Introduction
Left ventricular (LV) thrombus is usually seen in patients with significantly reduced LV systolic function especially those surviving a large ST-elevation myocardial infarction (STEMI). It usually occurs when the STEMI is anterior, anterolateral or anteroseptal with a large area of akinesia or dyskinesia involving the apex. It may occur following an inferior or a posterior STEMI with large akinetic segments in the inferior or posterior walls in rare occasions (1).
The main risk associated with LV thrombi is distal systemic embolization that usually occurs during the first 3 - 4 months after infarction (2, 3).
The main clinical consequence of thromboembolism is the occurrence of stroke, and the current guidelines do recommend the use of vitamin K antagonists (VKAs) as a preventive measure in patients with LV thrombus. Non-VKA direct oral anticoagulants (DOACs) are currently replacing VKA in several clinical indications, such as in patients with non-valvular atrial fibrillation (AF) where they were found to be either non-inferior or superior to VKAs. However, to our knowledge, there are no robust data on the use of DOACs for the treatment of LV thrombi, and all the available data are limited to individual case reports (4, 5).
We present the effect of rivaroxaban, a DOAC, in the dissolution of LV thrombi in a series of patients presenting with acute coronary syndrome (ACS) and receiving dual antiplatelet therapy (DAPT) without valvular heart disease.
Case Report
We report eight cases of LV thrombi where rivaroxaban was used instead of warfarin. Some of the patients were indicated for the use of DOACs on top of AF. Written consent was obtained from all the patients for the use of the DOACs in their cases after proper explanation. Tables 1 and 2 show the demographic characteristics, and clinical and follow-up data.
Table 1.
Detailed data of the included cases
| Case no. | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| Age (years) | 45 | 40 | 69 | 52 | 39 | 46 | 65 | 60 |
| Sex | Male | Male | Male | Male | Female | Male | Male | Female |
| Diabetes mellitus | Yes | No | No | No | No | No | Yes | Yes |
| Hypertension | Yes | Yes | No | Yes | No | Yes | No | No |
| Smoking | No | No | Yes | No | No | No | No | No |
| Presentation | NSTEMI | STEMI | STEMI | STEMI | STEMI | STEMI | NSTEMI | NSTEMI |
| Complications | VT | None | AF | None | None | None | VF | Shock/AF |
| PCI site | LAD & LCX | LAD* | LAD* | LAD* | LAD* | LAD* | LAD & RCA | LAD & RCA |
| Baseline EF | 40% | 35% | 30% | 35% | 40% | 40% | 25% | 30% |
| EDV (mL) | 140 | 155 | 159 | 157 | 142 | 132 | 169 | 160 |
| Creatinine clearance (mL/min.) | 122 | 140 | 78 | 89 | 142 | 135 | 102 | 108 |
| LV thrombus size (mm) | 10x10 | 12x5 | 13x7 | 14x7 | 8x2 | 10x6 | 12x10 | 12x12 |
| HAS-BLED score | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 1 |
| Aspirin dose (mg/day) | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
| Clopidogrel dose (mg/day) | 75 | 75 | 75 | 75 | 75 | 75 | 75 | 75 |
| Rivaroxaban dose (mg/day) | 15 | 15 | 20 | 20 | 15 | 15 | 15 | 20 |
| Follow-up EF | 50% | 55% | 45% | 50% | 55% | 55% | 35% | 50% |
| Follow-up thrombus | Absent | Absent | Absent | Absent | Absent | Absent | Present | Absent |
Culprit vessel.
AF - atrial fibrillation; EDV - end-diastolic volume; EF - ejection fraction; LAD - left anterior descending artery; LCX coronary intervention; RCA - right coronary artery; VF - ventricular fibrillation; VT - ventricular tachycardia
Table 2.
Baseline characteristics and follow-up data
| Baseline characteristics (n=8) | |
|---|---|
| Age (years) | 52.1±14.4 |
| Male sex | 6 (75) |
| STEMI | 5 (63) |
| Diabetes mellitus | 6 (75) |
| Hypertension | 6 (75) |
| Smoking | 5 (63) |
| Family history of CAD | 0 (0) |
| Baseline ejection fraction (%) | 34±6 |
| Valvular heart disease | 0 (0) |
| Atrial fibrillation | 3 (38) |
| Ventricular tachycardia | 1 (13) |
| Follow-up at 3 months (n=8) | |
| Ejection fraction (%) | 46±7 |
| Persistence of thrombus | 1 (13) |
| Stroke | 0 (0) |
| Distal embolization | 0 (0) |
| Any bleeding | 0 (0) |
Results are shown in the number of patients (%).
STEMI - ST-elevation myocardial infarction; CAD - coronary artery disease
Discussion
Rivaroxaban is one of the DOACs that act by direct inhibition of factor Xa and has been granted approval for several clinical indications, such as treatment of deep venous thrombosis, pulmonary embolism and non-valvular AF (6-8).
Currently, the only recommended oral anticoagulant for the treatment of LV thrombi is warfarin (VKA). There is a paucity of data on the role of DOACs in the treatment of LV thrombi except for few case reports (5, 9, 10).
In 2014, Nagamoto et al. (11) reported the successful resolution of LV thrombus in a 77-year-old male patient with old myocardial infarction after 27 days of treatment with dabigatran without thromboembolic or bleeding complications. Similarly, in 2015, Yamamoto et al. (12) reported the successful treatment of LV thrombi in two patients with old anteroseptal myocardial infarction within 2-6 weeks of treatment with dabigatran and antiplatelet drugs.
Rivaroxaban was also used for treating a case of intraventricular thrombus in Chagas disease (13) and dilated cardiomyopathy (14). Several reported cases have shown the efficacy of apixaban in cases of intraventricular thrombi without increased risk of thromboembolic or bleeding issues even when used with DAPT in patients with post-MI (15, 16).
Azizi et al. (17) described a case of post-infarction LV thrombus dissolution using a combination of DAPT plus rivaroxaban for 3 months (Fig. 1). Makrides (4) demonstrated total LV thrombus dissolution in three cases using a reduced dose of rivaroxaban 15 mg/day in a setting of ACS requiring DAPT. In patients requiring oral anticoagulation after percutaneous coronary intervention, the European Society of Cardiology (18) states that triple therapy should be limited in duration, depending on the clinical setting, thromboembolic, and bleeding risks assessed using CHA2DS2-VASc score and HAS-BLED score, respectively. The duration should depend on the individual risk for ischemic and bleeding events. The cases in our series had a HAS-BLED score of 1 - 2.
Figure 1.
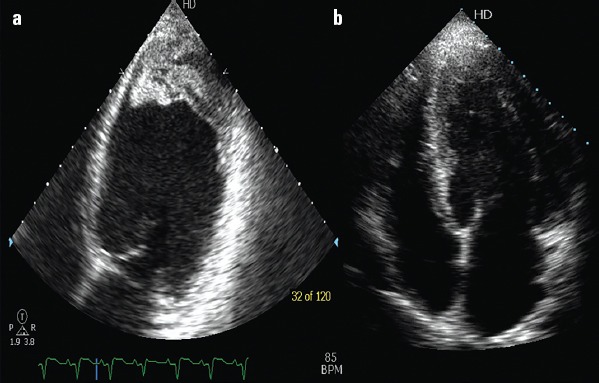
Two-dimensional transthoracic echocardiography showing the left ventricular apical thrombus before (a) and after (b) the use of rivaroxaban for 3 months
Triple therapy including a novel oral anticoagulant may have unpredictable clinical results as only a few studies addressed patients with coronary artery disease and non-valvular AF (17). In the APPRAISE-2 study, apixaban was combined with aspirin and clopidogrel in 81% of the patients and led to a significant increase in fatal and intracranial bleeding without clinical benefit (19). In ATLAS ACS 2, low-dose rivaroxaban (2.5–5 mg two times/day) was administered with aspirin and clopidogrel in 92% of the patients. This was associated with a 16% reduction in the composite efficacy endpoint (cardiovascular death, myocardial infarction and stroke) and a small increase in major bleedings (20). Most observational studies and meta-analyses reported embolic events in patients with LV thrombus to occur within the first 3-4 months. Based on this temporal profile, the current guidelines recommend the duration of anticoagulation therapy patients with LV thrombi to be limited to 3 months. For the cases being reported, rivaroxaban was initiated at a dose of 15-20 mg/day in addition to DAPT (acetylsalicylic acid 100 mg/day plus clopidogrel 75 mg/day) for a period of 3 months. A follow-up transthoracic echocardiography (TTE) at 3 months revealed dissolution of the LV thrombi in 7 out of 8 patients. No thromboembolic or bleeding events were experienced. This supports previous reports on the successful use of rivaroxaban along with DAPT in the treatment of LV thrombi complicating myocardial infarction. Randomized controlled trials are needed to validate the results of these encouraging observational data. A currently ongoing phase 3 clinical trial (Apixaban Versus Warfarin in Patients with LV Thrombus) is designed to assess whether apixaban is as effective as VKA for the treatment of LV thrombus after acute ST-segment elevation MI. The primary efficacy endpoint will be the presence of LV thrombus as assessed by TTE after 3 months of treatment with oral anticoagulation and secondary efficacy endpoints of clinically significant stroke or systemic embolism requiring hospitalization, major bleeding and all-cause mortality (time frame is 3 months).
In addition, it is noteworthy that the patient with residual LV thrombus underwent another TTE 3 months later revealing a complete resolution of the thrombus.
Conclusion
Rivaroxaban can be safely used in the treatment of LV thrombi without increased risk of bleeding instead of the routinely used VKA. A large-scale randomized trial is required to evaluate the benefits and risks of the use of DOACs compared with the conventional treatment with VKA in patients with or at high risk of LV mural thrombi, to confirm their safety and to define the optimal dosing if combined with DAPT in patients with LV thrombi complicating acute MI.
References
- 1.Weinsaft JW, Kim J, Medicherla CB, Ma CL, Codella NC, Kukar N, et al. Echocardiographic algorithm for post– myocardial infarction LV thrombus: a gatekeeper for thrombus evaluation by delayed enhancement CMR. JACC Cardiovasc Imaging. 2016;9:505–15. doi: 10.1016/j.jcmg.2015.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cregler LL. Antithrombotic therapy in left ventricular thrombosis and systemic embolism. Am Heart J. 1992;123:1110–4. doi: 10.1016/0002-8703(92)91069-d. [DOI] [PubMed] [Google Scholar]
- 3.Udell JA, Wang JT, Gladstone DJ, Tu JV. Anticoagulation after anterior myocardial infarction and the risk of stroke. PLoS One. 2010;5:e12150. doi: 10.1371/journal.pone.0012150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Makrides CA. Resolution of left ventricular postinfarction thrombi in patients undergoing percutaneous coronary intervention using rivaroxaban in addition to dual antiplatelet therapy. BMJ Case Rep. 2016;2016 doi: 10.1136/bcr-2016-217843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seecheran R, Seecheran V, Persad S, Seecheran NA. Rivaroxaban as an antithrombotic agent in a patient with ST-segment elevation myocardial infarction and left ventricular thrombus: a case report. J Investig Med High Impact Case Rep. 2017;5 doi: 10.1177/2324709617697991. 2324709617697991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Heidbuchel H, Verhamme P, Alings M, Antz M, Hacke W, Oldgren J, et al. European Heart Rhythm Association Practical Guide on the use of new oral anticoagulants in patients with non-valvular atrial fibrillation. Europace. 2013;15:625–51. doi: 10.1093/europace/eut083. [DOI] [PubMed] [Google Scholar]
- 7.Saar JA, Maack C European Society of Cardiology. Diagnosis and management of acute pulmonary embolism. ESC guidelines 2014. Herz. 2015;40:1048–54. doi: 10.1007/s00059-015-4378-0. [DOI] [PubMed] [Google Scholar]
- 8.Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, et al. ESC Scientific Document Group. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016;37:2893–962. doi: 10.1093/eurheartj/ehw210. [DOI] [PubMed] [Google Scholar]
- 9.Yildirim E, Kalkan K, Ipek E, Demirelli S, Ermiş E. Successful resolution of left ventricular thrombus with apixaban treatment. International Journal of the Cardiovascular Academy. 2016;2:57–8. [Google Scholar]
- 10.Kaku B. Intra-cardiac thrombus resolution after anti-coagulation therapy with dabigatran in a patient with mid-ventricular obstructive hypertrophic cardiomyopathy: a case report. J Med Case Rep. 2013;7:238. doi: 10.1186/1752-1947-7-238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nagamoto Y, Shiomi T, Matsuura T, Okahara A, Takegami K, Mine D, et al. Resolution of a left ventricular thrombus by the thrombolytic action of dabigatran. Heart Vessels. 2014;29:560–2. doi: 10.1007/s00380-013-0403-5. [DOI] [PubMed] [Google Scholar]
- 12.Yamamoto T, Konishi T, Funayama N, Kikuchi B, Hotta D, Ohori K. Resolution of Left Ventricular Thrombus after Dabigatran Therapy in Two Patients with Old Anteroseptal Myocardial Infarction. Cardiol Pharmacol. 2015;4:152. [Google Scholar]
- 13.Las Casas AA, Jr, Las Casas AA, Borges MAF, Melo-Souza SE. Rivaroxaban for treatment of intraventricular thrombus in Chagas disease. Journal of Cardiology Cases. 2016;13:75–7. doi: 10.1016/j.jccase.2015.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Padilla Pérez M, Salas Bravo D, Garcelán Trigo JA, Vazquez Ruiz, de Castroviejo E, Torres Llergo J, Lozano Cabezas C, et al. Resolution of left ventricular thrombus by rivaroxaban. Future Cardiol. 2014;10:333–6. doi: 10.2217/fca.14.12. [DOI] [PubMed] [Google Scholar]
- 15.Mano Y, Koide K, Sukegawa H, Kodaira M, Ohki T. Successful resolution of a left ventricular thrombus with apixaban treatment following acute myocardial infarction. Heart Vessels. 2016;31:118–23. doi: 10.1007/s00380-014-0562-z. [DOI] [PubMed] [Google Scholar]
- 16.Berry A, Brancheau D, Zughaib M. Rapid resolution of left ventricular thrombus with apixaban therapy. SAGE Open Med Case Rep. 2017;5 doi: 10.1177/2050313X17745211. 2050313X17745211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Azizi A, Puricel S, Cook S, Brugger N. Rivaroxaban dissolves postinfarction left ventricular thrombus. Cardiovascular Medicine - Kardiovaskuläre Medizin - Médecine Cardiovasculaire. 2016;19:25–7. [Google Scholar]
- 18.Valgimigli M, Bueno H, Byrne RA, Collet JP, Costa F, Jeppsson A, et al. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS. Eur J Cardiothorac Surg. 2018;53:34–78. doi: 10.1093/ejcts/ezx334. [DOI] [PubMed] [Google Scholar]
- 19.Alexander JH, Lopes RD, James S, Kilaru R, He Y, Mohan P, et al. APPRAISE-2 Investigators. Apixaban with antiplatelet therapy after acute coronary syndrome. N Engl J Med. 2011;365:699–708. doi: 10.1056/NEJMoa1105819. [DOI] [PubMed] [Google Scholar]
- 20.Mega JL, Braunwald E, Wiviott SD, Bassand JP, Bhatt DL, Bode C, et al. ATLAS ACS 2– TIMI 51 Investigators. Rivaroxaban in patients with a recent acute coronary syndrome. N Engl J Med. 2012;366:9–19. doi: 10.1056/NEJMoa1112277. [DOI] [PubMed] [Google Scholar]


