Abstract
Disorders of the long head of the biceps tendon (LHB) are a well-recognised cause of shoulder pain despite the function of the long head of the biceps remaining poorly understood. There has been a dramatic rise in the number of biceps tenodesis procedures being performed in the last decade. This may partly be attributed to concerns regarding residual cosmetic deformity and pain after biceps tenotomy though there is little evidence to suggest that functional outcomes of tenodesis are superior to biceps tenotomy. Current literature focuses on LHB disorders with concomitant rotator cuff tears. The aim of this review is to discuss the anatomy of the LHB, the pathogenesis of tendinopathy of the LHB, indications of biceps tenodesis and tenotomy and compare the current literature on the functional outcomes of these procedures for LHB disorders in the absence of rotator cuff tears.
Keywords: Biceps tenodesis, Biceps tenotomy, Biceps tendinopathy
1. Introduction
Disorders of the long head of biceps (LHB) are well recognised as causes of shoulder pain and dysfunction to patients. There is a plethora of evidence available on the management of these conditions. However, the vast majority of studies report the treatment of biceps disorders in patients with concomitant rotator cuff tears.1 Therefore it may be challenging to fully assess the impact of the biceps procedure in these patients.2 The objective of this review is to evaluate the current literature on managing LHB lesions without associated rotator cuff tears (RCTs).
2. The long head of biceps
2.1. Background
LHB lesions are commonly associated with RCTs with the prevalence being as high as 93%.3 Primary LHB tendinopathy is a recognised entity and was described by Meyer in 1936.4 The incidence is low and accounts for about 5% of all LHB pathology.5 LHB disorders are recognised pain generators in the shoulder. Wilk et al.6 classified the causes of LHB pain into 6 categories: 1) Traumatic injuries; 2) Instability; 3) Tendinopathies; 4) Biomechanical dysfunction; 5) Capsular involvement 6) Superior Labrum from Anterior to Posterior (SLAP) lesions.
2.2. Anatomy
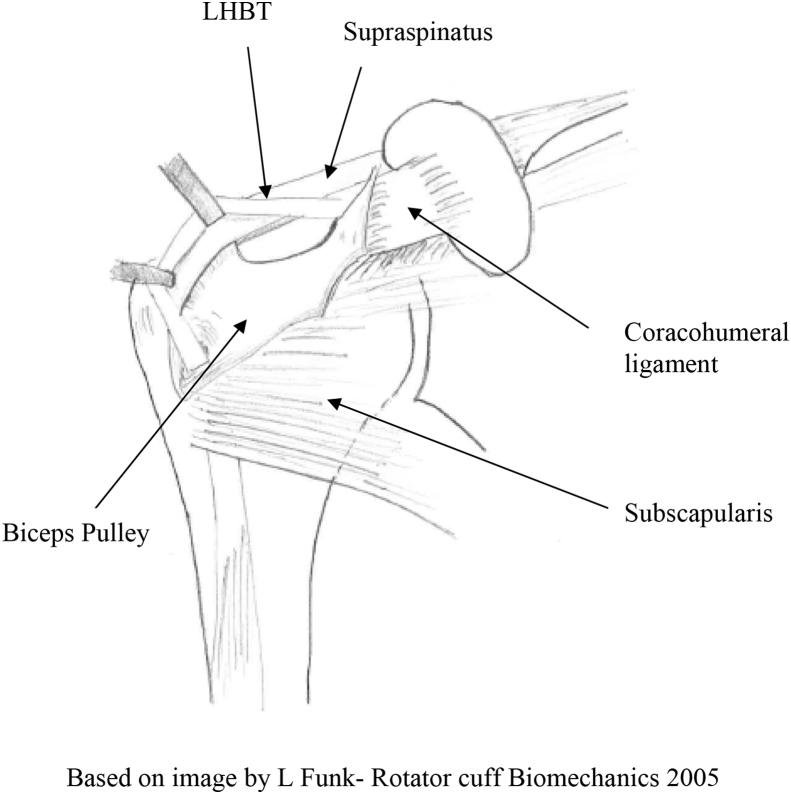
The origin of the LHB tendon (LHBT) is the supraglenoid tubercle and superior glenoid labrum. Distally it attaches to the bicipital tuberosity in the proximal radius with the short head of the biceps. The site of attachment of the LHBT to the superior labrum varies with the main labral origin coming from the posterior labrum in >50% of cadaveric specimens.6 As it exits the joint, the LHBT is stabilised by a capsule-ligamentous complex attached to the medial side of the bicipital groove and often referred to as the “biceps pulley”. The biceps pulley receives contributions from the superior glenohumeral ligament, the coracohumeral ligament, the upper border of the subscapularis tendon and the anterior fibres of the supraspinatus7(Fig. 1). The LHB tendon travels inferiorly into the bicipital groove along the anterior surface of the humerus through the osteoligamentous sheath formed by the transverse humeral ligament.8
Fig. 1.
Drawing illustrating the biceps reflection pulley system (BRP).
In a cadaveric study by Hussain et al.9 the mean length of the LHB was 13.6 ± 2.6 cm. Additionally they calculated the distance from tendon origin to other important landmarks: 1) Proximal bicipital groove- 2.8 ± 0.6; 2) Distal bicipital groove 5.2 ± 0.8; 3) Proximal border of the pectoralis major insertion 8.1 ± 1.0. When performing LHB tenodesis to different locations these figures give surgeons more knowledge about the anatomy allowing them to perform a more accurate re-approximation of the length-tendon relationship of the biceps. It is important to note that the musculotendinous junction of the LHB lies proximal to the distal margin of the Pectoralis Major tendon.10 This has implications for techniques of subpectoral tenodesis.
The LHB and glenoid labrum have been described as a single unit, the biceps-labral-complex (BLC).11 The authors divide the BLC into three main parts: Inside (includes the superior labrum and biceps anchor), Junction (Intra-articular LHBT and its pulley system) and the Bicipital tunnel (Extra-articular biceps).
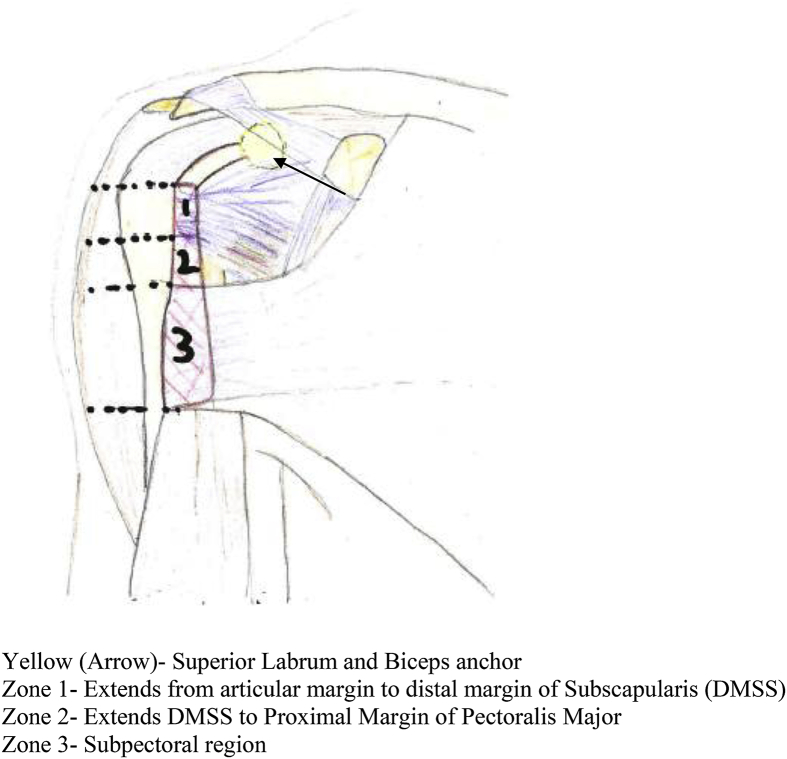
The bicipital tunnel is further divided into 3 separate clinically relevant zones: 1) Articular margin to the distal margin of the subscapularis; 2) Extending from distal margin of Subscapularis to the proximal margin of pectoralis major; 3) Subpectoralis region (Fig. 2). This is clinically relevant as extra-articular biceps lesions (Zone 2 and 3) may be missed during routine glenohumeral arthroscopy and can result in recalcitrant shoulder pain despite surgery. In their case series of 36 subpectoral biceps tenodesis patients, Moon et al.12 found a 80% incidence of ‘hidden lesions’ of the LHB extending distally beyond the bicipital groove. This is in agreement with Taylor et al.13 where diagnostic arthroscopy failed to identify extra-articular bicipital tunnel lesions in 47% of symptomatic patients that underwent LHB transfer to the conjoint tendon.
Fig. 2.
Drawing illustrating the different zones of the bicipital tunnel described by Taylor et al. Taylor SA, Newman AM, Dawson C et al. The “3-Pack” Examination Is Critical for Comprehensive Evaluation of the Biceps-Labrum Complex and the Bicipital Tunnel: A Prospective Study. Arthroscopy: The Journal of Arthroscopic & Related.
2.3. Function
The function of the LHBT in the shoulder is still controversial. Cadaveric studies suggest it has a role as a humeral head depressor14 and in glenohumeral joint stability.15 It may also have a role in maintaining humeral head stability during shoulder abduction, particularly in the anterosuperior and anterior directions.16
Some consider the LHBT functionless in the glenohumeral joint and treat it as a vestigial structure. EMG studies by Yamaguchi17 and Levy et al.18 demonstrated the LHBT is not active during isolated shoulder movements when elbow and forearm movements are controlled postulating that the LHB may have a role in proprioception of the shoulder.
2.4. Pathogenesis
Similar to other common tendinopathies, LHB tenosynovitis involves a spectrum of different pathology ranging from an inflammatory tendinitis to a more degenerative tendinosis type process.19,20 Streit et al. have demonstrated that the changes in the biceps tendon are mostly degenerative and are similar to disorders of other tendons and thus the term “tendinopathy” may be preferable to “tendinitis”.21The intra-articular part of the tendon due to its anatomical location in the bicipital groove22 is susceptible to tear due to the presence of compressive and frictional forces.23 Nuelle et al.24 published a radiological and histological evaluation of primary LHB tendinopathy in patients undergoing open subpectoral biceps tenodesis. Using the anatomical zones described by Taylor, the specimens of each of the three zones were evaluated. Inflammatory changes were significantly higher in the proximal two zones which were in keeping with previous studies.25 In a cadaveric study, the LHBT was also found to contain a network of sensory and sympathetic nerve fibers and interestingly the innervations was unevenly distributed with a predilection for the proximal part of the tendon.26
2.5. Clinical assessment and investigations
LHB disorders are frequently associated with other conditions such as subacromial impingement and RCTs which can make isolating biceps related pain challenging.27 The ‘3-pack’ examination described by O'Brien for assessing LHB disorders is a useful algorithm.28 They utilised the active compression test (O'Brien's sign), Throwing sign and bicipital tunnel palpation in evaluating patients awaiting a biceps transfer procedure and compared them with a control group. The ‘3-pack’ test had excellent inter-rater reliability and sensitivity. Additionally, concluding that ‘hidden’ extra-articular can reliably be excluded on negative tenderness to palpation or negative O'Brien sign (Negative predictive value 93–96%).
Plain shoulder radiographs should routinely be performed and is useful in assessing bony anomalies. Ultrasonography is a valuable tool particularly to assess LHB instability but is user dependant. MRI Arthrography can provide additional information on associated conditions such as impingement and SLAP lesions. However, its role in identifying LHB pathology is questionable with some studies reporting poor to moderate sensitivity for identifying LHB lesions.29,30
2.6. The role of non-operative treatment
First line management for LHB disorders is a period of non-surgical treatment. This typically involves a period of activity modification, physiotherapy and NSAIDs. Ultrasound-guided steroid injection in conjunction with diagnostic ultrasonography is a useful option providing information regarding tendon morphology and assessment for instability.31
3. Methodology
A literature review was performed using PubMed searching for articles published between 1970 and 2018. Only full articles published in English were considered for analysis. The keywords used were: ‘biceps tenodesis versus biceps tenotomy’; ‘biceps tenodesis’; ‘biceps tenotomy’. All studies with concomitant procedures involving the rotator cuff or with associated RCTs were excluded from analysis but have been discussed briefly in this study. Biceps procedures for SLAP lesions was considered beyond the scope of this article.
Most of the pertinent studies identified investigated the treatment of isolated LHB pathology with tenodesis rather than tenotomy. Therefore, this limits the possibility of making a meaningful statistical comparison and conclusion between tenodesis and tenotomy. This narrative does however provide an updated review on the current literature available for the surgical treatment of isolated LHB pathology.
4. Biceps tenodesis for isolated LHB disorders
The incidence of biceps tenodesis procedures have steadily increased in the last decade. Werner et al. reported a 1.8-fold increase in the incidence of an isolated biceps tenodesis procedure being performed in the USA for a variety of diagnoses from 2008-2011.32 Proponents of tenodesis state it preserves length-tension relationship minimising exertional muscle cramping and reduces the incidence of cosmetic deformities.
Traditionally, younger high demand patients were more likely to be offered biceps tenodesis. Currently trends have changed with 68% of tenodesis procedures in 2011 being performed in over 60 year olds.32 This is further supported by a questionnaire-based study which assessed patient preferences and perception of a successful bicep's procedure. Age was not found to have a significant predictive effect towards either tenodesis or tenotomy. Factors predictive for patients preferring tenodesis included residual post-operative tenotomy pain, concern for cosmetic deformity and female sex.33 Although there is consensus amongst orthopaedic surgeons regarding the preferred use of tenodesis rather than tenotomy for LHB pathology there is little agreement regarding the various specificities of the biceps tenodesis procedures.34 Current areas for discussion are whether to perform the procedure open or arthroscopic, the method of fixation (Interference screw/Suture anchor/Soft tissue tenodesis) and the location of tenodesis (Suprapectoral/Subpectoral).
4.1. Open LHB tenodesis procedures
Mazzoca et al.35 performed subpectoral biceps tenodesis for presumed diagnosis of biceps tendinosis but found concomitant RCTs which required repair in 59% of cases. Like other studies, they reported higher functional outcomes scores in patients without cuff tears. We identified 7 studies reporting outcomes on open biceps tenodesis procedures for LHB disorders without RCTs (Table 1).
Table 1.
Overview of literature assessing Long Head of Biceps Disorders without rotator cuff tears.
| Authors | Study type | Surgical procedure | No of cases | Average Age (years) | LHB Disorder | Follow up (months) | Functional outcomes scores |
|---|---|---|---|---|---|---|---|
| Froimson 197584 | Retrospective case series | Open deltopectoral. Keyhole tenodesis (Floor of bicipital groove) | 12 | 48 (25–61) | Tenosynovitis, Rupture, Subluxation | 24 (2–59) | No |
| Becker 1988 | Retrospective case series | Open deltopectoral (Limited) .30 sutured to prepared bone in bicipital groove. 14 Keyhole tenodesis. 10 Transfer procedures to LHB | 51 | *51 (19–71) | Chronic biciptal tendinitis | 6 (1–36) | No |
| Kelly 2001 | Retrospective case series | Arthroscopic Tenotomy | 30 | 50 (16–75) | LHBT tear, instability and chronic recalcitrant tenosynovitis | 19 (12–69) | ASES |
| Boileau 2009 | Cohort study | Arthroscopic Proximal Biceps tenodesis with interference screw | 25 | 37 (19–57) | SLAP II Tears | 35 (24–69) | CS |
| Tangari 2011 | Retrospective case series | Mini Open without arthroscopic assistance | 5 | 32.6 (28–40) | Acute traumatic LHB ruptures | 91.2 (24–156) | CS, MEPS |
| Delle Rose 2012 | Retrospective comparative review | Arthroscopic Soft tissue tenodesis Vs Tenotomy | 104 | 48.3 (31–65) | Partial tears, tendinoses, Pulley lesions and SLAP | 51.6 (28.8–72) | VAS, DASH, CS |
| Funk 2012 | Retrospective case series | Mini Open Subpectoral. 5 Interference screws. 6 Suture anchors | 11 | 41 (23-65 | Isolated Chronic ruptures | 29(6–60) | No |
| Said 2014 | Retrospective case series | Arthroscopic assisted and Mini Open subpectoral tenodesis with modified bone bridge technique | 30 | (25–48) | Isolated LHB Pathology | 12 to 18 | CS, OSS |
| Shen 2014 | Retrospective case series | Arthroscopic Proximal Biceps tenodesis with suture anchors | 49 | 56(37–65) | Tendinitis, Ruptures, Subluxation and SLAP | 14 (12–34) | CS, ASES, UCLA |
| Werner 201485 | Cohort study | Open Subpectoral Biceps Tenodesis Vs Arthroscopic suprapectoral | 82 | Arthroscopic: 49.3 ± 7.2 Open: 52.3 ± 7.7 | Isolated superior labrum or LHB pathology | 37.2 (26.4–64.8) | CS, ASES |
| Gombera 201686 | Cohort study | Open Subpectoral Biceps Tenodesis Vs Arthroscopic suprapectoral | 46 | 57.2 (45–70) | Partial LHBT tears, tendinitis, instability or with a tear of the subscapularis, SLAP | 30.1 (21.1–44.9) | ASES |
| Tahal 2017 | Retrospective outcomes data with prospective collected data | Arthroscopic + Open incision for subpectoral tenodesis | 24 | 37 (29–45) | Tenosynovitis | 37.2 (24–87.6) | ASES, SANE, SF12-PCS and MCS, Quick DASH, VAS |
| Vitali 2016 | Retrospective case series | Arthroscopic Biceps tenodesis(PITT technique) | 60 | 48 (22–55) | Tendinosis, tenosynovitis, subluxation, instability. SLAP II and IV | 12 | UCLA, VAS, CS |
| Green 2017 | Retrospective comparative trial | Arthroscopic Suprapectoral Biceps Tenodesis Versus Open Subpectoral | 38 | Open: 56.6 ± 10.7 Arthroscopic: 60.0 ± 10.2 | All Biceps pathology without RCTs | 54 (24–109.2) | VAS, ASES |
| Schoch 2017 | Prospective case series | Arthroscopic assisted + Mini Open Suprapectoral using a suture plate | 50 | 49 (23–75) | Biceps tendinitis, tears, pulley lesions and SLAP | 29 (22–32) | CS, VAS, Scheibel LHBS |
* Median not mean.
** Age in years.
CS- Constant Score. ASES American Shoulder and Elbow Score.
MEPS- Mayo Elbow Performance Score. VAS-Visual Analogue Score.
OSS- Oxford Shoulder Score UCLA-University of California at Los Angeles Shoulder Score.
SANE- Single Assessment Numerical Evaluation.
Quick DASH- Disabilities of the Arm, Shoulder and Hand.
SF-12 PCS and MCS- Short form Physical and Mental Component Summary Score.
Scheibel LHBS- Long Head of Biceps Score.
WOSI- Western Ontario Shoulder Instability Score.
Tahal et al.36 performed 24 arthroscopic assisted subpectoral tenodess with interference screw fixation for LHB tenosynovitis with significantly improved PROM scores at minimum 2 year follow up. Schoch et al.37 also reported good results in terms of improved pain and functional outcome scores in their case series of 50 patients undergoing open suprapectoral tenodesis with suture button fixation. They utilised the LHB Score devised by Scheibel38 which is a useful post-operative assessment tool specific to post LHB surgery. Only Becker et al.39 presented poor functional outcomes after tenodesis with 50% reporting moderate to severe pain scores. Although the authors subsequently identified associated pathology in some patients it is likely that the functional scores maybe related to the variation in fixation techniques (Tranosseous suture/Keyhole/Transfer to Conjoint tendon) some of which are likely to be biomechanically inferior to current modern techniques.
Spontaneous LHB ruptures account for 90% of all bicep tendon ruptures.40 This is likely secondary to attritional forces acting on the tendon whilst traversing a narrow bicipital groove or friction from with osteophytes in the extra-tendinous portion. Most patients can be managed non-operatively but there are some that continue to get residual pain or cramping. The pain maybe attributable to the failure of the LHBT to auto-tenodese to its surroundings structures resulting in the characteristic cramping pain with prolonged repetitive activity. Open procedures are preferred for isolated painful chronic biceps ruptures due to chronic muscle retraction. Studies by Funk and Provencher described good outcomes following open subpectoral tenodesis using either SA (where tendon quality was felt to be a friable) or IS fixation in patients without RCTs.41,42 Euler et al. also described significant improvements in functional outcome measures post-operatively in 20 patients being treated with open tenodesis after chronic ruptures of LHBT. They devised a biceps specific score ‘Subjective Proximal Biceps Score (SPBS)’ which assessed pain, strength, cosmesis and cramping pre- and post-operatively. The SPBS correlated with the other validated outcomes scores (SF-12 PCS and ASES) suggesting early initial validity.
A similar technique can be used to treat acute LHB ruptures. Tangari et al.43 treated 5 professional wrestlers with excellent results. Incidentally all tears in this group were extra-articular and extended to the groove.
4.2. Arthroscopic LHB tenodesis procedures
Two studies were identified that performed all arthroscopic biceps tenodesis procedures for isolated LHB pathology. One study which included 49 patients and utilised positional portals tailored for proximal lesions of the biceps reported good outcomes in 98% patients and no serious complications.43 Vitali et al.44 also described satisfactory outcomes in 99% of patients that underwent a ‘totally’ intra-articular suture anchor suprapectoral tenodesis. In one of the largest reported studies on arthroscopic tenodesis at the articular margin including 1083 patients, Brady et al. reported a lack of intra or post-operative complications, a low rate of revision (0.4%) for biceps related problems and proposed the benefit of a significant portion of the tendon still being available for revision if required.45
4.3. Open vs arthroscopic LHB tenodesis
A systematic review of all the studies performing open and arthroscopic methods for LHB tenodesis until April 2015 was performed by Abraham et al.46 They excluded procedures performed with associated RCTs and biomechanical studies. A total of 205 arthroscopic and 271 procedures were performed. Both groups had good to excellent outcomes in 98% patients and the complication profile was low. The most recent study by Green et al. comparing Arthroscopic Vs Open biceps tenodesis in isolated biceps disorders showed similar findings.47 No poor outcomes were noted and ultrasound examination revealed an intact tenodesis site in all 30 patients.
One of the concerns of open subpectoral tenodesis is injury to the brachial plexus.48 There were 2 cases of transient brachial plexopathy in the open group which resolved completely. It is recommended that medial retractors are used with care and complete identification of the LHBT is performed prior to performing the tenodesis.49
The benefits of using an open technique in extra-articular biceps lesions are that it gives better visualisation of extra-tendinous lesions such as inflamed synovium, loose bodies and tubercular osteophytes. The role of the bicipital sheath release has been the subject of debate and some hypothesize a stenosing tenosynovitis effect of the sheath on the LHBT akin to the process seen in the first extensor compartment of the wrist.8 Sanders et al. analysed 127 biceps surgeries retrospectively and compared techniques that released the sheath with those that did not. They found that revisions were higher in the group where the bicipital sheath was not released (20.6% Vs 6.8%). Revision rates were highest in the arthroscopic group where tenodesis was performed proximally at the superior edge of intertubercular groove.
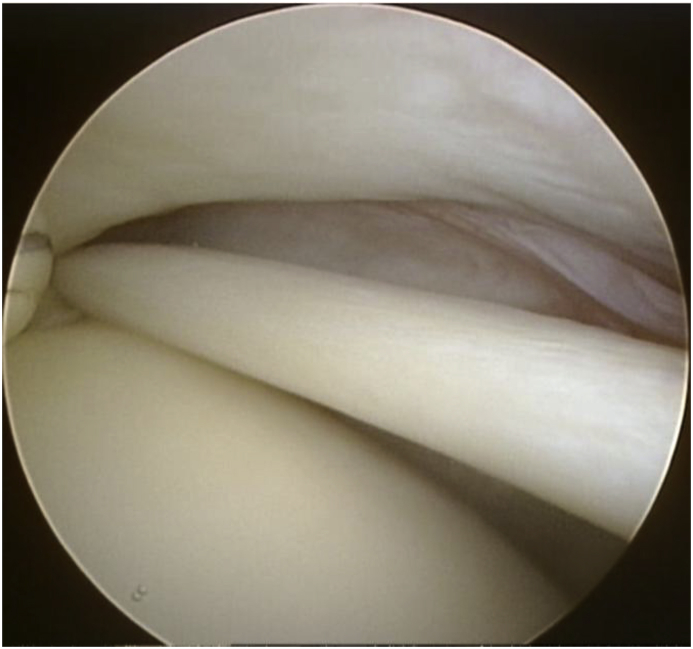
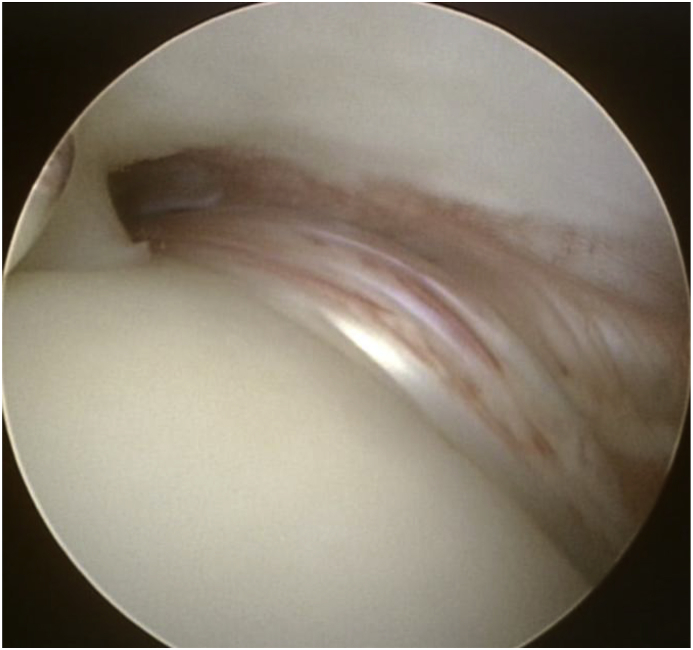
There have been techniques described to help arthroscopic visualisation of the LHBT and its extra-tendinous pathology. Bhatia at al described their technique of direct arthroscopy of the biciptal groove which utilised a superior medial portal and placing the arm abduction, external rotation and forward to facilitate alignment of the scope with the groove.50 The arthroscopic pull test with a probe or hook should be used routinely to pull the intra-articular LHBT providing a more thorough assessment of the tendon as a further 14 mm on average can be visualised (Fig. 3a, Fig. 3b).13
Fig. 3a.
Arthroscopic view of the left shoulder from a posterior viewing portal showing a normal intra-articular tendon of the long head of the biceps (LHBT).
Fig. 3b.
The extra-articular part of the LHBT visualised by pulling the tendon into the joint showing thickening of the tendon with areas of hypervascularity.
4.4. Fixation techniques in biceps tenodesis
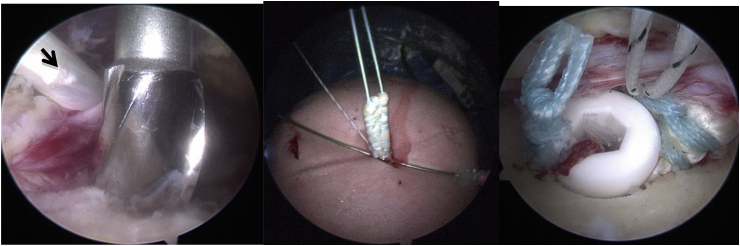
Several fixation techniques for biceps tenodesis have been described. The most popular implants used in current clinical practice are interference screws (IS) and suture anchors (SA). Mazzocca et at51 compared 4 different fixation methods on cadaveric specimens which included the open subpectoral bone tunnel, the arthroscopic SA, the open subpectoral IS and arthroscopic IS technique. All methods had favourable load to failure characteristics with only the open subpectoral bone tunnel group showing statistically significant displacement on cyclic loading. More recent biomechanical studies have found IS to have a higher ultimate failure load than SA.52,53 Park et al. performed a randomised controlled trial comparing clinical and anatomical outcomes of the IS and SA fixation techniques for biceps tenodesis performed with RCT.54 They found no functional difference in both groups but found a statistically significant 21% anatomical failure rate in the IS group compared to 6% in the SA group. The reasons for the results are likely to be multifactorial and maybe in part due to LHBT in patients with RCTs being more degenerate than those studied in cadaveric specimens thus creating more damage between the ‘teeth’ of the screw and cortical bone or in part to the technique itself. We use an IS technique where the tendon is exteriorised, secured with a whip stitch using high grade abrasion resistant sure and then secured in a socket with an IS55(Fig. 4). This reinforces the fixation and, in our experience, leads to a lower incidence of failure.
Fig. 4.
Demonstrates senior authors preferred technique for arthroscopic biceps tenodesis. (Left to right) a): Arthroscopic view of the right shoulder demonstrating a socket being drilled with a cannulated reamer in the floor of the bicipital sulcus in the suprapectoral area. The LHB has been displaced medially (arrow) after placing a marker suture at the level of the socket. b) LHB has been exteriorised and prepared by placing a whip-stitch with high grade abrasion-resistant suture. The black and white marker suture denotes the level of the tendon, which will lie at the mouth of the socket. c) The LHB is fixed in the socket with an interference screw. One strand of the whip-stitch in the LHB is passed though the screw and tied to the other strand thus reinforcing the fixation. The marker suture comes to lie at the edge of the socket thus confirming maintenance of the length-tension relationship.
4.5. Soft tissue biceps tenodesis and transfer procedures
No soft tissue biceps tenodesis for isolated LHB pathology were found. Two recent studies describing soft tissue biceps tenodesis with concomitant RCTs utilised the Percutaneous intra-articular trans tendon technique (PITT) described by Sekiya et al.56 Elkousy et al.57 compared the PITT technique biceps tenodesis with a group treated with the interference screw technique and found both techniques had equivalent failure rates but no functional outcome scores were assessed. Scheibel et al. compared SA fixation versus the PITT technique and had higher LHB Scores in the SA group but equivalent constant scores.58
The LHB transfer procedure to the coracoid process was described by Gilcreest in 1926.59 Gumina et al.60 retrospectively reviewed 28 young, active patients with an acute isolated LHBT ruptures treated at their institution over a period of 12 years with the transfer procedure. Patients were reviewed at a mean of 31 years after the procedure. The vast majority had good functional and cosmetic outcomes with a mean average constant score of 74 for the entire group.
An arthroscopic technique for transfer of the LHB to the conjoint tendon was described by O'Brien in 2005.61 Taylor et al. reported good to excellent results in 56 shoulder after an arthroscopic transfer of the LHB to the conjoint tendon at mid-term follow-up with only one instance of a “Popeye” deformity.62
5. Biceps tenotomy in isolated LHB disorders
Although the evidence for biceps tenotomy in managing LHB pain is well described, it is rarely used in LHB pathology without RCTs. It is frequently performed in elderly, lower demand patients where it is used in conjunction with other procedures such as RCT repair. Gill et al.63 performed an analysis of 32 highly active individuals undergoing arthroscopic biceps tenotomy with a mean follow up 19 months. Overall return to work and sports was <2 weeks and the vast majority returned to their occupation (97%). Four patients reported poor outcomes with 1 patient revised to tenodesis for cosmetic deformity complaints, 1 had persistent pain and 2 were subsequently diagnosed with subacromial impingement.
Incidence of the ‘Popeye’ deformity has been described as high as 50% after biceps tenotomy.64 A number of authors have described arthroscopic techniques to limit distal migration of the LHB after tenotomy to minimise the occurrence of ‘Popeye’ deformity.65, 66, 67, 68 Some patients may experience fatigue discomfort or cramping after a biceps tenotomy and has been reported to occur in 44% of patients.69
6. Biceps tenodesis vs tenotomy for isolated LHB disorders
Several studies have investigated the differences between these procedures but mainly for LHB tendinopathy with RCTs. A recent randomised controlled trial, found no functional difference between the 2 groups where the procedures were performed for combined supraspinatus and biceps lesions in patients aged >40 years old.70 A cosmetic deformity however was noted in 55% of tenotomy patients compared to 8% in the tenodesis group. Previous systematic reviews and Meta-analysis have alluded to better subjective outcomes and lower rates of muscular cramps with tenodesis rather than tenotomy.27,71 Some surgeons thus have concerns regarding post-operative muscle strength and endurance following tenotomy. Case control studies performing isokinetic assessment of elbow flexion and forearm supination strengths comparing tenotomy and tenodesis showed no difference in strengths between both groups.72,73 The most recent meta-analysis by Shang et al.74 found no difference in arm cramping pain between both groups but did note lower Constant scores in the tenotomy group.
Delle rose et al.75 compared the outcomes of tenotomy vs soft tissue biceps tenodesis for isolated LHB conditions (excluding cuff tears, capsulitis and impingement) in 104 patients. The results of this study were in accordance with the above studies where no difference in functional outcome data was noted between the groups.
7. Instability of the LHB
The subscapularis tendon plays a key role along with the biceps reflection pulley (BRP) system in stabilising the LHBT.76 This includes the transverse humeral ligament which has been shown to keep the biceps tendon aligned in the tubercular groove and prevent medial dislocation.77 It is thus a disruption in this anatomical complex that can lead to the ‘subluxing’ biceps. Therefore, traumatic injuries to the subscapularis tendon, particularly the upper tendinous portion, are likely to cause disruption to the LHBT. Maier et al.78 performed stabilisation of the LHBT in acute tears of the subscapularis in 21 patients. The authors concluded that LHB stabilisation is a viable option as an alternative to tenodesis or tenotomy in the context of a traumatic subscapularis tear.
Isolated lesions to the BRP system are rare. On retrospective review of 1184 open subpectoral biceps tenodesis performed by single surgeon over 8 years only 14 were performed for isolated pulley lesions.7 The authors reported no complications and significant improvements in all patient related outcomes measures.
8. Complications of LHB procedures
Complications related specifically to biceps tenotomy include “Popeye deformity”, persistent groove pain, subjective weakness and fatigue discomfort. Weakness and fatigue discomfort are encountered less frequently in patients over the age of 60 years.69 The general risks of shoulder arthroscopy must also be discussed with the patient. Stiffness after arthroscopic tenotomy is the most frequently encountered problem thus post-operative advice must stress the importance of early mobilisation. Other complications include infection, transient nerve injuries, complex regional pain syndrome and stroke secondary to cerebral hypoperfusion for patients in the beach-chair position.79
Biceps tenodesis is comparatively a longer and technically more challenging procedure often requiring hardware to achieve fixation of the tendon to the bone. Some of the main risks pertaining to all tenodesis procedures have been discussed which include infection, loss of fixation and recurrence of ‘Popeye’ deformity, persistent bicipital groove pain and injury to the brachial plexus (rare). Complications can be related to the type of fixation technique with some reports of implant failures and rarely proximal humerus fractures.49 Fractures are thought to be secondary to stress risers in patients that underwent an open procedure where larger cortical drill holes (Keyhole or IS fixation) were made.80,81 Subsequently biomechanical studies comparing subpectoral tenodesis groups to suprapectoral tenodesis or control groups have shown maximum torque and rotation to failure were reduced in the subpectoral group. This potentially can predispose them to a higher risk of humeral fracture.82,83
9. Conclusion
LHB lesions without associated RCTs are uncommon. This review only identified one comparative study comparing tenodesis with tenotomy for isolated LHB disorders. Additionally, most studies discussed in this article are comparative cohort studies or retrospective case series representing level III and IV evidence. One reason for the lack of convincing data maybe the absence of a validated LHB specific outcome measure.71 Scheibel's LHB Score is currently the only one described but it has not been independently validated.
Biceps tenotomy is technically a simpler and quicker procedure than tenodesis and is not associated with any implant costs. However, studies suggest higher rates of muscle cramping and cosmetic deformities after biceps tenotomy. Current evidence suggests little, if any difference, in functional outcome between the two procedures. Whilst tenodesis may offer a lower incidence of ‘Popeye’ deformity and cramping pain, this must be offset against a longer operating time, higher implant costs and the potential for more serious complications, particularly if performed in the subpectoral location.
Our approach is to individualise the surgical management decision for each patient. The functional demands, consideration for cosmetic appearance and early return to work are important factors when discussing operative treatments.
Disclosures
No benefits have been received relating to the subject of this article.
Conflicts of interest
None.
Funding
This researched received no financial grant from any agency in the public, commercial or non-profit sector.
Acknowledgements
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jcot.2018.12.013.
Contributor Information
Syed Hassan, Email: Syedimon@doctors.org.uk.
Vipul Patel, Email: Vipul.Patel4@nhs.net.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Zhang Q., Zhou J., Ge H., Cheng B. Tenotomy or tenodesis for long head biceps lesions in shoulders with reparable rotator cuff tears: a prospective randomised trial. Knee Surg Sports Traumatol Arthrosc. 2015;23(2):464–469. doi: 10.1007/s00167-013-2587-8. [DOI] [PubMed] [Google Scholar]
- 2.Frank R.M., Cotter E.J., Strauss E.J., Jazrawi L.M., Romeo A.A. Management of biceps tendon pathology: from the glenoid to the radial tuberosity. J Am Acad Orthop Surg. 2018;26(4):e77–e89. doi: 10.5435/JAAOS-D-17-00085. [DOI] [PubMed] [Google Scholar]
- 3.Vestermark G.L., Van Doren B.A., Connor P.M., Fleischli J.E., Piasecki D.P., Hamid N. The prevalence of rotator cuff pathology in the setting of acute proximal biceps tendon rupture. J Shoulder Elbow Surg. 2018;27(7):1258–1262. doi: 10.1016/j.jse.2018.01.006. [DOI] [PubMed] [Google Scholar]
- 4.Meyer A.W. Chronic functional lesions of the shoulder. Arch Surg. 1937;35(4):646. [Google Scholar]
- 5.Favorito P.J., Harding W.G., Heidt R.S. Complete arthroscopic examination of the long head of the biceps tendon. Arthroscopy. 2001;17(4):430–432. doi: 10.1053/jars.2001.22360. [DOI] [PubMed] [Google Scholar]
- 6.Vangsness C.T., Jorgenson S.S., Watson T., Johnson D.L. The origin of the long head of the biceps from the scapula and glenoid labrum. An anatomical study of 100 shoulders. J Bone Joint Surg Br. 1994;76(6):951–954. [PubMed] [Google Scholar]
- 7.Vap A.R., Katthagen J.C., Tahal D.S. Isolated biceps reflection pulley tears treated with subpectoral biceps tenodesis: minimum 2-year outcomes. Arthrosc J Arthrosc Relat Surg. 2017;33(10):1788–1794. doi: 10.1016/j.arthro.2017.04.021. [DOI] [PubMed] [Google Scholar]
- 8.Sanders B., Lavery K.P., Pennington S., Warner J.J.P. Clinical success of biceps tenodesis with and without release of the transverse humeral ligament. J Shoulder Elbow Surg. 2012;21(1):66–71. doi: 10.1016/j.jse.2011.01.037. [DOI] [PubMed] [Google Scholar]
- 9.Hussain W.M., Reddy D., Atanda A., Jones M., Schickendantz M., Terry M.A. The longitudinal anatomy of the long head of the biceps tendon and implications on tenodesis. Knee Surg Sports Traumatol Arthrosc. 2015;23(5):1518–1523. doi: 10.1007/s00167-014-2909-5. [DOI] [PubMed] [Google Scholar]
- 10.Denard P.J., Dai X., Hanypsiak B.T., Burkhart S.S. Anatomy of the biceps tendon: implications for restoring physiological length-tension relation during biceps tenodesis with interference screw fixation. Arthroscopy. 2012;28(10):1352–1358. doi: 10.1016/j.arthro.2012.04.143. [DOI] [PubMed] [Google Scholar]
- 11.Taylor S.A., O'Brien S.J. Clinically relevant anatomy and biomechanics of the proximal biceps. Clin Sports Med. 2016;35(1):1–18. doi: 10.1016/j.csm.2015.08.005. [DOI] [PubMed] [Google Scholar]
- 12.Moon S.C., Cho N.S., Rhee Y.G. Analysis of “hidden lesions” of the extra-articular biceps after subpectoral biceps tenodesis: the subpectoral portion as the optimal tenodesis site. Am J Sports Med. 2015;43(1):63–68. doi: 10.1177/0363546514554193. [DOI] [PubMed] [Google Scholar]
- 13.Taylor S.A., Khair M.M., Gulotta L.V. Diagnostic glenohumeral arthroscopy fails to fully evaluate the biceps-labral complex. Arthrosc J Arthrosc Relat Surg. 2015;31(2):215–224. doi: 10.1016/j.arthro.2014.10.017. [DOI] [PubMed] [Google Scholar]
- 14.Kumar V.P., Satku K., Balasubramaniam P. The role of the long head of biceps brachii in the stabilization of the head of the humerus. Clin Orthop Relat Res. 1989;244:172–175. [PubMed] [Google Scholar]
- 15.Pagnani M.J., Deng X.H., Warren R.F., Torzilli P.A., O'Brien S.J. Role of the long head of the biceps brachii in glenohumeral stability: a biomechanical study in cadavera. J Shoulder Elbow Surg. 1996;5(4):255–262. doi: 10.1016/s1058-2746(96)80051-6. [DOI] [PubMed] [Google Scholar]
- 16.Warner J.J., Bowen M.K., Deng X., Torzilli P.A., Warren R.F. Effect of joint compression on inferior stability of the glenohumeral joint. J Shoulder Elbow Surg. 1999;8(1):31–36. doi: 10.1016/s1058-2746(99)90051-4. [DOI] [PubMed] [Google Scholar]
- 17.Yamaguchi K., Riew K.D., Galatz L.M., Syme J.A., Neviaser R.J. Biceps activity during shoulder motion: an electromyographic analysis. Clin Orthop Relat Res. 1997;336:122–129. doi: 10.1097/00003086-199703000-00017. [DOI] [PubMed] [Google Scholar]
- 18.Levy A.S., Kelly B.T., Lintner S.A., Osbahr D.C., Speer K.P. Function of the long head of the biceps at the shoulder: electromyographic analysis. J Shoulder Elbow Surg. 2001;10(3):250–255. doi: 10.1067/mse.2001.113087. [DOI] [PubMed] [Google Scholar]
- 19.Nho S.J., Strauss E.J., Lenart B.A. Long head of the biceps tendinopathy: diagnosis and management. J Am Acad Orthop Surg. 2010;18(11):645–656. doi: 10.5435/00124635-201011000-00002. [DOI] [PubMed] [Google Scholar]
- 20.Zabrzyński J., Paczesny Ł., Łapaj Ł., Grzanka D., Szukalski J. Is the inflammation process absolutely absent in tendinopathy of the long head of the biceps tendon? Histopathologic study of the long head of the biceps tendon after arthroscopic treatment. Pol J Pathol. 2017;68(4):318–325. doi: 10.5114/pjp.2017.73928. [DOI] [PubMed] [Google Scholar]
- 21.Shishani Y., Streit J., Rodgers M., Gobezie R. Tendinopathy of the long head of the biceps tendon: histopathologic analysis of the extra-articular biceps tendon and tenosynovium. Open Access J Sports Med. March 2015;63 doi: 10.2147/OAJSM.S76325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Refior H.J., Sowa D. Long tendon of the biceps brachii: sites of predilection for degenerative lesions. J Shoulder Elbow Surg. 1995;4(6):436–440. doi: 10.1016/s1058-2746(05)80035-7. [DOI] [PubMed] [Google Scholar]
- 23.Joseph M., Maresh C.M., McCarthy M.B. Histological and molecular analysis of the biceps tendon long head post-tenotomy. J Orthop Res. 2009;27(10):1379–1385. doi: 10.1002/jor.20868. [DOI] [PubMed] [Google Scholar]
- 24.Nuelle C.W., Stokes D.C., Kuroki K., Crim J.R., Sherman S.L. Radiologic and histologic evaluation of proximal bicep pathology in patients with chronic biceps tendinopathy undergoing open subpectoral biceps tenodesis. Arthrosc J Arthrosc Relat Surg. 2018;34(6):1790–1796. doi: 10.1016/j.arthro.2018.01.021. [DOI] [PubMed] [Google Scholar]
- 25.Mazzocca A.D., McCarthy M.B.R., Ledgard F.A. Histomorphologic changes of the long head of the biceps tendon in common shoulder pathologies. Arthrosc J Arthrosc Relat Surg. 2013;29(6):972–981. doi: 10.1016/j.arthro.2013.02.002. [DOI] [PubMed] [Google Scholar]
- 26.Alpantaki K., McLaughlin D., Karagogeos D., Hadjipavlou A., Kontakis G. Sympathetic and sensory neural elements in the tendon of the long head of the biceps. J Bone Joint Surg Am. 2005;87(7):1580–1583. doi: 10.2106/JBJS.D.02840. [DOI] [PubMed] [Google Scholar]
- 27.Gurnani N., van Deurzen D.F.P., Janmaat V.T., van den Bekerom M.P.J. Tenotomy or tenodesis for pathology of the long head of the biceps brachii: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2016;24(12):3765–3771. doi: 10.1007/s00167-015-3640-6. [DOI] [PubMed] [Google Scholar]
- 28.Taylor S.A., Newman A.M., Dawson C. The “3-Pack” examination is critical for comprehensive evaluation of the biceps-labrum complex and the bicipital tunnel: a prospective study. Arthrosc J Arthrosc Relat Surg. 2017;33(1):28–38. doi: 10.1016/j.arthro.2016.05.015. [DOI] [PubMed] [Google Scholar]
- 29.Mohtadi N.G., Vellet A.D., Clark M.L. A prospective, double-blind comparison of magnetic resonance imaging and arthroscopy in the evaluation of patients presenting with shoulder pain. J Shoulder Elbow Surg. 2004;13(3):258–265. doi: 10.1016/j.jse.2004.01.003. [DOI] [PubMed] [Google Scholar]
- 30.Zanetti M., Weishaupt D., Gerber C., Hodler J. Tendinopathy and rupture of the tendon of the long head of the biceps brachii muscle: evaluation with MR arthrography. AJR Am J Roentgenol. 1998;170(6):1557–1561. doi: 10.2214/ajr.170.6.9609174. [DOI] [PubMed] [Google Scholar]
- 31.Patel K.V., Bravman J., Vidal A., Chrisman A., McCarty E. Biceps tenotomy versus tenodesis. Clin Sports Med. 2016;35(1):93–111. doi: 10.1016/j.csm.2015.08.008. [DOI] [PubMed] [Google Scholar]
- 32.Werner B.C., Brockmeier S.F., Gwathmey F.W. Trends in long head biceps tenodesis. Am J Sports Med. 2015;43(3):570–578. doi: 10.1177/0363546514560155. [DOI] [PubMed] [Google Scholar]
- 33.Galdi B., Southren D.L., Brabston E.W. Patients have strong preferences and perceptions for biceps tenotomy versus tenodesis. Arthrosc J Arthrosc Relat Surg. 2016;32(12):2444–2450. doi: 10.1016/j.arthro.2016.04.022. [DOI] [PubMed] [Google Scholar]
- 34.Corpus K.T., Garcia G.H., Liu J.N. Long head of biceps tendon management: a survey of the American shoulder and elbow surgeons. HSS Journal®. 2018;14(1):34–40. doi: 10.1007/s11420-017-9575-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mazzocca A.D., Cote M.P., Arciero C.L., Romeo A.A., Arciero R.A. Clinical outcomes after subpectoral biceps tenodesis with an interference screw. Am J Sports Med. 2008;36(10):1922–1929. doi: 10.1177/0363546508318192. [DOI] [PubMed] [Google Scholar]
- 36.Tahal D.S., Katthagen J.C., Vap A.R., Horan M.P., Millett P.J. Subpectoral biceps tenodesis for tenosynovitis of the long head of the biceps in active patients younger than 45 Years old. Arthrosc J Arthrosc Relat Surg. 2017;33(6):1124–1130. doi: 10.1016/j.arthro.2016.10.013. [DOI] [PubMed] [Google Scholar]
- 37.Schoch C., Geyer M., Drews B. Suprapectoral biceps tenodesis using a suture plate: clinical results after 2 years. Arch Orthop Trauma Surg. 2017;137(6):829–835. doi: 10.1007/s00402-017-2664-4. [DOI] [PubMed] [Google Scholar]
- 38.Kerschbaum M., Arndt L., Bartsch M., Chen J., Gerhardt C., Scheibel M. Using the LHB score for assessment of LHB pathologies and LHB surgery: a prospective study. Arch Orthop Trauma Surg. 2016;136(4):469–475. doi: 10.1007/s00402-015-2391-7. [DOI] [PubMed] [Google Scholar]
- 39.Becker D.A., Cofield R.H. Tenodesis of the long head of the biceps brachii for chronic bicipital tendinitis. Long-term results. J Bone Joint Surg Am. 1989;71(3):376–381. [PubMed] [Google Scholar]
- 40.Euler S.A., Horan M.P., Ellman M.B., Greenspoon J.A., Millett P.J. Chronic rupture of the long head of the biceps tendon: comparison of 2-year results following primary versus revision open subpectoral biceps tenodesis. Arch Orthop Trauma Surg. 2016;136(5):657–663. doi: 10.1007/s00402-015-2393-5. [DOI] [PubMed] [Google Scholar]
- 41.Ng C.Y., Funk L. Symptomatic chronic long head of biceps rupture: surgical results. Int J Shoulder Surg. 2012;6(4):108–111. doi: 10.4103/0973-6042.106222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Anthony S.G., McCormick F., Gross D.J., Golijanin P., Provencher M.T. Biceps tenodesis for long head of the biceps after auto-rupture or failed surgical tenotomy: results in an active population. J Shoulder Elbow Surg. 2015;24(2):e36–e40. doi: 10.1016/j.jse.2014.06.031. [DOI] [PubMed] [Google Scholar]
- 43.Tangari M., Carbone S., Gallo M., Campi A. Long head of the biceps tendon rupture in professional wrestlers: treatment with a mini-open tenodesis. J Shoulder Elbow Surg. 2011;20(3):409–413. doi: 10.1016/j.jse.2010.08.008. [DOI] [PubMed] [Google Scholar]
- 44.Vitali M., Pedretti A., Naim Rodriguez N., Valenti M., Fraschini G. Our totally intra-articular “Needle-Anchor” tenodesis technique applied in isolated long head of the biceps tendinopathy: clinical and functional results in 60 patients. Tech Hand Up Extrem Surg. 2016;20(1):26–31. doi: 10.1097/BTH.0000000000000110. [DOI] [PubMed] [Google Scholar]
- 45.Brady P.C., Narbona P., Adams C.R. Arthroscopic proximal biceps tenodesis at the articular margin: evaluation of outcomes, complications, and revision rate. Arthrosc J Arthrosc Relat Surg. 2015;31(3):470–476. doi: 10.1016/j.arthro.2014.08.024. [DOI] [PubMed] [Google Scholar]
- 46.Abraham V.T., Tan B.H.M., Kumar V.P. Systematic review of biceps tenodesis: arthroscopic versus open. Arthrosc J Arthrosc Relat Surg. 2016;32(2):365–371. doi: 10.1016/j.arthro.2015.07.028. [DOI] [PubMed] [Google Scholar]
- 47.Green J.M., Getelman M.H., Snyder S.J., Burns J.P. All-arthroscopic suprapectoral versus open subpectoral tenodesis of the long head of the biceps brachii without the use of interference screws. Arthrosc J Arthrosc Relat Surg. 2017;33(1):19–25. doi: 10.1016/j.arthro.2016.07.007. [DOI] [PubMed] [Google Scholar]
- 48.Rhee P.C., Spinner R.J., Bishop A.T., Shin A.Y. Iatrogenic brachial plexus injuries associated with open subpectoral biceps tenodesis: a report of 4 cases. Am J Sports Med. 2013;41(9):2048–2053. doi: 10.1177/0363546513495646. [DOI] [PubMed] [Google Scholar]
- 49.Virk M.S., Nicholson G.P. Complications of proximal biceps tenotomy and tenodesis. Clin Sports Med. 2016;35(1):181–188. doi: 10.1016/j.csm.2015.08.011. [DOI] [PubMed] [Google Scholar]
- 50.Bhatia D.N., van Rooyen K.S., de Beer J.F. Direct arthroscopy of the bicipital groove: a new approach to evaluation and treatment of bicipital groove and biceps tendon pathology. Arthrosc J Arthrosc Relat Surg. 2008;24(3) doi: 10.1016/j.arthro.2007.06.009. 368.e1-368.e6. [DOI] [PubMed] [Google Scholar]
- 51.Mazzocca A.D., Bicos J., Santangelo S., Romeo A.A., Arciero R.A. The biomechanical evaluation of four fixation techniques for proximal biceps tenodesis. Arthrosc J Arthrosc Relat Surg. 2005;21(11):1296–1306. doi: 10.1016/j.arthro.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 52.Golish S.R., Caldwell P.E., Miller M.D. Interference screw versus suture anchor fixation for subpectoral tenodesis of the proximal biceps tendon: a cadaveric study. Arthrosc J Arthrosc Relat Surg. 2008;24(10):1103–1108. doi: 10.1016/j.arthro.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 53.Patzer T., Santo G., Olender G.D., Wellmann M., Hurschler C., Schofer M.D. Suprapectoral or subpectoral position for biceps tenodesis: biomechanical comparison of four different techniques in both positions. J Shoulder Elbow Surg. 2012;21(1):116–125. doi: 10.1016/j.jse.2011.01.022. [DOI] [PubMed] [Google Scholar]
- 54.Park J.S., Kim S.H., Jung H.J., Lee Y.H., Oh J.H. A prospective randomized study comparing the interference screw and suture anchor techniques for biceps tenodesis. Am J Sports Med. 2017;45(2):440–448. doi: 10.1177/0363546516667577. [DOI] [PubMed] [Google Scholar]
- 55.Lo I.K.Y., Burkhart S.S. Arthroscopic biceps tenodesis using a bioabsorbable interference screw. Arthroscopy. 2004;20(1):85–95. doi: 10.1016/j.arthro.2003.11.017. [DOI] [PubMed] [Google Scholar]
- 56.Sekiya L.J.K., Elkousy H.A., Rodosky M.W. Arthroscopic biceps tenodesis using the percutaneous intra-articular transtendon technique. Arthrosc J Arthrosc Relat Surg. 2003;19(10):1137–1141. doi: 10.1016/j.arthro.2003.10.022. [DOI] [PubMed] [Google Scholar]
- 57.Elkousy H., Romero J.A., Edwards T.B., Gartsman G.M., O'Connor D.P. Ultrasound and clinical evaluation of soft-tissue versus hardware biceps tenodesis: is hardware tenodesis worth the cost? Am J Orthoped. 2014;43(2):62–65. [PubMed] [Google Scholar]
- 58.Scheibel M., Schröder R.-J., Chen J., Bartsch M. Arthroscopic soft tissue tenodesis versus bony fixation anchor tenodesis of the long head of the biceps tendon. Am J Sports Med. 2011;39(5):1046–1052. doi: 10.1177/0363546510390777. [DOI] [PubMed] [Google Scholar]
- 59.Gilcreest E. Two cases of spontaneous rupture of the long head of the biceps flexor cubiti. Surg Clin. 1926;6:539–554. [Google Scholar]
- 60.Gumina S., Carbone S., Perugia D., Perugia L., Postacchini F. Rupture of the long head biceps tendon treated with tenodesis to the coracoid process. Results at more than 30 years. Int Orthop. 2011;35(5):713–716. doi: 10.1007/s00264-010-1099-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Verma N.N., Drakos M., O'Brien S.J. Arthroscopic transfer of the long head biceps to the conjoint tendon. Arthroscopy. 2005;21(6):764. doi: 10.1016/j.arthro.2005.03.032. [DOI] [PubMed] [Google Scholar]
- 62.Taylor S.A., Fabricant P.D., Baret N.J. Midterm clinical outcomes for arthroscopic subdeltoid transfer of the long head of the biceps tendon to the conjoint tendon. Arthroscopy. 2014;30(12):1574–1581. doi: 10.1016/j.arthro.2014.07.028. [DOI] [PubMed] [Google Scholar]
- 63.Gill T.J., McIrvin E., Mair S.D., Hawkins R.J. Results of biceps tenotomy for treatment of pathology of the long head of the biceps brachii. J Shoulder Elbow Surg. 2001;10(3):247–249. doi: 10.1067/mse.2001.114259. [DOI] [PubMed] [Google Scholar]
- 64.Walch G., Edwards T.B., Boulahia A., Nové-Josserand L., Neyton L., Szabo I. Arthroscopic tenotomy of the long head of the biceps in the treatment of rotator cuff tears: clinical and radiographic results of 307 cases. J Shoulder Elbow Surg. 2005;14(3):238–246. doi: 10.1016/j.jse.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 65.Lemos D., Esquivel A., Duncan D., Marsh S., Lemos S. Outlet biceps tenodesis: a new technique for treatment of biceps long head tendon injury. Arthroscopy Techniques. 2013;2(2):e83–e88. doi: 10.1016/j.eats.2012.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Narvani A.A., Atoun E., Van Tongel A., Sforza G., Levy O. The “anchor shape” technique for long head of the biceps tenotomy to avoid the popeye deformity. Arthroscopy Techniques. 2013;2(2):e167–e170. doi: 10.1016/j.eats.2013.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Cho N.S., Cha S.W., Rhee Y.G. Funnel tenotomy versus intracuff tenodesis for lesions of the long head of the biceps tendon associated with rotator cuff tears. Am J Sports Med. 2014;42(5):1161–1168. doi: 10.1177/0363546514523719. [DOI] [PubMed] [Google Scholar]
- 68.Goubier J.-N., Bihel T., Dubois E., Teboul F. Loop biceps tenotomy: an arthroscopic technique for long head of biceps tenotomy. Arthrosc Tech. 2014;3(4):e427–e430. doi: 10.1016/j.eats.2014.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kelly A.M., Drakos M.C., Fealy S., Taylor S.A., O'Brien S.J. Arthroscopic release of the long head of the biceps tendon: functional outcome and clinical results. Am J Sports Med. 2005;33(2):208–213. doi: 10.1177/0363546504269555. [DOI] [PubMed] [Google Scholar]
- 70.Castricini R., Familiari F., De Gori M. Tenodesis is not superior to tenotomy in the treatment of the long head of biceps tendon lesions. Knee Surg Sports Traumatol Arthrosc. 2018;26(1):169–175. doi: 10.1007/s00167-017-4609-4. [DOI] [PubMed] [Google Scholar]
- 71.Ge H., Zhang Q., Sun Y., Li J., Sun L., Cheng B. Tenotomy or tenodesis for the long head of biceps lesions in shoulders: a systematic review and meta-analysis. PLoS One. 2015;10(3) doi: 10.1371/journal.pone.0121286. Screen HR, ed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wittstein J., Queen R., Abbey A., Moorman C.T. Isokinetic testing of biceps strength and endurance in dominant versus nondominant upper extremities. J Shoulder Elbow Surg. 2010;19(6):874–877. doi: 10.1016/j.jse.2010.01.018. [DOI] [PubMed] [Google Scholar]
- 73.Shank J.R., Singleton S.B., Braun S. A comparison of forearm supination and elbow flexion strength in patients with long head of the biceps tenotomy or tenodesis. Arthrosc J Arthrosc Relat Surg. 2011;27(1):9–16. doi: 10.1016/j.arthro.2010.06.022. [DOI] [PubMed] [Google Scholar]
- 74.Shang X., Chen J., Chen S. A meta-analysis comparing tenotomy and tenodesis for treating rotator cuff tears combined with long head of the biceps tendon lesions. PLoS One. 2017;12(10) doi: 10.1371/journal.pone.0185788. Nordez A, ed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Delle Rose G., Borroni M., Silvestro A. The long head of biceps as a source of pain in active population: tenotomy or tenodesis? A comparison of 2 case series with isolated lesions. Musculoskeletal Surgery. 2012;96(S1):47–52. doi: 10.1007/s12306-012-0189-0. [DOI] [PubMed] [Google Scholar]
- 76.Godenèche A., Nové-Josserand L., Audebert S. Relationship between subscapularis tears and injuries to the biceps pulley. Knee Surg Sports Traumatol Arthrosc. 2017;25(7):2114–2120. doi: 10.1007/s00167-016-4374-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Slätis P., Aalto K. Medial dislocation of the tendon of the long head of the biceps brachii. Acta Orthop Scand. 1979;50(1):73–77. doi: 10.3109/17453677909024092. [DOI] [PubMed] [Google Scholar]
- 78.Maier D., Jaeger M., Suedkamp N.P., Koestler W. Stabilization of the long head of the biceps tendon in the context of early repair of traumatic subscapularis tendon tears. J Bone Joint Surg. 2007;89(8):1763–1769. doi: 10.2106/JBJS.F.01012. [DOI] [PubMed] [Google Scholar]
- 79.Farmer K.W., Wright T.W. Shoulder arthroscopy: the basics. J Hand Surg. 2015;40(4):817–821. doi: 10.1016/j.jhsa.2015.01.002. [DOI] [PubMed] [Google Scholar]
- 80.Sears B.W., Spencer E.E., Getz C.L. Humeral fracture following subpectoral biceps tenodesis in 2 active, healthy patients. J Shoulder Elbow Surg. 2011;20(6):e7–e11. doi: 10.1016/j.jse.2011.02.020. [DOI] [PubMed] [Google Scholar]
- 81.Reiff S.N., Nho S.J., Romeo A.A. Proximal humerus fracture after keyhole biceps tenodesis. Am J Orthoped. 2010;39(7):E61–E63. [PubMed] [Google Scholar]
- 82.Beason D.P., Shah J.P., Duckett J.W., Jost P.W., Fleisig G.S., Cain E.L. Torsional fracture of the humerus after subpectoral biceps tenodesis with an interference screw: a biomechanical cadaveric study. Clin BioMech. 2015;30(9):915–920. doi: 10.1016/j.clinbiomech.2015.07.009. [DOI] [PubMed] [Google Scholar]
- 83.De Villiers D.J., Loh B., Tacey M., Keith P. Proximal versus distal screw placement for biceps tenodesis: a biomechanical study. J Orthop Surg. 2016;24(2):258–261. doi: 10.1177/1602400227. [DOI] [PubMed] [Google Scholar]
- 84.Froimson A.I., Oh I. Keyhole tenodesis of biceps origin at the shoulder. Clin Orthop Relat Res. 1975;112(1):245–249. [PubMed] [Google Scholar]
- 85.Werner B.C., Evans C.L., Holzgrefe R.E. Arthroscopic suprapectoral and open subpectoral biceps tenodesis: a comparison of minimum 2-year clinical outcomes. Am J Sports Med. 2014;42(11):2583–2590. doi: 10.1177/0363546514547226. [DOI] [PubMed] [Google Scholar]
- 86.Gombera M.M., Kahlenberg C.A., Nair R., Saltzman M.D., Terry M.A. All-arthroscopic suprapectoral versus open subpectoral tenodesis of the long head of the biceps brachii. Am J Sports Med. 2015;43(5):1077–1083. doi: 10.1177/0363546515570024. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.