 |
| Referral to ICA within 90 days of randomization | 76/190 (40.0%) | 165/287 (57.5%) | 58/106 (54.7%) | 103/162 (63.6%) | 18/84 (21.4%) | 62/125 (49.6%) | |||
| ICA Positive | 41/76 (53.9%) | 107/165 (64.8%) | 32/58 (55.2%) | 73/103 (70.9%) | 9/18 (50.0%) | 34/62 (54.8%) | |||
| Referral for revascularization within 30 days of ICA | 36/41 (87.8%) | 94/107 (87.9%) | 28/32 (87.5%) | 64/73 (87.7%) | 8/9 (88.9%) | 30/34 (88.2%) | |||
| Mild abnormalities | 1382/4720 (29.3%) | 1502/4246 (35.4%) | <.001 | 1185/2332 (50.8%) | 1276/2168 (58.9%) | <.001 | 197/2388 (8.2%) | 226/2078 (10.9%) | 0.003 |
| Referral to ICA within 90 days of randomization | 100/1382 (7.2%) | 117/1502 (7.8%) | 80/1185 (6.8%) | 92/1276 (7.2%) | 20/197 (10.2%) | 25/226 (11.1%) | |||
| ICA Positive | 28/100 (28.0%) | 53/117 (45.3%) | 23/80 (28.8%) | 40/92 (43.5%) | 5/20 (25.0%) | 13/25 (52.0%) | |||
| Referral for revascularization within 30 days of ICA | 24/28 (85.7%) | 39/53 (73.6%) | 19/23 (82.6%) | 27/40 (67.5%) | 5/5 (100.0%) | 12/13 (92.3%) | |||
| Normal | 2880/4720 (61.0%) | 2104/4246 (49.6%) | <.001 | 963/2332 (41.3%) | 542/2168 (25.0%) | <.001 | 1917/2388 (80.3%) | 1562/2078 (75.2%) | <.001 |
| Referral to ICA within 90 days of randomization | 27/2880 (0.9%) | 31/2104 (1.5%) | 2/963 (0.2%) | 1/542 (0.2%) | 25/1917 (1.3%) | 30/1562 (1.9%) | |||
| ICA Positive | 4/27 (14.8%) | 6/31 (19.4%) | 0/2 (0.0%) | 0/1 (0.0%) | 4/25 (16.0%) | 6/30 (20.0%) | |||
| Referral for revascularization within 30 days of ICA | 2/4 (50.0%) | 5/6 (83.3%) | - | - | 2/4 (50.0%) | 5/6 (83.3%) | |||
Data reported as n/N (%).
Figure 1:
NIT test results by sex and NIT type. *This is the only non-statistically significant comparison between women and men presented in this figure.
Sex Differences in Processes of Care after Noninvasive Testing
Similar proportions of women and men with severe abnormalities, mild abnormalities, or normal NITs were referred for catheterization (Table 3). However, among those with a moderately abnormal NIT, fewer women than men were referred for catheterization (40.0% vs 57.5%, p<0.001). After adjustment for clinical factors, including NIT type and 4-tier test result, women overall were less likely to be referred for catheterization compared with men (OR [95% CI] 0.75 [0.62–0.90], p=0.002) (Table 4). This sex-based difference in referral for catheterization was not modified by type of NIT or by 4-tier NIT result (adjusted interaction p=0.25).
Table 4:
Associations between sex and processes of care measures*
| Frequency of Event (# Events/Sample Size) | Unadjusted | Adjusted | ||||
|---|---|---|---|---|---|---|
| Factor of Interest | Women | Men | Odds Ratio (95% CI) | P-value | Odds Ratio (95% CI) | P-value |
| Association between sex and referral for catheterization† | ||||||
| Women vs Men | 358/4720 (7.58%) | 534/4246 (12.58%) | 0.57 (0.50–0.66) | <.001 | 0.75 (0.62–0.90) | 0.002 |
| Association between sex and revascularization‡ | ||||||
| Women vs Men | 124/358 (34.64%) | 286/534 (53.56%) | 0.46 (0.35–0.61) | <.001 | 0.73 (0.45–1.20) | 0.214 |
| Association between sex and medication use§ | ||||||
| Aspirin|| | ||||||
| Women vs Men | 322/462 (69.70%) | 480/598 (80.27%) | 0.57 (0.43–0.75) | <.001 | 0.78 (0.56–1.08) | 0.131 |
| Statin¶ | ||||||
| Women vs Men | 2072/3291 (62.96%) | 1937/2806 (69.03%) | 0.76 (0.69–0.85) | <.001 | 0.81 (0.73–0.91) | <.001 |
For each of the models presented in the table, we tested the interaction between sex and NIT modality with the given process of care outcome measure. None of the relationships between sex and each process of care measure were modified by NIT modality (all interaction p=NS).
Adjusted model for catheterization referral controls for NIT modality (CTA/stress test); NIT results (4-tier); BMI (kg/m2); age (standardized by sex); chest pain vs other as primary symptoms; chest pain typicality (typical, atypical, non-cardiac); and risk factors such as smoker (ever/never), diabetes, hypertension, history of peripheral artery or cerebrovascular disease, sedentary lifestyle, depression, family history of premature CAD, and dyslipidemia.
Adjusted model for revascularization controls for NIT modality (CTA/stress test); NIT results (4-tier); ICA results (positive/negative); BMI (kg/m2); age (standardized by sex); chest pain vs other as primary symptoms; chest pain typicality (typical, atypical, non-cardiac); and risk factors such as smoker (ever/never), diabetes, hypertension, history of peripheral artery or cerebrovascular disease, sedentary lifestyle, depression, family history of premature CAD, and dyslipidemia.
Medication use at 60-day visit. Adjusted models control for NIT modality (CTA/stress test); BMI (kg/m2); age (standardized by sex); chest pain vs other as primary symptoms; chest pain typicality (typical, atypical, non-cardiac); risk factors such as smoker (ever/never), diabetes, hypertension, history of peripheral artery or cerebrovascular disease, sedentary lifestyle, depression, family history of premature CAD, and dyslipidemia.
Includes N=1106 patients who had a history of stroke/TIA, peripheral arterial disease, or who had a positive CTA or catheterization prior to 60 day visit.
Includes N=6758 patients who had a history of dyslipidemia, diabetes, stroke/TIA, peripheral arterial disease, 10-year ASCVD risk ≥ 7.5%, or who had a positive CTA or catheterization prior to 60-day visit.
Of the subjects who underwent catheterization, a significantly smaller proportion of women compared with men had obstructive CAD (40.8% vs 60.9%, p<0.001) and fewer women underwent subsequent revascularization within 30 days (34.6% vs 53.6%, p<0.001) (Table 4). However, after adjustment for clinical factors, including presence of obstructive CAD on catheterization, the likelihood of referral for revascularization was not significantly different in women and men (adjusted OR [95%CI] 0.73 [0.45–1.20], p=0.21). This relationship was not modified by NIT modality (adjusted interaction p=0.74) or catheterization results (adjusted interaction p=0.62).
Of the patients with a history of dyslipidemia, stroke/TIA, peripheral arterial disease, or with a positive CTA or catheterization showing obstructive CAD, women were less likely than men to report statin use at a 60-day visit (adjusted OR 0.81 [0.73–0.91]; p<0.001). In contrast, there was no sex-based difference in likelihood of being on aspirin therapy among patients with history of stroke/TIA, peripheral arterial disease, or with a positive CTA or catheterization (adjusted OR 0.78 [0.56–1.08]; p=0.13) (Table 4).
Sex Differences in Outcomes after Noninvasive Testing
Over a median follow-up of 25 months, women had better outcomes than men both before and after adjustment for clinical factors and care, including catheterization results and revascularization (adjusted HR [95%CI] for composite outcome of death/MI/UAH: 0.74 [0.57–0.95], p=0.019) (Figure 2). This also held true for the secondary outcome of CV death/MI/UAH (0.73 [0.55–0.97], p=0.032), and was shy of statistical significance for CV death/MI (0.71 [0.49–1.02], p=0.064).
Figure 2:
Associations between patient sex (women vs men) and the primary outcome of all-cause death, myocardial infarction, or unstable angina in different subsets of the PROMISE population. (1): Adjusted model controls for NIT modality (CTA/stress test); NIT results (4-tier); ICA referral and results (positive/negative); referral for revascularization; and factors listed in (2) below. (2): Adjusted model controls for BMI (kg/m2); age (standardized by sex); chest pain vs other as primary symptoms; chest pain typicality (typical, atypical, non-cardiac); and risk factors such as smoker (ever/never), diabetes, hypertension, history of peripheral artery or cerebrovascular disease, sedentary lifestyle, depression, family history of premature CAD, and dyslipidemia.
Compared with men, women less often experienced the primary composite endpoint both among those who were referred for catheterization (8.9% vs 11.1%, adjusted HR [95% CI] 0.77 [0.49–1.21], p=0.26) and among those who were not (1.8% vs 2.5%, adjusted HR 0.75 [0.55–1.02], p=0.07; Figure 2). However, only when all patient groups were pooled together was a statistically significant difference in outcomes between women and men observed (0.74 [0.57–0.95], p=0.019). No difference in the primary outcome was observed among women and men who underwent revascularization (adjusted HR 1.02 [0.59–1.76], p=0.94).
Discussion
Many prior studies have reported differences in management of established CAD by sex.3,6,13 However, the increasing use of CTA as an NIT strategy may have impacted the management of women and men with suspected CAD. Our data from the PROMISE trial suggest that the large majority of patients of both sexes undergoing NIT have negative results — in women more than in men, and with stress testing more than with CTA. After accounting for differences in NIT results, women with stable symptoms concerning for ischemia were less likely to be referred for catheterization than men, and less likely to have obstructive CAD on catheterization once referred. However, among those referred for catheterization, women and men were similarly likely to undergo revascularization. Women were less likely than men to report statin therapy usage, even when indicated. Despite these differences, women were less likely to experience adverse cardiovascular outcomes than their male counterparts.
Our finding that the majority of individuals who underwent stress testing had negative results, with a significantly higher rate of negative tests in women than in men, has been observed in multiple prior studies of stress testing.14,15 We further show that with CTA, women continue to have higher rates of negative tests than their male counterparts. A lower referral rate for catheterization in women compared with men was first shown 4 decades ago in the stable angina population,1 and has since been confirmed by many,3–6 but not all,16–18 subsequent studies on the matter. The reasons for this difference were postulated to be related to interpretation of stress test findings given the known sex differences in the sensitivity and specificity of stress testing.7 Physicians may have been aware of the higher false-positive rates of exercise tolerance testing, nuclear stress testing, and echo stress testing in women,8 and may therefore have been less likely to refer women with a positive stress test for catheterization compared with men. However, our data indicate that even with CTA testing, which provides a visual, anatomic assessment of the amount of coronary atherosclerosis present and provides similar accuracy in both sexes,8 women were still less frequently referred for catheterization than men, after accounting for test results. This suggests that suspicion of an inaccurate non-invasive test cannot entirely explain the lower rate of catheterization referral in women. It is possible that the higher use of beta-blocker therapy in women vs men could have led to fewer anginal symptoms in women, and could therefore have contributed to the lower rate of referral for catheterization in women.
Nonetheless, women had better outcomes compared with men. This may be related to the higher rate of completely normal coronary anatomy seen in women compared with men. Because even mild non-obstructive disease is associated with greater CV morbidity than completely normal coronary arteries,19 the higher prevalence of this finding in men may account, at least in part, for the higher event rate in men than in women who did not undergo catheterization. This is also likely related to the overall lower cardiovascular risk of women compared with men in this study, as evidenced by the lower Framingham and ASCVD risk scores.
Among individuals who underwent catheterization, and specifically among those who underwent revascularization, the outcomes of women in our study were not significantly different from those of men. Similar cardiovascular event rates in women and men with documented CAD have previously been described,7 though a higher event rate in women in this group has also been demonstrated.6 Our data from the PROMISE trial indicate that once women were referred for catheterization, their management with revascularization as well as their cardiovascular outcomes were similar to men who were referred for catheterization. Statin therapy, on the other hand, was lower in women, which has been shown in multiple settings in the U.S.20, 21 This could be related to the lower overall ASCVD pooled cohort risk score noted in women in this study compared with men (median [25th, 75th percentile]: 8.8% [4.7%, 16.2%] vs 14.0% [8.5%, 22.5%], p=<0.001).
Our study has several strengths. PROMISE is the first large pragmatic comparative effectiveness trial of functional vs anatomic testing strategies in stable symptomatic outpatients, and because all decision-making after NIT was left up to the providers, it provides insight into current clinical practice. Second, the trial is uniquely able to address sex-based differences in the management and outcomes of patients with suspected CAD, since to our knowledge it includes the largest number of stable symptomatic women of any prospective trial of diagnostic testing to date.
Our study also has several caveats that should be considered when interpreting the results. Randomization was not stratified by patient sex; however, within each sex, the 2 testing arms were similar. Physician rationale for various management decisions was not collected, so we were unable to directly evaluate the reasons behind sex-based differences in patient management. Because less than 5% of our study population underwent coronary revascularization, this study likely lacked the power to detect a difference in the adjusted likelihood of revascularization between sexes. Although patients were followed for a median of >2 years, there were relatively few clinical endpoint events, limiting the ability to assess differences in outcomes by sex.
Conclusion
In the PROMISE trial population, women with stable symptoms concerning for ischemia had more normal and fewer abnormal NITs than men. Women with abnormalities on NIT were less likely to be referred for catheterization than men, regardless of whether they initially underwent stress testing or anatomic imaging with CTA, and they were less likely to receive statin therapy when indicated. Nonetheless, women had better cardiovascular outcomes than their male counterparts, perhaps related to the lower overall cardiovascular risk in women in this group. Thus, discrepancies in the management of women and men with stable angina still exist, but despite these, the outcomes of women with stable angina referred for NIT were not adversely affected compared with men. Sex-specific algorithms to determine which patients need to undergo NIT and how they should subsequently be managed are urgently needed.
Supplementary Material
Acknowledgments
This project was supported by grants R01HL098237, R01HL098236, R01HL98305, and R01HL098235 from the National Heart, Lung, and Blood Institute (NHLBI). The first author (N.J.P.) was supported by a National Institutes of Health T32 Grant (T32HL069749). The authors are solely responsible for the design and conduct of this study, all study analyses, the drafting and editing of the paper and its final contents. This paper does not necessarily represent the official views of NHLBI.
Disclosures
DBM reported receiving personal fees from Medtronic, CardioDx, and St. Jude Medical and grant support from Eli Lilly, Bristol-Myers Squibb, Gilead Sciences, AGA Medical, Merck, Oxygen Biotherapeutics, and AstraZeneca; MRP reported receiving grant support from Astra Zeneca, CSL, Heart Flow Technologies, Jansen, Johnson & Johnson, MAQUET, Medtronic, and the NHLBI; and serving on advisory boards for Astra Zeneca, Bayer, CSL, Genzyme Corp., Janssen, Medtronic, and Merck. UH reported receiving grant support from Siemens Healthcare and HeartFlow; PSD reported receiving grant support from HeartFlow and serves on a data and safety monitoring board for GE Healthcare. No other author reported relevant disclosures.
Footnotes
Clinical Trial Registration: ClinicalTrials.gov # NCT01174550
All statistical calculations were carried out using SAS version 9.4 (SAS Institute, Cary, North Carolina).
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Tobin JN, Wassertheil-Smoller S, Wexler JP, Steingart RM, Budner N, Lense L, Wachspress J. Sex bias in considering coronary bypass surgery. Ann Intern Med 1987;107:19–25. [DOI] [PubMed] [Google Scholar]
- 2.Bickell NA, Pieper KS, Lee KL, Mark DB, Glower DD, Pryor DB, Califf RM. Referral patterns for coronary artery disease treatment: Gender bias or good clinical judgment? Ann Intern Med 1992;116:791–797. [DOI] [PubMed] [Google Scholar]
- 3.Miller TD, Roger VL, Hodge DO, Hopfenspirger MR, Bailey KR, Gibbons RJ. Gender differences and temporal trends in clinical characteristics, stress test results and use of invasive procedures in patients undergoing evaluation for coronary artery disease. J Am Coll Cardiol 2001;38:690–697. [DOI] [PubMed] [Google Scholar]
- 4.Shaw LJ, Miller DD, Romeis JC, Kargl D, Younis LT, Chaitman BR. Gender differences in the noninvasive evaluation and management of patients with suspected coronary artery disease. Ann Intern Med 1994;120:559–566. [DOI] [PubMed] [Google Scholar]
- 5.Daugherty SL, Peterson PN, Magid DJ, Ho PM, Bondy J, Hokanson JE, Ross CA, Rumsfeld JS, Masoudi FA. The relationship between gender and clinical management after exercise stress testing. Am Heart J 2008;156:301–307. [DOI] [PubMed] [Google Scholar]
- 6.Daly C, Clemens F, Lopez Sendon JL, Tavazzi L, Boersma E, Danchin N, Delahaye F, Gitt A, Julian D, Mulcahy D, Ruzyllo W, Thygesen K, Verheugt F, Fox KM; Euro Heart Survey Investigators. Gender differences in the management and clinical outcome of stable angina. Circulation 2006;113:490–498. [DOI] [PubMed] [Google Scholar]
- 7.Roger VL, Jacobsen SJ, Weston SA, Pellikka PA, Miller TD, Bailey KR, Gersh BJ. Sex differences in evaluation and outcome after stress testing. Mayo Clin Proc 2002;77:638–645. [DOI] [PubMed] [Google Scholar]
- 8.Dolor RJ, Patel MR, Melloni C, Chatterjee R, McBroom AJ, Musty MD, Wing L, Coeytaux RR, Ross AK, Bastian LA, Anderson M, Kosinski AS, Sanders GD. Noninvasive technologies for the diagnosis of coronary artery disease in women. Rockville, MD: Agency for Healthcare Research and Quality; 2012. [PubMed] [Google Scholar]
- 9.Douglas PS, Hoffmann U, Patel MR, Mark DB, Al-Khalidi HR, Cavanaugh B, Cole J, Dolor RJ, Fordyce CB, Huang M, Khan MA, Kosinski AS, Krucoff MW, Malhotra V, Picard MH, Udelson JE, Velazquez EJ, Yow E, Cooper LS, Lee KL; PROMISE Investigators. Outcomes of anatomical versus functional testing for coronary artery disease. N Engl J Med 2015;372:1291–1300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Douglas PS, Hoffmann U, Lee KL, Mark DB, Al-Khalidi HR, Anstrom K, Dolor RJ, Kosinski A, Krucoff MW, Mudrick DW, Patel MR, Picard MH, Udelson JE, Velazquez EJ, Cooper L, PROMISE Investigators. Prospective multicenter imaging study for evaluation of chest pain: Rationale and design of the promise trial. Am Heart J 2014;167:796–803.e791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014;129(25 Suppl 2):S1–45. [DOI] [PubMed] [Google Scholar]
- 12.Hemal K, Pagidipati NJ, Coles A, Dolor RJ, Mark DB, Pellikka PA, Hoffmann U, Litwin SE, Daubert MA, Shah SH, Ariani K, Bullock-Palmer RP, Martinez B, Lee KL, Douglas PS. Sex differences in demographics, risk factors, presentation, and noninvasive testing in stable outpatients with suspected coronary artery disease: Insights from the PROMISE trial. JACC Cardiovasc Imag 2016;9:337–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Anand SS, Xie CC, Mehta S, Franzosi MG, Joyner C, Chrolavicius S, Fox KA, Yusuf S; CURE Investigators. Differences in the management and prognosis of women and men who suffer from acute coronary syndromes. J Am Coll Cardiol 2005;46:1845–1851. [DOI] [PubMed] [Google Scholar]
- 14.Shaw LJ, Vasey C, Sawada S, Rimmerman C, Marwick TH. Impact of gender on risk stratification by exercise and dobutamine stress echocardiography: Long-term mortality in 4234 women and 6898 men. Eur Heart J 2005;26:447–456. [DOI] [PubMed] [Google Scholar]
- 15.Lewis JF, Lin L, McGorray S, Pepine CJ, Doyle M, Edmundowicz D, Holubkov R, Pohost G, Reichek N, Rogers W, Sharaf BL, Sopko G, Merz CN. Dobutamine stress echocardiography in women with chest pain. Pilot phase data from the National Heart, Lung and Blood Institute Women’s Ischemia Syndrome Evaluation (WISE). J Am Coll Cardiol 1999;33:1462–1468. [DOI] [PubMed] [Google Scholar]
- 16.Wong Y, Rodwell A, Dawkins S, Livesey SA, Simpson IA. Sex differences in investigation results and treatment in subjects referred for investigation of chest pain. Heart 2001;85:149–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hachamovitch R, Berman DS, Kiat H, Bairey-Merz N, Cohen I, Cabico JA, Friedman JD, Germano G, Van Train KF, Diamond GA. Gender-related differences in clinical management after exercise nuclear testing. J Am Coll Cardiol 1995;26:1457–1464. [DOI] [PubMed] [Google Scholar]
- 18.Mark DB, Shaw LK, DeLong ER, Califf RM, Pryor DB. Absence of sex bias in the referral of patients for cardiac catheterization. N Engl J Med 1994;330:1101–1106. [DOI] [PubMed] [Google Scholar]
- 19.Maddox TM, Stanislawski MA, Grunwald GK, Bradley SM, Ho PM, Tsai TT, Patel MR, Sandhu A, Valle J, Magid DJ, Leon B, Bhatt DL, Fihn SD, Rumsfeld JS. Nonobstructive coronary artery disease and risk of myocardial infarction. JAMA 2014;312:1754–1763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Salami JA, Warraich H, Valero-Elizondo J, Spatz ES, Desai NR, Rana JS, Virani SS, Blankstein R, Khera A, Blaha MJ, Blumenthal RS, Lloyd-Jones D, Nasir K. National trends in statin use and expenditures in the US adult population from 2002 to 2013: Insights from the medical expenditure panel survey. JAMA Cardiol 2017;2:56–65. [DOI] [PubMed] [Google Scholar]
- 21.Rodriguez F, Olufade TO, Ramey DR, Friedman HS, Navaratnam P, Heithoff K, Foody JM. Gender disparities in lipid-lowering therapy in cardiovascular disease: Insights from a managed care population. J Women’s Health (Larchmt). 2016;25:697–706. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.