Abstract
Additive manufacturing is a rapidly emerging technology which is being successfully implemented in the various field of medicine as well as in orthopaedics, where it has applications in reducing cartilage defects and treatments of bones. The technology helps through systematic collection of information about the shape of the "defects" and precise fabrication of complex 3D constructs such as cartilage, heart valve, trachea, myocardial bone tissue and blood vessels. In this paper, a large number of the relevant research papers on the additive manufacturing and its application in medical specifically orthopaedics are identified through Scopus had been studied using Bibliometric analysis and application analysis is undertaken. The bibliometric analysis shows that there is an increasing trend in the research reports on additive manufacturing applications in the field of orthopaedics. Discussions are on using technological advancement like scanning techniques and various challenges of the orthopaedic being met by additive manufacturing technology. For patient-specific orthopaedic applications, these techniques incorporate clinical practice and use for effective planning. 3D printed models printed by this technology are accepted for orthopaedic surgery such as revision of lumbar discectomy, pelvic surgery and large scapular osteochondroma. The applications of additive manufacturing in orthopaedics will experience a rapid translation in future. An orthopaedic surgeon can convert need/idea into a reality by using computer-aided design (CAD) software, analysis software to facilitate the manufacturing. Thus, AM provides a comprehensive opportunity to manufacture orthopaedic implantable medical devices.
Keywords: Additive manufacturing (AM), Orthopaedic, 3D scanning, magnetic resonance imaging (MRI) and computer tomography (CT)
1. Introduction
Applications of AM have become prevalent in various medical areas. Researchers and surgeons increasingly use this technology for fabricating of complex implant that is helpful for medical as well as in orthopaedics. Patient's anatomy is represented by a three-dimensional virtual model which can be easily obtained from different scanning techniques and printed by Additive manufacturing technology. The fabrications of these implants were previously just prohibitive by using subtractive manufacturing methods. 3D printed model gives a better understanding of complex pathology and anatomy of patients which is also suitable for surgical training.1,2 It is also a method of prototyping of personalised instrumentation for traumatology and orthopaedic surgery3.
AM is used in surgical fields such as orthopaedic surgery, preoperative evaluation, diagnosis, operative planning and paediatric surgery. AM is suitable for maxillofacial surgery as ceramic, and metal powder can be used for the fabrication of personalised prostheses. This technology is continuously improving the manufactured parts as it focuses on the utilisation and has great ability to incorporate scaffolds. The main advantages of AM are the reduction of surgery time and improved medical outcome. Currently, this technology is available for surgical planning of orthopaedic procedure. However, in case of individual patient histories, there is a shortfall of standardised orthopaedic solutions and is costly & time-consuming. By the application of AM, these problems are identified in relatively lesser time and with lower cost.4 In medical there is a requirement of innovation for clinicians and scientists.5
It allows the designing and fabrication of customised prosthetic implants that as per the specific requirement of the patient, like shape, size and mechanical properties of the implant. AM helps in reducing design and manufacturing time because implant pattern is scanned with Magnetic resonance imaging (MRI) and Computer tomography (CT). It solves the various problem of orthopaedics where standard implants cannot fulfil the individual requirement of the patient. Previous the implants were modified manually by the surgeon to make them fit for the patient.6 It is also professionally used in various other specialities such as neurosurgery, plastic surgery, oncology, craniofacial and dentistry.
In medical usually, four additive manufacturing technologies are being used, these include stereolithography (SLA), selective laser sintering (SLS), fused deposition modelling (FDM) and electron beam melting (EBM). By the application of these technologies the structural parameters, like the diameter of pore, porosity and Interconnectivity can be precisely controlled to maintain the proliferation, adhesion and differentiation of cells.7
In cardiothoracic surgery, 3D printed patient-specific model are for pre-operative simulation; such as complex aortic arch obstruction, tracheoesophageal fistula model, lung vasculature model and hypoplastic aortic arch model. In transplant surgery, a 3D printed patient model has been used for planning & simulating kidney and lobar lung transplantation. Before lobar lung transplantation, the model donor and recipient pulmonary vasculature are printed by the application of this technology. In transplantation of kidney, pelvic cavity replica can also be printed easily.4,8
2. Advancement of additive manufacturing
Additive manufacturing is a rapidly emerging technology that is used successfully in the various field of medical, like cartilage defects reduction and treatments of bones. The information about the shape of the defects is collected and is used to fabricate complex 3D constructs such as cartilage, heart valve, trachea, myocardial bone tissue and blood vessels. It can overcome some challenges of engineering as encountered in tissue engineering and regenerative medicine fields. Additive manufacturing is used to develop and manufacture scaffolds for tissue engineering as per the various requirements including porosity, biodegradability and biocompatibility at the exact shape. 6,9
The printing of bone regeneration scaffolds which are accurately made up of calcium phosphate and collagen. It is used for the construction of vascularised cell-laden and cartilaginous tissues that contains hyaluronic acid and chondrocytes. This technology has demonstrated the ability for the fabrication of scaffolds with multiple cells and biomaterials. It is a powerful tool that reconstructs organ and tissue structures after some injury. It fulfils difficult challenges and easily obtains the shape of defects; fabricate customised from hydrogel and synthesising appropriate biomaterials.10,11
3. Techniques, process and materials used in different additive manufacturing technologies
Additive manufacturing technologies offer different materials with different flexibilities, colour, density, durability, texture, and tensile strength. AM technologies can print craniofacial bone models, providing a 3D printed tactile sensation of human bone. Various processes and materials that are used commonly in additive manufacturing technologies with their medical use are listed in Table 1.
Table 1.
Additive manufacturing technologies techniques, process, materials, layer thickness with medical applications.
| S. No | AM techniques | Process | Materials | Medical application | Layer thickness | References |
|---|---|---|---|---|---|---|
| 1 | Stereolithography (SLA) | It uses the application of ultraviolet laser inside a vat of resin | Acrylate photopolymer Plastic Glass Ceramic Epoxy resin |
Anatomical model Prosthetics |
0.002mm | Zhou et al. 12; Bens et al. 13 |
| 2 | Selective laser sintering (SLS) | Sintering is done by the application of CO2 laser A fine thermoplastic powder like nylon or polycarbonate is used to form model layer by layer |
Ceramic Thermoplastics Powder Plastic Metals |
Human anatomy Customised implants for training |
0.060 mm to 0.150 mm | Sing et al. 14; Deckers et al. 15 |
| 3 | Electron Beam Melting (EBM) | Powerful electron beam used to built layer by layer metal powder by command of CAD model with exact geometry | Metal powder Titanium |
Fabrication of implant | 0.050- 0.200 mm | Wysocki et al. 16; Gibbon and Hansell, 17 |
| 4 | Direct metal laser sintering (DMLS) | This technique is similar to SLS where the application of laser does sintering of metal powder | Titanium Cobalt Aluminium Bronze alloy Steel Stainless steel Nickel alloy |
Manufacturing of prostheses or implants Dental Crowns |
0.0008-0.0016 mm | Salmi et al. 6; Gale and Chuhan, 18 |
| 5 | Laminated Object Manufacturing (LOM) | 3D model fabricated by adding layers of the defined sheet of materials | Metal Plastic Paper |
Customised joint replacement Prosthesis | 0.1mm | Kechagias, 19; Park et al. 20 |
| 6 | Fused deposition modelling (FDM) | The process is similar to extrusion, where a heated thermoplastic material is added layer by layer to fabricate a model | polycarbonate Acrylonitrile butadiene styrene (ABS) polypropylene Wax polyesters |
Pharmaceutical Drug delivery device Helpful for maxillofacial surgery |
0.005- 0.010 mm | Armillotta et al. 21; Singh, 22 |
| 7 | Inkjet 3D printing | Use different fluid fluids such as polymer solution provided in the form of liquid and deposited layer by layer to built a product | Power Liquid binder |
Medical education Surgical planning |
0.087mm | Gua et al. 23 Yang et al. 24; Mancanares et al. 25 |
| 8 | Polyjet 3D printing | Production is done through a UV-curable acrylic plastic Uses various types of printing materials, and its post-processing stage is straightforward. |
Photopolymers | Orthopaedic implant Preclinical Testing Anatomical models |
0.00065mm | Moore and Williams, 26; Javaid et al. 7 |
| 9 | Colour-Jet-Printing (CJP) | Part is built by spreading material in the layer, over the build platform using a roller Printing head jets layer of binder on the material layer |
Gypsum powder Binder |
Full-colour implants of heart | 0.003-0.004mm | Yang et al. 24; Mancanares et al. 25 |
| 10 | Multi-Jet Printing | Nozzles are used to spray binding of liquid onto metallic powder or ceramic to create a solid thin layer After production of the model, it must be sintered in the furnace to increase the strength |
Powder Plastics |
Orthopaedics Dental |
0.016mm | Kan and Yuen, 27; El-Wahab et al. 28 |
The properties of the raw material and layer thickness have a significant impact on the quality of product/implant produced. Appropriate quality of raw material creates a product with higher mechanical strength. If layer thickness is decreased, the parts printed through these technologies give better surface finish and mechanical strength.
4. Benefits of additive manufacturing in medical
Additive manufacturing fabricates custom implants of any complex shape and in the exact geometric feature, which is not previously possible by using traditional manufacturing techniques. Various benefits of additive manufacturing are as under:
-
•
It gives perfect-fit production of a patient-specific implant
-
•
During implant manufacturing, offers unlimited geometric freedom.
-
•
Used to generate free-form scaffold of an individual patient
-
•
Precise setting of desired elasticity
-
•
Precise setting of grid structures/surface roughness
-
•
High bio-compatibility
-
•
It quickly creates a bone defect
-
•
Manufacture of the parts in one shot
-
•
Faster availability and shorter build times
-
•
Fully automated and digitised manufacturing
-
•
Cost savings and resource conservation
-
•
Overall improvement with economies of scale and cost saving
-
•
Potential to reduce the stiffness mismatch at junctions of bone–implant and minimised the porosity.
-
•
Allows biomechanical evaluation of the design of specific patient under specific loading conditions to the actual implant fabrication.
5. Research status on additive manufacturing applications in orthopaedics
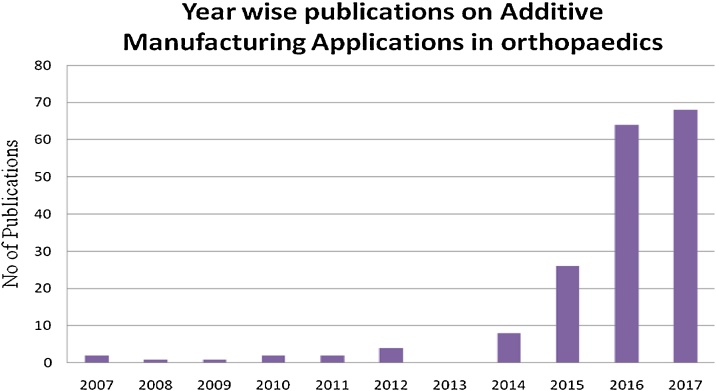
Extensive research is done in the area of AM applications in orthopaedics. Scopus database is used to identify the research articles related to this area; here we have identified 181 research articles about this area. The first paper published on additive manufacturing was in 2000. Here we show data from 2007 to 2017. In the year 2007, there were only two research articles published in this area, and it has now increased to 68 in 2017. Fig. 1 shows year-wise publications on additive manufacturing from 2007 to 2017.
Fig. 1.
Additive manufacturing applications in orthopaedics: Year-wise publications (Source: Scopus).
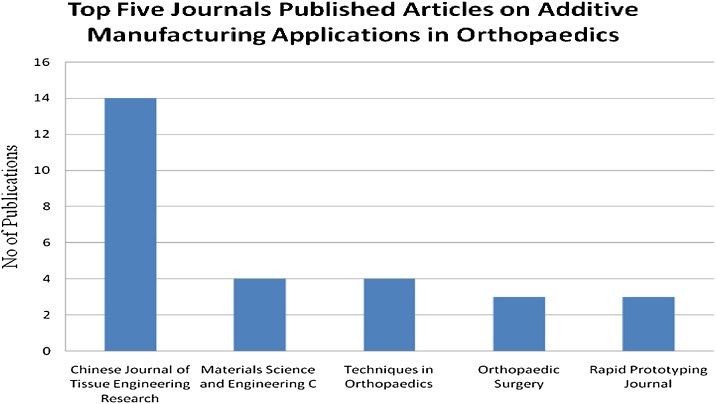
There is a sustained increase of articles related to additive manufacturing applications in orthopaedics. The details of the papers published in different journals on orthopaedics through the application of this technology. Fig. 2 shows the top five journals publish research articles in this area. Out of top five, Chinese Journal of tissue engineering research have highest publications of 14. Materials science and engineering: C and Techniques in orthopaedics have four publications each is at position 2 and 3. Orthopaedic Surgery and Rapid Prototyping Journal both have the equal number of publications, i.e. three are ranked fourth and fifth respectively and presents a large contribution by tissue engineering research.
Fig. 2.
Additive manufacturing applications in orthopaedics (Source: Scopus).
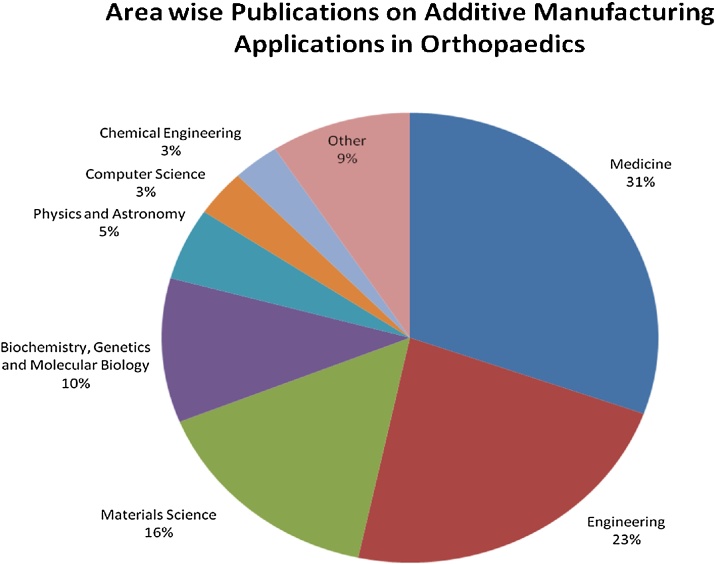
Fig. 3 shows the area-wise research on additive manufacturing applications in orthopaedics; It observes that medicine have maximum utilisation (31%) of this technology mainly in the field of orthopaedics; whereas engineering fields contribute 23%, material science contribute 16%, and biochemistry, genetics and molecular biology contribute 10%. The diverse application of AM in areas of physics & astronomy (5%), computer science (3%), chemical engineering (3%) and others area (9%) which includes chemistry, dentistry, pharmacology, toxicology and pharmaceutics, health professions, mathematics, neuroscience, immunology and microbiology, agricultural and biological sciences and energy.
Fig. 3.
Additive manufacturing applications in orthopaedics: Area-wise contributions (Source: Scopus).
From Scopus data, it is analysed that applications of additive manufacturing are increasing in the area of orthopaedics. Thus these technologies/machines are becoming commercially viable and acceptable in the field of orthopaedics.
6. Devices used to capture data to make implant by additive manufacturing in orthopaedics
AM produce customised patient-specific implants with the help of computerised tomography (CT), magnetic resonance imaging (MRI) and 3D scanner. DICOM software is used to converts patient (CT, MRI) scan data into 3D files or we can use a 3D scanner to take patient data and print using additive manufacturing technologies. But the main limitation of the 3D scanner over CT and MRI scan is that 3D scanner can measure outer body surface, whereas CT and MRI provide information about hard/soft tissue structure.
CT scan: A CT scan sends X-ray beam to the body that moves through an arc and captures many pictures. It is used for imaging and collected data of hard tissue like bone. It takes fewer minutes because sometimes radiation scan is unsuitable for the patient3.
MRI scan: It uses a powerful magnet to align nuclei atoms inside the body. It provides clear information of normal and abnormal tissue as compared to CT scan. It uses powerful magnetic field and radio frequency pulses to achieve the detailed picture of soft tissues, bone, organs and other internal structure of the body. It is also useful to obtain an accurate diagnosis. It cannot take a longer time to complete the scan.29,30
3D scanning: 3 D scanning is used to scan outer surface of object/ patient body in the form of a point cloud or a triangle mesh and generate a 3D surface. It captures data of the outer surface of the body such as skin which is difficult to measure precisely by CT and MRI scanning and have extensive applications4.
7. Challenges of additive manufacturing in orthopaedics
AM technologies can print multiple types of material and different colours which are helpful for doctors and surgeon towards analysing the defects. This technology reduces product development time & the cost and improves communication between surgeon and the patient. AM meet various challenges in orthopaedics are discussed in following Table 2.
Table 2.
Challenges of Additive Manufacturing in Orthopaedics.
| S. No | Challenges | Description | References |
|---|---|---|---|
| 1 | Facilitate surgery design | CT and MRI scan are used to create 3D images of bones and fabricate bones by using additive manufacturing technologies Useful for presentation, teaching and surgical design Technology is used efficiently for reverse engineering techniques such as missing parts Applied for custom made prosthesis Doctors have now used this technique for medical education and facilitate complex surgery design |
Cai 31; Verma et al. 32; Lal et al. 33 |
| 2 | Orthopaedics metal implants | AM technologies such as Direct Metal Laser printing (DMLS) can also produce metal implants The main advantages of DMLS are to offer both macro and microstructural scales personalised implants. |
Salmi et al. 6; Morrison et al. 34 |
| 3 | Multi-material prints | Different AM technologies are available to print a 3D model of multi-materials. Models represent a different section of bone, soft tissue and organ which provide a clear understanding of the patient body and helpful for training of medical students. |
Yap et al. 35; Javaid and Haleem, 4 |
| 4 | Prosthetics | Easily create artificial device/model which easily replaces missing body part lost by accident or other diseases Prosthetic manufactured by this technology has the ability to intended normal function in the body Produces prosthetic which perfectly match with used anatomy Technology manufactured customised, low-cost prosthetics such as artificial leg which improve human comfort |
Vaish and Vaish, 3; Chung et al. 36 |
| 5 | Lead time | One of the challenges of AM is to create iterate design and prototype that reduce time to market This technology can speed up the design improvements of any medical devices by analysing feedback from doctors and the surgeons It supports clinical trials by optimising the design of medical instruments. |
Cohen et al. 37; Horn et al. 9 |
| 6 | Instruments designing | Effective design and development of instruments that simplify the surgical procedure improve the accuracy of the alignment and shorten the operative time The applications of AM based instruments for orthopaedics, spinal surgery and trauma Uses effectively to achieve clinical practices |
Rose et al. 38; Vaish and Vaish, 3 |
| 7 | Innovative ideas for the surgeon | AM impact on the orthopaedic field where surgeons and doctors use 3D printed or bone model to train students Suitable for the patient to explain in detail of surgery and surgeon can also practice before the actual surgery which gives innovative ideas |
Costello et al. 10; Javaid and Haleem, 1 |
| 8 | Customisation | AM is an ideal solution for individualised patient data in medical as well as in orthopaedics Enables to create orthotic and prosthetic devices of patient-specific anatomy |
Kim et al. 39; Bagaria et al. 40 |
| 9 | Research and Development | In the orthopaedic field, the important direction of this technology is for the development of personalised prostheses and metallic implants Cobalt-chromium alloy, Ti6Al4V, and stainless steel types of material are used for manufacturing By using CAD file, AM technologies easily manufactured customised shape implants It makes more promising of research and development of orthopaedic implants |
Wong, 2; Horn et al. 9 |
| 10 | Cost | AM is efficient for low volume production which can create complex & customised components with lesser cost No expensive toolings are required and produce an implant with low waste As a result, there is a reduction of cost |
Kumar et al. 41; Javaid and Haleem, 1 |
| 11 | Complexity | Conventional manufacturing technologies are not flexible to manufacture complex shape implant in less time AM technologies are available to print complicated shape product, implants, medical tools and instruments Thin and complicated shape scaffolds accurately follow the contour of bone are easily manufactured which is not previously possible |
Starosolski et al. 42; Schmauss et al. 43 |
| 12 | Improve Communication | 3D model printed by this technology enables to improve the communication between doctors/surgeon and patient It plays an important role to build effective communication for proper healthcare Doctors can now provide appropriate information to the patient Provide better understanding of treatment outcomes |
Javaid and Haleem, 1; Tevanov et al. 44; |
AM has the potential to create an anatomic model so that patient anatomy can be examined easily by the surgeon in a concrete way as compared to 2D radiological images. AM can be used for comparing a normal anatomic model with a customised printed specially for complex shapes. A 3 D model of fractures bone model, provide a better understanding of the fracture to the surgeon as compared to the 2D/3D image on the screen. A 3D printed model can accurately show various features such as dislocation of the articular surfaces and joint fragmentations. In surgical planning, these elements aid in plate positioning and screw measurement. AM easily create 3D implants and the applications of these implants are used to repair a range of bone structures.
8. Some significance development
AM is used in many cases of orthopaedics to solve the present day challenges. Companies successfully implement this technology for the production of implants and surgical instruments because one human body differs from another. Some significant developments made by AM in orthopaedic are as follows:
-
•
Design and development of orthopaedic implants
-
•
Examination of defect bone geometry
-
•
Provides a better understanding to doctors about the patient
-
•
Provides a better idea for performing the operation
-
•
Reduces operation time
-
•
Manufactures exact fit bone implants
-
•
Produces lightweight implants with excellent surface quality
-
•
Print 3D model of multi-materials that represent a different section of bone, soft tissue and organ for a clear understanding of the patient body.
-
•
Increases the success rate of operation of the patient
-
•
Improvement in the quality of life of the patient.
-
•
Artificial bone produced that used to replaced defective areas.
-
•
Finally, surgeon's job becomes easy by the use patient fit implant and fulfils the requirement of highly individualised products with maximum flexibility.
As compared to conventional method of implant production this technology has increasing benefits. By CAD data it produces patient-specific parts with high quality without any additional tool requirement. The application of this technology minimises unpleasant side effects and optimises patient treatment. AM technologies are expanding their capabilities to fulfil various challenges of optimisation of design and manufacturing performance. It continuously changes the way of orthopaedic product and become more competitive and efficient in a global marketplace.
9. Discussion
AM is an evolving technological platform that seems to have extensive applications in various areas of medicine. It can produce complex shape prototype with a wide variety of materials and also the implants of biocompatible materials that meet structural requirements. This technology makes surgeon job easier with minimum side effects which meet various challenges of orthopaedics. 3D printed model gives a better understanding of complex pathology and anatomy of patients that are suitable for surgical training. Technology has potential to make lightweight, durable, and geometrically complex objects. There is an improvement in the quality of life of the patient and efficiently solve the problem in Medical. Thus lowering the operation cost and improving cooperation between engineer, surgeon and the patient. In future, additive manufacturing will fulfil more challenges in orthopaedics because the human body is different; this technology creates implants that fit perfectly and quickly accepted by the body of the patient. The surgeons print an implant to practice before the surgery. One of the advantages of the 3D printed implant is that the shape and size match with the excised bone site and onto existing bone it lowering the pressure as compared to conventional implant.
10. Limitations and future scope
The main limitation of this technology is the conversion of scan data into STL format which is time-consuming. AM technologies, software and material, cost these technologies is high. The strength of part is another limitation of this technology.
In future with the help of additive manufacturing applications, orthopaedic surgeons will embrace the knowledge. The applications of these technologies will helpful in clinical practices are used to develop the planning. Implant with inherent geometric freedom is the flexibility of this technology. In future, this technology will become perfect for personalised digital medicine. The application of patient customised 3D printed models of bone may become standard in surgical simulation, preoperative planning, implant development and intra-operative guidance. Its' application is for the reconstruction of large bone defects that optimally fit implant with proper dimensions before performing the surgery.
11. Conclusion
Additive manufacturing is used efficiently in orthopaedics for a replica of the bone which helps for various treatments of bones. The current status shows continuously increasing research work undertaken by additive manufacturing applications and challenges in the field of orthopaedic. This technique is incorporated in pre-surgical planning and clinical practice. Information of defected bone is collected easily by CT and MRI scan and printed by this technology. This provides a virtual model of patient anatomy that successfully provides planning about patient-specific orthopaedic procedures. AM is used for providing education to implant designing and pre-operative planning to training. For medical applications, this technology becomes prevalent and creates manufacturing flexibility. Additive manufacturing in orthopaedics will experience a rapid translation in future because due to its geometric freedom it fulfils various challenges. It successfully produces anatomic models for the planning of surgery, fabrication of complex custom implants for education and training. Technology tends to convert any idea or requirement into reality. Additive manufacturing technologies create an on-demand production of customised surgical instruments otherwise not available easily, due to its rare use and prohibitive cost. 3D printed bone, and biologic implants are used to orthopaedics restoration of function and original structure and have potential to design and develop tools for doctors and surgeons.
Conflict of interest
None.
Contributor Information
Mohd. Javaid, Email: mjavaid@jmi.ac.in.
Abid Haleem, Email: ahaleem@jmi.ac.in.
References
- 1.Javaid M., Haleem A. Additive manufacturing applications in orthopaedics: a review. J Clin Orthop Trauma. 2018 doi: 10.1016/j.jcot.2018.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wong K.C. 3D-printed patient-specific applications in orthopedics. Orthop Res Rev. 2016;8:57–66. doi: 10.2147/ORR.S99614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vaish A., Vaish R. 3D printing and its applications in orthopedics. J Clin Orthop Trauma. 2018 doi: 10.1016/j.jcot.2018.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Javaid M., Haleem A. Additive manufacturing applications in medical cases: a literature-based review. Alexandria J Med. 2017 [Google Scholar]
- 5.Vaishya R., Lal H. Learn through innovation, research and publication. J Clin Orthop Trauma. 2016;7:219–220. doi: 10.1016/j.jcot.2016.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Salmi M., Tuomi J., Paloheimo K.S., Björkstrand R., Paloheimo M., Salo J., Kontio R., Mesimäki K., Mäkitie A.A. Patient-specific reconstruction with 3D modeling and DMLS additive manufacturing. Rapid Prototyp J. 2012;18:209–214. [Google Scholar]
- 7.Javaid M., Kumar L., Kumar V., Haleem A. Product design and development using polyjet Rapid prototyping technology. Control Theory Inf. 2015;5:12–19. [Google Scholar]
- 8.Hoang D., Perrault D., Stevanovic M., Ghiassi A. Surgical applications of three-dimensional printing: a review of the current literature & how to get started. Ann Transl Med. 2016;4(23):1–19. doi: 10.21037/atm.2016.12.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Horn T.J., Harrysson O.L.A., West H.A., Little J.P., Marcellin-Little D.J. Development of a patient-specific bone analog for the biomechanical evaluation of custom implants. Rapid Prototyp J. 2014;20(1):41–49. [Google Scholar]
- 10.Costello J.P., Olivieri L.J., Krieger A., Thabit O., Marshall M.B., Yoo S.J., Kim P.C., Jonas R.A., Nath D.S. Utilizing Three-dimensional printing technology to assess the feasibility of High-fidelity synthetic ventricular septal defect models for simulation in medical education. World J Pediatr Congenit Heart Surg. 2014;5:421–426. doi: 10.1177/2150135114528721. [DOI] [PubMed] [Google Scholar]
- 11.Lee V., Singh G., Trasatti J.P., Bjornsson C., Xu X., Tran T.N., Yoo S.S., Dai G., Karande P. Design and fabrication of human skin by three-dimensional bioprinting. Tissue Eng Part C Methods. 2014;20:473–484. doi: 10.1089/ten.tec.2013.0335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhou C., Chen Y., Yang Z., Khoshnevis B. Digital material fabrication using mask image projection based stereolithography. Rapid Prototyp J. 2013;19:153–165. [Google Scholar]
- 13.Bens A., Seitz H., Bermes G., Emons M., Pansky A., Roitzheim B., Tobiasch E., Tille C. Non toxic flexible photopolymers for medical stereolithography technology. Rapid Prototyp J. 2007;13:38–47. [Google Scholar]
- 14.Sing S.L., Yeong W.Y., Wiria F.E., Tay B.Y., Zhao Z., Zhao L., Tian Z., Yang S. Direct selective laser sintering and melting of ceramics: a review. Rapid Prototyp J. 2017;23:611–623. [Google Scholar]
- 15.Deckers J.P., Shahzad K., Cardon L., Rombouts M., Vleugels J., Kruth J.P. Shaping ceramics through indirect selective laser sintering. Rapid Prototyp J. 2016;22:544–558. [Google Scholar]
- 16.Wysocki B., Maj P., Sitek R., Buhagiar P., Kurzydłowski K.J., Swieszkowski W. Laser and electron beam additive manufacturing methods of fabricating titanium bone implants. Appl Sci. 2017;7:1–20. [Google Scholar]
- 17.Gibbons G.J., Hansell R.G. Direct tool steel injection mould inserts through the arcam EBM free form fabrication process. Assembly Autom. 2005;25(4):300–305. [Google Scholar]
- 18.Gale J., Achuhan A. Application of ultrasonic peening during DMLS production of 316L stainless steel and its effect on material behavior. Rapid Prototyp J. 2017;23:1185–1194. [Google Scholar]
- 19.Kechagias J. An experimental investigation of the surface roughness of parts produced by LOM process. Rapid Prototyp J. 2007;13(1):17–22. [Google Scholar]
- 20.Park J., Tari M.J., Hahn H.T. Characterization of the laminated object manufacturing (LOM) process. Rapid Prototyp J. 2000;6(1):36–50. [Google Scholar]
- 21.Armillotta A., Bianchi S., Cavallaro M., Minnella S. Edge quality in fused deposition modeling: II. experimental verification. Rapid Prototyp J. 2017;23:686–695. [Google Scholar]
- 22.Singh R. Some investigations for small sized product fabrication with FDM for plastic components. Rapid Prototyp J. 2013;19:58–63. [Google Scholar]
- 23.Guo Y., Patanwala H.S., Bognet B., Ma A.W.K. Inkjet and inkjet-based 3D printing: connecting fluid properties and printing performance. Rapid Prototyp J. 2017;23(3):562–576. [Google Scholar]
- 24.Yang M., Lv X., Liu X., Zhang J. Research on color 3D printing based on color adherence. Rapid Prototyp J. 2018;24(1):37–45. [Google Scholar]
- 25.Mancanares C.G., Zancul E.D.S., Silva J.C.D., Miguel P.A.C. Additive manufacturing process selection based on parts’ selection criteria. Int J Adv Manuf Technol. 2015;80(5):1007–1014. [Google Scholar]
- 26.Moore J.P., Williams C.B. Fatigue properties of parts printed by PolyJet material jetting. Rapid Prototyping J. 2015;21:675–685. [Google Scholar]
- 27.Kan C.W., Yuen C.W.M. Digital ink-jet printing on textiles. Res J Textile Apparel. 2012;16:1–24. [Google Scholar]
- 28.El-Wahab H.A., El-Molla M.M., Lin L. Preparation and characterisation of ink formulations for jet printing on nylon carpet. Res J Textile Apparel. 2012;16:24–33. [Google Scholar]
- 29.Vaishya R., Vijaya V., Krishnan B.M., Agarwala A.K. Fallacies of CT based component size prediction in total knee arthroplasty – are patient-specific instruments the answer? J Clin Orthop Trauma. 2017 doi: 10.1016/j.jcot.2017.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Srivastava A., Aggarwal A.N., Mishra P., Bhateja D. Femoral fracture acting as an “ominous masquerade’’ in a 7-year-old child. J Clin Orthop Trauma. 2016;7:27–29. doi: 10.1016/j.jcot.2016.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cai H. Application of 3D printing in orthopedics: status quo and opportunities in China. Ann Transl Med. 2015;(Suppl 1):S12. doi: 10.3978/j.issn.2305-5839.2015.01.38. May 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Verma T., Sharma A., Sharma A., Maini L. Customized iliac prosthesis for reconstruction in giant cell tumour: a unique treatment approach. J Clin Orthop Trauma. 2016 doi: 10.1016/j.jcot.2016.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lal H., Kumar L., Kumar R., Boruah T., Jindal P.K., Sabharwal V.K. Inserting pedicle screws in lumbar spondylolisthesis – the easy bone conserving way. J Clin Orthop Trauma. 2017 doi: 10.1016/j.jcot.2016.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Morrison R.J., Kashlan K.N., Flanangan C.L., Wright J.K., Green G.E., Hollister S.J., Weatherwax K.J. Regulatory considerations in the design and manufacturing of implantable 3D-printed medical devices. Clin Transl Sci. 2015;8:594–600. doi: 10.1111/cts.12315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yap Y.L., Tan Y.S.E., Tan H.K.J., Peh Z.K., Low X.Y., Yeong W.Y., Tan C.S.H., Laude H. 3D printed bio-models for medical applications. Rapid Prototyping J. 2017;23(2):227–235. [Google Scholar]
- 36.Chung K.J., Hong-do Y., Kim Y.T., Yang I., Park Y.W., Kim H.N. Preshaping plates for minimally invasive fixation of calcaneal fractures using a real-size 3D-printed model as a preoperative and intraoperative tool. Foot Ankle Int. 2014;35:1231–1236. doi: 10.1177/1071100714544522. [DOI] [PubMed] [Google Scholar]
- 37.Cohen A., Laviv A., Berman P., Nashef R., Abu-Tair J. Mandibular reconstruction using stereolithographic 3-dimensional printing modeling technology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:661–666. doi: 10.1016/j.tripleo.2009.05.023. [DOI] [PubMed] [Google Scholar]
- 38.Rose A.S., Webster C.E., Harrysson O.L., Formeister E.J., Rawal R.B., Iseli C.E. Pre-operative simulation of pediatric mastoid surgery with 3D-printed temporal bone models. Int J Pediatr Otorhinolaryngol. 2015;79:740–744. doi: 10.1016/j.ijporl.2015.03.004. [DOI] [PubMed] [Google Scholar]
- 39.Kim G.B., Lee S., Kim H., Yang B.H., Kim Y.H., Kyung Y.S., Kim C.S., Choi S.H., Kim B.J., Ha H., Kwon S.U., Kim N. Three-dimensional printing: basic principles and applications in medicine and radiology. Korean J Radiol. 2016;17:182–197. doi: 10.3348/kjr.2016.17.2.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bagaria V., Deshpande S., Rasalkar D.D., Bhawan A.K., Paunipagar B.K. Use of rapid prototyping and three-dimensional reconstruction modeling in the management of complex fractures. Eur J Radiol. 2011;80:814–820. doi: 10.1016/j.ejrad.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 41.Kumar L., Tanveer Q., Kumar V., Javaid M., Haleem A. Developing low cost 3 d printer. Int J Appl Sci Eng Res. 2016;5:433–447. [Google Scholar]
- 42.Starosolski Z.A., Kan J.H., Rosenfeld S.D., Krishnamurthy R., Annapragada A. Application of 3-d printing (rapid prototyping) for creating physical models of pediatric orthopedic disorders. Pediatr Radiol. 2014;44:216–221. doi: 10.1007/s00247-013-2788-9. [DOI] [PubMed] [Google Scholar]
- 43.Schmauss D., Gerber N., Sodian R. Three-dimensional printing of models for surgical planning in patients with primary cardiac tumors. J Thorac Cardiovasc Surg. 2013;145:1407–1408. doi: 10.1016/j.jtcvs.2012.12.030. [DOI] [PubMed] [Google Scholar]
- 44.Tevanov L., Liciu E., Chirila M.O., Dusca A., Ulici A. The use of 3D printing in improving patient-doctor relationship and malpractice prevention. Rom J Leg Med. 2017;25:279–282. [Google Scholar]