Abstract
Use of recommended screening tests can reduce new colorectal cancers (CRC) and deaths, but screening uptake is suboptimal in the United States (U.S.). The Centers for Disease Control and Prevention (CDC) funded a second round of the Colorectal Cancer Control Program (CRCCP) in 2015 to increase screening rates among individuals aged 50–75 years. The 30 state, university, and tribal awardees supported by the CRCCP implement a range of multicomponent interventions targeting health systems that have low CRC screening uptake, including low-income and minority populations. CDC invited a select subset of 16 CRCCP awardees to form a learning laboratory with the goal of performing targeted evaluations to identify optimal approaches to scale-up interventions to increase uptake of CRC screening among vulnerable populations. This commentary provides an overview of the CRCCP learning laboratory, presents findings from the implementation of multicomponent interventions at four FQHCs participating in the learning laboratory, and summarizes key lessons learned on intervention implementation approaches. Lessons learned can support future program implementation to ensure scalability and sustainability of the interventions as well as guide future implementation science and evaluation studies conducted by the CRCCP learning laboratory.
Keywords: Colorectal cancer screening, Learning laboratory, Implementation economics, Implementation science, Economic evaluation, Cost-effectiveness
Introduction
Screening for colorectal cancer (CRC) and subsequent removal of polyps has been shown to prevent CRC [1]. However, uptake for CRC screening is suboptimal with 67.3% of the United States population being up-to-date with CRC screening recommended by the United States Preventive Services Task Force [2]. Screening uptake is lower at federally qualified health centers (FQHCs) where only about 40% of the age appropriate population has been screened [3]. With limited resources at FQHCs, finding cost-effective interventions to improve CRC screening that can be scaled up to reduce burden of the disease is paramount.
In 2009 the Centers for Disease Control and Prevention (CDC) launched the Colorectal Cancer Control program (CRCCP) with the purpose of increasing CRC screening uptake among individuals aged 50–75 years through provision of screening services and promotion of screening [4]. In 2015 the emphasis of the CRCCP shifted from screening to implementation of evidence-based interventions (EBIs) recommended in The Community Guide that effectively increase CRC screening in health systems [5]. EBIs include patient and provider reminder systems, provider assessment and feedback, and reduction of structural barriers. Awardees are required to implement at least 2 EBIs; they can also implement support activities (SAs) such as small media, patient navigation, and health information technology.
Currently, CDC supports 30 awardees including 23 state health departments, six universities, and one American Indian tribal organization. Each CRCCP awardee collaborates with health systems and clinics serving medically underserved populations, including those with disproportionately lower screening rates than their state average. CDC provides oversight and technical assistance to awardees. To assess the CRCCP’s impact, awardees report baseline clinic-level data at the time a clinic is recruited and annually thereafter, allowing for longitudinal assessment. Clinic-level CRC screening rate is the primary outcome of interest.
The purpose of this commentary is to describe the CRCCP learning laboratory and present findings from the implementation of multicomponent interventions at four participating FQHCs. The CRCCP learning laboratory brings together a group of awardees and their partner health systems to better understand the CRC intervention implementation process and to identify lessons learned to implement cost-effective interventions in the future.
CRCCP Learning Laboratory
The CRCCP provides a unique opportunity to evaluate the role of multicomponent interventions (i.e., multiple EBIs and SAs) to increase CRC screening in the real-world community and organizational settings. CDC initiated the CRCCP learning laboratory (“learning laboratory”) to systematically evaluate the implementation processes, including related barriers and facilitators, and assess effectiveness and cost-effectiveness of the interventions to inform future scale-up of the interventions. Selected CRCCP programs and their implementation partners (mostly clinics) were invited to participate in the learning laboratory based on availability of high-quality data, willingness to collaborate with members of CDC’s learning laboratory, and leadership commitment to ensure adequate follow-up to track outcomes (i.e., CRC screening rates).
The awardees engaged in the learning laboratory are located in all geographic regions of the United States (Fig. 1). The majority of the awardees partner with FQHCs, often multiple FQHCs in their states. Across the U.S., FQHCs are located in both rural and urban areas.
Fig. 1.
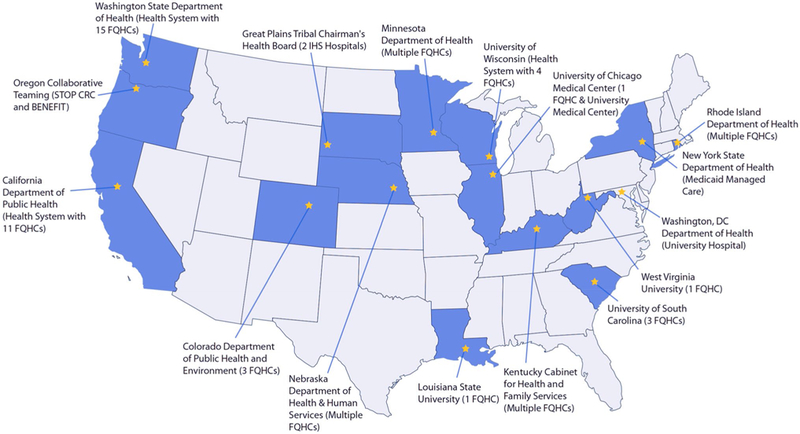
Awardees and health system partners participating in the Colorectal Cancer Control Program learning laboratory
The types and mix of EBIs/SAs implemented vary across clinics. Awardees work with their clinic partners to select and implement EBIs and SAs, almost always implementing multicomponent interventions, including provider reminders and patient reminders. A list and description of EBIs and SAs is provided in Table 1 [6]. During program year 1, awardees provided resources to implement new or enhanced EBIs in 95.2% of partnering clinics [6]. Some awardees have integrated their CRCCP with existing cancer programs, such as the CDC-funded National Breast and Cervical Cancer Early Detection Program (NBCCEDP) and with other chronic disease programs, such as ones addressing hypertension, diabetes, and tobacco use.
Table 1.
Evidence-based interventions (EBIs) and supporting activities (SAs) Source: DeGroff et al. [6]
| Name | Definitiona |
|---|---|
| Evidence-based interventions | |
| Patient reminders | Patient reminders or recalls are textual (letter, postcard, e-mail) or telephone messages advising people that they are due (reminder) or overdue (recall) for screening. Reminder messages might be general to address an overall priority population or tailored to specific individuals |
| Provider reminders | Reminders inform healthcare providers it is time for a Patient’s cancer screening test (reminder) or that the Patient is overdue for screening (recall). The reminders can be provided in different ways, such as Patient charts or by e-mail |
| Provider assessment and feedback | Provider assessment and feedback interventions both evaluate provider performance in offering and/or delivering screening to patients (assessment) and present providers with information about their performance in providing screening services (feedback). Feedback might describe the performance of a group of providers or an individual provider, and might be compared with a goal or standard |
| Reducing structural barriers | Structural barriers are noneconomic burdens or obstacles that impede access to screening. Interventions designed to reduce these barriers might facilitate access to cancer screening services by reducing time or distance between service delivery settings and target populations, modifying hours of service to meet patient needs, offering services in alternative or non-clinical settings or eliminating or simplifying administrative procedures and other obstacles |
| Supporting activities | |
| Small media | Small media include videos and printed materials such as letters, brochures, and newsletters. These materials can be used to inform and motivate people to be screened for cancer. They can provide information tailored to specific individuals or targeted to general audiences |
| Patient navigation | Patient navigation is a strategy aimed at reducing disparities by helping patients overcome barriers to healthcare. For purposes of the CRCCP, patient navigation is defined as individualized assistance offered to patients to help overcome healthcare system barriers and facilitate timely access to quality screening and follow-up as well as initiation of treatment services for persons diagnosed with cancer. Patient navigation includes assessment of Patient barriers, Patient education, resolution of barriers, and Patient tracking and follow-up. Patient navigators might be professional (e.g., nurse) or lay workers |
| Professional development/provider education | Professional development/provider education are interventions directed at healthcare staff and providers to increase their knowledge as well as to change attitudes and practices in addressing cancer screening. Activities might include distribution of provider education materials, including screening recommendations, and/or continuing medical education opportunities |
| Community health workers | Community health workers are lay health educators with a deep understanding of the community and are often from the community being served. Community health workers work in community settings, in collaboration with a health promotion program, clinic, or hospital, to educate people about cancer screening, promote cancer screening, and provide peer support to people referred to cancer screening |
Based on Community Guide definitions
The learning laboratory partners use a mixed-methods approach to conduct evaluations of the interventions and their impacts. The approach includes the collection of process measures, screening outcomes, cost and resource use data, and qualitative interviews to learn more about the design of programs and implementation procedures. To provide comprehensive support to awardees and their partners to evaluate the interventions being implemented, CDC works with a selected group of four or five health systems participating in the learning laboratory for a specified period of time, and then transitions to support another group.
Research Triangle Institute (RTI) International serves as the CRCCP learning laboratory Coordinating Center for the CDC’s CRCCP awardees (Fig. 1). In addition to clinic-level data, CDC has developed standardized metrics and data collection tools to collect cost data for use in the evaluation. Cohesion and coordination between learning laboratory partners is fostered through webinars, in-person meetings, and regular conference calls. These interactions enhance communication across all stakeholders. The learning laboratory provides awardees with feedback on lessons learned on a continual, real-time basis. Furthermore, in-depth case studies are performed to obtain contextual details on facilitators and barriers. To reach a broader audience of stakeholders, findings from the learning laboratory are shared through peer-reviewed journals, conference presentations, and infographics.
Data collection and analysis
All partners collect data using standardized approaches. They report on the screening uptake at baseline and during the implementation period. The number of individuals up-to-date with screening (numerator) and the total population recommended for CRC screening (denominator) during both the baseline and intervention periods are reported based on guidelines established by the CRCCP [7]. The baseline screening uptake percentages are reported for a 12-month period prior to implementation; the same 12-month measurement period is used to then report screening uptake percentages annually thereafter. Implementation periods range from 12 to 36 months. To ensure that high-quality data are available for reporting, CRCCP awardees received support and technical assistance.
Resource use data to implement the intervention are collected at the clinic, health system, and awardee level using standardized methods previously developed for economic evaluation of CRC programs and tailored to reflect the interventions implemented by the CRCCP awardees [8, 9]. Cost incurred to develop the interventions, to implement the interventions (“implementation costs”), as well as support needed for program evaluation, administration, and data quality assessment are collected from each program. For this analysis, we only report the implementation costs for the awardee, health system and clinic as they reflect the resources that are likely required to support the interventions in subsequent years. To assess the impact of the interventions, we report the screening at baseline and uptake during the implementation period, additional number of individuals screened (the difference in the number of individuals screened at implementation compared to baseline), implementation cost of the intervention, and the incremental intervention cost per person successfully screened (calculated utilizing implementation costs and the number of additional persons screened).
Quantitative Findings from Three Selected CRCCP Awardee Programs
We report results from our work with three awardees and their FQHC partners: Colorado Department of Health & Environment (CDPHE) and two of its FQHC partners (Health Systems 1 and 2); Washington State Department of Health and one FQHC partner (Health System 3); and West Virginia University (WVU) and one FQHC partner (Health System 4). These awardees and partners were selected to serve as examples as they were all among the first set of participants that conducted in-depth analysis and implemented interventions to increase CRC screening in the FQHC settings.
In Table 2 we present the clinic and patient characteristics, costs and screening uptake of the four health systems participating in the cost-effectiveness analysis; all are FQHCs. The number of patients aged 50–75 ranged from 3,012 in WVU to 10,933 in CO. More than half of the patients were female and 16% or less of patients were uninsured. The majority of patients were White (44.1–98.0%).
Table 2.
Clinic and patient characteristics, costs, and screening uptake by health system
| Awardee | Colorado Department of Public Health & Environment | Washington State Department of Health |
West Virginia University | |
|---|---|---|---|---|
| Partner (# of clinic sites) | Health System 1 (9) | Health System 2 (4) | Health System 3 (9) | Health System 4(1) |
| Patients age 50–75 years (N) | 10,933 | 6,421 | 15,516 | 3,012 |
| Female (%) | 64.8 | 72.9 | 59.7 | 52.0 |
| Uninsured (%) | 12.0 | 11.5 | 15.9 | 4.0 |
| Race and ethnicity (%) | ||||
| Non-Hispanic White | 55.2 | 61.8 | 44.1 | 98.0 |
| Non-Hispanic Black | 1.5 | 1.8 | 12.3 | 0.0 |
| Hispanic | 38.7 | 35.1 | NR | NR |
| Other/unknown | 4.6 | 1.3 | 43.6 | 2 |
| Evidence-based interventions implemented | ||||
| Patient reminder systems | ✓ | ✓ | ✓ | ✓ |
| Provider reminder systems | ✓ | ✓ | ||
| Provider assessment and feedback | ✓ | ✓ | ✓ | ✓ |
| Reduction of structural barriers | ✓ | |||
| Intervention evaluated | Multicomponent interventions implemented over a 2-year period |
Multicomponent interventions implemented over a 3-year period |
Mailed FIT and outreach activities to increase FIT uptake over a 12-month period |
Multicomponent interventions implemented over a 12-month period |
|---|---|---|---|---|
| Time period | ||||
| Baseline | 7/2012–6/2013 | 7/2013–6/2014 | 7/2014–6/2015 | 11/2015–12/2015 |
| Implementation | 7/2013–6/2015 | 7/2014–6/2017 | 7/2015–6/2016 | 1/2016–12/2016 |
| Screening uptake (%) | ||||
| Baseline | 21.1 | 25.7 | 51.2 | 38.3 |
| Implementationa | 39.2 | 35.4 | 58.3 | 57.2 |
| Change in screening uptake | 18.1 | 9.7 | 7.1 | 18.9 |
| Intervention implementation phase cost ($) | $60,224 | $27,497 | $30,148 | $13,278 |
| Additional persons screened (#) | 2,533b | 943c | 1,607 | 332 |
| Based on changes between baseline and implementation |
Based on changes between baseline and implementation |
Based on number of individu- als who returned FIT kitd |
Based on changes between baseline and implementation |
|
|---|---|---|---|---|
| Incremental intervention cost per person successfully screened ($) | $23.78 | $29.16 | $18.76 | $40.00 |
NR not reported
Screening uptake was assessed for the last 12-month period of implementation
The calculation for the additional person screened was for the 2-year period
The calculation for the additional person screened was for the 3-year period
The fecal immunochemical test (FIT) return rate for Washington was 31%
In addition, we summarize the EBIs and SAs implemented in each health system in Table 2. Patient and provider reminder systems as well as provider assessment and feedback were implemented in Health System 1 while Health System 2 implemented a patient reminder system and provider assessment and feedback. CRC interventions in these two health systems are integrated with interventions for other conditions (e.g., breast and cervical cancer screening, hypertension control, and diabetes control) to maximize resources in addressing a comprehensive set of chronic conditions. Health System 3 implemented all four of the EBIs in its nine clinic sites, as well as small media and health information technology. Health System 4 implemented patient reminders, provider assessment and feedback, and small media.
We also present in Table 2 the screening uptake for four FQHCs for the baseline and implementation periods, the implementation costs and the incremental cost per person successfully screened. Screening uptake increased across all the sites during the implementation period, ranging from 7.1 to 18.9 % points. Implementation costs varied from $13,278 to $60,224 but it is important to note that the implementation period differed across the health systems (12–36 months). The lowest incremental implementation cost per person successfully screened was $18.76 while the highest was $40.
Lessons Learned for Future CRC Screening Program Implementation
Results indicated that the three awardees analyzed in this study successfully partnered with health systems to implement EBIs/SAs and that screening uptake increased during the implementation period. Without concurrent comparison groups, we were unable to determine the extent to which the interventions contributed to these increases; however, when compared to CRC screening rates reported across all FQHCs nationally, increases for these four health systems were greater. The national average CRC screening rate for FQHCs increased from 34.5% in 2014 to 39.9% in 2016, an increase of 5.4 % points [10]. Additionally, for Health Systems 3 and 4, we were able to track process measures which provide additional confidence that the interventions were having the intended effect. In Health System 3, the mailed fecal immunochemical test (FIT) program had a 31% return rate which provides clear evidence that this approach can work to increase screening uptake among a diverse group of low-income individuals. In Health System 4, screening rates were tracked at the provider level to assess the impact of the patient assessment and feedback intervention. These rates showed consistent improvements over the period of the intervention.
The implementation cost per person successfully screened provides CDC and CRC programs with an estimate of the resources required to implement multicomponent interventions. As in previous evaluations of the cost of cancer screening programs [11, 12], there appears to be some economies of scale associated with the cost of implementing the interventions. Specifically, Health Systems with larger numbers of patients were likely able to distribute fixed costs associated with the interventions across more patients. In other words, the interventions are effective in all settings but may be more costly to implement in smaller clinics based on their number of patients. These findings will be confirmed in future studies, but they suggest smaller clinics may require incentives or other support to implement CRC interventions when the cost per person is prohibitive.
The evaluation thus far of three awardees and the ongoing assessment of the participants in the CRCCP learning laboratory offer multiple lessons for future program implementation to ensure cost-effectiveness and sustainability of the interventions. We summarize these findings below.
-
(1)
Implementation sites often differ in the types and combination of EBI(s) and SA(s) implemented, how the EBI(s) and SA(s) are implemented, and the amount of resources utilized for development and implementation. Therefore, comparison across programs should include an in-depth description or mapping of intervention processes to understand how programs are similar and how they differ to support future implementation efforts.
-
(2)
Impact of EBI/SA implementation may take time to be realized and therefore, the follow-up period for measurement in research studies should be sufficiently long (e.g., at least 12 months) to adequately assess effectiveness.
-
(3)
FQHCs, especially stand-alone health centers, face substantial challenges in tracking the completion of diagnostic colonoscopy referrals. Standards of practices for the health systems could be defined and enhanced to ensure that endoscopy findings are consistently reported back to the primary care physician and recorded in the patient record to ensure appropriate and complete follow-up and record the patient’s recommended screening interval.
-
(4)
Integrated delivery of EBIs, SAs, and other interventions for multiple cancer screenings and other chronic conditions is a promising approach, but additional work is required to evaluate outcomes and cost efficiency.
-
(5)
Integrating CRC interventions into the standard operating procedures and work flow processes of health systems, when possible, will contribute to sustainability (e.g., incorporating client reminders into the electronic health record system so that reminders are automated).
Through the CRCCP learning laboratory, CDC will continue to identify appropriate intervention combination and factors influencing intervention selection, as they are essential to foster sustainability and broad scale-up of evidence-based interventions. CDC, awardees, and implementation partners will employ multi-modal methods, including process and outcome evaluation, cost-effectiveness analysis, and qualitative case studies, to improve understanding of implementation of multicomponent interventions, including those targeted at integrated delivery of screening for multiple cancers. The learning laboratory will also focus on efforts to identify optimal approaches to track diagnostic colonoscopy completion rates following positive FIT tests. Finally, we will evaluate alternative payment methods that are used to incentivize health systems to increase CRC screening uptake. An advantage of having the learning laboratory is the ability to work over several years with the same group of awardees to systematically build on prior analysis and findings and to continually explore appropriate approaches to implement and scale-up EBIs and SAs. Furthermore, it will also be important to assess the generalizability of the findings from the learning laboratory partner organizations and therefore we hope to be able to evaluate the implementation of interventions shown to be effective in non-partner organizations to understand reproducibility of the results.
Acknowledgments
Funding Funding support for Sujha Subramanian and Sonja Hoover was provided by the Centers for Disease Control and Prevention (CDC) (Contract No. 200-2014-61263 Task 4, to RTI International). The provision of data by awardees was supported through funding under a cooperative agreement (DP15-1502) with CDC.
The findings and conclusions in this manuscript are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- 1.United States Preventive Services Task Force (2016) Screening for colorectal cancer: US Preventive Services Task Force recommendation statement. JAMA 315(23):2564–2575. 10.1001/jama.2016.5989 [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention (CDC) (2017) Behavioral Risk Factor Surveillance System (BRFSS). http://www.cdc.gov/brfss/index.html. Accessed 18 Dec 2017 [Google Scholar]
- 3.Health Resources & Services Administration (2016) National Health Center Data. https://bphc.hrsa.gov/uds/datacenter.aspx?q=t6b&year=2016&state=. Accessed 26 Jan 2018
- 4.Seeff LC, DeGroff A, Joseph DA, Royalty J, Tangka FK, Nadel MR, Plescia M (2013) Moving forward: using the experience of the CDCs’ Colorectal Cancer Screening Demonstration Program to guide future colorectal cancer programming efforts. Cancer 119(Suppl 15):2940–2946. 10.1002/cncr.28155 [DOI] [PubMed] [Google Scholar]
- 5.Community Preventive Services Task Force (2016) The guide to community preventive services. Centers for Disease Control and Prevention, Community Preventive Services Task Force, Atlanta: https://www.thecommunityguide.org/findings/cancer-screening-multicomponent-interventions-colorectal-cancer. Accessed 6 Oct 2017 [Google Scholar]
- 6.DeGroff A, Sharma K, Satsangi A, Kenney K, Joseph D, Ross K, Leadbetter S, Helsel B, Kammerer B, Firth R, Rockwell T, Short W, Tangka F, Wong F, Richardson L (2018) Implementing evidence-based interventions in U.S. Healthcare Systems to increase colorectal cancer screening: year 1 results of the CDC Colorectal Cancer Control Program. Prev Chronic Dis (Paper Under Review) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention (2016) Guidance for measuring colorectal cancer (CRC) screening rates in health system clinics. US Department of Health and Human Services, Atlanta: https://www.cdc.gov/cancer/crccp/pdf/Guidance_Measuring_CRC_Screening_Rates.pdf [Google Scholar]
- 8.Subramanian S, Tangka F, Hoover S, Royalty J, DeGroff A, Joseph D (2017) Costs of colorectal cancer screening provision in CDC’s Colorectal Cancer Control Program: comparisons of colonoscopy and FOBT/FIT based screening. Eval Program Plan 62:73–80. 10.1016/j.evalprogplan.2017.02.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tangka F, Subramanian S, Hoover S, Royalty J, Joseph K, DeGroff A, Joseph D, Chattopadhyay S (2017) Costs of promoting cancer screening: evidence from CDC’s Colorectal Cancer Control Program (CRCCP). Eval Program Plan 62:67–72. 10.1016/j.evalprogplan.2016.12.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Health Resources and Services Administration (2018) UDS data comparison. https://bphc.hrsa.gov/uds/datacenter.aspx. Accessed on 7 Jan 2018
- 11.Subramanian S, Tangka F, Hoover S, Cole Beebe ME, DeGroff A, Royalty J et al. (2013) Costs of planning and implementing federally funded colorectal cancer screening. Cancer 119(Suppl.15):2855–2862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Trogdon JG, Ekwueme DU, Subramanian S, Crouse W (2014) Economies of scale in federally-funded, state-organized public health programs: results from the National Breast and Cervical Cancer Early Detection Programs. Health Care Manag Sci 17(4):321–330 [DOI] [PMC free article] [PubMed] [Google Scholar]


