Abstract
Background
The concept of preparing the body before a stressful event, such as surgery, has been termed “prehabilitation” (preoperative physiotherapy and exercise programs). Prehabilitation programs for people awaiting total knee arthroplasty (TKA) have positive effects on patients health status and may also lead to better postoperative outcomes.
Aim
The purpose of this study was to examine effect of a prehabilitation program on knee pain, functional ability among patients with knee osteoarthritis after TKA surgery.
Study Design
A Prospective Controlled Study.
Patients and Methods
Subjects enrolled in this prospective controlled study who referred to our Orthopedics and Traumatology outpatient clinic between 2014 April–2015 May, had severe OA with pain not responsive to conservative treatment and scheduled for unilateral TKA. Subjects were assigned to a control or prehabilitation group. Patients of prehabilitation group were recruited from the orthopaedic waiting lists for primary unilateral TKA. Partipicants in the prehabilitation group were prescribed a training program that consisted of education and home-based exercise 12 weeks before the operation. After the TKA, all subjects partipicated in the same postoperative rehabilitation protocol. Evaluations were made before the surgery, with follow-up assessments at 3 and 6 months after surgery. Knee pain was assessed by the use of a 10-cm Visual Analog Scale (VAS) and function assesed by Knee injury and Osteoarthritis Outcome Score (KOOS) scale.
Results
A statistically significant improvement was observed in the values of VAS and all subsclaes of KOOS in both groups at third and sixth month compared to baseline. The intergroup comparison of the improvement (pre-post scores at sixth month) did not show any statistically significant diffeferences in VAS and KOOS scores.
Conclusion
Our results show that prehabilitation before TKA is not superior to surgical treatment alone but about 20% of the patients changed their operation decision. So it is important to be able to postpone this process especially in the early period.
Keywords: Function, Pain, Prehabilitation, Total knee arthroplasty
1. Introduction
Osteoarthritis (OA) is a chronic, progressive and noninflamatory joint disease, of unknown cause, the end stage of degeneration articular and subchondral bone.1,2 It is most prevalent in the hands and the weight-bearing joints of the hips and the knees.1 Characteristics of knee OA include decrease in strength and functional ability and increase in joint pain.3 There is no definitive cure for knee OA, management strategies are targeted at reduction pain and improve function. When conservative managemets fails, total knee arthroplasty (TKA) becomes the traetment of choice.2 TKA is a safe and cost-effective treatment for alleviating pain and restoring physical function in patients who do not respond to non-surgical therapies. TKA involves removal of the OA-diseased knee joint, which is replaced by a prosthetic device and commonly involves prolonged rehabilitation.3 Poor preoperative function are reported to reduce the magnitude of postoperative functional recovery.2,4 Preoperative strength, functional ability and pain have been shown to be greatest overall predictors of postoperative function for those undergoing TKA.3,5 Individulas with knee OA have significantly lower quadriceps strength compared to their non-affected leg or with healthy age-matched controls.6 Patients with knee OA, even those with severe disease, have demonstrated they can reduce their knee pain, improve their quadriceps strength, and improve their functional ability through regular exercise training.3 The concept of preparing the body before a stressful event, such as surgery, has been termed “prehabilitation” (preoperative physiotherapy and exercise programmes).7 Prehabilitation have been proposed as a potential way to expetide recovery times and improve overall extend of recovery in patients planning to undego joint replacement.8 Although some studies have reported no benefit of this presurgery interventions, others have demonstrated that prehabilitation programmes for people awaiting TKA have positive effects on patients health status and may also lead to better postoperative outcomes.2 Unfortunately it is not possible to compare these studies because lack of consistency in type, frequency, duration and intensity of the exercise intervention and different evaluation criteria were utilised. So this area still needs new studies.
TKA operation is usually planned for the elderly patients; altough sometimes younger patients may develop prosthetic need. Timing for surgery is very important because of the life of the prothesis. It is important to be able to postpone this process in the early period.
The purpose of this study was to examine effect of a prehabilitation program on knee pain, functional ability among patients with knee OA after TKA surgery. To examine this purpose we addressed two hypotheses:
-
1
In prehabilitated patients, postoperative functional levels and pain status are better than who are not prehabilitated.
-
2
After prehabilitation, the patients may change their decision about having the surgery.
2. Methods
Subjects enrolled in this prospective controlled study who referred to our Orthopedics and Traumatology outpatient clinic between 2014 April–2015 May, had severe OA with pain not responsive to conservative treatment and scheduled for unilateral TKA. Exclusion criteria included inflammatory arthritis, dermatological conditions affecting the thigh, neurological disorders, implanted pacemakers, history of uncontrolled angina, severe cardiomyopathy, contraindications for exercise or were undergoing a revision surgery. All patients provided written informed consent. The study was approved by the local Ethics Committee.
The demographic characteristics of patients [age, gender, weight, height, body mass index (BMI)] and Kellgren-Lawrence radiographic grade (KLS)9] of the problem (affected knee)] knee were recorded.
Subjects were assigned to a control or prehabilitation group. Patients of prehabilitation group were recruited from the orthopaedic waiting lists for primary unilateral TKA. Partipicants in the prehabilitation group were prescribed a training program that consisted of education and home-based exercise 12 weeks before the operation. They received general education about OA, joint protection, home safety, and TKA. A home-based exercise program (ankle pumping, knee range of motion, straight leg rising, quadriceps isometric, streching and strengthening) was practically demonstrated by a physiatrist and the importance of continuning regular appropriate exercise were explained. Partipicipants performed 2 sets of 10 repetitions of each exercise for five days per week at home before the operation.
Moreover, a training and exercise manual booklet was given to all the patients. The prehabilitation group checked by phone weekly. After the TKA, all subjects partipicated in the same postoperative rehabilitation protocol.
Evaluations were made 3 months before the surgery, with follow-up assessments at 3 and 6 months after surgery in the prehabilitation group. In the control group 3 visits made; before TKA, with follow-up assessments at 3 and 6 months after TKA.
Knee pain was assessed by the use of a 10-cm Visual Analog Scale (VAS). Subjects were requested to indicate on the VAS the severity of knee pain they experienced in the knee at rest (VASpr) and during activity (VASpa). The VAS was anchored at the terminal points of the scale by the terms ‘no pain’ and ‘extreme pain’. Higher scores indicate increased severity. The VAS has been demonstrated to correlate well with physician assesment of pain and to have high test-retest reliability.10, 11, 12
Knee injury and Osteoarthritis Outcome Score (KOOS) is a useful scale in evaluating symptoms and functional status related to knee injury and knee OA. This tool has five subscales, namely pain, symptoms, daily living, sports and recreational activities, and quality of life related to the knee. Each subscale consists of multiple items scored on a 4-point Likert scale. Scores range from 0 (worst) to 100 (best).13 Reliability and validity of the Turkish version of the KOOS was made by Paker and at al.14
The orthopaedic surgeon used a standart anterior midline surgical approach to the affected knee with cement application technique while preserving lateral the collateral ligament and the posterior cruciate ligament. Releasing was performed as necessary in the medial collateral ligament. No resurfacing the patella was performed.
Patients were allowed to take paracetamol if needed
Statistical tests were performed using the Statistical Package for Social Sciences version 21.00 (SPSS,Inc.,Chicago,IL). Descriptive data were presented as mean ± standard deviation (SD). Categorical data were given as counts/percentage (n/%). Comparison of gender was carried out using chi-squared test. The conformability of the data to the normal distribution was tested with Shapiro-Wilktest. Analysis were performed on intention-to-treat basis which encompasses all patients who were included. Independent t-tests were used to evaluate potential group differences for age and BMI. Non-parametric Friedman test was used to compare within group differences. Post hoc analyses were performed using the Wilcoxon signed ranks test with Bonferroni adjustment for multiple comparisons. Between group comparisons were performed using the Mann-Whitney U test. Confidence interval was set at 95% and the level of significance was set to 5%. The intergroup comparison of the improvement (differences of pre-post scores) between two groups was also evaluated with Mann-Whitney U tests.
3. Results
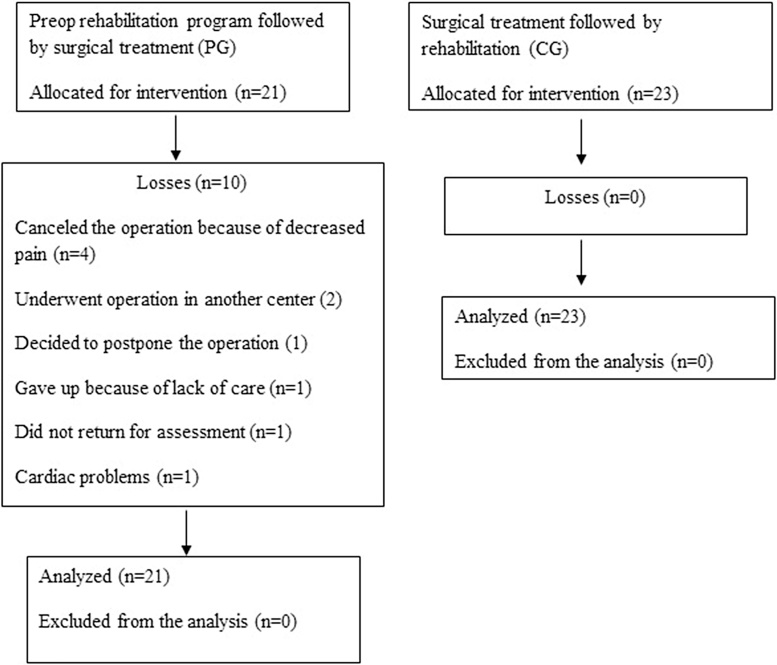
Forty-four patients included in the study. Thirty-four patients completed the assessment (Fig. 1). Four patients (19.4%) in the prehabilitation group canceled the operation because of decreased pain. Clinical and radiographic features of the participants are represented in Table 1. The groups were homogeneous regarding age, gender, BMI and OA grade evaluated with KLS.
Fig. 1.
Flow diagram of the study population.
Table 1.
Demographic and radiological characteristics of both groups.
| Prehabilitation Group (n:21) | Control Group (n:23) | P | |
|---|---|---|---|
| Gender (Female/Male) (n) | 18/3 | 18/5 | >0.05 |
| Age (years) (mean ± SD) | 67.8 ± 6.3 | 69.7 ± 6.4 | >0.05 |
| BMI | 32.8 ± 5.9 | 30.2 ± 4.9 | >0.05 |
| Stay in hospital | 5.5 ± 2.0 | 7.9 ± 2.3 | >0.05 |
| KL grade 3 | 8 | 12 | >0.05 |
| KL grade 4 | 13 | 11 |
A statistically significant improvement was observed in the values of VASpr, VAS pa, all subsclaes of KOOS in both groups at third and sixth month compared to baseline. There were no significant differences between the third and sixth month values within both groups. There were also no statistically significant differences between groups according to VAS pr, VAS pa, all subsclaes of KOOS at third and sixth month (Table 2).
Table 2.
Baseline, third and sixth month results of VAS and KOOS of prehabilitation and control groups.
| Prehabilitation Group (n:21) |
Control Group (n:23) |
|||||
|---|---|---|---|---|---|---|
| T1 | T2 | T3 | T1 | T2 | T3 | |
| VASpr | 4.1 ± 2.9 | 0.7 ± 0.9 | 0.4 ± 0.9** | 3.2 ± 2.7 | 0.8 ± 1.2 | 0.8 ± 1.1** |
| VASpa | 7.6 ± 1.6 | 1.7 ± 1.6 | 1.5 ± 1.5** | 7.6 ± 1.5 | 2.6 ± 2.4 | 2.3 ± 2.3** |
| KOOS | 36.7 ± 10.9 | 80.2 ± 15.9 | 82.2 ± 16.1** | 39.6 ± 12.5 | 85.9 ± 10.6 | 85.5 ± 9.5** |
| KOOSstiffness | 50.8 ± 16.6 | 83.1 ± 15.9 | 87.1 ± 13.3** | 47.0 ± 17.0 | 92.4 ± 10.2 | 91.4 ± 11.7** |
| KOOSpain | 34.3 ± 11.7 | 85.6 ± 15.2 | 87.9 ± 15.4** | 44.9 ± 15.8 | 88.9 ± 11.0 | 92.7 ± 8.3** |
| KOOSdaily living activities | 39.8 ± 15.9 | 83.9 ± 16.6 | 87.2 ± 18.3** | 43.9 ± 14.2 | 90.4 ± 10.5 | 91.1 ± 9.2** |
| KOOSsports | 9.5 ± 11.9 | 54.1 ± 23.5 | 52.8 ± 24.4** | 18.3 ± 17.7 | 59.8 ± 14.9 | 56.1 ± 13.1** |
| KOOSquality of life | 32.4 ± 15.9 | 75.0 ± 22.4 | 76.1 ± 19.7** | 23.7 ± 15.1 | 80.7 ± 19.0 | 72.8 ± 18.5** |
T1 Baseline; T2 three months after surgery; T3 six months after surgery; VASpr Visual Analog Scale pain resting; VASpa Visual Analog Scale pain acitivity; KOOS Knee injury and Osteoarthritis Outcome Score.
*p < 0.05, **p < 0.01 within groups.
The intergroup comparison of the improvement (pre-post scores at sixth month) did not show any statistically significant diffeferences in VAS and KOOS scores (Table 3).
Table 3.
Intergroup comparison of the improvement (pre-post scores at sixth month /T1-T3) of VAS, KOOS of prehabilitation and control groups.
| Pre-post scores (T1–T3) |
|||
|---|---|---|---|
| Prehabilitation Group | Control Group | p | |
| VASpr | 2.9 ± 3.3 | 2.4 ± 2.2 | 0.942 |
| VASpa | 6.0 ± 1.8 | 5.3 ± 2.3 | 0.403 |
| KOOS | −49.0 ± 19.9 | −45.9 ± 10.5 | 0.258 |
| KOOS stiffness | −43.2 ± 23.1 | −44.4 ± 15.9 | 0.828 |
| KOOS pain | −56.7 ± 21.7 | −47.8 ± 15.6 | 0.071 |
| KOOS daily living activities | −51.8 ± 21.9 | −47.2 ± 11.9 | 0.344 |
| KOOS sports | −44.1 ± 28.9 | −37.8 ± 21.1 | 0.612 |
| KOOS quality of life | −48.4 ± 25.9 | −49.2 ± 20.8 | 0.913 |
4. Discussion
OA is a degenerative disease for which there is currently no known cure. When conservative managemets fails, TKA becomes the treatment of choice. Long wait times for surgery have deleterious effects on health status: both pain and function have been shown to deteriorate in patients waiting for TKA. Several studies have reported preoperative physical function is a major determinant of post-operative physical function. Therefore minimizing deterioration in function and worsening of pain for people awaiting TKA is important to maximize their rehabilitation potential.2 In the present study, both groups had substantial improvement with respect to pain and functional ability. Prehabilitation before TKA is not superior to surgery providing pain relief and improving function. But 19.4% of the patients in prehabilitation group canceled the operational time as a result of decreased pain.
Knee OA can be more severe in women, especially after age 50, compared to men. In one study females had more severe radiographic knee OA than males, which was weighted more towards the presence of osteophytes. Srikanth at all also reported that man had 45% lower incident risk of knee OA than woman. The presence of sex differences in OA prevalence and incidence, with females generally at a higher risk. Females also tend to have more severe knee OA, particularly after menopausal age. The site differences indicate the need for further studies to explore mechanisms underlying OA.15 In our study 82% of patients were female. This was consistent with the criterion of osteoarthritis, which has a strong association with the female gender and advanced age.16 A number of studies demonstrate the assosication of preoperative comorbidities with a worse post-operative outcome but others do not observe such an association. Age, however should not be a barrier to having a good outcome from TKA, with reports of a successful outcome in patients aged over 80 years.17 The mean age group of our patients was 67.8 and 69.7 in the prehabilitation and control group, respectively and patients with advanced comorbidity were not included in the study.
The majority of published studies on the effects of a prehabilitation intervention used prehabilitation programmes of shorter duration and these studies often show no or little effect of prehabilitation. As in our study, Nunez and colleauges used a 3-month prehabilitation programme for patients awaiting knee TKA, using the Western Ontario and McMaster Universities Arthritis Index(WOMAC) as the primary outcome measure, they found that partipiciants in the prehabilitation programme showed a significant improvement in self reported function compared to a control group receiving usual pharmalogical care.18 Topp and his collageues 5-month protocol study involving a usual care and intervention group supported the theory of prehabilitation.3 Mat Eil Ismail and his collageues reported that six-week preoperative physiotherapy showed no significant impact on short-term functional outcomes (KOOS subscales) and range of motion of the knee following primary TKA.19
In a case study including two TKA patients: 1 of whom partipicated in a 4 week prehabilitation programme where as the other received the ususal care before TKA, prehabilitation had a positive effect on functional task (6-minute walk, number of times up from a chair in 30 s, WOMAC index) and knee proprioception before surgery and after the surgery intervention case continued to exhibit higher levels of functioning and less pain compared with the usual care condition.7 These interventions were diverse, there was lack of consistency in type, frequency, duration and intensity of the exercise intervention utilised.20
In our study patients who underwent TKA had significant improvement in symptom and functional outcomes regardless of whether they underwent prehabilitation or not. The statistical results for KOOS subscales correlated with previous reports suggesting that TKA improved functional status and relieved pain.19 In our study, 4 (19.4%) of the patients who were initially included in the prehabilitation program were changed decision of the operation due to a decrease in pain, so we saw that we can postpone the operation age of patients who undergo regular prehabilitation programme. This result showed the importance of preoperative exercise in these patients.
Escalante and Beardmore attempted to identify predictors of length of hospital stay after TKA and total hip artroplasty (THA) surgeries. They concluded that prehabilitation programmes enhance postoperative functional ability and decrease post-operative hospital stay.21 And also Fernandes and his colleauges found that patients allocated to exercise had a lower total length of hospital stay and total cost during the follow up period.22 In our study the lenght of hospital stay was shorter in prehabilitation group than control group, but it did not reach a statistically significant level.
Clinical comissioning group typically will found four to six sessions of outpatient postoperative physiotherapy, however Rajan at all found that this short course of physiotherapy is not needed by all patients to help them recover after surgery.23,24 Moffet at al. found that 12–18 h or a mean of 17 visits may be needed to produce benefit.25 The fact remains that in the literature some studies have focused on home exercise, and home exercises have been shown to be as effective as supervised physical therapy.26 We have chosen to focus our intervention as a community home-based treatment package. We believe this to be particularly suited to those patients likely to find it hard to access traditional physiotherapy because of transport difficulaties, social isolation, frailty and low self-efficacy.
Consumption of pain medication was not strictly measured in this study and only allowed to take paracetamol if needed. The dose and amount of paracetamol taken not recorded. It may have affected self reports of pain. In our hospital, unilateral TKA is often preferred considering perioperative morbidity (infectious, venous tromboembolism, etc.) and mortality. As a result of this we decided to include only unilateral TKA patients at the beginning of the study. Further studies including bilateral TKA are necessary.
In conclusion, our results show that prehabilitation before TKA is not superior to surgical treatment alone at long term follow-up but about 20% of the patients changed their operation decision. So it is important to be able to postpone this process especially in the early period.
Conflict of interest
No conflict of interest was declared by the authors.
Financial disclosure
The authors declared that this study has received no financial support.
Footnotes
The manuscript has been presented in a 25. National Turkish Orthopedics and Traumatology Congress as a poster presentation at 27/10/2015-01/11/2015 in Antalya, Turkey.
Contributor Information
Ebru Aytekin, Email: ebruaytekin@hotmail.com.
Erhan Sukur, Email: erhansukur@hotmail.com.
Nuran Oz, Email: nrnkvrgcz@gmail.com.
Atakan Telatar, Email: atakantelatar@gmail.com.
Saliha Eroglu Demir, Email: saliha45@yahoo.com.
Nil Sayiner Caglar, Email: nilcag@yahoo.com.
Yusuf Ozturkmen, Email: yozturkmen@gmail.com.
Levent Ozgonenel, Email: levento26@yahoo.com.
References
- 1.Marcinkowski K., Wong V.G., Dignam D. Getting back to the future: a grounded theory study of the patient perspective of total knee joint arthroplasty. Orthop. Nurs. 2005;24:202–209. doi: 10.1097/00006416-200505000-00009. [DOI] [PubMed] [Google Scholar]
- 2.Desmeules F., Hall J., Woodhouse L.J. Prehabilitation improves physical function of individuals with severe disability from hip or knee osteoarthritis. Physiother. Can. 2013;65:116–124. doi: 10.3138/ptc.2011-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Topp R., Swank A.M., Quesada P.M., Nyland J., Malkani A. The effect of prehabilitation exercise on strength and functioning after total knee arthroplasty. PMR. 2009;1:729–735. doi: 10.1016/j.pmrj.2009.06.003. [DOI] [PubMed] [Google Scholar]
- 4.McKay C., Prapavessis H., Doherty T. The effect of a prehabilitation exercise program on quadriceps strength for patients undergoing total knee arthroplasty: a randomized controlled pilot study. PMR. 2012;4:647–656. doi: 10.1016/j.pmrj.2012.04.012. [DOI] [PubMed] [Google Scholar]
- 5.Brown K., Swank A.M., Quesada P.M., Nyland J., Malkani A., Topp R. Prehabilitation versus usual care before total knee arthroplasty: a case report comparing outcomes within the same individual. Physiother. Theory Pract. 2010;26:399–407. doi: 10.3109/09593980903334909. [DOI] [PubMed] [Google Scholar]
- 6.Swank A.M., Kachelman J.B., Bibeau W., Quesada P.M., Nyland J., Malkani A., Topp R.V. Prehabilitation before total knee arthroplasty increases strength and function in older adults with severe osteoarthritis. J. Strength Cond. Res. 2011;25:318–325. doi: 10.1519/JSC.0b013e318202e431. [DOI] [PubMed] [Google Scholar]
- 7.Jaggers J.R., Simpson C.D., Frost K.L., Quesada P.M., Topp R.V., Swank A.M., Nyland J.A. Prehabilitation before knee arthroplasty increases postsurgical function: a case study. J Strength Cond. Res. 2007;21:632–634. doi: 10.1519/R-19465.1. [DOI] [PubMed] [Google Scholar]
- 8.Wang L., Lee M., Zhang Z., Moodie J., Cheng D., Martin J. Does preoperative rehabilitation for patients planning to undergo jointreplacement surgery improve outcomes? A systematic review and meta-analysis of randomised controlled trials. BMJ Open. 2016;6:e009857. doi: 10.1136/bmjopen-2015-009857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ravaud P., Chastang C., Auleley G.R., Giraudeau B., Royant V., Amor B., Genant H.K. Assessment of joint space width in patients with osteoarthritis of the knee: a comparison of 4 measuring instruments. J. Rheumatol. 1996;23:1749–1755. [PubMed] [Google Scholar]
- 10.Kersten P., Küçükdeveci A.A., Tennant A. The use of the visual analogue scale (VAS) in rehabilitation outcomes. J. Rehabil. Med. 2012;44:609–610. doi: 10.2340/16501977-0999. [DOI] [PubMed] [Google Scholar]
- 11.Jensen M.P., Karoly P., Braver S. The measurement of clinical pain intensity: a comparison of six methods. Pain. 1986;27:117–126. doi: 10.1016/0304-3959(86)90228-9. [DOI] [PubMed] [Google Scholar]
- 12.Price D.D., McGrath P.A., Rafii A., Buckingham B. The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain. 1983;17:45–56. doi: 10.1016/0304-3959(83)90126-4. [DOI] [PubMed] [Google Scholar]
- 13.Roos E.M., Lohmander L.S. The knee injury and osteoarthritis outcome score (KOOS): from joint injury to osteoarthritis. Health Qual. Life Outcomes. 2003;1:64. doi: 10.1186/1477-7525-1-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Paker N., Buğdayci D., Sabirli F., Ozel S., Ersoy S. Knee injury and osteoarthritis outcome score: reliability and validation of the Turkish version. Turkiye Klinikleri J. Med. Sci. 2007;27:350–356. [Google Scholar]
- 15.Srikanth V.K., Fryer J.L., Zhai G., Winzenberg T.M., Hosmer D., Jones G. A meta-analysis of sex differences prevalence, incidence and severity of osteoarthritis. Osteoarthr. Cartil. 2005;13:769–781. doi: 10.1016/j.joca.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 16.Felson D.T., Zhang Y., Hannan M.T., Naimark A., Weissman B.N., Aliabadi P., Levy D. The incidence and natural history of knee osteoarthritis in the elderly. The framingham osteoarthritis study. Arthritis Rheum. 1995;38:1500–1505. doi: 10.1002/art.1780381017. [DOI] [PubMed] [Google Scholar]
- 17.Barker K.L., Beard D., Price A., Toye F., Underwood M., Drummond A., Collins G., Dutton S., Campbell H., Kenealy N., Room J., Lamb S.E. COmmunity-based rehabilitation after knee arthroplasty (CORKA): studyprotocol for a randomised controlled trial. Trials. 2016;17:501. doi: 10.1186/s13063-016-1629-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nunez M., Nuñez E., Segur J.M., Macule F., Quinto L., Hernandez M.V., Vilalta C. The effect of an educational program to improve health-related quality of life in patients with osteoarthritis on waiting list for total knee replacement: a randomized study. Osteoarthr. Cartil. 2006;14:279–285. doi: 10.1016/j.joca.2005.10.002. [DOI] [PubMed] [Google Scholar]
- 19.Mat Eil Ismail M.S., Sharifudin M.A., Shokri A.A., Ab Rahman S. Preoperative physiotherapy and short-term functional outcomes of primary total knee arthroplasty. Singap. Med J. 2016;57:138–143. doi: 10.11622/smedj.2016055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Valkenet K., van de Port I.G., Dronkers J.J., de Vries W.R., Lindeman E., Backx F.J. The effects of preoperative exercise therapy on postoperative outcome: a systematic review. Clin. Rehabil. 2011;25:99–111. doi: 10.1177/0269215510380830. [DOI] [PubMed] [Google Scholar]
- 21.Escalante A., Beardmore T.D. Predicting length of stay after hip or knee replacement for rheumatoid arthritis. J. Rheumatol. 1997;24:146–152. [PubMed] [Google Scholar]
- 22.Fernandes L., Roos E.M., Overgaard S., Villadsen A., Søgaard R. Supervised neuromuscular exercise prior to hip and knee replacement: 12-month clinical effect and cost-utility analysis alongside a randomised controlled trial. BMC Musculoskelet. Disord. 2017;18:5. doi: 10.1186/s12891-016-1369-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Artz N., Dixon S., Wylde V., Beswick A., Blom A., Gooberman-Hill R. Physiotherapy provision following discharge after total hip and total knee replacement: a survey of current practice at high-volume NHS hospitals in England and wales. Musculoskelet. Care. 2013;11:31–38. doi: 10.1002/msc.1027. [DOI] [PubMed] [Google Scholar]
- 24.Rajan R.A., Pack Y., Jackson H., Gillies C., Asirvatham R. No need for outpatient physiotherapy following total knee arthroplasty: a randomized trial of 120 patients. Acta Orthop. Scand. 2004;75:71–73. doi: 10.1080/00016470410001708140. [DOI] [PubMed] [Google Scholar]
- 25.Moffet H., Collet J.P., Shapiro S.H., Paradis G., Marquis F., Roy L. Effectiveness of intensive rehabilitation on functional ability and quality of life after first total knee arthroplasty: a single-blind randomized controlled trial. Arch. Phys. Med. Rehabil. 2004;85:546–556. doi: 10.1016/j.apmr.2003.08.080. [DOI] [PubMed] [Google Scholar]
- 26.Büker N., Akkaya S., Akkaya N., Gökalp O., Kavlak E., Ok N., Kıter A.E., Kitiş A. Comparison of effects of supervised physiotherapy and a standardized home program on functional status in patients with total knee arthroplasty: a prospective study. J. Phys. Ther. Sci. 2014;26:1531–1536. doi: 10.1589/jpts.26.1531. [DOI] [PMC free article] [PubMed] [Google Scholar]