Abstract
A prospective, comparative study was done over a period of 3 years to compare the complications and functional results of two treatment modalities of unstable intertrochanteric fractures of the femur in the elderly; i.e closed reduction and internal fixation (CRIF) with proximal femur nail (PFN) and primary cemented hemireplacement arthroplasty (HRA) with bipolar prosthesis. 100 elderly patients with unstable intertrochanteric fractures of femur were studied over a period of 3 years. 50 patients underwent CRIF with PFN and 50 patients were treated with primary cemented hemireplacement arthroplasty with bipolar prosthesis. Harris Hip score analysis revealed that the difference between the patients treated with cemented hemiarthroplasty and proximal femoral nailing was statistically significant in favour of the hemiarthroplasty group within the first 3 months. However, this difference diminished at the 6th month time point and reversed at the 12 month time point indicating a better functional outcome of Proximal Femur Nail in the long term. Although cemented hemireplacement arthhroplasty allows early pain free mobilization and has a good short term outcome, over time it is associated with a variety of complications which significantly affects quality of life of patients. On the other hand, although patients treated with PFN had delayed post op mobilization, they had better results when followed up at 1 year post surgery.
Keywords: Unstable intertrochanteric femur, Proximal femur nail, Cemented hemireplacement arthroplasty
1. Introduction
As the life expectancy of elderly population has been steadily rising, there is a significant increase in the incidence of hip fractures, and it also expected to further rise in the coming decade.1 90% of hip fractures in the elderly are contributed nearly equally by fractures of neck and femur and intertrochanteric fractures.2 The accepted modality of treatment of intertrochanteric fractures in the elderly is by osteosynthesis, preferably with intrameduallary nails.3 Fixation with these devices allows for early mobilization and weight bearing which is necessary to prevent complications like bed sores, pulmonary infections, deep vein thrombosis etc.4 Due to the rising incidence of intertrochanteric fractures and its common association with osteoporosis, complications of fixation with intramedullary devices have been unveiled like cut through of screws, loss of fixation and excessive collapse.5 An implant failure rate of up to 50% has been recorded in the treatment of unstable intertrochanteric fractures.6 A need for a viable alternative to internal fixation of intertrochanteric fractures with intramedullary nails has thus arisen, and cemented hemireplacement arthroplasty has been noted to give acceptable results by many studies 7, 8, 9 as it allows early mobilization and return to previous activity level at the earliest. A study by Osman Rodop et al.10 who treated 54 elderly patients with unstable intertrochanteric fractures with primary cemented bipolar prosthesis concluded that short term advantages seemed to give a significant advantage to the elderly in terms of outcome, but long term complications need to be studied and taken into account due to the increase in life expectancy world over.
Therefore this study was undertaken to compare the complications and functional outcome of patients with unstable intertrochanteric fracture of femur treated with closed reduction and internal fixation with proximal femur nail and primary cemented hemireplacement arthroplasty with bipolar prosthesis and review the results reported in literature.
2. Materials and methods
2.1. Source of data
The study was conducted in the Department of Orthopaedics, K.R Hospital, Mysore Medical College and Research Institute, Mysuru, between January 2012 to January 2016. The study was a prospective, randomised study. Randomization was done after we had taken written informed consent from the study participants and obtained base line information. The random assignment scheme was created from a table of random numbers.
2.2. Sample size
A total of 100 patients admitted with unstable intertrochanteric fractures were studied. 50 of them were randomly chosen to be treated with CRIF with proximal femur nail, and the remaining 50 were treated with primary cemented hemiarthroplasty with bipolar prosthesis.
Keeping confidence level of 95% and confidence interval of 9.8%, with an incidence of Unstable Intertrochanteric fracture of around 200 per 105 population per year aged above 65 years, a sample size of 100 was obtained.
2.3. Inclusion criteria
All patients aged more than 75 years and less than 85 years with unstable intertrochanteric fracture of femur (according to Evans classification) were included into the study.
Patient with Stable intertrochanteric fracture of femur (according to Evans classification) and those unfit or unwilling for surgery, polytrauma patients, pathological fractures or those with compound fractures were excluded from the study. Patients initially included in the study, but who dropped out later, were excluded.
3. Treatment
In the PFN group of patients, Closed Reduction and Internal Fixation was done with the patient on a traction table with short or standard length proximal femur nails under fluoroscopic guidance. The average operating time was 38.4 min and average blood loss was 46 ml.
In the cemented hemiarthroplasty group, the patient was placed in the lateral position under anaesthesia and the fracture was exposed via the posterior approach. A bipolar prosthesis of appropriate size was fixed with 40 g of bone cement (poly methyl-methacrylate). The average operating time was 50.4 min and the average blood loss during the procedure was 187 ml.
4. Follow up and outcome
All operated cases were followed up in the outpatient department of K.R Hospital, Mysore at 3 weeks, 6 weeks, 3 months and 3 monthly thereafter. The primary outcome measures of the patients were based on Harri’s Hip Scoring (HHS) system and the Mean Mobility Score (MMS), which evaluated pain, walking capacity and examination findings. The secondary outcome measure was the incidence of complications in both the groups.
5. Results
The patients belonging to both groups were comparable in terms of demography, pre-existing comorbidities and mean interval between trauma and surgery (Table 1, Table 2, Table 3).
Table 1.
Comparison of preoperative data of the patients.
| Preoperative data | PFN group | Cemented Bipolar group |
|---|---|---|
| Number of patients | 50 | 50 |
| Mean age in years (SD) | 81.2 (7.8) | 78.7 (8.3) |
| Mean mobility score before fracture (SD) | 4.0 (2.1) | 4.1 (1.9) |
| Pre-existing comorbidities including cardiovascular disease, Respiratory disease and Diabetes. (%) | 64% | 60% |
| Mean interval between trauma and surgery in hours (SD) | 28.3 (7.3) | 30.4 (9.1) |
There was no significant difference between the two groups on the compared parameters [p > 0.05].
Table 2.
Comparison of the intra-operative parameters between the two groups.
| Intraoperative parameters | PFN group | Cemented Bipolar group |
|---|---|---|
| Average Intraoperative blood loss in ml (SD) | 46 (13.5) | 187 (38.1) |
| Mean Operative time in minutes (SD) | 48.4 (6.4) | 60.4 (9.9) |
A significant difference was seen when intraoperative blood loss and operating time were compared between the two groups, favouring the PFN group [p < 0.05].
Table 3.
Immediate Post-operative results during 1 st month post surgery.
| Immediate post-op parameters | PFN group | Cemented Bipolar group |
|---|---|---|
| Superficial infections | 4 (8%) | 8 (16%) |
| Deep infections | 0 | 4 (8%) |
| Bed sores | 16 | 4 |
| Urinary tract infections | 8 | 4 |
| Venous thromboembolism | 6 | 2 |
| Time to full weight bearing in weeks [SD] | 10.1 [3.5] | 3.2 [4.7] |
| Lower respiratory tract infection | 4 | 4 |
| Mortality | 4 | 2 |
Among the immediate post-operative parameters recorded, a significant difference was seen in the incidence of bed sores among the two groups [p < 0.05]. The PFN group showed a significantly higher incidence of bed sores. The average time to full weight bearing was significantly different in the two groups, favouring the Cemented Bipolar group [p < 0.05] (Fig. 1, Fig. 2, Fig. 3, Fig. 4, Fig. 5).
Fig. 1.
Bending of prosthesis was seen in 1 case in the Cemented Bipolar group. It was treated with redoing with Modular Bipolar Prosthesis and locking plate and screws.
Fig. 2.
1 of the patients suffered a dislocated bipolar prosthesis which was treated by closed reduction under General Anaesthesia.
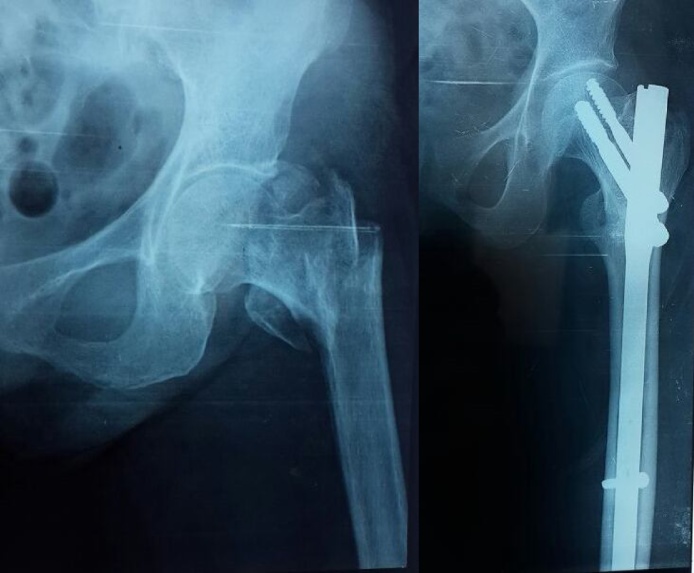
Fig. 3.
A peri-prosthetic fracture was sustained by 1 of the patients in the Cemented Bipolar group due to a fall following surgery. It was treated with a 3.5 mm Locking compression plate.
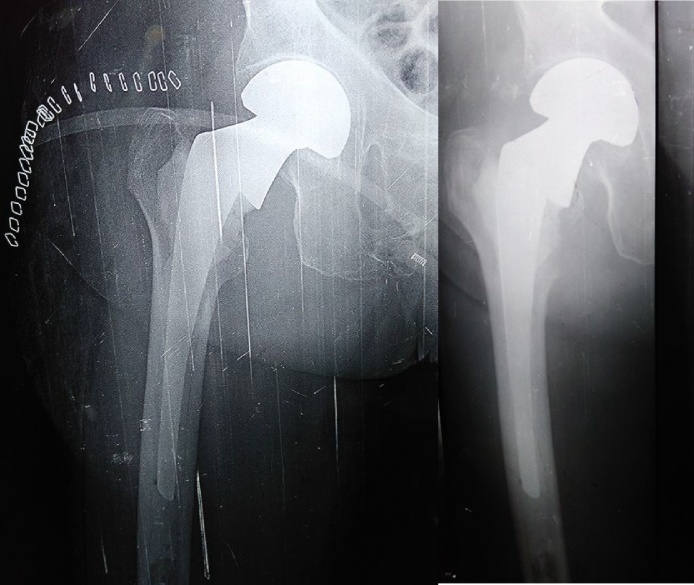
Fig. 4.
Cemented bipolar prosthesis for a case of unstable Intertrochanteric fracture at 2 days and 3 months post-op.
Fig. 5.
Unstable intertrochanteric fracture treated with PFN at 3 months post op with signs of good union.
The incidence of urinary tract infections, venous thromboembolism and mortality were lower in the Cemented Bipolar group, although not statistically significant. The incidence of superficial and deep infections was higher in the cemented bipolar group without a significant difference.
The mortality observed in both groups in the early post-operative period was attributed to pre-existing co-morbidities of the patients. There was no statistically significant difference between the two groups (Table 4).
Table 4.
Late post-operative data recorded at 3, 6 and 12 months.
| Late post-op parameters | PFN group | Cemented Bipolar group |
|---|---|---|
| No. of patients followed up | 46 | 48 |
| Mean Harris Hip Score at 3 months [SD] | 42.1 [7.3] | 66.8 [9.1] |
| Mean Harris Hip Score at 6 months [SD] | 74.2 [14.3] | 70.4 [15.1] |
| Mean Harris Hip Score at 12 months [SD] | 86.7 [13.1] | 70.3 [18.7] |
| Excellent Harris Hip score at 12 months | 44% | 30% |
| Good Harris score at 12 months | 26% | 24% |
| Mean reduction in Mobility Score at 6 months [SD] | 1.8 [1.4] | 2.0 [0.2] |
| Mean reduction in Mobility Score at 12 months [SD] | 1.2 [0.9] | 2.5 [1.5] |
| Mortality at 1 year (including 1st month mortality) | 10 | 12 |
| Number of Complications related to implant | 6 | 10 |
When patients were followed up at 3 months, 6 months and 12 months, a higher mortality was observed in the cemented bipolar group at 1 year, although not statistically significant.
The Harris Hip Scores of the two groups, when compared at 3 months, indicated a significantly better outcome of the cemented hemiarthroplasty group (p < 0.05). The PFN group showed a better Mean Harris Hip Score at 6 months although not statistically significant when compared to the cemented bipolar group, whereas when the Harris Hip Score was compared at 12 months a significant difference [p < 0.05] was noted favouring the PFN group.
The mean reduction in mobility score when measured at 6 months showed a better outcome with the PFN group but with no statistically significant difference, but at 12 months a significant advantage was seen in the PFN group [p < 0.05]
6 patients in the PFN group developed implant related complications. 4 cases had cut out of implant proximally with all patients requiring Hemiarthroplasty. 1 case developed avascular necrosis of head of femur. 1 case developed Z-effect with cut out and backing out of screws.
10 patients in the Cemented bipolar group developed complications related to the prosthesis. 5 of them had a dislocation of the implant due to non-adherence to surgeon’s advice. Closed reduction of the dislocations was done under general anaesthesia. 4 patients sustained a peri-prosthetic fracture at the level of the termination of the stem of the prosthesis. The fractures were fixed with locking plates and screws. 1 patient developed bending of the prosthesis with periprosthetic fracture due to a fall from stairs. It was managed by redoing with modular bipolar prosthesis (Table 5).
Table 5.
Trend of Harris Hip score in the two groups.
 |
6. Discussion
Fractures around the hip are an important cause of morbidity and mortality in the elderly and the advent of internal fixation of these fractures has seen a significant reduction in this mortality.11 One of the limitations of internal fixation is the prolonged immobilization required in comminuted fractures, osteoporosis or poor fixation.12 Thus the need arose for a method that allowed early pain free mobilization of elderly patients having sustained intertrochanteric fractures to avoid complications of being bed ridden like pneumonia, atelectasis, bed sores, etc.13 Primary cemented hemiarthroplasty, having first being used in 1971 for failed internal fixation, was seen to give early pain-free mobility to patients having sustained intertrochanteric fractures, and thus avoid morbidity related to immobilization by returning to pre-morbid mobility.14, 15 Liang et al. and Grimsrud et al studied the effects of primary hemireplacemement arthroplasty on the outcome of patients with intertrochanteric fractures 16, 17 and concluded that it allows early post-operative weight bearing, reduces mortality, improves the quality of life of the patient and reduces burden on the family of the patient. Kesmezacare et al. cited a difference in the mortality between patients of intertrochanteric femur fractures treated with internal fixation (34.2% at 13 months) vs those treated with hemireplacement arthroplasty (48.8% at 6 months).18 Few studies have been done in the Indian population to assess hemireplacement arthroplasty as a viable option to internal fixation in unstable intertrochanteric fractures 19 and our study aimed at comparing it with internal fixation devices, and reviewing the reported results.
The patients in the two groups of our study were comparable at the baseline in terms of demography, pre-existing comorbidities and interval between trauma and surgery. Intraoperative observations showed that the PFN group had an upper hand in terms of blood loss and duration of surgery.
Our study showed that there was a statistically significant difference in earliest possible weight bearing of the patients in the two groups, favouring the cemented bipolar group. This is likely responsible for the other observations including a lower incidence of urinary tract infections, bed sores and venous thromboembolism in the hemiarthroplasty group. Complications were observed very commonly when patients of unstable, osteoporotic intertrochanteric fractures were allowed early weight bearing after internal fixation by Karthik et al.20. The only limitation we observed in the early post-operative period was a higher incidence of superficial and deep wound infections in the cemented bipolar group, attributable to longer duration of surgery and more soft tissue damage. We reported a higher incidence of deep wound infections (8%) than other similar studies which had deep infection rates of around 2.8%,21 although all our cases were treated conservatively.
Our late post-operative follow up showed that patients in the PFN group had a clear and rising advantage over those in the Cemented Bipolar group in terms of Mean Harris Hip Score. Harris Hip Score is a frequently used gold standard criteria for quantifying patient reported outcome measures (PROs) after procedures around the hip.22 Thus a significantly better Mean Harris Hip Score of the cemented bipolar group in the early postoperative period (3 months) clearly indicated that patients in this group did well initially as compared to the PFN group. The Mean Harris Hip score in the late post operative period (12 months) in the PFN group reliably suggested a better outcome of PFN in long term.
We recorded a significant advantage in the PFN group when we compared the mean reduction in mobility score between the two groups at 12 months. This clearly indicated the extent to which the patients in the PFN group could return to pre-morbid mobility when treated with PFN instead of cemented hemiarthrolplasty.
Our study found no significant difference between the two groups when mortality at 1 year follow up was compared. Karaman et al. have stated that the factors affecting the mortality rate include age, pre-existing comorbidities, ASA score and type of anaesthesia.23 These factors were comparable in both the groups in our study and that further supported our findings. The mortality rate of our groups combined was 22%, quite comparable to other similar studies which reached about 20%.
Our study was limited by a number of factors and further studies need to be done to confirm or change our conclusions. Some of the limitations include a maximum follow up of only 3 years which did not allow us to study long term complications of either procedure. Our cohort size was small and no blinding was undertaken while assessing functional outcome of the patients.
7. Conclusion
Our study concluded that internal fixation with PFN gave a significantly better outcome of surgery in the long term and was associated with lesser number of implant related complications. Primary cemented hemiarthroplasty gave a significantly better functional outcome in the early post-operative period by allowing early weight bearing and return to pre-morbid mobility. In conclusion, although Cemented arthroplasty gave a better functional outcome until 3 months post surgery, the results came to be comparable at 6 months. Later the PFN group showed a significantly better outcome when followed up at 12 months.
Conflicts of interest
No conflicts to be declared.
References
- 1.Jensen J.S., Golan H.P., Porter P.J., Kass E.H. Trochanteric fractures. an epidemiological, clinical and biomechanical study. Acta Orthop Scand. 1981 doi: 10.3109/ort.1981.52.suppl-188.01. [DOI] [PubMed] [Google Scholar]
- 2.Dahl E. Mortality and life expectancy after hip fractures. Acta Orthop Scand. 1980 doi: 10.3109/17453678008990781. [DOI] [PubMed] [Google Scholar]
- 3.Uzun M., Ertürer E., Oztürk I., Akman S., Seçkin F., Ozçelik I.B. 2017. Longterm Radiographic Complications Following Treatment of Unstable Intertrochanteric Femoral Fractures with the Proximal Femoral Nail and Effects on Functional Results. [DOI] [PubMed] [Google Scholar]
- 4.Weller I., Wai E.K., Jaglal S., Kreder H.J. The effect of hospital type and surgical delay on mortality after surgery for hip fracture. J Bone Joint Surg Br. 2005 doi: 10.1302/0301-620x.87b3.15300. [DOI] [PubMed] [Google Scholar]
- 5.Bhandari M., Devereaux P.J., Swiontkowski M.F. Internal fixation compared with arthroplasty for displaced fractures of the femoral neck. A meta-analysis. J Bone Joint Surg Am. 2003 doi: 10.2106/00004623-200309000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Lindskog D.M., Baumgaertner M.R.J. Unstable intertrochanteric hip fractures in the elderly. Am Acad Orthop Surg. 2004;12(May–June (3)):179–190. doi: 10.5435/00124635-200405000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Green S., Moore T., Proano F. Bipolar prosthetic replacement for the management of unstable intertrochanteric hip fractures in the elderly. Clin Orthop Relat Res. 1987 [PubMed] [Google Scholar]
- 8.Sinno K., Sakr M., Girard J., Khatib H. The effectiveness of primary bipolar arthroplasty in treatment of unstable intertrochanteric fractures in elderly patients. N Am J Med Sci. 2010 doi: 10.4297/najms.2010.2561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bonnevialle P., Saragaglia D., Ehlinger M. French Hip and Knee Society (SFHG); Trauma Surgery Academy (GETRAUM). Trochanteric locking nail versus arthroplasty in unstable intertrochanteric fracture in patients aged over 75 years. Orthop Traumatol Surg Res. 2011 doi: 10.1016/j.otsr.2011.06.009. [DOI] [PubMed] [Google Scholar]
- 10.Rodop Osman, Kiral Ahmet, Kaplan Haluk, Akmaz Ibrahim. Primary bipolar hemiprosthesis for unstable intertrochanteric fractures. Int Orthop (SICOT) 2002;26:233–237. doi: 10.1007/s00264-002-0358-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.White B.L., Fisher W.D., Laurin C.A. Rate of mortality for elderly patients after fracture of the hip in the 1980’s. J Bone Joint Surg Am. 1987;69:1335–1340. [PubMed] [Google Scholar]
- 12.Wolfgang G.L., Bryant M.H., O'Neill J.P. Treatment of intertrochanteric fracture of the femur using sliding screw plate fixation. Clin Orthop Relat Res. 1982;163:148–158. [PubMed] [Google Scholar]
- 13.Haentjens P., Casteleyn P.P., Opdecam P. The Vidal-Goalard megaprosthesis: an alternative to conventional techniques in selected cases? Acta Orthop Belg. 1985;51:221–234. [PubMed] [Google Scholar]
- 14.Stern M.B., Angerman A. Comminuted intertrochanteric fractures treated with a Leinbach prosthesis. Clin Orthop Relat Res. 1987;218:75–80. [PubMed] [Google Scholar]
- 15.Stern M.B., Goldstein T.B. The use of the Leinbach prosthesis in intertrochantric fractures of the hip. Clin Orthop Relat Res. 1977;128:325–331. [PubMed] [Google Scholar]
- 16.Liang Y.T., Tang P.F., Guo Y.Z. Clinical research of hemiprosthesis arthroplasty for the treatment of unstable intertrochanteric fractures in elderly patients. Zhonghua Yi Xue Za Zhi. 2005;85:3260–3262. [PubMed] [Google Scholar]
- 17.Grimsrud C., Monzon R.J., Richman J., Ries M.D. Cemented hip arthroplasty with a novel cerclage cable technique for unstable intertrochanteric hip fractures. J Arthroplast. 2005;20:337–343. doi: 10.1016/j.arth.2004.04.017. [DOI] [PubMed] [Google Scholar]
- 18.Kesmezacar H., Ogut T., Bilgili M.G., Gokay S., Tenekecioglu Y. Treatment of intertrochanteric femur fractures in elderly patients: internal fixation or hemiarthroplasty. Acta Orthop Traumatol Turc. 2005;39:287–294. [PubMed] [Google Scholar]
- 19.Thakur A., Orth M.S., Lal M., Orth M.S. Cemented hemiarthroplasty in elderly osteoporotic unstable trochanteric fractures using fracture window. Malays Orthop J. 2016;10(March (1)):5–10. doi: 10.5704/MOJ.1603.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Karthik K., Natarajan M. Unstable trochanteric fractures in elderly osteoporotic patients: role of primary hemiarthroplasty. Orthop Surg. 2012;4(May (2)):89–93. doi: 10.1111/j.1757-7861.2012.00173.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stern M.B., Angerman A. Comminuted intertrochanteric fractures treated with a Leinbach prosthesis. Clin Orthop Relat Res. 1987;218(May):75–80. [PubMed] [Google Scholar]
- 22.Shields R.K., Enloe L.J., Evans R.E., Smith K.B., Steckel S.D. Reliability, validity, and responsiveness of functional tests in patients with total joint replacement. Phys Ther. 1995;75(3):169–176. doi: 10.1093/ptj/75.3.169. [DOI] [PubMed] [Google Scholar]
- 23.Karaman Ö., Özkazanlı G., Orak M.M. Factors affecting postoperative mortality in patients older than 65 years undergoing surgery for hip fracture. Ulus Travma Acil Cerrahi Derg. 2015;21:44–50. doi: 10.5505/tjtes.2015.02582. [DOI] [PubMed] [Google Scholar]