Abstract
Despite an abundance of information about frozen shoulders, larger prospective studies on the outcomes of intervention are limited. The purpose of our study was to assess the functional and clinical outcomes with a further aim to analyse the independent effects of diabetes and BMI.
A prospective cohort study of all 210 primary frozen shoulders over a 12 – month period was analysed. The Oxford Shoulder score was used to assess functional outcomes before and after interventions. Further demographic data was collected. The effect of interventions including steroid injections, arthroscopic release and manipulation was analysed.
54% patients responded to intra-articular steroid injections. Patients with recalcitrant symptoms (46%) had an arthroscopic release. Failure of initial injection therapy was higher in diabetes [70%] than non-diabetes [44%] patients. After surgery, the Oxford shoulder score improved from a mean of 41.6 to 27.2 at 3 months [p < 0.05]. 85% of patients had satisfactory resolution of symptoms with external rotation improving from a mean of 10.5 ° to 61.3 ° [p < 0.05]. There was no statistical significance in outcomes of patients with BMI of >_30 and <30.
Understanding the outcomes of surgical intervention is important in counselling patients with frozen shoulder. We found that patients with diabetes had higher failure rates of conservative management and increasing needs for multiple surgery but complete resolution of symptoms can still be achieved and that BMI status in isolation was not a predictor of poorer outcome.
Keywords: Frozen shoulder, Outcomes, Diabetes, Obesity
1. Introduction
Frozen shoulder is a disabling and painful condition that is commonly managed in the primary care setting. Frozen shoulder has a protracted natural history that usually ends in resolution.1
The consensus definition from the American Shoulder and Elbow Surgeons Society (ASES) is that frozen shoulder “is a condition characterised by functional restriction of both active and passive shoulder motion for which radiographs of the glenohumeral joint are essentially unremarkable except for the possible presence of osteopenia or calcific tendonitis”.2
Adhesive capsulitis is characterised by gradual increase in stiffness and pain. This self-limiting disorder has three stages with the mean duration of 30 months for untreated cases with some subsequent restricting of movement of the shoulder1, 3, 4.
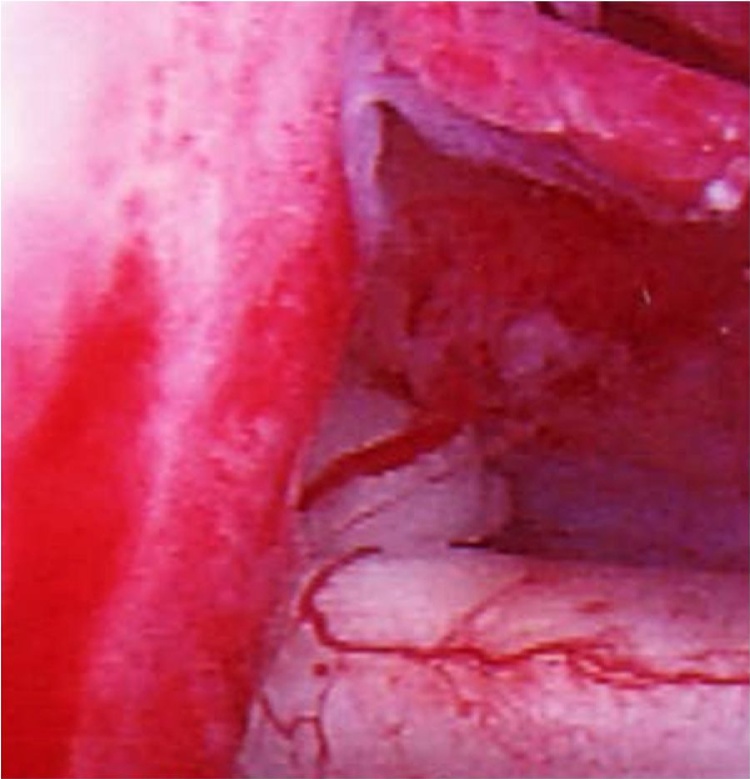
The incidence of frozen shoulder is only <2%. The exact aetiology of frozen shoulder is not known.4 Type III collagen, fibroblasts and myofibroblasts have been demonstrated in the capsule of a frozen shoulder, similar to the histology of Dupuytren’s disease.5 It has been suggested that vascular endothelial growth factor (VEGF) may have a role in neovascularisation (Fig 1) associated with frozen shoulder.6
Fig. 1.
Arthroscopic picture of 62 year old male with frozen shoulder showing neovascularization.
Forms of treatment include conservative (i.e. steroid injection, physiotherapy) and operative (i.e. distension arthrography, manipulation under anaesthesia and arthroscopic release)13, 14, 15, 16. When conservative management has failed arthroscopic release and MUA provides effective benefit.17, 18, 19
Inferior outcomes have been reported in diabetics,17, 20 though also there has been reports that show no difference between the two groups.21, 22
Despite an abundance of information about frozen shoulders, larger prospective studies on the outcomes of intervention are limited. There are no studies looking at the effect of obesity and frozen shoulder to the best of our knowledge.
The purpose of our study was to assess the functional and clinical outcomes with a further aim to analyse the independent effect of diabetes and BMI
2. Materials and methods
We conducted a prospective study on the outcome of treatment of primary frozen shoulder in a cohort of 210 consecutive patients. Institutional approval was obtained prior to the review of surgical logs at Royal Derby Hospital Trauma & Orthopaedics Department. Only patients with idiopathic frozen shoulder were recruited from 4 specialist upper limb clinics. Patients were included in the study if they had a painful shoulder with global restriction of active and passive movements and a normal rotator cuff and a normal x-ray. All patients underwent a trial of non-operative treatment including steroid injection, physiotherapy and home exercises for at least six months prior to surgery. Exclusion criteria included presence of other pathology (i.e. rheumatological disorders, neurological disorders, disorders of the cervical spine), secondary frozen shoulder (shoulder stiffness with cuff disease, fracture, calcific tendonitis) and stiffness post injury or post rotator cuff disease.
2.1. Clinical evaluation
Each subject completed a comprehensive questionnaire (Oxford Shoulder Score-OSS) that included items regarding current pain and functional level before and after any interventions.
2.2. Interventions
All patients had initial conservative management- glenohumeral intra-articular injection of Triamcinolone 40 mg and 10mls 0.5% Bupivacaine was given and all patients had supervised physiotherapy post injection.
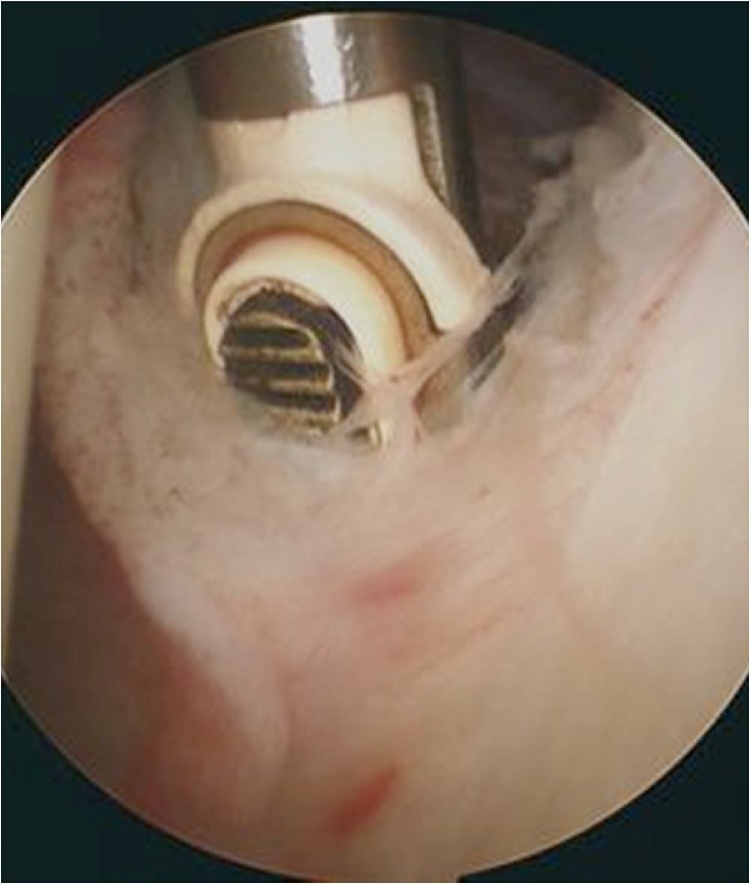
Those that had recalcitrant symptoms went on to have arthroscopic release as a day case surgery under general anaesthesia. Surgical release was standardised to include the release of anterior capsule, rotator interval, coracohumeral ligament and thickened MGHL (Fig 2) and all patients had supervised physiotherapy started immediately after surgery.
Fig. 2.
Arthroscopic picture of release of anterior capsule.
2.3. Statistical analysis
Statistical analysis was performed using the Mann–Whitney U test. The mean and standard deviations (SD) were calculated for variables in both groups and compared. A p-value of <0.05 was considered statistically significant.
3. Results
Our cohort was made of 130 females and 80 males with a mean age of 55 (range, 33–77). The median duration of symptoms prior to first clinic appointment was 11 months (range, 3–24 months). 22% (n = 46 patients) had diabetes and 37% (n = 78 patients) had BMI >_30 (obese). Prior to the first visit 63.8% (n = 132) had physiotherapy and 63% (n = 132) had at least one cortisone injection. The correct diagnosis had been made in 30% of patients, no diagnosis given in 40% and the incorrect diagnosis given in the remaining 30%.
53.8% (n = 113) of patients responded well to conservative measures (i.e. steroid injection and physiotherapy). Patients with recalcitrant symptoms [n = 97] had an arthroscopic release.
Out of the patients with BMI >30 (n = 78), 37 were successfully treated with non-operative intervention, leaving 41 patients to undergo arthroscopic capsular release. Failure of initial treatment (injection therapy and physiotherapy) was higher in the diabetic group 70% (n = 32) than non-diabetic 44% (n = 72) patients (p < 0.05). Furthermore 25% (n = 8) of patients with diabetes who underwent surgery needed further surgical intervention compared to 10% in non-diabetics, (i.e. steroid injection or arthroscopic release) (p < 0.05)
The post-operative improvement at 3 months in the OSS improved from 17.9 to 33 and in the range of movement, i.e. ER, from 10.5 to 61.3° (Fig. 3). 85% (n = 82) of patients had satisfactory resolution of symptoms. The minimum follow-up was 12 months.
Fig. 3.
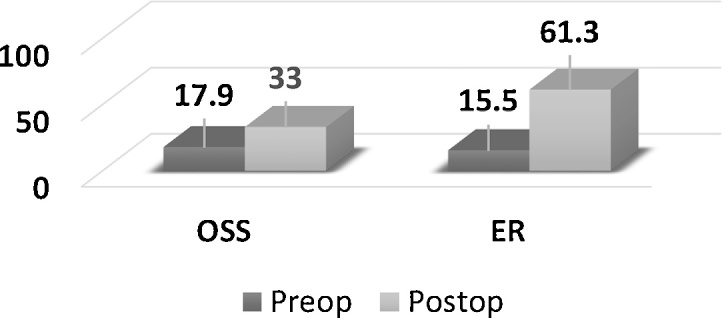
Pre-operative and post-operative OSS and ER (p < 0.01).
Final functional results for the ninety-seven subjects with complete preoperative and postoperative clinical data were compared between diabetics and non-diabetics (Table 1).
Table 1.
DM and non-DM group mean scores differences after surgery.
| Mean Oxford Shoulder Score Differences (OSS) | ||||
|---|---|---|---|---|
| Preop | 3 mths | 6 mths | 12 mths | |
| DM (n = 46) |
19 | 26.6 | 30.9 | 33.4 |
| Non-DM (n = 51) |
17.5 | 34.4 | 28.9 | 30 |
| p-value | – | <0.01 | <0.01 | 0.603 |
| Mean External Rotation Diffreences (ER) | ||||
|---|---|---|---|---|
| Preop | 3 mths | 6 mths | 12 mths | |
| DM (n = 46) | 3.9 | 58.7 | 25.8 | 29.7 |
| Non-DM (n = 51) | 14.5 | 62.8 | 50.6 | 48.3 |
| p-value | – | 0.509 | 0.017 | 0.8 |
Final functional results for the ninety-seven subjects with complete preoperative and postoperative clinical data were compared between obese (BMI >30) and non-obese (Table 2).
Table 2.
Obese and non-obese group mean scores differences after surgery.
| Mean Oxford Shoulder Score (OSS) | ||||
|---|---|---|---|---|
| Preop | 3 mths | 6 mths | 12 mths | |
| Obese (n = 41) | 17.9 | 29.5 | 20.3 | 32.7 |
| Non-obese (n = 56) | 18.2 | 35.6 | 30.9 | 37.7 |
| p-value | – | 0.036 | 0.582 | 0.810 |
| Mean External Rotation (ER) | ||||
|---|---|---|---|---|
| Preop | 3 mths | 6 mths | 12 mths | |
| Obese (n = 41) | 17.5 | 60.7 | 43.5 | 30 |
| Non-obese (n = 56) | 8.4 | 60.9 | 37.7 | 34.6 |
| p-value | – | 0.904 | 0.771 | 0.459 |
Significant improvement of range of movement at 3 months are seen in all groups, though at further follow-up a progressive loss of external rotation is noted in all patients undergoing arthroscopic capsular release.
4. Discussion
These results confirm that the efficacy of intraarticular cortisone is less effective in patients with diabetes. Both diabetic and non-diabetic patients undergoing arthroscopic release had good outcomes but the initial greater post-operative improvement in those without diabetes confirms the findings in other studies.17, 22 Suggestions have been made that the outcome after manipulation under anaesthesia is similar in both groups.21
An association between frozen shoulder and diabetes [DM] has been well described. The reported incidence of frozen shoulder in Type I DM is up to 10% and up to 29% in Type II DM. Although the duration of diabetes has been correlated with frozen shoulder, a definite association with glycosylated hemoglobin A1c (HbA1c) levels has not been proven.7 Frozen shoulder is common in type 2 diabetes, as are other musculoskeletal disorders of the upper limb with abnormal collagen deposition such as cheiroarthropathy and Dupuytren’s disease.8 The advanced glycation end products formed in diabetes have been implicated in abnormal collagen cross-linking, leading to fibrosis.9, 10 All these studies attempt to provide reasoning for the delay in response to treatment in diabetic patients. The cause of frozen shoulder in diabetes may be multifactorial.11, 12
Obesity represents a major public health problem and carries with it the risk of developing significant medical problems. The global burden of obesity is rising at an alarming rate. The World Health Organization estimates that more than one billion people are overweight and of these, 300 million are obese. 23 Obesity is associated with a range of disabling musculoskeletal conditions in adults. As the prevalence of obesity increases, the societal burden of these chronic musculoskeletal conditions, in terms of disability, health-related quality of life, and health-care costs, also increases. No studies to date have shown an association between frozen shoulder and obesity, though due to high incidence of obesity it is not unexpected that we will continue to treat a large number of obese patients with frozen shoulder. Our study shows that BMI in isolation is not a predictor of surgical success.
Adhesive capsulitis has a protracted natural history, most patients having symptoms up to three years. The purpose of treatment is to relieve pain and hasten recovery. Reporting early postoperative results give a more accurate postoperative outcome. Up to 40% of patients with untreated frozen shoulder have persistent symptoms at mean follow-up of 4.4 years.24
A survey done in the UK that included 303 health care professionals showed that 50% of them would prefer surgery during the resolution phase. However, 57% of responders were physiotherapists, and some did not consider surgery at all. Reasons for this included lack of resources and the belief that symptoms would resolve over time.25
The objective of surgery is to hasten recovery i.e. reduce the duration of symptoms and our study shows that early improvement of symptoms is provided in all groups.
In conclusion, understanding the outcomes of frozen shoulder management is important in counselling patients with this condition. Although frozen shoulder has protracted natural history, resolution of symptoms is achieved. We found that patients with diabetes responded less well to conservative management and arthroscopic release. These patients may require further measures for symptom resolution, but complete resolution of symptoms is still achieved. BMI in isolation is not a predictor of surgical success. Progressive loss of external rotation was seen at follow-up in all treatment groups.
Conflict of interest
The authors declare that they have no conflict of interest. There is no funding source. This article does not contain any studies with human participants or animals performed by any of the authors.
References
- 1.Reeves B. The natural history of the frozen shoulder syndrome. Scand J Rheumatol. 1975;4(4):193–196. doi: 10.3109/03009747509165255. [DOI] [PubMed] [Google Scholar]
- 2.Zuckerman J.D., Rokito A. Frozen shoulder: a consensus definition. J Shoulder Elbow Surg. 2011;20:322–325. doi: 10.1016/j.jse.2010.07.008. [DOI] [PubMed] [Google Scholar]
- 3.Grey R.G. The natural history of idiopathic frozen shoulder. J Bone Joint Surg (A) 1978;60(4):564. [PubMed] [Google Scholar]
- 4.Dias R., Cutts S., Massoud S. Frozen shoulder. BMJ. 2005;331:1453–1456. doi: 10.1136/bmj.331.7530.1453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bunker T.D. Frozen shoulder: unravelling the enigma. Ann R Coll Surg Engl. 1997;79:210–213. [PMC free article] [PubMed] [Google Scholar]
- 6.Ryu J.D., Kirpalani P.A., Kim J.M. Expression of vascular endothelial growth factor and angiogenesis in the diabetic frozen shoulder. J Shoulder Elbow Surg. 2006;15:679–685. doi: 10.1016/j.jse.2006.01.002. [DOI] [PubMed] [Google Scholar]
- 7.Yian E.H., Contreras R., Sodl J.F. Effects of glycemic control on prevalence of diabetic frozen shoulder. J Bone Joint Surg Am. 2012;94:919–923. doi: 10.2106/JBJS.J.01930. [DOI] [PubMed] [Google Scholar]
- 8.Aydeniz A., Gursoy S., Guney E. Which musculoskeletal complications are most frequently seen in type 2 diabetes mellitus? J Int Med Res. 2008;36:505–511. doi: 10.1177/147323000803600315. [DOI] [PubMed] [Google Scholar]
- 9.Rosenbloom A.L., Silverstein J.H. Connective tissue and joint disease in diabetes mellitus. Endocrinol Metab Clin North Am. 1996;25:473–483. doi: 10.1016/s0889-8529(05)70335-2. [DOI] [PubMed] [Google Scholar]
- 10.Monnier V.M., Glomb M., Elgawish A., Sell D.R. The mechanism of collagen crosslinking in diabetes: a puzzle nearing resolution. Diabetes. 1996;45(Suppl 3):S67–S72. doi: 10.2337/diab.45.3.s67. [DOI] [PubMed] [Google Scholar]
- 11.Cinar M., Akpinar S., Derincek A., Circi E., Uysal M. Comparison of arthroscopic capsular release in diabetic and idiopathic frozen shoulder patients. Arch Orthop Trauma Surg. 2010;130:401–406. doi: 10.1007/s00402-009-0900-2. [DOI] [PubMed] [Google Scholar]
- 12.Berghs B.M., Sole-Molins X., Bunker T.D. Arthroscopic release of adhesive capsulitis. J Shoulder Elbow Surg. 2004;13:180–185. doi: 10.1016/j.jse.2003.12.004. [DOI] [PubMed] [Google Scholar]
- 13.(a) van Royen B. Int Orthop SICOT. 1996;20:207. doi: 10.1007/s002640050064. [DOI] [PubMed] [Google Scholar]; (b) Hamdan T., Al-Essa K. Int Orthop (SICOT) 2003;27:107. doi: 10.1007/s00264-002-0397-6. [DOI] [PubMed] [Google Scholar]
- 14.Othman A., Taylor G. Int Orthop (SICOT) 2002;26(268) doi: 10.1007/s00264-002-0348-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sharma S. Management of frozen shoulder – conservative vs surgical? Ann R Coll Surg Engl. 2011;93:343–344. doi: 10.1308/147870811X582080. discussion 345–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Maund E., Craig D., Suekarran S. Management of frozen shoulder: a systematic review and cost-effectiveness analysis. Health Technol Assess. 2012;16(11):1–264. doi: 10.3310/hta16110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ogilvie-Harris D.J., Biggs D.J., Fitsialos D.P., MacKay M. The resistant frozen shoulder: manipulation versus arthroscopic release. Clin Orthop Relat Res. 1995;319:238–248. [PubMed] [Google Scholar]
- 18.Ide J., Takagi K. Early and long-term results of arthroscopic treatment for shoulder stiffness. J Shoulder Elbow Surg. 2004;13:174–179. doi: 10.1016/j.jse.2003.11.001. [DOI] [PubMed] [Google Scholar]
- 19.Le Lievre H.M., Murrell G.A. Long-term outcomes after arthroscopic capsular. J Bone Joint Surg Am. 2016 doi: 10.2106/JBJS.J.00952. [DOI] [PubMed] [Google Scholar]
- 20.Pollock R.G., Duralde X.A., Flatow E.L., Bigliani L.U. The use of arthroscopy in the treatment of resistant frozen shoulder. Clin Orthop Relat Res. 1994 [PubMed] [Google Scholar]
- 21.Wang J.P., Huang T.F., Ma H.L. International Orthopaedics (SICOT) 2010;34(1227) doi: 10.1007/s00264-010-0968-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hand C., Clipsham K., Rees J.L., Carr A.J. Long-term outcome of frozen shoulder. J Shoulder Elbow Surg. 2008;17:231–236. doi: 10.1016/j.jse.2007.05.009. [DOI] [PubMed] [Google Scholar]
- 23.World Health Organisation. 2006, http://www.who.int/dietphysicalactivity/publications/facts/obesity/en/.
- 24.Rill B.K., Fleckenstein C.M., Levy M.S., Nagesh V., Hasan S.S. Predictors of outcome after nonoperative and operative treatment of adhesive capsulitis. Am J Sports Med. 2011;39:567–574. doi: 10.1177/0363546510385403. [DOI] [PubMed] [Google Scholar]
- 25.Dennis L., Brealey S., Rangan A., Rookmoneea M., Watson J. Managing idiopathic frozen shoulder: a survey of health professionals’ current practice and research priorities. Shoulder Elbow. 2010;2:294–300. [Google Scholar]