Abstract
Introduction
In Plantar Fasciitis, the main concern of the patients is the pain that disturbs their day to day activities. Different modalities of treatments are being used for its pain management. This study seeks to investigate and compare decrease in level of pain following treatment with Methylprednisolone injections (DMP) Vs Extra-Corporeal Shock Wave Therapy (ESWT) in plantar fasciitis.
Methods
This prospective comparative non randomized study was conducted in 60 patients of any age presenting with Plantar Fasciitis at B&B Hospital, Kathmandu. Patients were divided into 2 groups (30 each) based on patients preference. Methylprednisolone injection was given to one group and another group received ESWT. Follow up of both groups were carried out at 6 weeks, 3 months and 6 months and the outcome was measured with Visual Analogue Pain Scale (VAS). Statistical analysis wasdone using SPSS software, version 13. Chi-square and Independent t-test were applied to look for significant variations in outcome.
Results
Follow-up at 6 weeks revealed 26 (86.7%) patients attaining VAS < 5 in ESWT group in comparison to 16 (53.3%) patients of DMP group (p = 0.005). At the end of 6 months, 5 patients in DPM group still had significant pain (VAS ≥ 5) compared to 2 patients in ESWT group (p = 0.02). However 11 patients of DMP group and 23 of ESWT group received single episode of treatment only and had persistent symptomatic pain relief (VAS < 5) during all follow ups at 6 weeks, 3 months and 6 months (p = 0.004).
Conclusions
Plantar fasciitis was more prevalent in overweight population and females. Significant improvement in pain was observed with both ESWT and DMP Injections. However, ESWT was found to be more effective than DMP Injections for treatment of Plantar Fasciitis.
Abbreviations: ESWT, extra-corporeal shock wave therapy; DMP, methylprednisolne; VAS, visual analogue scale; BMI, body mass index; PMT, point of maximal tenderness; NSAIDs, non-steroid anti-inflammatory drugs
Keywords: Plantar fasciitis, Corticosteroid injection, Extracorporeal shockwave therapy
1. Background
Planar fasciitis is the inflammation of plantar fascia, usually in the centro- medial subcalcaneal region. It is reported to be the most common cause for inferior heel pain in adults and affects both sedentary and active individuals.1 The etiology of the condition is not well understood and 85% of the cases occur without any identifiable risk factors. Overuse due to prolonged weight bearing, obesity, unaccustomed walking/running & limited dorsiflexion of ankle joint are cited to be the causative risk factors for the condition.2 Tightness/weakness of the gastroc-soleus, Achilles tendon or intrinsic foot muscles is also associated with plantar fasciitis in some of the published literature.3
The condition is diagnosed clinically. Most patients complain of throbbing or piercing type of heel pain that is troublesome especially after taking first few steps in the morning or after periods of inactivity.2, 4 The discomfort often improves with further ambulation but worsens with continued activity, often limiting daily activity.4 The only clinical sign is the tenderness at medial tubercle of calcaneum. Radiographs may show calcifications in the soft tissue around heel or anterior calcaneal osteophyte (heel spur) in among half of the patients with Plantar fasciitis. One fifth of the normal population may also have asymptomatic heel spur.4, 5 Plain radiographs are routinely advised to rule out any other bony pathology. Bone scan may show increased calcaneal uptake & MRI may show thickening of the plantar fascia. However, accuracy of these imaging modalities is inconclusive and thus is not routinely recommended.4
Conservative physical therapy for the condition include stretching of gasctroc-soleus/Achilles tendon & plantar fascia, cushioned heel inserts and walking casts.3 Intralesional corticosteroid injection has been used for treatment since 1950s6 and is still popular because of its easy availability, low cost and rapid pain relief. Platelet Rich Plasma has also been used in recent years but its results are not superior to steroids.7 Some authors have shown better results of Injection botulinum toxin over steroids in treating plantar fasciitis.8 However, because of its high cost and complex administration, it is not as popular as injection steroid. Another non-invasive modality for the treatment is Extracorporeal shock wave therapy which has gained popularity in recent years.9, 10, 11 Surgical release of plantar fascia is an option for recalcitrant cases.3
Plantar fasciitis occurs in approximately 2 million Americans per year and affects 10% of the population during the course of a life time.2 There is paucity of literature published regarding prevalence and associated risk factors from Nepalese Population. There are no reports comparing the outcomes of two different treatment modalities i.e. steroid injection and ESWT from Nepalese population. Our study aims to fulfill the same lacunae.
2. Materials and methods
Ours was a non-randomized prospective comparative study comparing outcomes of two different treatment modalities viz. injection methyl prednisolone and Extra-corporeal shock wave therapy in patients with plantar fasciitis in Nepalese population. The study was carried out at B & B Hospital, Nepal between September 2011 and April 2013. All cases of plantar fasciitis were initially treated with NSAIDS for 7 days and physical therapy including gastro-soleus/Tendo-Achilles & Plantar fascia stretching exercises along with heel inserts. Those not responding to the initial treatment at 2 weeks (VAS score > 5) were included in our study & were given options of injection methyl-prednisolone (DPM) & Extracorporeal shock wave therapy (ESWT) in addition to physical therapy. The treatment modality was chosen as per patient’s preference. Patients were divided into two groups: DPM group and ESWT group. The DMP group received injection methyl-prednisolone 40 mg at point of maximal tenderness (PMT) and the ESWT group received 2500 impulses of low energy Extra-corporeal shock wavetargeting heel from plantar side. Patients who got relief with only physical therapy or who have bilateral plantar fasciitis & who didn’t give consent to the study were excluded from the study. The patients were followed up at 6 weeks, 3 months and 6 months and outcome was measured with VAS score. Patients with VAS score <5 were considered to have relief whereas in patients with VAS score ≥5, the initial treatment (DPM or ESWT) was repeated. The physical therapy was continued in all the patients. The cases with incomplete follow up data or those who asked to switch over to other treatment modality during follow-ups were also excluded. The outcome measures were compared among the two groups. Data was collected and assembled in database (Excel 2010, Window’s Software). Statistical analysis wasdone using the software SPSS, version 13. Chi-square and Independent t-test were applied to look for significant variations in outcome between the two groups.
3. Results
Total 92 patients with plantar fasciitis visited to outpatient at our hospital during the study period. All were given NSAIDs for a week and started on physical therapy. 16 had bilateral affection and were excluded. 12 patients were excluded because they didn’t require further treatment modality (injection methyl-prednisolone or ESWT) as their VAS scores were always less than 5. Of the remaining 64 cases who were not relieved (VAS score ≥ 5) at 2 weeks of presentation, 34 opted for injection methyl prednisolone and 30 for ESWT. 4 patients from injection group were excluded because they switched over to ESWT at 6 weeks of follow up. Final analysis consisted of 60 patients, 30 each in two groups: DPM and ESWT.
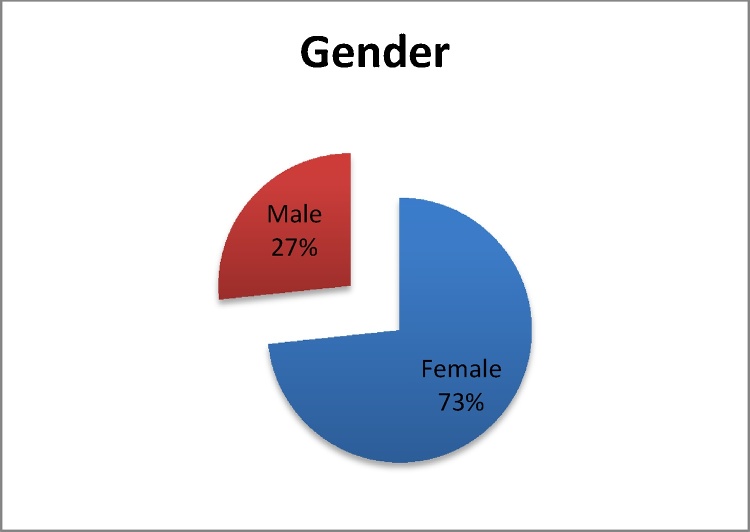
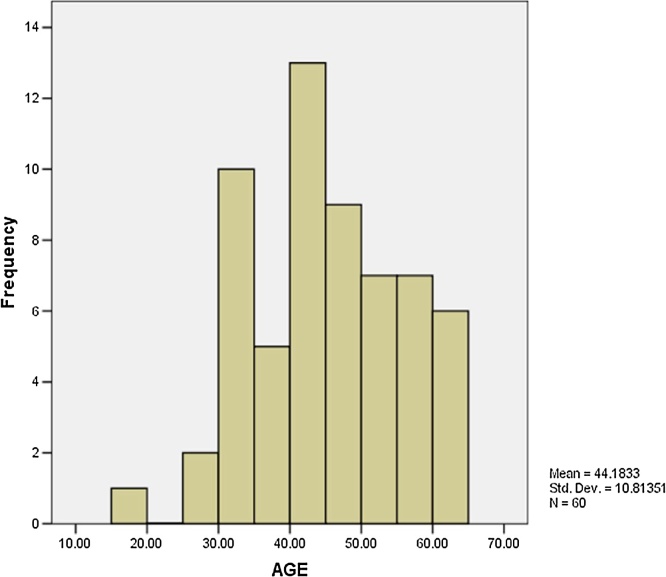
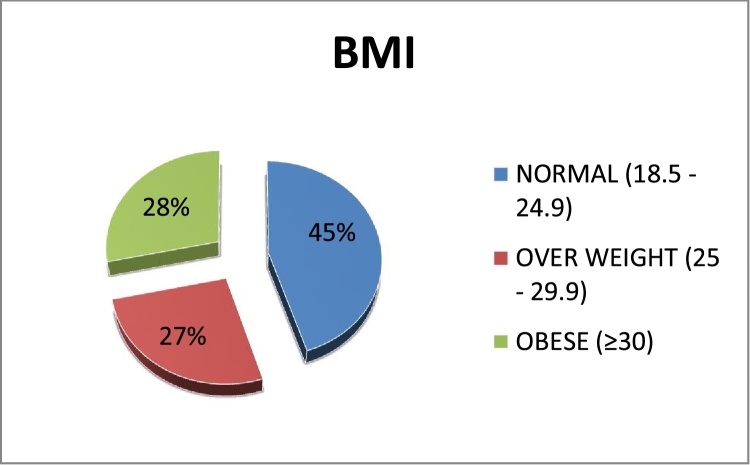
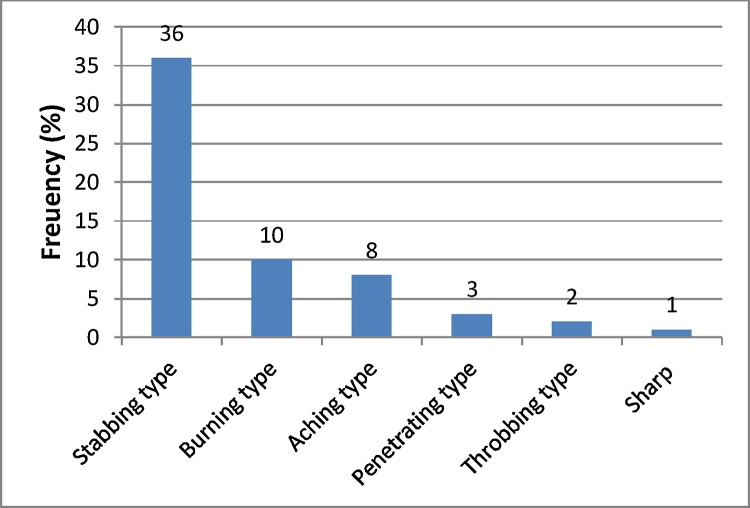
Of the 60 patients enrolled in our study 44 (73%) were females and 16 (27%) were males [Fig. 1]. The mean age was 44.18 years (range: 15–65 years) [Fig. 2]. 27 patients (45%) had a normal BMI (18.5–24.9), 16 (26.66%) were overweight (BMI: 25–29.9) and the remaining 17 patients (28.34%) were obese (BMI ≥ 30) [Fig. 3]. 31 patients (51.67%) reported their heel pain to be continuous persisting throughout the day. The nature of pain was stabbing in 36 (60%), burning in 10 (16.67%), aching in 8 (13.34%), penetrating in 3 (5%), throbbing in 2 (3.34%) and sharp in 1 (1.67%) patients [Fig. 4]. 48 (80%) patients reported their heel pain to be the worst after their first steps in the morning. Improvement of pain with continued walking was reported in 24 (50%) of these patients.
Fig. 1.
Gender Distribution.
Fig. 2.
Age distribution.
Fig. 3.
BMI distribution.
Fig. 4.
Nature of pain.
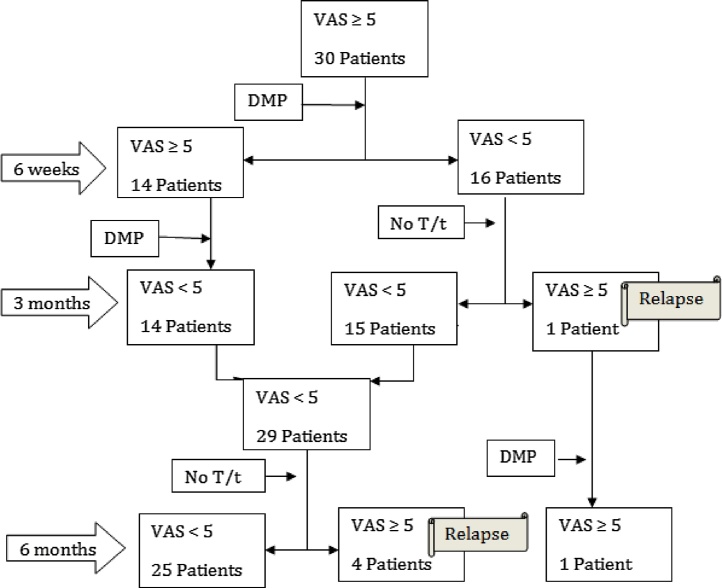
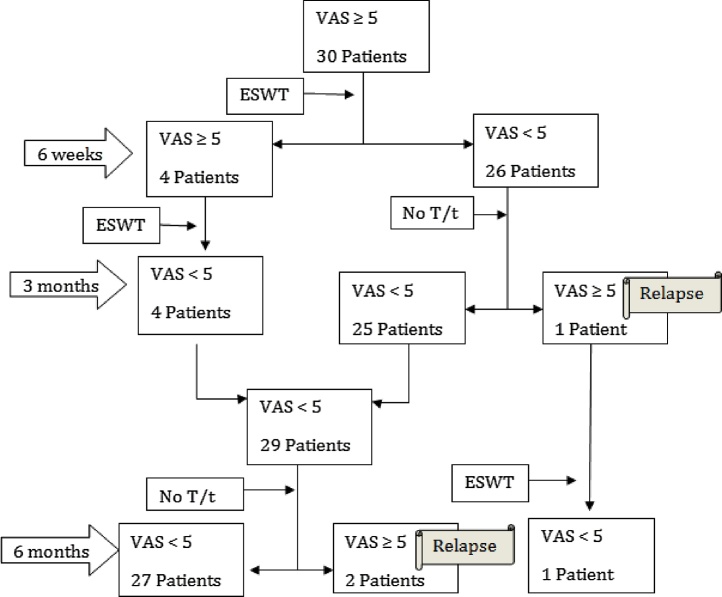
Chart 1, Chart 2 show the treatment summary in the DMP and ESWT groups respectively.
Chart 1.
DMP group treatment.
Chart 2.
ESWT group treatment.
Of the 30 patients from each group, 16 (53.3%) patients in DPM group had significant symptomatic relief (VAS score < 5) compared to 26 (86.7%) patients in ESWT group, at 6 week of follow up (p = 0.005). Remaining 14 (46.7%) patients in DPM group and 4 (13.3%) patients in ESWT group with VAS scores ≥5 were continued with the second episode of same treatment modality.
All the 14 patients who received second injectionat 6 weeks from DPM group and 4 patients who received second episode at 6 weeks from ESWT group had significant symptomatic relief (VAS scores < 5) at 3 months follow up. Of the 16 patients from DPM group & 26 patients from ESWT group who had symptomatic relief at 6 weeks following first episode of treatment, 1 in each group had a relapse (VAS scores ≥ 5) at 3 months of follow up (p = 1.00). At 3 months follow up, 29 of 30 patients in each group had VAS score <5 and the remaining 1 relapse in each group were continued with the second episode of same treatment.
At 6 months follow up, one case from DMP group who had relapse at 3 months had VAS score ≥5, whereas that from ESWT group had VAS score <5. However, 4 of 29 patients in DPM group whose VAS scores were <5 at 3 months follow up had worsening of pain (VAS ≥ 5) as compared to 2 of 29 patients from ESWT group (p = 0.67). 5 patients in DPM group still had significant pain (VAS ≥ 5) compared to 2 patients in ESWT group at 6 months of follow-up (p = 0.02). Moreover 11 of 30 in DMP group and 23 of 30 patients in ESWT group received single episode of treatment only as they had persistent symptomatic relief (VAS < 5) during the follow ups at 6 weeks, 3 months and 6 months (p = 0.004). This also signifies that in comparison to ESWT more episodes of DMP injections were needed for pain relief in patients with plantar fasciitis.
Our results show better outcomes with Extracorporeal shock wave therapy (ESWT) as compared to injection methyl prednisolone (DPM) mode of treatment for plantar fasciitis.
4. Discussion
Plantar fascia is the most important structure for the dynamic arch support of the foot and is the most common cause for inferior heel pain.12, 13 Riddle et al. in 2003,2 from a matched case control study published the risk factors for development of plantar fasciitis via limited dorsiflexion of the ankle, obesity and spending majority of the day weight-bearing. In all of their cases, pain was provoked when patient took the first few steps in the morning and increased with weight bearing during the day whereas in our study, 80% patients reported their heel pain to be the worst after their first steps in the morning and improvement with continued walking was reported in 50% of these patients. Out of 60 patients enrolled in our study, 33 had BMI ≥25. 16 patients were Overweight (BMI 25–29.9) and 17 were Obese (BMI–>30). Weight loss can thus be an effective preventive measure for this painful heel condition.
Plantar fasciitis is more common in middle aged and old individuals.1 It is more common in athletic and military personnel.14, 15 There is no clear sex predilection for this condition.2, 14 In our study, 58.34% of patients were between 40 and 60 years of age. Interestingly, 73.3% cases were females.
In a randomized control trial published by Eslamian et al. in 2016,10 they compared outcomes between two groups. 20 patients in one group received five sessions of extracorporealshock wave therapy (EWST) [radial EWST with 2000 shock waves/session of 0.2 mJ/mm2] and 20 patients in the other group received single injection methylprednisolone. Both interventions caused improvement in pain and functional ability 2 months after the treatment. Foot Function Index (FFI) was improved more with ESWT and patients were more satisfied with ESWT. In another study by Rompe et al.,9 three treatment with 1000 impulses of low energy shock waves led to superior clinical outcomes compared to three applications of 10 impulses of low energy shock waves. On the contrary, in a study by Porter et al.,16 they had better results with single steroid injection as compared to course of low-dose ESWT comprising 3 treatments over a period of 3 weeks. In our study, we looked only for VAS pain scores and didn’t look into foot function index.Of the 30 patients from each group, 16 patients in DPM group had significant symptomatic relief (VAS score < 5) compared to 26 patients in ESWT group, at 6 week of follow up (p = 0.005). 11 of them in DPM group had persistent symptomatic relief (VAS < 5) at 3 months and 6 months of follow up compared to 23 patients in the ESWT group. Aqil et al. also concluded ESWT to be a safe and effective mode of treatment for plantar fasciitis in their published meta-analysis of RCTs.11
Though corticosteroid injection is the most popular treatment for plantar fasciitis, rupture of plantar fascia and heel pad atrophy are the most feared complications.17, 18, 19 Calcification of plantar fascia following steroid injection is also reported in literature.20 Therefore, physicians should be cautious while administrating steroid injections. However, we didn’t come across any cited adverse effects in our study. A recent systematic analysis of RCTs by Ang TW et al.21 concluded steroid injections to provide only short term relief lasting 4–12 weeks. Physicians need to weigh the treatment benefits against risks of steroid injection. These types of complications have not been reported with extracorporeal shock wave therapy and it is gaining popularity in the recent years for treatment of plantar fasciitis.
Our study shows ESWT as a better treatment modality as compared to injection steroid for the management of symptomatic plantar fasciitis not relieved with conservative measures.
However our study has some limitations. The limitations are small sample size, non-randomized design with possible selection bias, heterogeneous patient population, lack of functional scoring and a short follow up. The value of repeat DMP injections or ESWT is not studied as well. Future research studying the value of repeat injections/ESWT using functional assessment tools at longer term follow-up is needed to consolidate the preliminary observations made in our study.
5. Conclusion
Plantar fasciitis was more prevalent in overweight/obese population and Females. The pain of plantar fasciitis was found to be more pronounced during morning hours, it improved with rest and worsened with walking in majority. In more than half, the pain was continuously persisting throughout the day. Significant improvement in pain was observed with both ESWT and DMP Injections. However, ESWT was found to be more effective than DMP Injections for treatment of Plantar Fasciitis.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Availability of data and materials
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Authors’ contribution
BNM made substantial contributions to conception and design, to analysis and interpretation of data and to writing the manuscript. RRP made substantial contributions to analysis and interpretation of data and to writing the manuscript. BB, BKS and AKB made substantial contributions to conception and design and to the acquisition of data. All authors were involved in drafting of the manuscript or revising it critically for important intellectual content. All authors read and approved the final manuscript.
Conflict of interest
The authors have none to declare.
Ethics approval and consent to participate
The study was approved by Institutional Research/Review Committee (IRC), B&B Hospital, Gwarko, Lalitpur, Nepal (Ref: IRC_2011_09_20_1). All participants provided written informed consent.
Acknowledgement
We thank Dr. Anuja Jha for her valuable suggestions and co-operation in computer works.
Contributor Information
Bibhuti Nath Mishra, Email: drbibhuti5@gmail.com.
Rishi Ram Poudel, Email: rishipoudel2004@gmail.com.
Bibek Banskota, Email: bibekbanskota@gmail.com.
Babu Kaji Shrestha, Email: bkshrestha7@hotmail.com.
Ashok Kumar Banskota, Email: ashokbanskota@gmail.com.
References
- 1.Scher D.L., Belmont P.J., Bear R., Mountcastle S.B., Orr J.D., Owens B.D. The incidence of plantar fasciitis in the United States military. J Bone Joint Surg Am. 2009;91(December (12)):2867–2872. doi: 10.2106/JBJS.I.00257. [DOI] [PubMed] [Google Scholar]
- 2.Riddle D.L., Pulisic M., Pidcoe P., Johnson R.E. Risk factors for Plantar fasciitis: a matched case-control study. J Bone Joint Surg Am. 2003;85–A(May (5)):872–877. doi: 10.2106/00004623-200305000-00015. [DOI] [PubMed] [Google Scholar]
- 3.Young C.C., Rutherford D.S., Niedfeldt M.W. Treatment of plantar fasciitis. Am Fam Phys. 2001;63(February (3)):467–474. 477–478. [PubMed] [Google Scholar]
- 4.Cole C., Seto C., Gazewood J. Plantar fasciitis: evidence-based review of diagnosis and therapy. Am Fam Phys. 2005;72(December (11)):2237–2242. [PubMed] [Google Scholar]
- 5.DiMarcangelo M.T., Yu T.C. Diagnostic imaging of heel pain and plantar fasciitis. Clin Podiatr Med Surg. 1997;14(April (2)):281–301. [PubMed] [Google Scholar]
- 6.Lapidus P.W., Guidotti F.P. Local injections of hydrocortisone in 495 orthopedic patients. Ind Med Surg. 1957;26(May (5)):234–244. [PubMed] [Google Scholar]
- 7.Acosta-Olivo C., Elizondo-Rodriguez J., Lopez-Cavazos R., Vilchez-Cavazos F., Simental-Mendia M., Mendoza-Lemus O. Plantar fasciitis. A comparison of treatment with intralesional steroids versus platelet-rich plasma (PRP). A randomized, blinded study. J Am Podiatr Med Assoc. 2016;(October) doi: 10.7547/15-125. [DOI] [PubMed] [Google Scholar]
- 8.Elizondo-Rodriguez J., Araujo-Lopez Y., Moreno-Gonzalez J.A., Cardenas-Estrada E., Mendoza-Lemus O., Acosta-Olivo C. A comparison of botulinum toxin a and intralesional steroids for the treatment of plantar fasciitis: a randomized, double-blinded study. Foot Ankle Int. 2013;34(January (1)):8–14. doi: 10.1177/1071100712460215. [DOI] [PubMed] [Google Scholar]
- 9.Rompe J.D., Schoellner C., Nafe B. Evaluation of low-energy extracorporeal shock-wave application for treatment of chronic plantar fasciitis. J Bone Joint Surg Am. 2002;84–A(March (3)):335–341. doi: 10.2106/00004623-200203000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Eslamian F., Shakouri S.K., Jahanjoo F., Hajialiloo M., Notghi F. Extra corporeal shock wave therapy versus local corticosteroid injection in the treatment of chronic plantar fasciitis, a single blinded randomized clinical trial. Pain Med Malden Mass. 2016;17(September (9)):1722–1731. doi: 10.1093/pm/pnw113. [DOI] [PubMed] [Google Scholar]
- 11.Aqil A., Siddiqui M.R.S., Solan M., Redfern D.J., Gulati V., Cobb J.P. Extracorporeal shock wave therapy is effective in treating chronic plantar fasciitis: a meta-analysis of RCTs. Clin Orthop. 2013;471(November (11)):3645–3652. doi: 10.1007/s11999-013-3132-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Atkins D., Crawford F., Edwards J., Lambert M. A systematic review of treatments for the painful heel. Rheumatol Oxf Engl. 1999;38(October (10)):968–973. doi: 10.1093/rheumatology/38.10.968. [DOI] [PubMed] [Google Scholar]
- 13.Martin R.L., Irrgang J.J., Conti S.F. Outcome study of subjects with insertional plantar fasciitis. Foot Ankle Int. 1998;19(December (12)):803–811. doi: 10.1177/107110079801901203. [DOI] [PubMed] [Google Scholar]
- 14.Buchbinder R. Clinical practice. Plantar fasciitis. N Engl J Med. 2004;350(May (21)):2159–2166. doi: 10.1056/NEJMcp032745. [DOI] [PubMed] [Google Scholar]
- 15.Tahririan M.A., Motififard M., Tahmasebi M.N., Siavashi B. Plantar fasciitis. J Res Med Sci Off J Isfahan Univ Med Sci. 2012;17(August (8)):799–804. [PMC free article] [PubMed] [Google Scholar]
- 16.Porter M.D., Shadbolt B. Intralesional corticosteroid injection versus extracorporeal shock wave therapy for plantar fasciopathy. Clin J Sport Med Off J Can Acad Sport Med. 2005;15(May (3)):119–124. doi: 10.1097/01.jsm.0000164039.91787.dc. [DOI] [PubMed] [Google Scholar]
- 17.Acevedo J.I., Beskin J.L. Complications of plantar fascia rupture associated with corticosteroid injection. Foot Ankle Int. 1998;19(February (2)):91–97. doi: 10.1177/107110079801900207. [DOI] [PubMed] [Google Scholar]
- 18.Kim C., Cashdollar M.R., Mendicino R.W., Catanzariti A.R., Fuge L. Incidence of plantar fascia ruptures following corticosteroid injection. Foot Ankle Spec. 2010;3(December (6)):335–337. doi: 10.1177/1938640010378530. [DOI] [PubMed] [Google Scholar]
- 19.Tatli Y.Z., Kapasi S. The real risks of steroid injection for plantar fasciitis, with a review of conservative therapies. Curr Rev Musculoskelet Med. 2009;2(March (1)):3. doi: 10.1007/s12178-008-9036-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fox T.P., Oliver G., Wek C., Hester T. Plantar fascia calcification a sequelae of corticosteroid injection in the treatment of recalcitrant plantar fasciitis. BMJ Case Rep [Internet] 2013 doi: 10.1136/bcr-2013-200303. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3762432/ [cited 2017 Jun 12]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ang T.W.A. The effectiveness of corticosteroid injection in the treatment of plantar fasciitis. Singapore Med J. 2015;56(August (8)):423–432. doi: 10.11622/smedj.2015118. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.