Graphical abstract
Keywords: Left ventricular aneurysm, Pediatrics, Trauma, Cardiac magnetic resonance imaging
Highlights
-
•
LV aneurysms are rare in the pediatric population.
-
•
Given different implications, it is key to distinguish aneurysm and pseudoaneurysm.
-
•
The authors describe multimodality imaging to manage a pediatric LV aneurysm.
Introduction
Left ventricular (LV) aneurysms are a rare finding in the pediatric population. True aneurysms can be defined as congenital or acquired. In contrast to adults with true aneurysms, in whom myocardial infarction is the predominant cause, the most common cause of acquired aneurysms in pediatrics is blunt-force trauma, classically found following a motor vehicle accident. We present the unusual case of a 9-year-old boy who developed an LV aneurysm following a motor vehicle accident. He was initially managed conservatively. Because of symptomatic worsening, he underwent aneursymectomy and ventricular repair.
Case Presentation
A previously healthy 9-year-old boy presented to the pediatric emergency department following a motor vehicle accident resulting in blunt-force trauma to the chest and abdomen. He was riding in the back of a truck when he fell out. He was subsequently run over by a trailer in tow. When his father found him, he was lying on the ground crying. Emergency medical services were called immediately.
He was awake and alert upon arrival to the emergency department. His only reported symptom was right ankle pain. He denied chest pain, shortness of breath, or palpitations. Physical examination demonstrated a well-developed boy in no apparent distress. He had good central and distal pulses in all four extremities. His precordium was active, with a normal S1 and a physiologically split S2 with inspiration. A II/VI, high-pitched, S1-coincident murmur was heard throughout systole at the left sternal border. His lungs were clear to auscultation bilaterally. His liver edge was not palpable. Standard trauma surveillance computed tomographic imaging revealed a small laceration in the posterior lobe of the left lower lung, a small splenic laceration, a tiny laceration of the right kidney, and a nondisplaced fracture of the right sacrum. Initial laboratory investigation demonstrated elevated troponin T at 4.55 ng/mL. After initial stabilization, the patient was transferred to the pediatric intensive care unit for further management.
His electrocardiogram demonstrated sinus rhythm with nonspecific t-wave flattening in leads II, III, and aVF. Chest radiography demonstrated a normal cardiothymic silhouette with normal pulmonary vascularity and no evidence of parenchymal lung disease. Because of the elevated troponin T level and abnormal electrocardiographic findings, pediatric cardiology was consulted for further recommendations.
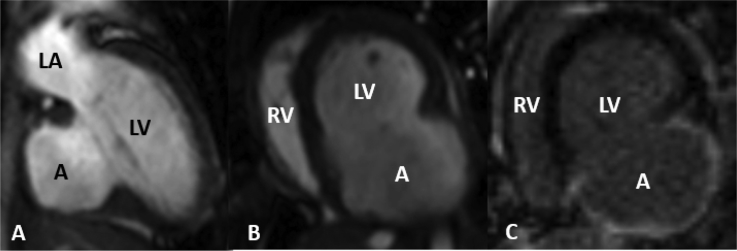
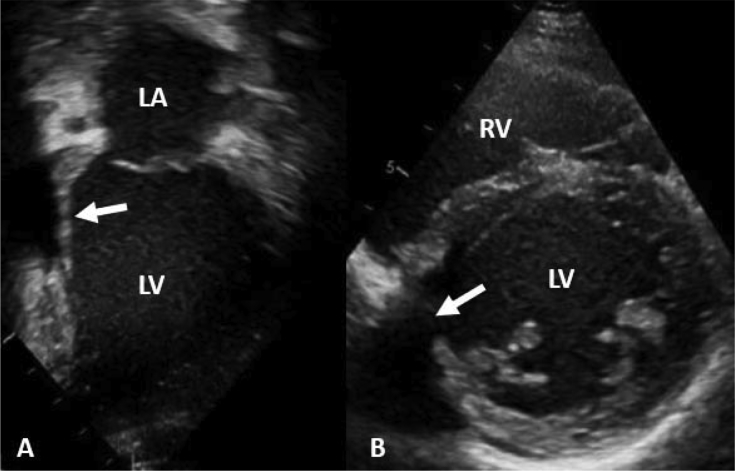
The patient's initial transthoracic echocardiogram demonstrated a small aneurysm in the inferior portion of the LV wall (Figures 1A and 1B). The wall of the aneurysm was thin and hypokinetic. His overall LV ejection fraction appeared normal. There was a small muscular ventricular septal defect near the aneurysm. There was no evidence of a pericardial effusion.
Figure 1.
Transthoracic echocardiography in the apical two-chamber (A) and parasternal short-axis (B) views. A, Aneurysm; LV, left ventricle; RV, right ventricle.
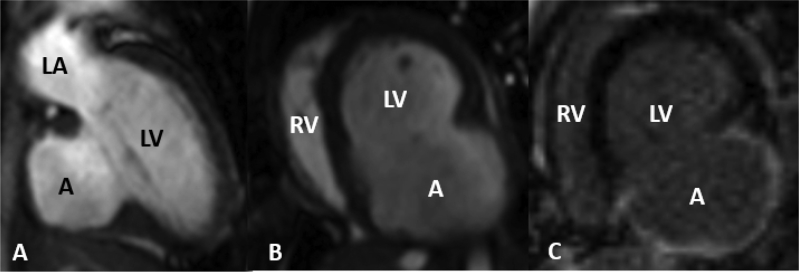
Although transthoracic echocardiography appeared diagnostic in this case, cardiac magnetic resonance imaging (CMR; Figures 2A and 2B) was performed for better anatomic delineation and medical decision making due to the rarity of pediatric LV aneurysms. CMR demonstrated a basal to mid inferior and inferoseptal LV aneurysm measuring 3.7 × 1.7 cm. The aneurysmal myocardial wall was thin and hypokinetic. The overall LV ejection fraction was 58%. Late gadolinium enhancement demonstrated near transmural hyperenhancement in the inferior and inferoseptal segments of the LV wall surrounding the aneurysm (Figure 2C). The findings were consistent with an LV aneurysm. On the basis of the known mechanism of injury and confirmation of a true LV aneurysm, we opted for conservative management. The patient was discharged home 10 days after admission following recovery from noncardiac injuries.
Figure 2.
Multiplanar cardiac magnetic resonance imaging. Electrocardiographically gated, breath-hold steady-state free precession cine images in the ventricular two-chamber (A) and short-axis (B) views. (C) Myocardial delayed enhancement imaging in the ventricular short-axis view. A, Aneurysm; LA, left atrium; LV, left ventricle; RV, right ventricle.
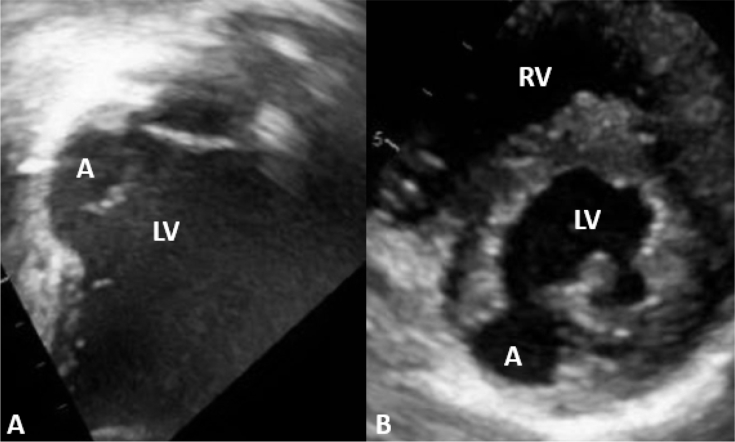
Six weeks later, the patient presented to our emergency department with palpitations. He was admitted to the pediatric acute care cardiology service for further evaluation. On continuous telemetry monitoring, he was noted to have a 22-beat run of asymptomatic nonsustained monomorphic ventricular tachycardia. Repeat transthoracic echocardiography (Figures 3A and 3B, Videos 1 and 2) demonstrated interval enlargement of the aneurysm. The wall of the aneurysm was dyskinetic.
Figure 3.
Transthoracic echocardiography in the apical two-chamber (A) and parasternal short-axis (B) views. A, Aneurysm; LV, left ventricle.
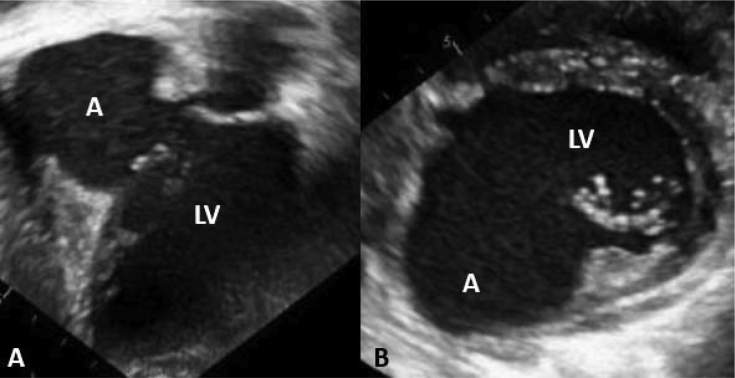
Because of significant enlargement of the LV aneurysm with the development of nonsustained monomorphic ventricular tachycardia, we elected to proceed with surgical repair. CMR was repeated to provide the surgical team valuable anatomic information about the location of the defect and the potential viability of the adjacent myocardium. CMR (Figures 4A and 4B, Videos 3 and 4) demonstrated a basal to mid inferior and inferoseptal LV aneurysm now measuring 4.4 × 5.8 cm with a neck measuring 3.5 cm. The aneurysmal myocardial wall was very thin and dyskinetic. There was no evidence of thrombus within the aneurysm. Late gadolinium enhancement imaging demonstrated transmural hyperenhancement in the inferior segment of the LV wall surrounding the aneurysm (Figure 4C).
Figure 4.
Multiplanar CMR. Electrocardiographically gated, breath-hold steady-state free precession cine images in the ventricular two-chamber (A) and short-axis (B) views. (C) Myocardial delayed enhancement imaging in the ventricular short-axis view. A, Aneurysm; LA, left atrium; LV, left ventricle; RV, right ventricle.
At surgery, a large, thin myocardial outpouching consistent with a true aneurysm was found in the inferior left ventricle. An aneurysmectomy was performed, and the ventriculotomy was closed with an oval endoventricular Gore-Tex patch (Figure 5). Histologic examination of the excised tissue confirmed a true LV aneurysm. The patient's postoperative course was uneventful. His discharge echocardiogram revealed normal LV systolic function. His systolic function remains normal in the 12 months following surgery (Figures 6A and 6B).
Figure 5.
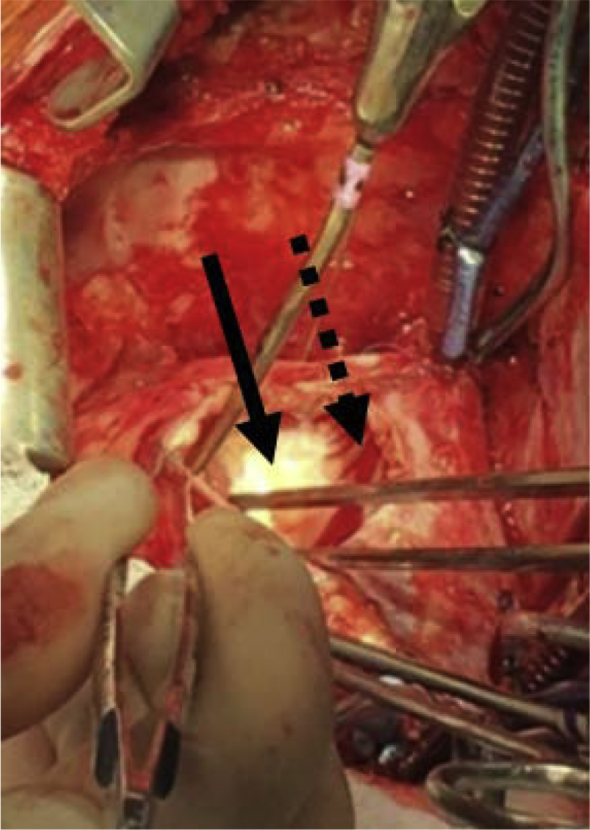
Surgical closure of ventriculotomy using an oval endoventricular Gore-Tex patch. Solid arrow indicates Gore-Tex patch; dashed arrow indicates viable myocardium.
Figure 6.
Transthoracic echocardiography in the apical two-chamber (A) and parasternal short-axis (B) views. Arrows indicate the Gore-Tex patch. LA, Left atrium; LV, left ventricle; RV, right ventricle.
Discussion
An LV aneurysm is a dyskinetic pouch with wide connection to the ventricle involving the full thickness of the ventricular wall on histologic examination.1 LV aneurysms are a rare finding in the pediatric population. They can be either congenital or acquired. Congenital causes include intrinsic abnormalities in the embryogenesis of the muscular ventricular wall, ischemia secondary to congenital coronary stenosis or hypoplasia, or viral infection.1 Acquired causes include blunt trauma, myocardial infarction, infection, and as a complication of cardiovascular surgery.2 Whereas congenital aneurysms often present in the neonatal period, acquired aneurysms tend to present months to years after the inciting event.
The majority of aneurysms following blunt-force trauma are true aneurysms, whereas pseudoaneurysms typically occur following penetrating trauma. Although the exact pathogenesis remains unclear, true LV aneurysms are thought to result from either a transmural myocardial contusion and subsequent necrosis or trauma-induced thrombosis of a coronary artery causing ischemia.2
Echocardiography is the method of choice for the diagnosis of aneurysms in younger children.1 As children grow, their acoustic windows become more challenging; therefore, CMR is important in diagnosis and long-term follow-up. Typical findings of a true ventricular aneurysm using CMR include intact epicardial fat, a neck/body width ratio > 0.9, and hyperenhancement within the wall of the aneurysm on delayed gadolinium enhancement.3, 4, 5, 6, 7
There is a paucity of evidence regarding the management of LV aneurysms in the pediatric population. Although some suggest immediate surgical intervention, many have advocated for a more conservative approach. In asymptomatic adults, true aneurysms have a low risk for rupture, whereas pseudoaneurysms require urgent intervention. In the adult literature, indications for intervention on a true LV aneurysm include refractory congestive heart failure, ventricular arrhythmias, or thrombus formation with systemic emboli.2, 8, 9
Following the evidence presented in the adult literature, we initially opted to manage our patient conservatively. Given the rapid expansion of the aneurysm over the course of a few weeks and the documentation of ventricular tachycardia, we felt that surgical intervention was necessary.
Conclusion
A true LV aneurysm is a rare phenomenon in children. The natural history and appropriate management strategy for acquired aneurysms are largely unknown in children. Although multiple case reports have suggested that LV aneurysms often develop years after the inciting event, this report highlights the importance of close outpatient follow-up in pediatric patients with true LV aneurysms.10, 11 Echocardiography and CMR are invaluable tools in the management of LV aneurysms in older children following blunt-force trauma.
Footnotes
Conflicts of interest: The authors report no actual or potential conflicts of relative to this document.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.case.2018.08.002.
Supplementary Data
Transthoracic echocardiography in the apical two-chamber view. A, Aneurysm.
Transthoracic echocardiography in the parasternal short-axis view. A, Aneurysm.
Multiplanar CMR. Electrocardiographically gated, breath-hold steady-state free precession cine images in the ventricular two-chamber view. A, Aneurysm.
Multiplanar CMR. Electrocardiographically gated, breath-hold steady-state free precession cine images in the ventricular short-axis view. A, Aneurysm.
References
- 1.Marijon E., Phalla O., Concordet S., Le Bidois J., Sidi D., Bonnet D. Diagnosis and outcome in congenital ventricular diverticulum and aneurysm. J Thorac Cardiovasc Surg. 2006;131:433–437. doi: 10.1016/j.jtcvs.2005.09.046. [DOI] [PubMed] [Google Scholar]
- 2.Veeragandham R.S., Backer C.L., Mavroudis C., Wilson A.D. Traumatic left ventricular aneurysm and tricuspid insufficiency in a child. Ann Thorac Surg. 1998;65:247–248. doi: 10.1016/s0003-4975(98)00380-4. [DOI] [PubMed] [Google Scholar]
- 3.Cho M.N., Mehta S.K., Matulevicius S., Weinstein D., Wait M.A., McGuire D.K. Differentiating true versus pseudo left ventricular aneurysm: a case report and review of diagnostic strategies. Cardiol Rev. 2006;14:e27–e30. doi: 10.1097/01.crd.0000233756.66532.45. [DOI] [PubMed] [Google Scholar]
- 4.Duvernoy O., Wikstrom G., Mannting F., Larsson S.G., Andren B., Dubiel T. Pre- and postoperative CT and MR in pseudoaneurysms of the heart. J Comput Assis Tomogr. 1992;16:401–409. doi: 10.1097/00004728-199205000-00011. [DOI] [PubMed] [Google Scholar]
- 5.Gill S., Rakhit D.J., Ohri S.K., Harden S.P. Left ventricular true and false aneurysms identified by cardiovascular magnetic resonance. Br J Radiol. 2011;84:e35–e37. doi: 10.1259/bjr/25590962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kumbasar B., Wu K.C., Kamel I.R., Lima J.A.C., Bluemke D.A. Left ventricular true aneurysm: diagnosis of myocardial viability shown on MR imaging. AJR Am J Roentgenol. 2002;179:472–474. doi: 10.2214/ajr.179.2.1790472. [DOI] [PubMed] [Google Scholar]
- 7.Sharma K., Kumar S. Overview of left ventricular outpouchings on cardiac magnetic resonance imaging. Cardiovasc Diagn Ther. 2015;5:464–470. doi: 10.3978/j.issn.2223-3652.2015.11.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grondin P., Kretz J.G., Bical O., Donzeau-Gouge P., Petitclerc R., Campeau L. Natural history of saccular aneurysms of the left ventricle. J Thorac Cardiovasc Surg. 1979;77:57–64. [PubMed] [Google Scholar]
- 9.Shapira O.M., Davidoff R., Hilkert R.J., Aldea G.S., Fitzgerald C.A., Shemin R.J. Repair of left ventricular aneurysm: long-term results of linear repair versus endoaneurysmorraphy. Ann Thorac Surg. 1997;63:701–705. doi: 10.1016/s0003-4975(96)01112-5. [DOI] [PubMed] [Google Scholar]
- 10.Grieco J.G., Montoya A., Sullivan H.J., Bakhos M., Foy B.K., Blakeman B. Ventricular aneurysm due to blunt chest injury. Ann Thorac Surg. 1989;47:3229. doi: 10.1016/0003-4975(89)90306-8. [DOI] [PubMed] [Google Scholar]
- 11.Jorden J., Dietz R. Traumatic ventricular aneurysm. N Engl J Med. 1997;336:625. doi: 10.1056/NEJM199702273360905. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Transthoracic echocardiography in the apical two-chamber view. A, Aneurysm.
Transthoracic echocardiography in the parasternal short-axis view. A, Aneurysm.
Multiplanar CMR. Electrocardiographically gated, breath-hold steady-state free precession cine images in the ventricular two-chamber view. A, Aneurysm.
Multiplanar CMR. Electrocardiographically gated, breath-hold steady-state free precession cine images in the ventricular short-axis view. A, Aneurysm.