Abstract
Objective:
Acute heart failure (AHF) is a life-threatening clinical syndrome characterized by rapid onset of heart failure (HF) symptoms and signs and requires urgent therapy. The aim of the present study was to evaluate the overall clinical characteristics, management, and in-hospital outcomes of hospitalized patients with AHF in a large sample of Turkish population.
Methods:
The Journey HF-TR study is a cross-sectional, multicenter, non-invasive and observational trial. Patients who were hospitalized with a diagnosis of AHF in the intensive care unit (ICU)/coronary care unit and cardiology wards between September 2015 and September 2016 were included in our study.
Results:
A total of 1606 (male: 57.2%, mean age: 67.8±13 years) patients who were diagnosed with AHF were enrolled in the study. Seventeen percent of the patients were admitted to the hospital with a diagnosis of new onset AHF. Hypertension (67%) and coronary artery disease (CAD) (59.6%) were the most frequent underlying diseases. Acute coronary syndrome accompanying HF (14.7%), infection (29.3%), arrhythmia (25.1%), renal dysfunction (23%), and non-compliance with medication (23.8%) were the precipitating factors. The median length of stay in the ICU was 3 days (interquartile range, IQR 1–72) and 7 days (IQR 1–72) for in-hospital journey. The guideline recommended medications were less likely used in our patient population (<73%) before admission and were similar to European and US registers at discharge. The in-hospital mortality rate was 7.6%. Hypertension and CAD were the most frequent underlying diseases in our population similar to other European surveys. Although our study population was younger than other registers, in-hospital mortality was high.
Conclusion:
Analyses of such real-world data will help to prepare a national database and distinctive diagnosis and treatment algorithms and to provide observing compliance with the current European Society of Cardiology guidelines for more effective management of HF.
Keywords: heart failure, length of stay, Turkey/national database, acute heart failure, mortality
Introduction
Heart failure (HF) is one of the most important causes of morbidity and mortality worldwide (1). Its prevalence is 0.4% to 2% in the general European population (2), and 5 million Americans with chronic HF are mostly attributable to inpatient hospitalization (3). Acute exacerbation of chronic HF is a life-threatening clinical syndrome characterized by rapid onset of HF symptoms and signs and requires urgent therapy. Patients with acute HF (AHF) have poor short- and long-term prognoses. In-hospital mortality rates are high in patients with AHF despite medical therapy and remains high after discharge (4).
Surveys and registries provide valuable information regarding the epidemiology, outcomes of the real world, and better understanding of medical practice in this clinical condition (5–8). However, to our knowledge, there are no published national data on the management of hospitalized patients with AHF in a large sample of Turkish population.
In the present study, we aimed to evaluate the overall clinical characteristics, management, and in-hospital outcomes [from intensive care unit (ICU) admission to discharge] of hospitalized patients with AHF in a Turkish population.
Methods
The Journey HF-TR study is a cross-sectional, multicenter, non-invasive and observational trial that was conducted in the ICU/coronary care unit (CCU) and cardiology wards. We enrolled a total of 1606 patients in 37 centers in seven geographical regions in Turkey. The study centers were designed to represent the 12 territorial units of Turkey, accepted by the National Statistics Unit. Patients who were hospitalized with a diagnosis of AHF in the ICU/CCU of a participating center between September 2015 and September 2016 were included in our study. Acute decompensated chronic HF (ADCHF) was defined as the worsening of HF in patients with a previous diagnosis or hospitalization for HF. De novo AHF was defined as AHF in patients with no history of HF. Patients were classified by the current European Society of Cardiology (ESC) guidelines on AHF as decompensated HF, cardiogenic shock, pulmonary edema, hypertensive HF, and right ventricular HF (1, 6). The inclusion criteria were patients >18 years old, hospitalization with AHF, and providing an informed consent to participate in the study. The exclusion criteria were patients <18 years old and who do not want to provide an informed consent. Demographic and clinical characteristics, clinical history, symptoms and signs, initial emergency department evaluation, and subsequent inpatient management of patients were recorded. The most recent echocardiographic data and laboratory results were collected. Complications, length of stay (LOS), and in-hospital mortality rates were also recorded. Cardiorenal syndrome is defined as disorders of the heart and kidneys whereby acute or chronic dysfunction in one organ may induce acute or chronic dysfunction of the other. We accepted the infection as the cause of worsening of HF if there were signs of infection (fever, increase C-reactive protein, leukocytosis, and infectious focus). The Ethics Committee of the İstanbul Haydarpaşa Numune Training and Research Hospital approved the study.
Statistical analysis
Continuous variables are expressed as mean±standard deviation or as median and interquartile range (IQR). Categorical variables are presented as percentages (%) and χ2 test. The Kolmogorov–Smirnov test was used to identify the normal distribution of variables. Continuous variables were compared by the t-test if variable is normally distributed or the Mann–Whitney U test if it is non-normally distributed. A p value <0.05 was considered as statically significant. All tests were two-sided. The SPSS software for windows, version 22.0 was used for statistical analyses.
Results
Patient’s demographic and baseline characteristic
Between September 2015 and September 2016, 1606 (male: 57.2%, mean age: 67.8±13 years) patients who were diagnosed with AHF in 37 centers in seven geographical regions in Turkey were enrolled in the present study. Hypertension (67%), coronary artery disease (CAD) (59.6%), and diabetes (41.9%) were the most frequent underlying diseases. Anemia (using the World Health Organization definition: hemoglobin (Hb) <13.0 g/dL for males and Hb <12.0 g/dL for females) was detected in 48.1% of the patients. The prevalence of anemia is 2.7% in New York Heart Association (NYHA) class I, 18.5% in NYHA class II, 49.1% in NYHA class III, and 29.7% in NYHA IV (p=0.004). Chronic kidney disease [defined as glomerular filtration rate (GFR) <60 mL/min/1.73 m2] was detected in 28.2% of the patients. The mean GFR and Hb were 49.3±30.6 mL/min/1.73 m2 and 12.1±2.1 g/dL, respectively. The most frequent arrhythmia was atrial fibrillation (39% total, 35.3% permanent, and 3.7% paroxysmal AF). Table 1 shows the patients’ characteristics and co-morbidities.
Table 1.
Demographic, concomitant conditions, and precipitating factors
| Characteristics | Total (n) | Total (%) |
|---|---|---|
| Age (year), mean±SD | 67.8 (13.2) | |
| Male | 918 | 57.2 |
| Concomitant chronic conditions | ||
| Coronary artery disease | 957 | 59.6 |
| Hypertension | 1076 | 67 |
| Diabetes mellitus | 673 | 41.9 |
| Atrial fibrillation | 626 | 39 |
| Previous stroke or TIA | 177 | 11 |
| Renal failure | 453 | 28.2 |
| Anemia | 772 | 48.1 |
| Venous thromboembolism | 74 | 4.6 |
| Peripheral artery diseases | 103 | 6.4 |
| Depression | 273 | 17 |
| Ca ncer | 156 | 9.7 |
| Precipitating factors | ||
| Acute coronary syndrome | 236 | 14.7 |
| Arrhythmia | 403 | 25.1 |
| Infection | 471 | 29.3 |
| Non-compliance with therapy | 382 | 23.8 |
TIA - transient ischemic attack; SD - standard deviation
Clinical presentation, diagnosis, precipitant factors, and medications of patients at ICU admission
Seventeen percent of the patients were admitted to the hospital with a diagnosis of new onset AHF (de novo AHF), and 83% of the patients were admitted with a diagnosis of ADCHF (Fig. 1). The major symptoms include dyspnea on rest (n=1135, 70.7%), dyspnea on exercise (n=1501, 93.5%), orthopnea (n=1236, 77%), paroxysmal nocturnal dyspnea (n=978, 60.9%), angina (n=419, 26.1%), anxiety (n=775, 48.3%), and fatigue (n=1353, 84.3%). On physical examination, crackles on lung auscultation (n=1143, 71.2%), S3 gallop (n=772, 48.1%), elevated jugular venous pressure (n=565, 35.2%), abdominal distention and ascites (n=457, 28.5%), hepatojugular reflux (n=504, 31.4%), and peripheral edema (n=1061, 66.1%) were revealed. The average systolic blood pressure was 127.6±30.8 mm Hg, the average heart rate was 93.9±23.6 bpm, and the average oxygen saturation was 90±9.1% at admission.
Figure 1.
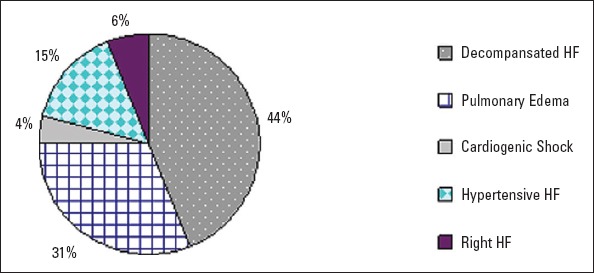
Distribution of all patients by clinical classification of AHF
Acute coronary syndrome accompanying HF (14.7%), infection (29.3%), arrhythmia (25.1%), renal dysfunction (23%), and non-compliance with medication (23.8%) were the precipitating factors. Time to clinical worsening was >1 month in 31.2% of the patients and <1 month in 68.8% of the patients.
Electrocardiography at admission was sinus rhythm in 59.5%, AF or atrial flutter in 35.3%, and pace rhythm in 5.2%. Left bundle branch block was revealed in 330 (20.5%) patients. The mean QRS duration was 106.5±36.2 ms.
All patients had chest X-ray: cardiomegaly (cardiothoracic ratio >50%) in 76.3%, alveolar edema in 42.3%, pulmonary congestion in 65.1%, and pleural effusion in 51.1%. Biomarkers were used in 41% of the patients at admission for diagnosis. The mean brain natriuretic peptide level was 8124.4±1691 pg/ml. Echocardiography was available in 92% of the patients and was performed at an average of 3 days after admission. The mean ejection fraction (EF) was 32.7±14.1%. Most of the patients (64%) had EF lower than 40% (defined as HF with reduced EF). The rest of the patients had HF with mid-range EF (19%) and HF with preserved EF (17%). The moderate-to-severe mitral regurgitation was the most common valvular disease (52%), and tricuspid insufficiency was the second most prevalent valve disease (49%). Pulmonary hypertension (defined as systolic pulmonary artery pressure >45 mm Hg) was detected in 59% of the patients.
Acetylsalicylic acid 61.8%, renin–angiotensin–aldosterone system blockers 62.1%, beta-blocker 72.5%, diuretic 71.2%, mineralocorticoid receptor antagonist (MRA) 38.6%, dihydropyridine calcium channel blocker 12.1%, digoxin 20.7%, amiodarone 6.7%, oral nitrate 17.5%, oral anti-diabetic 20.7%, insulin 19.9%, statin 24.7%, and ivabradine 6.7% were medications used prior to hospital admission.
Intravenous (i.v.) diuretic therapy (by bolus or infusion route) was administered to 91.2% of all patients at hospitalization. The diuretic infusion dosage after bolus was ≥1 g/day in 3.1% of the patients. The mean i.v. diuretic therapy duration was 4.5±4.8 days. The daily salt intake was restricted to 2.4±1.1 g, and fluid intake was 1.6±0.5 l/day.
Time passed from admission to initiation of i.v. diuretic therapy was <10 min in 25.5% of the patients, 10–29 min in 23.7% of the patients, and >30 min in 50.8% of the patients. Thirty percent of the patients had vasodilator therapy, and 19.5% had inotropic support. Of the patients, 16.4% were treated by non-invasive ventilation, and invasive mechanical ventilation was required for 7.8% at admission. Ultrafiltration and/or hemodialysis was necessary in 5.2% of the patients. The median LOS in the ICU was 3 days (IQR 1–72) 4 days (IQR 1–62) in the general or cardiology ward. The in-hospital mortality rate was 7.6%.
Clinical presentation and medications at discharge
Guideline-recommended drugs were prescribed more at discharge: diuretics (71%–81%), angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers (62%–81%), beta-blocker (73%–87%), and MRAs (39%–60%). Figure 2 shows the rates of evidence base medication of HF on admission and at discharge. The implanted cardiac device therapy (20: pacemakers, 47: cardiac resynchronization therapy implantable cardioverter defibrillator, and 32: cardiac resynchronization therapy pacemaker) was performed in 99 patients during hospitalization.
Figure 2.
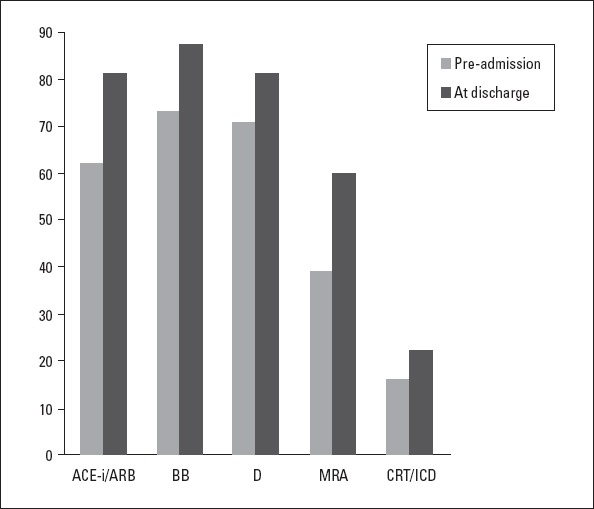
Medications prescribed before admission to the hospital and at discharge
The average heart rate and systolic and diastolic blood pressure were 72.7±22.1 bpm and 108.6±30.7 mm Hg and 62.8±30.4 mm Hg at discharge, respectively. The heart rate was >70 bpm in 58.1% of the patients at discharge. The mean weight difference between admission and discharge was 5.5±8.7 kg. The mean GFR was 58.8±26.5 mL/min/1.73 m2 at discharge. The median hospital journey (LOS) was 7 days (IQR 1–72). The mean LOS of patients survived was 5 days (IQR 1–62). Of the patients, 84.8% had NYHA class I–II at discharge. In addition, 94.2% of the patients were given information about their disease, 92.1% were suggested diet, 67.1% were suggested daily weight follow-up, and 71.4% were suggested influenza and pneumococcal vaccine.
Discussion
The Journey HF-TR study is a cross-sectional national database study aimed to survey patient journey in the hospital with HF in a large sample of Turkish population. Most of the patients were hospitalized with a diagnosis of decompensated HF (43.8%) similar to the Euro HF Survey II (EHFS II) (65.4%) and ESC-HF Pilot Survey (75%) (6, 7). Patients with a diagnosis of pulmonary edema were higher in our study (31.4%) than in the ESC-HF Survey II (16.2%) and ESC-HF Pilot Survey (13.3%) but was similar to the Italian survey on AHF (9). However, the rate of patients with de novo AHF was less than the ADHERE registry and EHFS II study (6, 8).
Our study population was younger (mean age: 67.8±13.2 years) than the EHFS II (mean: 70 years), ESC-HF Pilot (mean: 70 years), and Acute Decompensated Heart Failure National Registry (ADHERE) (mean: 72 years) (6, 8). The underlying causes of HF are different from other parts of the world. However, CAD and hypertension were the most frequent etiology of HF similar to other European surveys (6-8). However according to the EUROASPIRE III data, recordings from Turkey’s centers in comparison to the Europe population, the most important differences were observed in the higher rates of young patients with myocardial infarction (<50 years, 20% vs. 12.7%) (10).
The major precipitating factors were arrhythmia, infection, and non-compliance with medication in our study. The most frequent arrhythmia was atrial fibrillation that was similar to the rate in the EHFS II (39%) but less than the ESC-HF Pilot Survey (44%) and higher than the ADHERE (31%) (6-8).
In spite of the younger population in Journey HF-TR, the co-morbid conditions were much higher and had more severe HF than other registries (Table 2) (6-8). The presence of anemia was higher in our population than in other European population (EHFS II: 14.7% and ESC-HF pilot: 31.4%); however, it was similar to that reported in the ADHERE (53%) and OPTIMIZE-HF registries (51%) (8, 9, 11). The prevalence of anemia has been shown to increase with HF severity, from 9%, 19%, 53%, and 79% for NYHA class I–IV, respectively (12).
Table 2.
Comparison of demographic and clinical findings among our patients (Journey HF-TR) and patients with AHF in Europe and USA
| Journey HF-TR | EHFS II (3) | ESC-HF Pilot (4) | ADHERE (5) | |
|---|---|---|---|---|
| Age (year), mean±SD | 67.8±13.2 | 69.9±12.5 | 70±13 | 72.5±13.9 |
| De novo HF (%) | 17 | 37.1 | 25 | 24 |
| NYHA III—IV (%) | 75.2 | 28 | 35* | |
| LVEF (%), mean±SD | 32.7±14.1 | 38 | 38 | 34.4 |
| Anemia (%) | 48 | 14.7 | 31.4 | 53 |
| Atrial fibrillation (%) | 39 | 38.7 | 43.7 | 30 |
| Hypertension (%) | 67 | 62,5 | 61.8 | 72 |
| CAD (%) | 59.6 | 53.6 | 64 | 58 |
| Renal insufficiency (%) | 28.2 | 16.8 | 26 | 29 |
| In-hospital mortality (%) | 7.6 | 6.7 | 3.8 | 4 |
| LOS (median day) | 7 | 9 | 8 | 4.3 |
Dyspnea at rest (NYHA class IV).
LVEF - left ventricular ejection fraction, CAD - coronary artery disease, LOS - length of stay; NYHA - New York Heart Association
Moderate-to-severe mitral and tricuspid regurgitation was higher in our study population than in the EHFS II (52% and 49% vs. 43% and 30%, respectively) (6).
Diuretic therapy (by bolus or infusion route) was administered to 91.2% of all patients at hospitalization (83.4% in EHFS II) (6). Thirty percent of the patients had vasodilator therapy, and 19.5% had inotropic support (38.7% and 29.8% in EHFS II) (6). The proportion of patients requiring non-invasive and invasive mechanical ventilation was 16.4% and 7.8%, respectively (13.9% and 5.1% in EHFS II) (6). Previous studies have particularly emphasized that the early management of patients with AHF is important, as is the case in other cardiovascular emergencies (13-16). However, the initiation of i.v. therapy was <10 min only in 25.5% of our patients.
Our in-hospital mortality (7.6%) was higher than the EHFS II, ADHERE registry, and ESC-HF Pilot Survey (Table 2) (6-8, 16). The rate of dyspnea at rest, as one of the mortality predictors, was higher in our population than in other studies. In addition, our study population had more severe HF (mean EF: 33%) than the EHFS II and ESC-HF Pilot Survey (38% in both surveys) (6, 7). As the results of the CHARM study, the hazard ratio for all-cause mortality increased by 39% for every 10% reduction in EF <45% (17). In-hospital death, stroke, and myocardial infarction were reported with a frequency of 3.4%, 1.6%, and 2%, respectively, in the Turkish population of the TAKTIK study (Turkish Registry for Diagnosis and Treatment of Acute Heart Failure) who had a mean EF of 33±13% at admission (18). In the ADHERE, 46% of the registry patients had either normal or mild impairment of systolic function (8). The frequency of pulmonary edema, one of the reasons for in-hospital mortality, was relatively high (31.4%) in comparison to patients with pulmonary edema (7.4%) of the Romanian Acute Heart Failure Syndromes study (19).
The early diagnosis and management of hospitalized patients with appropriate strategies would be the main factor that determines the duration of in-hospital journey of patients with HF (14-16, 20). The median LOS in the ICU/CCU was 3 days in the Journey-HF (4 days in the ESC-HF Pilot Survey) (7). The median journey of the patient in the hospital (LOS) was 7, 9, and 8 days in our study, EHFS II, and ESC-HF Pilot Survey, respectively, whereas 4.3 days in the ADHERE registry (Table 2) (6-8). Guideline-directed medical therapy at discharge was similar to the European and US registers.
Study limitations
Surveys based on voluntary participation and recruitment of patients have obvious limitations that have to be acknowledged. Although participant sites were encouraged to enroll patients, as consecutively as possible, the study population may not represent the general population. Registry data are based only on documentation of medical history and management during hospitalization, and follow-up data are not obtained. Therefore, the readmission rate of the patients after discharge is unknown. Laboratory parameters, biomarkers, dosage, and duration of HF medications should be standardized. In addition, the medication dosage was not recorded, so we are not sure if the patients are taking the appropriate doses of HF medications.
Conclusion
In conclusion, this cross-sectional, multicenter and observational study that was performed in the Turkish AHF population showed higher in-hospital mortality despite younger patient population. The higher mortality rate might be associated with more common comorbidities and presence of more advanced stage HF population.
Analysis of such national real-world data can contribute to evaluate not only the main causes, comorbidities, and severity of HF but also the effectiveness of treatment and compliance of patients in each country.
Footnotes
Conflict of interest: None declared.
Peer-review: Externally peer-reviewed.
Authorship contributions: Concept – Ü.Y.S., M.Z.; Design – A.E.; Supervision – M.Z.; Fundings – M.Z.; Materials – B.Ö., F.A.A.; Data collection &/or processing – Ü.Y.S.; Analysis &/or interpretation – Ü.Y.S.; Literature search – L.B., Y.K.; Writing – Ü.Y.S.; Critical review – Ü.Y.S., İ.B., U.K., M.Z.
References
- 1.Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, et al. ESC Scientific Document Group. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37:2129–200. doi: 10.1093/eurheartj/ehw128. [DOI] [PubMed] [Google Scholar]
- 2.Cowie MR, Mosterd A, Wood DA, Deckers JW, Poole-Wilson PA, Sutton GC, et al. The epidemiology of heart failure. Eur Heart J. 1997;18:208–25. doi: 10.1093/oxfordjournals.eurheartj.a015223. [DOI] [PubMed] [Google Scholar]
- 3.Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, et al. Writing Group Members. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics--2010 update: a report from the American Heart Association. Circulation. 2010;121:e46–e215. doi: 10.1161/CIRCULATIONAHA.109.192667. [DOI] [PubMed] [Google Scholar]
- 4.Krumholz HM, Parent EM, Tu N, Vaccarino V, Wang Y, Redford MJ, et al. Readmission after hospitalization for congestive heart failure among Medicare beneficiaries. Arch Intern Med. 1997;157:99–104. [PubMed] [Google Scholar]
- 5.Cleland JG, Swedberg K, Follath F, Komajda M, Cohen-Solel A, Aguilar JC, et al. The EuroHeart Failure survey programme: a survey on the quality of care among patients with heart failure in Europe. Part 1: patient characteristics and diagnosis. Eur Heart J. 2003;24:442–63. doi: 10.1016/s0195-668x(02)00823-0. [DOI] [PubMed] [Google Scholar]
- 6.Nieminen MS, Brutsaert D, Dickstein K, Drexler H, Follath F, Harjola VP, et al. EuroHeart Survey Investigators;Heart Failure Association, European Society of Cardiology. EuroHeart Failure Survey II (EHFS II): a survey on hospitalized acute heart failure patients: description of population. Eur Heart J. 2006;27:2725–36. doi: 10.1093/eurheartj/ehl193. [DOI] [PubMed] [Google Scholar]
- 7.Maggioni AP, Dahlström U, Filippatos G, Chioncel O, Leiro MC, Drozdz J, et al. Heart Failure Association of ESC (HFA) EURObservational Research Programme: the Heart Failure Pilot Survey (ESC-HF Pilot) Eur J Heart Fail. 2010;12:1076–84. doi: 10.1093/eurjhf/hfq154. [DOI] [PubMed] [Google Scholar]
- 8.Adams KF, Jr, Fonarow GC, Emerman CL, LeJemtel TH, Costanzo MR, Abraham WT, et al. ADHERE Scientific Advisory Committee and Investigators. Characteristics and outcomes of patients hospitalized for heart failure in the United States: rationale, design, and preliminary observations from the first 100,000 cases in the Acute Decompensated Heart Failure National Registry (ADHERE) Am Heart J. 2005;149:209–16. doi: 10.1016/j.ahj.2004.08.005. [DOI] [PubMed] [Google Scholar]
- 9.Galvao M, Kalman J, DeMarco T, Fonarow GC, Galvin C, Ghali JK, et al. Gender differences in in-hospital management and outcomes in patients with decompensated heart failure: analysis from the Acute Decompensated Heart Failure National Registry (ADHERE) J Card Fail. 2006;12:100–7. doi: 10.1016/j.cardfail.2005.09.005. [DOI] [PubMed] [Google Scholar]
- 10.Tokgözoğlu L, Kaya EB, Erol C, Ergene O, EUROASPIRE III Turkey Study Group. [EUROASPIRE III: a comparison between Turkey and Europe] Turk Kardiyol Dern Ars. 2010;38:164–72. [PubMed] [Google Scholar]
- 11.Young JB, Abraham WT, Albert NM, Gattis Stough W, Gheorghiade M, Greenberg BH, et al. OPTIMIZE-HF Investigators and Coordinators. Relation of low hemoglobin and anemia to morbidity and mortality in patients hospitalized with heart failure (insight from the OPTIMIZE-HF registry) Am J Cardiol. 2008;101:223–30. doi: 10.1016/j.amjcard.2007.07.067. [DOI] [PubMed] [Google Scholar]
- 12.Silverberg DS, Wexler D, Iaina A. The importance of anemia and its correction in the management of severe congestive heart failure. Eur J Heart Fail. 2002;4:681–6. doi: 10.1016/s1388-9842(02)00115-0. [DOI] [PubMed] [Google Scholar]
- 13.Wuerz RC, Meador SA. Effects of prehospital medications on mortality and length of stay in congestive heart failure. Ann Emerg Med. 1992;21:669–74. doi: 10.1016/s0196-0644(05)82777-5. [DOI] [PubMed] [Google Scholar]
- 14.Farmakis D, Parissis J, Lekakis J, Filippatos G. Acute heart failure: Epidemiology, risk factors, and prevention. Rev Esp Cardiol (Engl Ed) 2015;68:245–8. doi: 10.1016/j.rec.2014.11.004. [DOI] [PubMed] [Google Scholar]
- 15.Peacock WF, Emerman C, Costanzo MR, Diercks DB, Lopantin M, Fonarow GC. Early vasoactive drugs improve heart failure outcomes. Congest Heart Fail. 2009;15:256–64. doi: 10.1111/j.1751-7133.2009.00112.x. [DOI] [PubMed] [Google Scholar]
- 16.Kaya H, Yilmaz MB. In-hospital journey of patients with heart failure. International Journal of the Cardiovascular Academy. 2015;1:31–3. [Google Scholar]
- 17.Solomon SD, Anavekar N, Skali H, McMurray JJ, Swedberg K, Yusuf S, et al. Candesartan in Heart Failure Reduction in Mortality (CHARM) Investigators. Influence of ejection fraction on cardiovascular outcomes in a broad spectrum of heart failure patients. Circulation. 2005;112:3738–44. doi: 10.1161/CIRCULATIONAHA.105.561423. [DOI] [PubMed] [Google Scholar]
- 18.Eren M, Zoghi M, Tuncer M, Çavuşoğlu Y, Demirbağ R, Şahin M, et al. TAKTIK Investigators. Turkish registry for diagnosis and treatment of acute heart failure: TAKTIK study. Turk Kardiyol Dern Ars. 2016;44:637–46. doi: 10.5543/tkda.2016.07572. [DOI] [PubMed] [Google Scholar]
- 19.Chioncel O, Ambrosy AP, Bubenek S, Filipescu D, Vinereanu D, Petris A, et al. Romanian Acute Heart Failure Syndromes study investigators. Epidemiology, pathophysiology, and in-hospital management of pulmonary edema: data from the Romanian Acute Heart Failure Syndromes registry. J Cardiovasc Med (Hagerstown) 2016;17:92–104. doi: 10.2459/JCM.0000000000000192. [DOI] [PubMed] [Google Scholar]
- 20.Moleerergpoom W, Hengrussamee K, Piyayotai D, Jintapakorn W, Sukhum P, Kunjara-Na-Ayudhya R, et al. Predictors of in-hospital mortality in acute decompensated heart failure (Thai ADHERE) J Med Assoc Thai. 2013;96:157–64. [PubMed] [Google Scholar]


