1. Introdution: rotator cuff tears and their management
Tears of the rotator cuff tendons remain a common source of pain and disability among the adult population. Age appears to be the most common aetiology, with 25% of individuals in their 60s and in 50% of individuals in their 80s being found to have rotator cuff tears.1
Codman first described the anatomy of the rotator cuff in 19342 and the concept of the insertional “footprint” was first introduced by Curtis in 1999.3
A successful repair of the rotator cuff tendons is dependent on multiple factors. Anatomic factors are of paramount importance. These include restoration of the footprint contact area,4 tendon and bone quality,5 adequate compression of the tendon on the footprint to facilitate healing6 and minimized motion at the bone–tendon interface.7 Intrinsic factors such as poor vascular supply, hypoxia, tendon atrophy, fibrocartilaginous changes and fatty infiltration of the cuff muscles have also been linked to suboptimal outcomes.5
The prevalence of partial thickness rotator cuff tears (PTRCTs) ranges from 15 to 32% in the general population, and is higher (40%) in the dominant arm of asymptomatic elite overhead athletes.8 In the past, the natural history of partial tears has been poorly understood. Recent evidence would suggest that tear progression is correlated with the percentage of tendon thickness involved on initial presentation. Patients with <50% tendon involvement had a 14% chance of tear progression, whereas patients with >50% tendon involvement progressed 55% of the time.9 Healing of PTRCTs does not appear to occur either spontaneously or with the aid of acromioplasty.10 Pain development in shoulders with an asymptomatic rotator cuff tear is associated with progression in tear size.9 Larger tears are more likely to develop pain in the short term than smaller tears.9
Given the relatively high re-tear rates in large and massive tears, it is generally accepted that the gold standard of management is repair, though some debate remains with regards to mini-open versus arthroscopic techniques. Systematic reviews have not shown a significant difference between the two techniques with regards to functional and pain scores or incidence of recurrent rotator cuff tears.11 Patients who do undergo arthroscopic repair do however suffer from decreased short term pain11 and fewer post op complications.12 There is also evidence to suggest that patients with Arthroscopic repair may return to work earlier.12
Adequate Initial fixation plays a key role in achieving successful healing with rotator cuff tears. A number of surgical techniques have been described for the repair of rotator cuff injuries. These include fixation both single- and double-row suture anchor techniques, transosseous tunnels or newer, knotless anchors.
Much debate exists over the gold standard surgical technique, in particular with regards to Single Vs Double row methods. For the purpose of this review we shall focus primarily on this particular controversy.
1.1. Surgical technique
With the single-row (SR) supraspinatus repair, two anchors are placed at the lateral edge of the footprint of the tendon's insertion. In the double-row (DR) supraspinatus repair, a medial row is typically placed just lateral to the articular margin and the lateral row is placed just medial to the drop of the greater tuberosity (Fig. 1, Fig. 2).
Fig. 1.
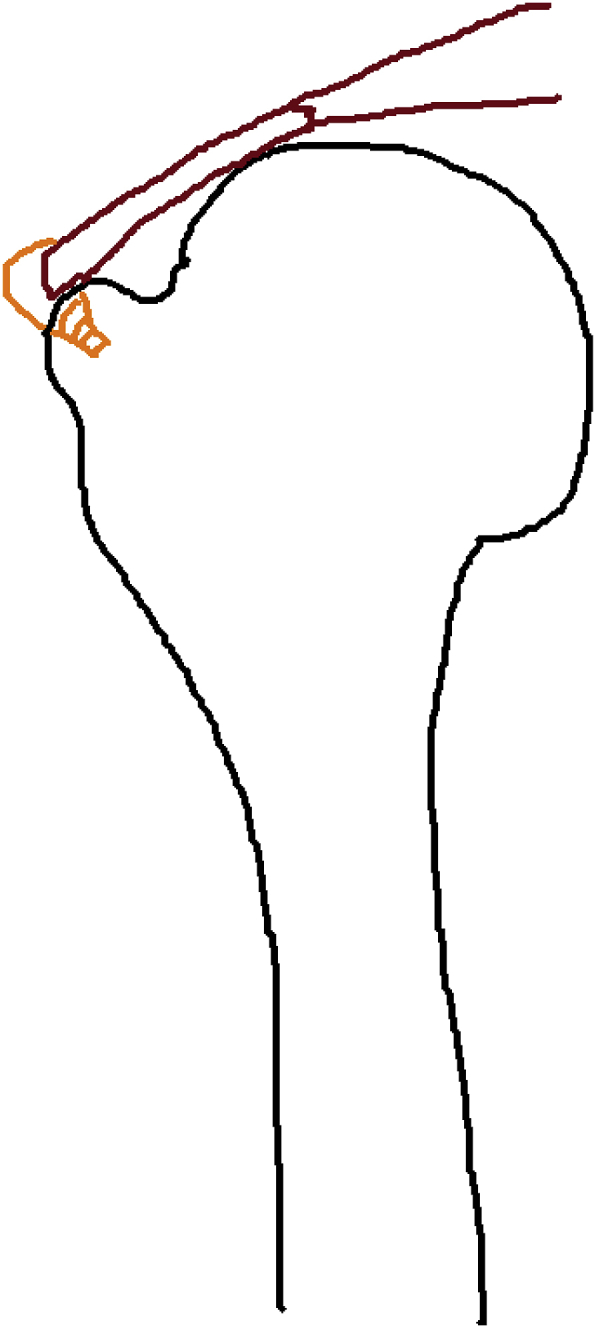
Single row technique.
Fig. 2.
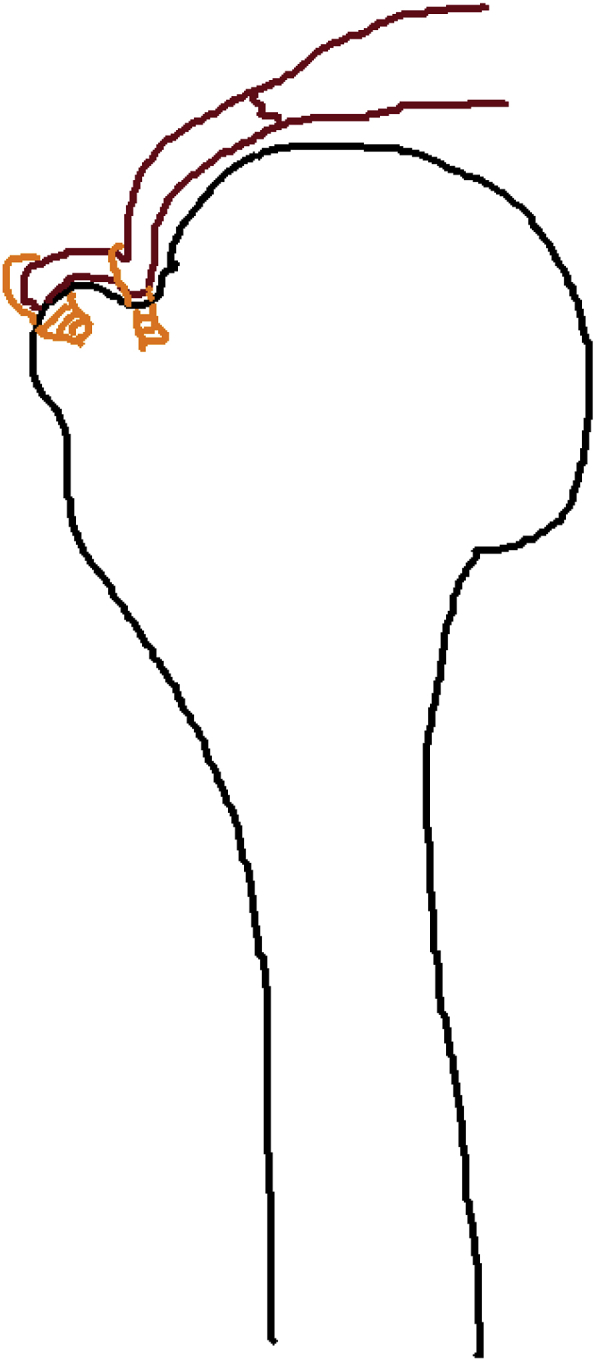
Double row technique.
1.2. Biomechanical studies
Ideally, the repair of a rotator cuff tear must have the potential to withstand physiological loads whilst simultaneously allowing healing to occur.13 The concept behind the use of a double row repair technique lies behind the rationale that the double-row suture repair recreates the native footprint more closely. This in turn results in significantly higher loads to failure and decreased gap formation under tensile loading.14 Several biomechanical studies have shown this to be true.15, 16, 17 While these studies - which are all cadaveric - would seem to indicate that the double row repair is a superior construct, the results of clinical trials are more controversial.
1.3. Clinical outcomes in randomised control trials
A number of randomised control trials (RCTs) comparing the two surgical techniques have been conducted. A study by Aydin et al., in 201018 on 64 patients split evenly into 2 groups with a minimum 2 year follow up showed no significant difference in clinical outcome (Constant score) compared with single-row repair in small to medium tears.
A prospective RCT by Nicholas et al.19 looking at 49 patients. This RCT found no advantage of DR repair compared with SR repair for medium, large, and massive rotator cuff tears in terms of outcome scores (ASES, Penn and SST), clinical tests of shoulder function, shoulder ROM, or shoulder strength.
These results are also borne out in larger trials such as that conducted by Lapner et al.20 No significant differences in functional or quality-of-life outcomes (ASES, WORC and Constant scores) were identified between single-row and double-row fixation techniques in a heterogenous group of patients with tears of all sizes.
A larger multicentre RCT by Carbonel et al.21 looked at 160 patients with a minimum 2 year follow up. These patients all had large, full thickness tears. The DR repair technique conferred significant difference in clinical outcomes (UCLA, Constant and ASES scores) compared with single-row repair. This was even more significant in large tears over 3 cm.
A prospective RCT on 53 patients by Ma et al.22 indicated that double-row fixation showed better shoulder strength in patients with larger tear size (>3 cm) in comparison with single-row fixation.
1.4. Clinical outcomes systematic reviews and meta analyses
A systematic review by Sobhy et al.23 found that within the domain of level I mid-term and short-term studies, DR repair showed improved UCLA scores only. ASES, Constant, WORC, and SANE scores showed no significant difference. The authors stipulated that this was due to lower partial-thickness re-tear rates of DR repairs. The authors also noted that long-term level III studies showed a direct correlation of both functional outcomes and cuff structural integrity, with significant superiority of DR over SR repair techniques.
A systematic review by Saridakis et al.24 reviewed six studies (Level III evidence and above) and found there was no significant difference between the single-row and double-row groups within each study in terms of postoperative clinical outcomes. The authors did however note that within their data, there was some evidence to support the use of DR repairs in patients with large (>3 cm) tears (level II evidence).
A systematic review and meta-analysis of 7 level I randomised clinical trials by Millett et al.25 concluded that there were no detectable differences in improvement in outcomes scores (ASES, UCLA and Constant) between single-row and double-row repairs.
A summary of 8 Meta-Analyses by Spiegl et al.26 (including 2 Level 1 studies and 5 level I and II studies) concluded that no clinical differences were seen between single-row and double-row repair for small and medium rotator cuff tears at either a short or medium term follow up.
1.5. Healing and re-rupture rates
A re-tear of the repaired rotator cuff tendon may be a significant clinical problem. Estimates of the re-tear vary widely between studies and range between 11% and 94%.27, 28, 29
Factors influencing a rotator cuff re-tear remain varied and include age, preoperative tear size, degree of muscular atrophy, degree of fatty infiltration, surgical technique, and inappropriate postoperative rehabilitation.30 It should be noted that no study to date has evaluated the re-tear rate with regard to the completeness of rotator cuff repair based on the extent of footprint coverage.30
Whether or not patients treated with rotator cuff repair do well regardless of the structural integrity of the repair remains controversial. Some studies within the literature suggest that patients with a re-rupture still have significant improvement compared to their preoperative state.27 Others studies directly contradict this, indicating that the absence of healing of the repaired rotator cuff is associated with inferior strength.31 There is still lack of high-level double blinded prospective studies that directly assess the impact of rotator cuff re-tear on the functional outcome, and a systematic review by Galanopoulos et al. was inconclusive.30
A systematic review by Duquin32 demonstrated significantly lower re-tear rates with DR repairs when compared to SR for large tears more than 10 mm in size. Millett et al.26 conducted a meta-analysis comparing SR with DR revealed significantly higher re-tear rates in SR repairs especially in partial thickness re-tears.
The aforementioned systematic review by Saredakis et al. indicated that two RCTs showed a significant difference in terms of structural healing of the rotator cuff tendons after surgery with the DR repairs.
In a randomised control trial involving 58 patients at high risk of shoulder stiffness, Franceschi et al.33 found that DR repair of the rotator cuff was associated with a lower re-tear rate if investigated with MRI at 2 years.
1.6. Cost
The DR technique has some known potential disadvantages. These include the fact that is more technically demanding, time-consuming and costly. These factors are particularly significant if DR repair is not associated with a significant improvement in clinical results.
Genuario et al.34 created a decision-analytic model in order to assess the cost-effectiveness of DR arthroscopic rotator cuff repair in comparison with single-row repair. Their model was created on the basis of the cost per quality-adjusted life year gained. Two cohorts of patients (one with tears of <3 cm and the other with a tear of = />3 cm) were evaluated. Data from the aforementioned systematic review of 1252 patients by Duquin was used to populate their model. They concluded that DR rotator cuff repair was not cost-effective for any size of tear.
Conversely, Huang et al.35 conducted a cost-utility analysis from the perspective of a publicly funded health-care system and used the aforementioned RCT by Lapner et al. as the basis for their analytic model.20 The findings of this RCT indicated that there “were no significant differences in functional or quality-of-life outcomes between single-row and double-row fixation techniques”. The authors double-row fixation was found to be more cost-effective than single-row fixation. Furthermore, a double-row reconstruction was found to be more economically attractive for larger rotator cuff tears (>3 cm).
2. Discussion
Surgical repair of the RC has been shown to been cost-effective solution to a rotator cuff tears that cause considerable burden on the general population in terms of quality of life. Nevertheless, the optimal technique for arthroscopic repair of the rotator cuff remains controversial. An ideal surgical technique involved in the repair of the RC tear must have the potential to withstand physiological loads while simultaneously allowing healing to occur and preventing re-rupture in the future.
While this would seem like an ideal concept overall, it fails to account for the wide heterogeneity within the population and the variety of methods used by individual surgeons. It is well known that a number of factors may influence both the chance of healing and the chance of re-rupture of the rotator cuff. These include: Initial tear size, muscle atrophy or fatty infiltration within the cuff, variety in repair methods, surgical skill, anchor type, number of sutures per anchor, suture technique, experience of the operating surgeon and rehab protocols.23
It would therefore seem incorrect to attempt to rationalise that one surgical technique would be superior to another whilst analysing patients with rotator cuff tears, as a large heterogenous group. For instance, if it is known that initial tear size has an impact of outcomes, then a study on a group of patients with a variety of tear sizes may produce results whose significance is difficult to interpret.
This may explain why RCTs looking at patients with tears of all sizes (Nicholas et al.19) or small to medium tears (Aydin et al.18) found no difference in functional outcome whereas studies looking at larger cuff tears (Carbonel et al.,21 Ma et al.22) showed both better shoulder strength and clinical outcomes.
The issue of heterogeneity is further compounded when Systematic reviews and meta analyses are considered and this would appear to explain why these studies show no difference is outcomes between the two techniques. Further confounding issues include study population sizes, different outcome variables (Different scoring systems, functional vs radiographic outcomes). The sample population sizes in the RCTS are often small and the length of follow up which is rarely more than 2 years. It is therefore difficult to gauge the long-term benefit of one technique over the other. In a systematic review of the literature in 2018, Sobhy et al.23 argued that “the inclusion of level II and level III trials or level I trials that do not strictly rely on both functional and radiographic evaluations creates a potential source of heterogeneity that interferes with accurate analysis of the relation of the function to the cuff integrity after both techniques”.
There is no clear consensus with regards to the financial viability of one technique over another. The outcomes of studies examining the cost effectiveness of each technique appear to be determined by end points and measures of cost set by the authors involved (which are different in each study). This matter is further complicated by the variability within the types of studies used. For instance one might assume that a cost analysis based on the population of a systematic review (Huang et al.35) may prove more powerful and significant than a study based on a RCT (Genuario et al.34). However, as mentioned above conglomerating such a large and disparate population may complicate rather than clarify any questions asked.
3. Conclusion
What is clear from the discussion is above is that there is a lack of clear consensus within the Level I evidence which is available. Table 1 summarises the evidence discussed in this review. What is clear is that those studies looking at tears separately appear to indicate superiority of the double row technique. More high-quality Level I studies on specifically homogenous groups are needed to guide practice and to identify characteristics of specific rotator cuff tears that would best be suited for the added expense involved in a double row repair. With consideration to the existing evidence, the authors conclude that the type of repair technique used should be selected according to tear size and surgical experience. Double row repairs should be ideally performed in those with larger tears or those patients undergoing accelerated rehabilitation.
Table 1.
A summary of the existing evidence.
| Study | Study type | Type of tears | Findings |
|---|---|---|---|
| Aydin et al. | RCT | All tears | No difference in outcome |
| Nicholas et al. | RCT | All tears | No difference outcome |
| Lapner et al. | Multicenter RCT | All tears | No difference outcome |
| Carbonel et al. | RCT | large tears >3 cm and small tears separately | improvement in function in both groups, greater in the large tears |
| Ma et al. | RCT | large tears >3 cm and small tears separately | improvement in function in large tears |
| Sobhy et al. | Systematic review | All tears | Improved UCLA scores with DR repair |
| Saridakis et al. | Systematic review | large tears >3 cm and small tears separately | no significant difference in postoperative clinical outcomes, weak evidence to supprt DR in large tears |
| Millett et al. | Systematic review | All tears | No difference outcome |
| Spiegl et al. | Systematic review | All tears | No difference outcome |
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jcot.2019.01.027.
Contributor Information
Al-achraf Khoriati, Email: alkhoriati@doctors.org.uk.
Tony Antonios, Email: tantonios@doctors.org.uk.
Abhinav Gulihar, Email: abhinav.gulihar@nhs.net.
Bijayendra Singh, Email: bijayendra.singh@nhs.net.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Yamamoto A., Takagishi K., Osawa T. Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg. 2010;19(1):116–120. doi: 10.1016/j.jse.2009.04.006. [DOI] [PubMed] [Google Scholar]
- 2.Codman E. 1934. The Shoulder; Rupture of the Supraspinatus Tendon and Other Lesions in or about the Subacromial Bursa. [Google Scholar]
- 3.Curtis A.S., Burbank K.M., Tierney J.J., Scheller A.D., Curran A.R. The insertional footprint of the rotator cuff: an anatomic study. Arthrosc J Arthrosc Relat Surg. 2006;22(6):603–609. doi: 10.1016/j.arthro.2006.04.001. e1. [DOI] [PubMed] [Google Scholar]
- 4.Roth K.M., Warth R.J., Lee J.T., Millett P.J., ElAttrache N.S. Arthroscopic single-row versus double-row repair for full-thickness posterosuperior rotator cuff tears: a critical analysis review. JBJS Rev. 2014;2(7) doi: 10.2106/JBJS.RVW.M.00081. [DOI] [PubMed] [Google Scholar]
- 5.Lee T.Q. Current biomechanical concepts for rotator cuff repair. Clin Orthop Surg. 2013;5(2):89–97. doi: 10.4055/cios.2013.5.2.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Park M.C., Cadet E.R., Levine W.N., Bigliani L.U., Ahmad C.S. Tendon-to-Bone pressure distributions at a repaired rotator cuff footprint using transosseous suture and suture anchor fixation techniques. Am J Sports Med. 2005;33(8):1154–1159. doi: 10.1177/0363546504273053. [DOI] [PubMed] [Google Scholar]
- 7.Ahmad C.S., Stewart A.M., Izquierdo R., Bigliani L.U. Tendon-bone interface motion in transosseous suture and suture anchor rotator cuff repair techniques. Am J Sports Med. 2005;33(11):1667–1671. doi: 10.1177/0363546505278252. [DOI] [PubMed] [Google Scholar]
- 8.Connor P.M., Banks D.M., Tyson A.B., Coumas J.S., D'Alessandro D.F. Magnetic resonance imaging of the asymptomatic shoulder of overhead athletes: a 5-year follow-up study. Am J Sports Med. 2003;31(5):724–727. doi: 10.1177/03635465030310051501. [DOI] [PubMed] [Google Scholar]
- 9.Mall N.A., Kim H.M., Keener J.D. Symptomatic progression of asymptomatic rotator cuff tears: a prospective study of clinical and sonographic variables. J Bone Joint Surg-Am. 2010;92(16):2623–2633. doi: 10.2106/JBJS.I.00506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kartus J., Kartus C., Rostgård-Christensen L., Sernert N., Read J., Perko M. Long-term clinical and ultrasound evaluation after arthroscopic acromioplasty in patients with partial rotator cuff tears. Arthroscopy. 2006;22(1):44–49. doi: 10.1016/j.arthro.2005.07.027. [DOI] [PubMed] [Google Scholar]
- 11.Lindley K., Jones G.L. Outcomes of arthroscopic versus open rotator cuff repair: a systematic review of the literature. Am J Orthoped. 2010;39(12):592–600. [PubMed] [Google Scholar]
- 12.Agrawal V., Stinson M. Ability and length of time to return to work after RCR in workers' compensation patient. Indiana Orthopaedic Journal. 2008;2:49. [Google Scholar]
- 13.Yadav H., Nho S., Romeo A., MacGillivray J.D. Rotator cuff tears: pathology and repair. Knee Surg Sports Traumatol Arthrosc. 2009;17(4):409–421. doi: 10.1007/s00167-008-0686-8. [DOI] [PubMed] [Google Scholar]
- 14.Hohmann E., König A., Kat C.-J., Glatt V., Tetsworth K., Keough N. Single- versus double-row repair for full-thickness rotator cuff tears using suture anchors. A systematic review and meta-analysis of basic biomechanical studies. Eur J Orthop Surg Traumatol. 2018;28(5):859–868. doi: 10.1007/s00590-017-2114-6. [DOI] [PubMed] [Google Scholar]
- 15.Ahmad C.S., Kleweno C., Jacir A.M. Biomechanical performance of rotator cuff repairs with humeral rotation: a new rotator cuff repair failure model. Am J Sports Med. 2008;36(5):888–892. doi: 10.1177/0363546508316285. [DOI] [PubMed] [Google Scholar]
- 16.Esquivel A.O., Duncan D.D., Dobrasevic N., Marsh S.M., Lemos S.E. Load to failure and stiffness: anchor placement and suture pattern effects on load to failure in rotator cuff repairs. Orthopaed J Sports Med. 2015;3(4) doi: 10.1177/2325967115579052. 2325967115579052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ma C.B., Comerford L., Wilson J., Puttlitz C.M. Biomechanical evaluation of arthroscopic rotator cuff repairs: double-row compared with single-row fixation. J Bone Joint Surg. 2006;88(2):403–410. doi: 10.2106/JBJS.D.02887. [DOI] [PubMed] [Google Scholar]
- 18.Aydin N., Kocaoglu B., Guven O. Single-row versus double-row arthroscopic rotator cuff repair in small- to medium-sized tears. J Shoulder Elbow Surg. 2010;19(5):722–725. doi: 10.1016/j.jse.2009.11.053. [DOI] [PubMed] [Google Scholar]
- 19.Nicholas S.J., Lee S.J., Mullaney M.J. Functional outcomes after double-row versus single-row rotator cuff repair: a prospective randomized trial. Orthopaed J Sports Med. 2016;4(10) doi: 10.1177/2325967116667398. 232596711666739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lapner P.L.C., Sabri E., Rakhra K. A multicenter randomized controlled trial comparing single-row with double-row fixation in arthroscopic rotator cuff repair. J Bone Joint Surg Am. 2012;94(14):1249–1257. doi: 10.2106/JBJS.K.00999. [DOI] [PubMed] [Google Scholar]
- 21.Carbonel I., Martinez A.A., Calvo A., Ripalda J., Herrera A. Single-row versus double-row arthroscopic repair in the treatment of rotator cuff tears: a prospective randomized clinical study. Int Orthop. 2012;36(9):1877–1883. doi: 10.1007/s00264-012-1559-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ma H.-L., Chiang E.-R., Wu H.-T.H. Clinical outcome and imaging of arthroscopic single-row and double-row rotator cuff repair: a prospective randomized trial. Arthroscopy. 2012;28(1):16–24. doi: 10.1016/j.arthro.2011.07.003. [DOI] [PubMed] [Google Scholar]
- 23.Sobhy M.H., Khater A.H., Hassan M.R., El Shazly O. Do functional outcomes and cuff integrity correlate after single- versus double-row rotator cuff repair? A systematic review and meta-analysis study. Eur J Orthop Surg Traumatol. 2018;28(4):593–605. doi: 10.1007/s00590-018-2145-7. [DOI] [PubMed] [Google Scholar]
- 24.Saridakis P., Jones G. Outcomes of single-row and double-row arthroscopic rotator cuff repair: a systematic review. J Bone Joint Surg Am. 2010;92(3):732–742. doi: 10.2106/JBJS.I.01295. [DOI] [PubMed] [Google Scholar]
- 25.Millett P.J., Warth R.J., Dornan G.J., Lee J.T., Spiegl U.J. Clinical and structural outcomes after arthroscopic single-row versus double-row rotator cuff repair: a systematic review and meta-analysis of level I randomized clinical trials. J Shoulder Elbow Surg. 2014;23(4):586–597. doi: 10.1016/j.jse.2013.10.006. [DOI] [PubMed] [Google Scholar]
- 26.Spiegl U.J., Euler S.A., Millett P.J., Hepp P. Summary of meta-analyses dealing with single-row double-row repair techniques for rotator cuff tears. Open Orthop J. 2016;10(Suppl 1):330–338. doi: 10.2174/1874325001610010330. M9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Galatz L.M., Ball C.M., Teefey S.A., Middleton W.D., Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004;86-A(2):219–224. doi: 10.2106/00004623-200402000-00002. [DOI] [PubMed] [Google Scholar]
- 28.Harryman D.T., Mack L.A., Wang K.Y., Jackins S.E., Richardson M.L., Matsen F.A. Repairs of the rotator cuff. Correlation of functional results with integrity of the cuff. J Bone Joint Surg. 1991;73(7):982–989. [PubMed] [Google Scholar]
- 29.Lafosse L., Brzoska R., Toussaint B., Gobezie R. The outcome and structural integrity of arthroscopic rotator cuff repair with use of the double-row suture anchor technique. Surgical technique. J Bone Joint Surg Am. 2008;90(Suppl 2 Pt 2):275–286. doi: 10.2106/JBJS.H.00388. [DOI] [PubMed] [Google Scholar]
- 30.Galanopoulos I., Ilias A., Karliaftis K., Papadopoulos D., Ashwood N. The impact of Re-tear on the clinical outcome after rotator cuff repair using open or arthroscopic techniques – a systematic review. Open Orthop J. 2017;11(Suppl-1):95–107. doi: 10.2174/1874325001711010095. M4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Boileau P., Brassart N., Watkinson D.J., Carles M., Hatzidakis A.M., Krishnan S.G. Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal? J Bone Joint Surg Am. 2005;87(6):1229–1240. doi: 10.2106/JBJS.D.02035. [DOI] [PubMed] [Google Scholar]
- 32.Duquin T.R., Buyea C., Bisson L.J. Which method of rotator cuff repair leads to the highest rate of structural healing?: a systematic review. Am J Sports Med. 2010;38(4):835–841. doi: 10.1177/0363546509359679. [DOI] [PubMed] [Google Scholar]
- 33.Franceschi F., Papalia R., Franceschetti E. Double-row repair lowers the retear risk after accelerated rehabilitation , double-row repair lowers the retear risk after accelerated rehabilitation. Am J Sports Med. 2016;44(4):948–956. doi: 10.1177/0363546515623031. [DOI] [PubMed] [Google Scholar]
- 34.Genuario J.W., Donegan R.P., Hamman D. The cost-effectiveness of single-row compared with double-row arthroscopic rotator cuff repair. J Bone Joint Surg-Am. 2012;94(15):1369–1377. doi: 10.2106/JBJS.J.01876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Huang A.L., Thavorn K., van Katwyk S., MacDonald P., Lapner P. Double-row arthroscopic rotator cuff repair is more cost-effective than single-row repair. J Bone Joint Surg. 2017;99(20):1730–1736. doi: 10.2106/JBJS.16.01044. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


