Abstract
Introduction
The aim of this study is to compare the outcomes of surgical management after primary anterior shoulder dislocation to the outcomes of patients who have surgical stabilization after recurrent anterior shoulder instability.
Methods
A Medline (PubMed) search was performed in November of 2016 using the following key terms: shoulder, labrum, Bankart, instability, repair, outcome, recurrent. In May 2017 a Cochrane search was performed using similar key terms to ensure we included all studies. Only level I and II studies were included.
Results
There were three studies that compared primary repair to delayed repair. In all three studies, the rate of recurrence was higher in group R than group S. When pooled, there was not a statistically significant difference between these groups, but there was a slightly higher odds of recurrence in group R (pooled OR 2.08, CI 0.69–6.26, p = 0.19). No significant differences were appreciated in functional outcomes or complications in these two groups.
Conclusion
Further level I and level II studies to compare surgical treatment after first time and recurrent instability are needed. This study failed to find a statistically significant difference in recurrence rates in patients who had stabilization acutely after a single episode compared to patients with recurrent instability events, although results suggest there may be a small benefit in primary stabilization.
Keywords: Shoulder, Labrum, Bankart, Dislocation, Instability, Repair, Outcome, Recurrent, PRISMA, Cochrane
1. Introduction
There is ongoing controversy regarding the optimal treatment of patients with first time, anterior shoulder instability. Nonoperative treatment has long been the standard treatment, with surgical repair reserved for patients with recurrent instability.1, 2, 3, 4 This treatment paradigm has remained relatively unchallenged, and remains the prevailing algorithm for management.
Continued use of this algorithm depends on several assumptions, including: (1) There is little or no structural damage from further recurrent episodes of instability (2) surgical management of instability is similarly effective whether completed acutely, after one episode, or when completed after multiple (≥2) episodes of instability. A recent case series, however, challenged these assumptions, demonstrating lower failure rate and less radiographic changes with surgical management after primary dislocation.5
Numerous studies have investigated outcomes of surgical management for recurrent shoulder instability (≥2 episodes of shoulder instability).5, 6, 7, 8, 9 The focus of these investigations has been into the recurrence rate with different approaches, anchors, techniques, and risk factors for failure of this approach. In addition, several studies have investigated the success rates of nonoperative and surgical management after a first time dislocation episode.10, 11, 12 These studies confirm a high rate of recurrent instability with nonoperative management in young, active patients. They also demonstrate good results with surgical management, but recurrence and stiffness are concerns.13, 14, 15 Given the small number of patients in each series, they have limited power to investigate the outcome of patients who go on to have recurrent instability, followed by subsequent surgery; the situation that is the “standard of care.”
The goal of this study was to compare the outcomes of surgical management after primary anterior shoulder dislocation, to the outcomes of patients who have surgical stabilization after recurrent anterior shoulder instability. A systematic review was conducted to evaluate the null hypothesis that patients surgically treated after a primary shoulder instability episode will not experience significant differences in recurrence rates, outcomes, post-operative complications or range of motion compared to patients with recurrent shoulder instability episodes.
2. Materials and methods
The goal of this systematic review was to compare the instability and revision surgery frequency after either open or arthroscopic Bankart repair for patients who experienced a single episode of instability before surgery (Group S) and patients who experienced recurrent (≥2) episodes of instability before surgery (Group R). Secondary outcome measures included clinical outcome measures such as range of motion, Rowe scores, and Constant Scores. We used only level I and level II studies in this analysis.
2.1. Literature search
We performed a Medline (PubMed) search in November of 2016 using the following key terms: shoulder, labrum, Bankart, instability, repair, outcome, recurrent. In May 2017 we performed a Cochrane search using similar key terms to ensure we included all studies. The studies’ title and abstract were first reviewed for inclusion. First pass inclusion criteria included English language articles in peer reviewed journals with a comparison group. Case reports, case series, animal studies, imaging studies, review articles, only non-surgical/conservative treatment, bio-mechanical/cadaveric studies or nonglenohumeral studies were excluded at this point. The remaining papers were reviewed in their entirety to determine if they would be included in the study. Second pass inclusion criteria included no revision surgeries, accessible pre-operative and post-operative instability data. Retrospective studies and studies lacking a comparison group were excluded, making this a systematic review of level I and II studies only. The reference section of each accepted paper was also reviewed to ensure all eligible studies were included in this review.
2.2. Quality assessment
We assessed the quality of accepted articles using a modified Coleman Methodology Score (CMS). Articles were graded on a scale of 0–100. Articles scoring higher have reduced bias, chance and confounding factors. Two authors independently reviewed all articles and scored them from 0 to 100. Disputes were resolved with discussion.
2.3. Data acquisition
Three authors reviewed the literature and recorded the data from each study. Study information and patient demographics, including age, sex, time from first injury to surgery and length of follow up were recorded (Table 1). The procedure for each patient (open and/or arthroscopic Bankart) was recorded, as well as any other additional procedures. Patients who underwent a bony procedure (Latarjet, Bristow etc.) were excluded from the data analysis. Furthermore, non-surgical patients were excluded from the data analysis.
Table 1.
Demographics. Study demographics.
| Authors | Title | Year | Study Design | Group | Level of Evidence | Number of shoulders total | Number of Shoulders usable for analysis | Average age of Patients | Male Patients (%) | Mean Follow Up, months (range) | Dominant Dislocations (%) | Time from First Injury |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Archetti Netto N et al.22 | Treatment of Bankart lesions in traumatic anterior instability of the shoulder: A randomized controlled trial comparing arthroscopy and open techniques | 2011 | R, PRO | R | 1 | 50 | 42 | 29.5 | 88.1 | 37.5 | 61.3 | 64.5 (43–89) mo |
| Arciero, R. A. et al.23 | Arthroscopic Bankart Repair Versus Nonoperative Treatment for Acute, Initial Anterior Shoulder Dislocations. | 1994 | NR, PRO | S | 2 | 36 | 21 | 20.5 (18–24) | NA | 32 (15–45) | 42.9 | 5.5 days |
| Balg, F., and P. Boileau24 | The Instability Severity Index Score. A Simple Pre-Operative Score to Select Patients for Arthroscopic or Open Shoulder Stabilisation. | 2007 | CC, PRO | R | 2 | 131 | 131 | 27.3 (14–26) | 78.6 | 31.2 (24–52) | 62.6 | NR |
| Bottoni, C. R. et al.15 | A Prospective, Randomized Evaluation of Arthroscopic Stabilization Versus Nonoperative Treatment in Patients with Acute, Traumatic, First-Time Shoulder Dislocations. | 2002 | R, PRO | S | 1 | 24 | 9 | 21.6 (19–26) | NR | 35 (17–56) | 40 | <10 days |
| Bottoni, Cr et al.25 | Arthroscopic versus open shoulder stabilization for recurrent anterior instability: a prospective randomized clinical trial | 2006 | R, PRO | R | 1 | 64 | 61 | 25 (19–42) | 98.4 | 29 (24–48) | 44.3 | 40 mo |
| Cole, B. J. et al.26 | Comparison of Arthroscopic and Open Anterior Shoulder Stabilization. A Two to Six-Year Follow-up Study. | 2000 | NR, PRO | R | 2 | 59 | 59 | 27.6 (15–53) | 86.4 | 53.1 (27–72) | 44 | 39.5 (3–360) mo |
| Elmlund, A. O. et al.27 | A 7-Year Prospective, Randomized, Clinical, and Radiographic Study after Arthroscopic Bankart Reconstruction Using 2 Different Types of Absorbable Tack. | 2009 | R, PRO | R | 1 | 36 | 36 | 28 (15–50) | 70 | 80.3 (64–96) | 60 | 34 (8–262) mo |
| Fabbriciani, C. et al.28 | Arthroscopic Versus Open Treatment of Bankart Lesion of the Shoulder: A Prospective Randomized Study. | 2004 | R, PRO | R | 1 | 60 | 60 | 25.5 (19–33) | 80 | 24 | 65 | 22.8 (6–52) mo |
| Hantes, M. E. et al.29 | Arthroscopic Repair for Chronic Anterior Shoulder Instability: A Comparative Study between Patients with Bankart Lesions and Patients with Combined Bankart and Superior Labral Anterior Posterior Lesions. | 2009 | NR, PRO | R | 2 | 63 | 63 | 27.6 (15–48) | 81 | 39.3 (25–66) | 60.3 | 3.73 (0.3–20) mo |
| Jaeger, A. et al.30 | Postoperative Functional Outcome and Stability in Recurrent Traumatic Anteroinferior Glenohumeral Instability: Comparison of Two Different Surgical Capsular Reconstruction Techniques. | 2004 | R, PRO | R | 1 | 62 | 62 | 28.9 (16–59) | 88.9 | 19.6 (5–75) | 51.6 | 53.4 mo |
| Jakobsen, B. W. et al.20 | Primary Repair Versus Conservative Treatment of First-Time Traumatic Anterior Dislocation of the Shoulder: A Randomized Study with 10-Year Follow-Up. | 2007 | R, PRO | S | 1 | 76 | 56 | 23 (15–39) | 81.1 | 120 | NR | NR |
| Jorgensen, U. et al.31 | Recurrent Post-Traumatic Anterior Shoulder Dislocation--Open Versus Arthroscopic Repair. | 1999 | R, PRO | R | 1 | 41 | 41 | median 28 (18–51) | 73.2 | median 36.2/36.6 (30–52) | 41.5 | NR |
| Karlsson J., L. et al.32 | Comparison of open and arthroscopic stabilization for recurrent shoulder dislocation in patients with a Bankart lesion | 2001 | NR, PRO | R | 2 | 119 | 108 | 26.4 (15–62) | 76.9 | 31.56 (24–63) | NR | 35.9 (4–360) mo |
| Kartus J., L. et al.33 | Arthroscopic and open shoulder stabilization using absorbable implants: A clinical and radiographic comparison of two methods | 1998 | NR, PRO | R | 2 | 36 | 36 | median 29/32 (16–62) | 75.8 | median 31/28 (18–46) | 55.6 | 43.5 (1–360) mo |
| Kim, D. S. et al.19 | Arthroscopic Repair for Combined Bankart and Superior Labral Anterior Posterior Lesions: A Comparative Study between Primary and Recurrent Anterior Dislocation in the Shoulder. | 2011 | NR, PRO | R | 2 | 110 | 110 | 26.4 (17–38) | 88.2 | 45.1 (25–118) | NR | 14.2 (2–32) days, 25.3 (10–28) mo |
| Kim, S. H. et al.34 | Accelerated Rehabilitation after Arthroscopic Bankart Repair for Selected Cases: A Prospective Randomized Clinical Study. | 2003 | R, PRO | S, R | 1 | 62 | 62 | 28.5 (15–39) | 80.6 | 31 (27–45) | NR | 40.4 (2–26) mo |
| Kirkley A et al.13 | Prospective randomized clinical trial comparing the effectiveness of immediate arthroscopic stabilization versus immobilization and rehabilitation in first traumatic anterior dislocations of the shoulder: long-term evaluation | 2005 | R, PRO | S | 1 | 31 | 19 | 23 | 54.8 | 79 (51–102) | 32.3 | NR |
| Larrain, M. V. et al.14 | Arthroscopic Repair of Acute Traumatic Anterior Shoulder Dislocation in Young Athletes. | 2001 | NR, PRO | S | 2 | 46 | 28 | 21 (17–27) | 94.4 | 67.4 (28–120) | NR | NR |
| Magnusson L. et al.35 | A prospective, randomized, clinical and radiographic study after arthroscopic Bankart reconstruction using 2 different types of absorbable tacks | 2006 | R, PRO | R | 1 | 40 | 40 | 28 (15–50) | 70 | 25.5 (23–35) | 60 | 34 (8–262) mo |
| Mahirogullari, M. et al.36 | Comparison of Outcomes of Two Different Surgeries in Regarding to Complications for Chronic Anterior Shoulder Instability. | 2006 | NR, PRO | R | 2 | 64 | 34 | 24.4 (19–33) | 100 | 25 (24–39) | 88.2 | 3.1 (1–6) yrs |
| Mahiroğulları M. et al.37 | Comparison between the results of open and arthroscopic repair of isolated traumatic anterior instability of the shoulder | 2010 | R, PRO | R | 1 | 64 | 64 | 25.5 | 100 | 26.3 | 78.1 | 4.1 (1–24) yrs |
| Milano G. et al.37 | Comparison between metal and biodegradable suture anchors in the arthroscopic treatment of traumatic anterior shoulder instability: a prospective randomized study | 2010 | R, PRO | R | 1 | 78 | 33 | 28 (16–43) | 83.3 | 24 | 50.0 | 36 (6–276) mo |
| Mohtadi N et al.2 | A Randomized Clinical Trial Comparing Open and Arthroscopic Stabilization for Recurrent Traumatic Anterior Shoulder Instability: Two-Year Follow-up with Disease-Specific Quality-of-Life Outcomes. | 2014 | R, PRO | R | 1 | 196 | 167 | 27.5 | 82 | 24 | 39 | 37.9 mo |
| Ng, D. Z., and V. P. Kumar39 | Arthroscopic Bankart Repair Using Knot-Tying Versus Knotless Suture Anchors: Is There a Difference? | 2014 | R, PRO | R | 1 | 87 | 87 | 21.1 | 88.5 | 32.4 (24–44.4) | NR | NR |
| Norlin, R.40 | Use of Mitek anchoring for Bankart repair: A comparative, randomized,prospective study with traditional bone sutures | 1994 | R, PRO | R | 1 | 40 | 20 | 24 median, (17–44) | 65 | 24 | 60 | NR |
| Nourissat, G. et al.41 | A Prospective, Comparative, Radiological, and Clinical Study of the Influence of The Remplissage Procedure on Shoulder Range of Motion after Stabilization by Arthroscopic Bankart Repair. | 2011 | NR, PRO | R | 2 | 32 | 32 | 24 | 62.5 | 27.5 | NR | NR |
| Potzl, W. et al.42 | Proprioception of the Shoulder Joint after Surgical Repair for Instability: A Long-Term Follow-up Study. | 2004 | NR, PRO | R | 2 | 14 | 14 | 28 (16–52) | 50 | 70.8 (66–90) | 92.9 | NR |
| Robinson CM et al.21 | Primary Arthroscopic Stabilization for a First-Time Anterior Dislocation of the Shoulder. A Randomized, Double-Blind Trial. | 2008 | R, PRO | S | 1 | 88 | 55 | 24.3 | 93.3 | 24 | 44.4 | 7.6 d |
| Salomonsson, B. et al.43 | The Bankart Repair Versus the Putti-Platt Procedure: A Randomized Study with Wosi Score at 10-Year Follow-up in 62 Patients. | 2009 | R, PRO | R | 1 | 66 | 32 | median 26 (16–33) | 81.2 | 120 | 57.6 | 42 (7–144) mo |
| Shih W-Y. et al.44 | Comparison of arthroscopic treatment with conservative treatment for acute first-time traumatic anterior shoulder dislocation in a high-demand population | 2011 | NR, PRO | S | 1 | 64 | 39 | 21.9 (18–29) | 100 | 18 | 33.3 | 5 (1–12) days |
| Sperber A et al.45 | Comparison of an arthroscopic and an open procedure for posttraumatic instability of the shoulder: a prospective, randomized multicenter study | 2001 | R, PRO | R | 1 | 56 | 56 | 26 (18–51) | 71.4 | 24 | 57.1 | 4.2 yrs |
| Steinbeck, J., and J. Jerosch46 | Arthroscopic Transglenoid Stabilization Versus Open Anchor Suturing in Traumatic Anterior Instability of the Shoulder. | 1998 | NR, PRO | R | 2 | 62 | 62 | 28.6 (17–49) | 82.3 | 38.1 (24–60) | 85.5 | NR |
| Tamai, K. et al.47 | Recurrences after the Open Bankart Repair: A Potential Risk with Use of Suture Anchors. | 1999 | NR, PRO | R | 2 | 87 | 87 | 25.4 (15–60) | 82.8 | 37.5 (18–85) | 59.8 | 6.4 yrs |
| Tan, C. K. et al.48 | Arthroscopic Stabilization of the Shoulder: A Prospective Randomized Study of Absorbable Versus Nonabsorbable Suture Anchors. | 2006 | R, PRO | R | 1 | 130 | 124 | 27.5 (17–49) | 87.1 | 31.2 (18–60) | 58.9 | 1.9 yrs |
| Warme, W. J. et al.49 | Nonabsorbable Versus Absorbable Suture Anchors for Open Bankart Repair. A Prospective, Randomized Comparison. | 1999 | R, PRO | R | 1 | 40 | 38 | 22 (17–46) | 74.4 | 25 (17–45) | NR | NR |
R, retrospective; PRO, prospective; NR, not reported.
Patients in each study were grouped into either a single instability episode prior to surgery (Group S) or multiple instability episodes prior to surgery (Group R). For these groups, an episode of subluxation or dislocation was considered to be an episode of instability. Apprehension on examination without subluxation or dislocation was not included. For example, a patient with 1 confirmed dislocation and multiple confirmed subluxations was placed in the multiple instability episodes group. We recorded the number of patients in each group who had revision surgery or an instability event after surgery. We also extracted clinical outcome data such as range of motion (ROM), Rowe scores and Constant scores, if present.
2.4. Statistical analysis
All statistical tests were performed with a standard software package (STATA 13.1, StataCorp, College Station, TX, USA). Descriptive data were first generated for Coleman quality scores and study demographics. Due to intrinsic differences in bias and study design, separate analyses were then performed for studies that directly compared recurrence rates by pre-operative instability status (n = 3 studies) versus those that did not (n = 32 studies). Among comparative studies (n = 3), a random effects meta-analysis using the Dersimian and Laird method16 was created to determine the effect of pre-operative instability status (single instability episode versus recurrent episodes) on post-operative instability rates. Effect heterogeneity was assessed using the I-squared measure as described by Higgins et al.17
Among non-comparative studies (n = 32 total), pooled rates of recurrence and other non-instability related complications were determined for studies with patients with a single pre-operative instability episode (n = 5 studies) versus studies with patients with multiple pre-operative episodes (n = 27 studies). Events were assumed to follow a Bernoulli distribution, and variance in within-study recurrence and complication rates were calculated with continuity correction.
Small study bias was assessed by funnel-plot and Begg's test of bias. Bias due to study reporting quality was assessed by correlation between recurrence and complication rates to modified Coleman methodology scores, level of evidence, and year of publication.
3. Results
3.1. Literature search
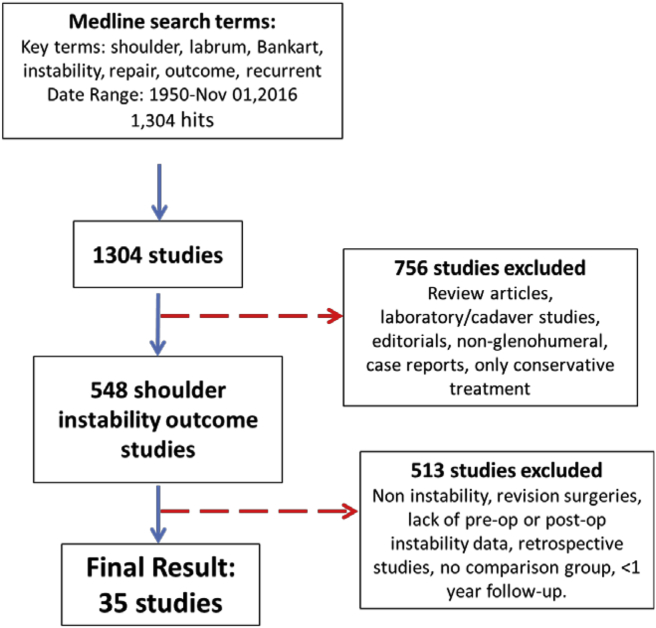
A total of 1304 papers were found in our initial search. Seven hundred and fifty-six studies were excluded because they were review articles, laboratory/cadaveric studies, editorials, non glenohumeral studies, case reports or only described conservative treatment methods. Five hundred and forty-eight studies were reviewed in their entirety, and 35 studies were included in the review. Five hundred and thirteen studies were excluded due to non-instability topics, patients reporting revision surgeries or lack of pre-operative or post-operative instability events. Retrospective studies and studies lacking a comparison group were also excluded at this point. Twenty-two randomized controlled trials (Level I) were included in our study, and 13 prospective comparison studies were included (Level II). Only one non-randomized, prospective study directly compared primary and recurrent shoulder instability. The literature review is documented per PRISMA guidelines (Fig. 1).
Fig. 1.
PRISMA. 35 studies were included in this meta-analysis.
3.2. Study quality and assessments of bias
The mean Coleman methodology score18 was high at 75.6 (SD 8.0, range 59–89), with higher scores observed for randomized studies (level I evidence, n = 12) (mean 78.3 SD SD 6.2, range 65–88) than non-randomized studies (level II evidence, n = 33) (71 SD 8.7 range SD 59–89)(p = 0.007, student's t-test). Coleman scores were positively correlated with year of publication (higher scores in more recent publications) (Spearman rho = 0.46, p = 0.005).
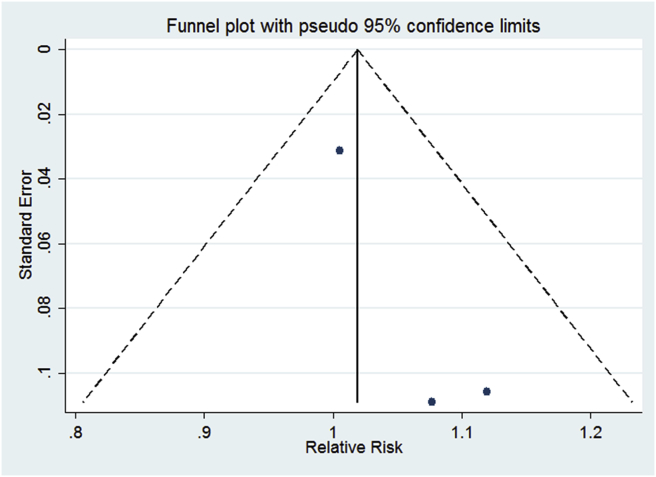
There was no significant small study bias among studies directly comparing recurrence rates by pre-operative instability status (n = 3 studies; Begg's p = 0.30) (Fig. 2). No small study bias existed in the remaining 32 studies with either patients with one pre-surgery instability episode (n = 5 studies, p = 0.22) or multiple episodes (n = 27 studies, p = 0.87). Reporting quality was not a significance source of bias, as modified Coleman scores were not correlated with recurrence rates for patients with a single (Spearman rho = 0.0, p = 1.0) or multiple pre-operative instability episodes (rho = −0.11, p = 0.57), or with non-instability related complication rates (rho = -0.03 p = 0.89). Year of publication and level of evidence were also not significantly correlated with recurrence rates or non-instability related complication rates (p > 0.20, all comparisons).
Fig. 2.
Funnel plot of the risk of recurrent instability after Bankart repair based on number of pre-operative instability episodes (one episode or multiple pre-operative instability episodes). There is no evidence of small study bias as indicated by inclusion of all study estimates (each of the 3 comparative studies in the meta-analysis are represented by a blue dot) within the 95% confidence limits (dashed lines). Additionally, Begg's test of small study bias was non-significant (p = 0.30).
3.3. Patient demographics
The authors, title, year published, study design, and level of evidence was recorded for each study included (Table 1). A total of 1751 patients with recurrent instability and 237 patients with a single instability episode were included. The pooled mean age was 25.7 (range 20.5–30) and percent male patients was 81% (range 50–100%). The number of shoulders, average age of patients, percentage male patients, and average length of follow up, dominant sided dislocations and time from first injury were recorded.
3.4. Surgical technique
In 16 studies, subjects underwent an arthroscopic Bankart repair for their instability. In 7 studies, patients underwent an open Bankart repair. Twelve studies included both arthroscopic and open Bankart repair. Other surgical procedures and notes are described in Table 1. In one study, patients underwent an open Bankart repair and either a Neer's capsulorraphy or T-plasty or modified anteroinferior capsular shift procedure. Another study investigated patients undergoing arthroscopic Bankart and arthroscopic Bankart with remplissage. These patients were included in our analysis. Two studies included patients undergoing Bristow procedures and Bankart procedures, the patients undergoing Bristow procedures were excluded.
3.5. Risk of recurrent instability and revision
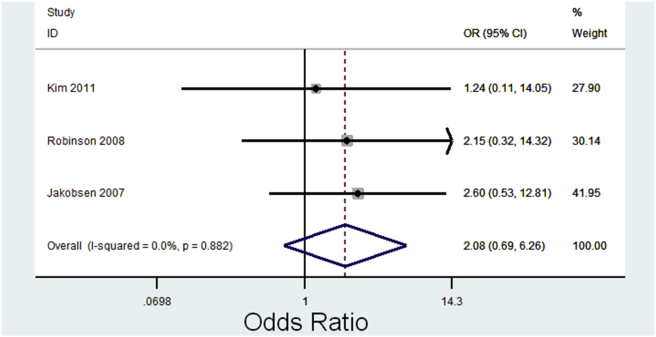
There were three papers in which both groups (S and R) were included, allowing a direct comparison between the groups. In each of these papers, the recurrence rate was lower in group S (S vs R: 2.4% vs 2.9%, 8.1% vs 21.1%, 7.1% vs 15.4%) (Table 2). Among these studies, there was a slightly elevated odds of recurrence among patients with multiple pre-operative instability episodes compared to those treated after a single episode (pooled OR 2.08, CI 0.69–6.26, p = 0.19) (Fig. 3). Heterogeneity among comparative studies was low (I-squared = 0.0%, p = 0.88).
Table 2.
Recurrence.
| Authors | Mean follow up months (range) | Patients with Single Pre-Procedure Instability (Group S) | Group S Post Procedure Instability | Group S Instability Rate (%) | Group S Revision Surgery | Patients with Multiple Pre-Procedure Instability (Group R) | Group R Post Procedure Instability | Group R Instability Rate (Percentage) | Group R Revision Surgery | Scope/Open | Notes |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Single Instability Episode Only | |||||||||||
| Arciero, R. A. et al.23 | 32 (15–45) | 21 | 3 | 14.3% | 1 | Scope | Transglenoid drilling | ||||
| Bottoni, C. R. et al. 200215 | 35 (17–56) | 9 | 1 | 11.1% | 1 | Scope | Bioabsorbable tack | ||||
| Kirkley A et al.13 | 79 (51–102) | 19 | 5 | 26.3% | 5 | Scope | Transglenoid drilling | ||||
| Larrain, M. V. et al.14 | 67.4 (28–120) | 28 | 1 | 3.6% | NR | Scope | Transglenoid, except 6 with anchors | ||||
| Shih W-Y. et al.44 | 18 | 39 | 2 | 5.1% | 2 | Scope | Metal anchors | ||||
| SUBTOTAL | 46 | 116 | 12 | 10.3% | 9 | ||||||
| Rate (Percentage) | 10.3% | NR | |||||||||
| Recurrent Instability Episodes Only | |||||||||||
| Archetti Netto N et al.22 | 61.3 | 42 | 2 | 4.8% | 2 | Scope/Open | Metal anchors | ||||
| Balg, F., and P. Boileau24 | 31.2 (24–52) | 131 | 19 | 14.5% | 6 | Scope | Absorbable anchor | ||||
| Bottoni, Cr et al. 200625 | 29 (24–48) | 61 | 3 | 4.9% | 2 | Scope/Open | Absorbable anchor | ||||
| Cole, B. J. et al.26 | 53.1 (27–72) | 59 | 8 | 13.6% | 3 | Scope/Open | Absorbable anchor | ||||
| Elmlund, A. O. et al.27 | 80.3 (64–96) | 36 | 5 | 13.9% | NR | Scope | Absorbable anchors | ||||
| Fabbriciani, C. et al.28 | 24 | 60 | 0 | 0.0% | 0 | Scope/Open | Metallic Anchors | ||||
| Hantes, M. E. et al.29 | 39.3 (25–66) | 63 | 2 | 3.2% | 0 | Scope | Absorbable anchors | ||||
| Jaeger, A. et al.30 | 19.6 (5–75) | 62 | 7 | 11.3% | NR | Open | Metallic Anchors | ||||
| Jorgensen, U. et al.31 | 36.2 (30–52) | 41 | 4 | 9.8% | 1 | Scope/Open | Anchors (Open)/Transglenoid (Scope) | ||||
| Karlsson J., L. et al.32 | 31.6 (24–63) | 108 | 14 | 13.0% | 3 | Scope/Open | Anchors (Scope: Suretak, Open:Mitek/TAG) | ||||
| Kartus J., L. et al.33 | 31 (18–46) | 36 | 1 | 2.8% | 2 | Scope/Open | Mix of Anchors, transglenoid | ||||
| Kim, S. H. et al.34 | 31 (27–45) | 62 | 0 | 0.0% | NR | Scope | Metallic Anchors | ||||
| Magnusson L. et al.35 | 25.5 (23–35) | 40 | 2 | 5.0% | 2 | Scope | Absorbable anchors | ||||
| Mahirogullari, M. et al. 200636 | 25 (24–39) | 34 | 1 | 2.9% | 1 | Open | Unspecified anchors | ||||
| Mahiroğulları M. et al. 201037 | 26.3 | 64 | 3 | 4.7% | 0 | Scope/Open | Mixed anchors | ||||
| Milano, G. et al.38 | 24 | 33 | 1 | 3.0% | NR | Scope | Metal anchors | ||||
| Mohtadi N et al.2 | 24 | 167 | 29 | 17.4% | 19 | Scope/Open | Mixed anchors | ||||
| Ng, D. Z., and V. P. Kumar39 | 32.4 (24–44) | 87 | 2 | 2.3% | 1 | Scope | Absorbable anchors | ||||
| Norlin, R40 | 24 | 20 | 2 | 10.0% | NR | Open | Mitek anchors | ||||
| Nourissat, G. et al.41 | 27.5 | 32 | 2 | 6.3% | 1 | Scope | Anchors, + Remplissage in half | ||||
| Potzl, W. et al.42 | 70.8 (66–90) | 14 | 3 | 21.4% | NR | Scope/Open | Anchors, Transglenoid | ||||
| Salomonsson, B. et al.43 | 120 | 32 | 19 | 59.4% | 4 | Open | Anchors | ||||
| Sperber A et al.45 | 24 | 56 | 10 | 17.9% | 2 | Scope/Open | Mixed anchors | ||||
| Steinbeck, J., and J. Jerosch46 | 38.1 (24–60) | 62 | 7 | 11.3% | 3 | Scope/Open | Mixed anchors | ||||
| Tamai, K. et al.47 | 37.5 (18–85) | 87 | 7 | 8.0% | 1 | Open | Mixed anchors | ||||
| Tan, C. K. et al.48 | 31.2 (18–60) | 124 | 11 | 8.9% | 4 | Scope | Mixed anchors | ||||
| Warme, W. J. et al.49 | 22 (17–45) | 38 | 3 | 7.9% | 1 | Open | Mixed anchors | ||||
| SUBTOTAL | 38.9 | 1651 | 167 | 58 | |||||||
| Rate (Percentage) | 10.1% | NR | |||||||||
| Both Groups Included | |||||||||||
| Kim, D. S. et al.19 | 45.1 (25–118) | 42 | 1 | 2.4% | NR | 68 | 2 | 2.9% | NR | Scope | Absorbable anchor |
| Jakobsen, B. W. et al.20 | 120 | 37 | 3 | 8.1% | 1 | 19 | 4 | 21.1% | NR | Open | Anchors |
| Robinson CM et al. 200821 | 24 | 42 | 3 | 7.1% | 3 | 13 | 2 | 15.4% | 2 | Scope | Absorbable anchor |
| SUBTOTAL | 63.0 | 121 | 7 | 4 | 100 | 8 | 2 | ||||
| Rate (percentage) | Single Episode [S] | 5.8% | NR | Recurrent [R] | 8.0% | NR | |||||
| Totals | 237 | 19 | NR | 1751 | 175 | NR | |||||
| Rate (Percentage) | Single Episode [S] | 8.0% | Recurrent [R] | 10.0% | |||||||
Fig. 3.
Forest plot of odds ratios of recurrent instability after Bankart repair among patients with multiple pre-operative instability episodes versus a single pre-operative instability episode. There was a trend toward increased odds of recurrent instability among patients with multiple pre-operative instability episodes (pooled OR 2.08 CI 0.69–6.26, p = 0.19). Between-study heterogeneity was low (I-squared = 0%, p = 0.88).
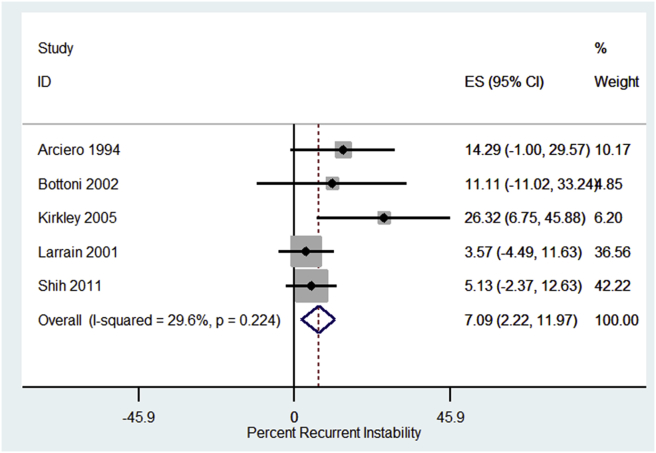
Among studies only of patients with one pre-operative instability episode (n = 5 studies), the pooled recurrence rate was 7.1% (CI 2.2%, 12.0%) and between-study heterogeneity was low (I-square = 29.6%, p = 0.22) (Fig. 4).
Fig. 4.
Forest plot of percent recurrent instability after Bankart repair among patients with a single pre-operative instability episode. The pooled recurrence rate was 7.1% (CI 2.2%, 12.0%) and between-study heterogeneity was low (I-square = 29.6%, p = 0.22).
Among studies only of patients with recurrent-instability (n = 27 studies), recurrence rates ranged from 0% to 59.4%. A pooled estimate could not be determined, as between-study heterogeneity was high, with or without correction for length of follow up (I-square = 77.2%, p < 0.001 without correction, I-square = 72.2%, p < 0.001 with correction).
Revision surgery was less reliably reported between the two groups. Qualitatively, there were no dramatic differences between the two groups. Further statistical analysis was not able to be completed given the incomplete data set (Table 2).
3.6. Non-instability related complications
Non-instability related complication rates among comparative studies ranged from 0%19,20 to 7.1%.21 There was inadequate reporting among included comparative studies to estimate risk of non-instability related complications by pre-operative instability status (single versus multiple instability episodes) (Table Appendix 1).2,13, 14, 15,19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49
Among non-comparative studies, non-instability related complication rates ranged from 0% to 14% with a pooled rate of 1% (CI 0.3%, 1.8%) (I-square = 0%, p = 0.80). The pooled infection rate was 0.6% (CI 0.0%, 1.0%) (I-square = 0%, p = 1.0), rate of nerve damage was 0.2% (CI 0.0%, 0.7%) (I-square = 0%, p = 1.0), and ‘other’ complications was 0.2% (CI 0.0%, 1.0%) (I-square = 0%, p = 1.0) which included adhesive capsulitis (3 reported cases), reflex sympathetic dystrophy (2 reported cases), and post-operative hematoma (1 reported case) (Table Appendix 1).
3.7. Postoperative range of motion and clinical outcome scores
The reviewed papers varied widely in reporting outcome scores. 19/35 studies reported numerical post-operative Rowe scores, the most common outcome measure reported. However, only one Group S paper reported this score. Constant scores, single assessment numerical evaluation (SANE), University of California Los Angeles (UCLA), Simple Shoulder Test (SST), Western Ontario Stability Index (WOSI), American Shoulder and Elbow Surgeons (ASES), Disabilities of the Arm, Shoulder and Hand (DASH), Oxford Instability Shoulder Score (OISS), Visual Analogue Scale (VAS) and San Francisco 12 (SF-12) were all reported to varying degrees. For completeness, available outcome measures can be found in the appendix (Table Appendix 2).
Range of motion was also variably reported. The most common measure reported was loss of external rotation in neutral post-operatively. 3 studies in the S group reported this, while 12 in the R. Average loss of external rotation in the S group was 4.47°, while it was 8.89 in the R group. These data are also included in the appendix (Table Appendix 3).
4. Discussion
Optimal management of primary anterior instability of the shoulder remains a controversial topic. Traditionally, nonoperative management has been the treatment of choice, as a subset of patients with isolated anterior instability will not have any further instability episodes. Operating on all first-time instability episodes would, therefore, induce operations on a number of patients who may have been asymptomatic without surgery.
In certain segments of the population, however, the risk of recurrent dislocation is at or above 80% (young, male, overhead/collision athletes).11,12,50,51 Furthermore, recurrent instability may increase the degree of labral injury, cartilage injury, and bone loss, eventually compromising the outcome of the stabilization procedure.5,38 This has pushed a subset of surgeons to discuss the outcomes of primary stabilization of the shoulder in young patients at high risk for recurrence.
The goal of this study was to assess the outcomes of surgical shoulder stabilization completed acutely, after a single instability episode, in comparison to those stabilized after recurrent instability. Our primary outcome measure was recurrence of instability (as measured by recurrent dislocations or subluxations). Secondary outcomes that were analyzed included revision surgery, complications, and functional outcome measures.
A previous systematic review approximately seven years ago looked at a similar question.52 The authors documented no substantial difference between groups with first time or recurrent instability episodes. Given increasing discussion about the failure rate of arthroscopic Bankart repair, and the increasing controversy regarding the role of acute fixation of shoulder instability, as well as the contribution of new studies to the literature, this updated systematic review provides new insight. Furthermore, the previous study included only arthroscopic stabilization. In the present study, both open and arthroscopic stabilization procedures were included.
Similar to the previous study, this study did not find a statistically significant difference between first time and recurrent instability surgery, however the current study demonstrates a small benefit for patients with primary stabilization. In spite of the wealth of literature on shoulder instability, there were only three papers that could provide a direct comparison between these two groups. In each group, there was a lower recurrence rate in patients who had stabilization after the first episode. While this was not a statistically defendable difference, it certainly deserves further investigation. Recent case series have demonstrated similar findings.52,53 Furthermore, the number of presurgical dislocations has been consistently demonstrated to be directly correlated with failure of surgical stabilization.54, 55, 56
Because of the heterogeneity of the literature, meaningful statistical analysis of the secondary outcome measures is challenging. Qualitatively, the risk of revision surgery is lower than the risk of recurrence. This indicates that some patients with recurrent instability after surgical management are able to be managed without revision surgery. Previous studies have demonstrated that some patients without revision surgical stabilization can become stable.57
Furthermore, the risk of complications, either in primary or recurrent dislocation, is very low. Only one study allowed meaningful comparison of intraoperative findings of patients in each of these groups. Kim et al. evaluated the rate and severity of concomitant shoulder injuries in patients after primary and recurrent instability.19 They demonstrated larger Hill-Sachs lesions in recurrent shoulder instability patients, but higher rates of SLAP tears in primary shoulder instability patients. They postulated that there may be some healing of SLAP tears with nonoperative management. The remainder of surgical findings between the two groups was similar or unable to be compared directly.
5. Conclusions
This systematic review failed to demonstrate a statistically significant difference in recurrence rates in patients with surgical stabilization after their primary instability episode compared to patients after multiple instability episodes, although a small benefit was shown. No conclusion could be made on the rate of complications, or functional outcomes with either approach or further shoulder injury with recurrent instability. Further high quality trials to evaluate the results of primary and delayed stabilization are necessary to help make better treatment decisions for this group of patients and to better inform patients of their risks, complications and expected outcomes post-operatively.
Disclaimer
The authors received no funding for this study and have no conflicts of interest to disclose.
Ethical committee review
This project did not require approval from the Ohio State University Biomedical Institutional Review Board.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jcot.2018.10.012.
Appendix A. Supplementary data
The following is the supplementary data to this article:
References
- 1.Neviaser R.J., Benke M.T., Neviaser A.S. Mid-term to long-term outcome of the open Bankart repair for recurrent traumatic anterior dislocation of the shoulder. J Shoulder Elbow Surg. 2017;3(17):30250–30251. doi: 10.1016/j.jse.2017.04.013. [DOI] [PubMed] [Google Scholar]
- 2.Mohtadi N.G., Chan D.S., Hollinshead R.M. A randomized clinical trial comparing open and arthroscopic stabilization for recurrent traumatic anterior shoulder instability: two-year follow-up with disease-specific quality-of-life outcomes. J Bone Joint Surg Am. 2014;96(5):353–360. doi: 10.2106/JBJS.L.01656. [DOI] [PubMed] [Google Scholar]
- 3.Carreira D.S., Mazzocca A.D., Oryhon J., Brown F.M., Hayden J.K., Romeo A.A. A prospective outcome evaluation of arthroscopic Bankart repairs: minimum 2-year follow-up. Am J Sports Med. 2006;34(5):771–777. doi: 10.1177/0363546505283259. [DOI] [PubMed] [Google Scholar]
- 4.Bak K., Wiesler E.R., Poehling G.G. Consensus statement on shoulder instability. Arthroscopy. 2010;26(2):249–255. doi: 10.1016/j.arthro.2009.06.022. [DOI] [PubMed] [Google Scholar]
- 5.Aboalata M., Plath J.E., Seppel G., Juretzko J., Vogt S., Imhoff A.B. Results of arthroscopic bankart repair for anterior-inferior shoulder instability at 13-year follow-up. Am J Sports Med. 2017;45(4):782–787. doi: 10.1177/0363546516675145. [DOI] [PubMed] [Google Scholar]
- 6.Dickens J.F., Rue J.P., Cameron K.L. Successful return to sport after arthroscopic shoulder stabilization versus nonoperative management in contact athletes with anterior shoulder instability:A prospective multicenter study. Am J Sports Med. 2017;45(22):2540–2546. doi: 10.1177/0363546517712505. [DOI] [PubMed] [Google Scholar]
- 7.Robins R.J., Daruwalla J.H., Gamradt S.C. Return to play after shoulder instability surgery in national collegiate athletic association division I intercollegiate football athletes. Am J Sports Med. 2017;45(10):2329–2335. doi: 10.1177/0363546517705635. [DOI] [PubMed] [Google Scholar]
- 8.Blonna D., Bellato E., Caranzano F., Assom M., Rossi R., Castoldi F. Arthroscopic bankart repair versus open Bristow-Latarjet for shoulder instability: a matched-pair multicenter study focused on return to sport. Am J Sports Med. 2016;44(12):3198–3205. doi: 10.1177/0363546516658037. [DOI] [PubMed] [Google Scholar]
- 9.Voos J.E., Livermore R.W., Feeley B.T. Prospective evaluation of arthroscopic bankart repairs for anterior instability. Am J Sports Med. 2010;38(2):302–307. doi: 10.1177/0363546509348049. [DOI] [PubMed] [Google Scholar]
- 10.Bishop J.A., Crall T.S., Kocher M.S. Operative versus nonoperative treatment after primary traumatic anterior glenohumeral dislocation: expected-value decision analysis. J Shoulder Elbow Surg. 2011;20(7):1087–1094. doi: 10.1016/j.jse.2011.01.031. [DOI] [PubMed] [Google Scholar]
- 11.Robinson C.M., Howes J., Murdoch H., Will E., Graham C. Functional outcome and risk of recurrent instability after primary traumatic anterior shoulder dislocation in young patients. J Bone Joint Surg Am. 2006;88(11):2326–2336. doi: 10.2106/JBJS.E.01327. [DOI] [PubMed] [Google Scholar]
- 12.Hovelius L., Olofsson A., Sandstrom B. Nonoperative treatment of primary anterior shoulder dislocation in patients forty years of age and younger. a prospective twenty-five-year follow-up. J Bone Joint Surg Am. 2008;90(5):945–952. doi: 10.2106/JBJS.G.00070. [DOI] [PubMed] [Google Scholar]
- 13.Kirkley A., Werstine R., Ratjek A., Griffin S. Prospective randomized clinical trial comparing the effectiveness of immediate arthroscopic stabilization versus immobilization and rehabilitation in first traumatic anterior dislocations of the shoulder: long-term evaluation. Arthroscopy. 2005;21(1):55–63. doi: 10.1016/j.arthro.2004.09.018. [DOI] [PubMed] [Google Scholar]
- 14.Larrain M.V., Botto G.J., Montenegro H.J., Mauas D.M. Arthroscopic repair of acute traumatic anterior shoulder dislocation in young athletes. Arthroscopy. 2001;17(4):373–377. doi: 10.1053/jars.2001.23226. [DOI] [PubMed] [Google Scholar]
- 15.Bottoni C.R., Wilckens J.H., DeBerardino T.M. A prospective, randomized evaluation of arthroscopic stabilization versus nonoperative treatment in patients with acute, traumatic, first-time shoulder dislocations. Am J Sports Med. 2002;30(4):576–580. doi: 10.1177/03635465020300041801. [DOI] [PubMed] [Google Scholar]
- 16.DerSimonian R., Laird N. Meta-analysis in clinical trials revisited. Contemp Clin Trials. 2015;45(Pt A):139–145. doi: 10.1016/j.cct.2015.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Higgins J.P., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Longo U.G., Rizzello G., Loppini M. Multidirectional instability of the shoulder: a systematic review. Arthroscopy. 2015;31(12):2431–2443. doi: 10.1016/j.arthro.2015.06.006. [DOI] [PubMed] [Google Scholar]
- 19.Kim D.S., Yi C.H., Yoon Y.S. Arthroscopic repair for combined Bankart and superior labral anterior posterior lesions: a comparative study between primary and recurrent anterior dislocation in the shoulder. Int Orthop. 2011;35(8):1187–1195. doi: 10.1007/s00264-011-1229-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jakobsen B.W., Johannsen H.V., Suder P., Sojbjerg J.O. Primary repair versus conservative treatment of first-time traumatic anterior dislocation of the shoulder: a randomized study with 10-year follow-up. Arthroscopy. 2007;23(2):118–123. doi: 10.1016/j.arthro.2006.11.004. [DOI] [PubMed] [Google Scholar]
- 21.Robinson C.M., Jenkins P.J., White T.O., Ker A., Will E. Primary arthroscopic stabilization for a first-time anterior dislocation of the shoulder. A randomized, double-blind trial. J Bone Joint Surg Am. 2008;90(4):708–721. doi: 10.2106/JBJS.G.00679. [DOI] [PubMed] [Google Scholar]
- 22.Archetti Netto N., Tamaoki M.J., Lenza M. Treatment of Bankart lesions in traumatic anterior instability of the shoulder: a randomized controlled trial comparing arthroscopy and open techniques. Arthroscopy. 2012;28(7):900–908. doi: 10.1016/j.arthro.2011.11.032. [DOI] [PubMed] [Google Scholar]
- 23.Arciero R.A., Wheeler J.H., Ryan J.B., McBride J.T. Arthroscopic Bankart repair versus nonoperative treatment for acute, initial anterior shoulder dislocations. Am J Sports Med. 1994;22(5):589–594. doi: 10.1177/036354659402200504. [DOI] [PubMed] [Google Scholar]
- 24.Balg F., Boileau P. The instability severity index score. A simple pre-operative score to select patients for arthroscopic or open shoulder stabilisation. J Bone Joint Surg Br. 2007;89(11):1470–1477. doi: 10.1302/0301-620X.89B11.18962. [DOI] [PubMed] [Google Scholar]
- 25.Bottoni C.R., Smith E.L., Berkowitz M.J., Towle R.B., Moore J.H. Arthroscopic versus open shoulder stabilization for recurrent anterior instability: a prospective randomized clinical trial. Am J Sports Med. 2006;34(11):1730–1737. doi: 10.1177/0363546506288239. [DOI] [PubMed] [Google Scholar]
- 26.Cole B.J., L'Insalata J., Irrgang J., Warner J.J. Comparison of arthroscopic and open anterior shoulder stabilization. A two to six-year follow-up study. J Bone Joint Surg Am. 2000;82-A(8):1108–1114. doi: 10.2106/00004623-200008000-00007. [DOI] [PubMed] [Google Scholar]
- 27.Elmlund A.O., Kartus J., Rostgard-Christensen L., Sernert N., Magnusson L., Ejerhed L. A 7-year prospective, randomized, clinical, and radiographic study after arthroscopic Bankart reconstruction using 2 different types of absorbable tack. Am J Sports Med. 2009;37(10):1930–1937. doi: 10.1177/0363546509335197. [DOI] [PubMed] [Google Scholar]
- 28.Fabbriciani C., Milano G., Demontis A., Fadda S., Ziranu F., Mulas P.D. Arthroscopic versus open treatment of Bankart lesion of the shoulder: a prospective randomized study. Arthroscopy. 2004;20(5):456–462. doi: 10.1016/j.arthro.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 29.Hantes M.E., Venouziou A.I., Liantsis A.K., Dailiana Z.H., Malizos K.N. Arthroscopic repair for chronic anterior shoulder instability: a comparative study between patients with Bankart lesions and patients with combined Bankart and superior labral anterior posterior lesions. Am J Sports Med. 2009;37(6):1093–1098. doi: 10.1177/0363546508331139. [DOI] [PubMed] [Google Scholar]
- 30.Jaeger A., Braune C., Welsch F., Sarikaya Y., Graichen H. Postoperative functional outcome and stability in recurrent traumatic anteroinferior glenohumeral instability: comparison of two different surgical capsular reconstruction techniques. Arch Orthop Trauma Surg. 2004;124(4):226–231. doi: 10.1007/s00402-003-0601-1. [DOI] [PubMed] [Google Scholar]
- 31.Jorgensen U., Svend-Hansen H., Bak K., Pedersen I. Recurrent post-traumatic anterior shoulder dislocation--open versus arthroscopic repair. Knee Surg Sports Traumatol Arthrosc. 1999;7(2):118–124. doi: 10.1007/s001670050133. [DOI] [PubMed] [Google Scholar]
- 32.Karlsson J., Magnusson L., Ejerhed L., Hultenheim I., Lundin O., Kartus J. Comparison of open and arthroscopic stabilization for recurrent shoulder dislocation in patients with a Bankart lesion. Am J Sports Med. 2001;29(5):538–542. doi: 10.1177/03635465010290050201. [DOI] [PubMed] [Google Scholar]
- 33.Kartus J., Ejerhed L., Funck E., Kohler K., Sernert N., Karlsson J. Arthroscopic and open shoulder stabilization using absorbable implants. A clinical and radiographic comparison of two methods. Knee Surg Sports Traumatol Arthrosc. 1998;6(3):181–188. doi: 10.1007/s001670050096. [DOI] [PubMed] [Google Scholar]
- 34.Kim S.H., Ha K.I., Jung M.W., Lim M.S., Kim Y.M., Park J.H. Accelerated rehabilitation after arthroscopic Bankart repair for selected cases: a prospective randomized clinical study. Arthroscopy. 2003;19(7):722–731. doi: 10.1016/s0749-8063(03)00397-9. [DOI] [PubMed] [Google Scholar]
- 35.Magnusson L., Ejerhed L., Rostgard-Christensen L. A prospective, randomized, clinical and radiographic study after arthroscopic Bankart reconstruction using 2 different types of absorbable tacks. Arthroscopy. 2006;22(2):143–151. doi: 10.1016/j.arthro.2005.12.016. [DOI] [PubMed] [Google Scholar]
- 36.Mahirogullari M., Kuskucu M., Solakoglu C. Comparison of outcomes of two different surgeries in regarding to complications for chronic anterior shoulder instability. Arch Orthop Trauma Surg. 2006;126(10):674–679. doi: 10.1007/s00402-006-0190-x. [DOI] [PubMed] [Google Scholar]
- 37.Mahirogullari M., Ozkan H., Akyuz M., Ugras A.A., Guney A., Kuskucu M. Comparison between the results of open and arthroscopic repair of isolated traumatic anterior instability of the shoulder. Acta Orthop Traumatol Turcica. 2010;44(3):180–185. doi: 10.3944/AOTT.2010.2289. [DOI] [PubMed] [Google Scholar]
- 38.Milano G., Grasso A., Russo A. Analysis of risk factors for glenoid bone defect in anterior shoulder instability. Am J Sports Med. 2011;39(9):1870–1876. doi: 10.1177/0363546511411699. [DOI] [PubMed] [Google Scholar]
- 39.Ng D.Z., Kumar V.P. Arthroscopic Bankart repair using knot-tying versus knotless suture anchors: is there a difference? Arthroscopy. 2014;30(4):422–427. doi: 10.1016/j.arthro.2014.01.005. [DOI] [PubMed] [Google Scholar]
- 40.Norlin R. Use of Mitek anchoring for Bankart repair: a comparative, randomized, prospective study with traditional bone sutures. J Shoulder Elbow Surg. 1994;3(6):381–385. doi: 10.1016/S1058-2746(09)80023-2. [DOI] [PubMed] [Google Scholar]
- 41.Nourissat G., Kilinc A.S., Werther J.R., Doursounian L. A prospective, comparative, radiological, and clinical study of the influence of the "remplissage" procedure on shoulder range of motion after stabilization by arthroscopic Bankart repair. Am J Sports Med. 2011;39(10):2147–2152. doi: 10.1177/0363546511416315. [DOI] [PubMed] [Google Scholar]
- 42.Potzl W., Thorwesten L., Gotze C., Garmann S., Steinbeck J. Proprioception of the shoulder joint after surgical repair for Instability: a long-term follow-up study. Am J Sports Med. 2004;32(2):425–430. doi: 10.1177/0363546503261719. [DOI] [PubMed] [Google Scholar]
- 43.Salomonsson B., Abbaszadegan H., Revay S., Lillkrona U. The Bankart repair versus the Putti-Platt procedure: a randomized study with WOSI score at 10-year follow-up in 62 patients. Acta Orthop. 2009;80(3):351–356. doi: 10.3109/17453670902988345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shih W.Y., Hung S.T., Shih J.T., Lee H.M., Ho Y.J. Comparison of arthroscopic treatment with conservative treatment for acute first-time traumatic anterior shoulder dislocation in a high-demand population. Formoson J Musculoskel Dis. 2011;2(1):16–19. [Google Scholar]
- 45.Sperber A., Hamberg P., Karlsson J., Sward L., Wredmark T. Comparison of an arthroscopic and an open procedure for posttraumatic instability of the shoulder: a prospective, randomized multicenter study. J Shoulder Elbow Surg. 2001;10(2):105–108. doi: 10.1067/mse.2001.112019. [DOI] [PubMed] [Google Scholar]
- 46.Steinbeck J., Jerosch J. Arthroscopic transglenoid stabilization versus open anchor suturing in traumatic anterior instability of the shoulder. Am J Sports Med. 1998;26(3):373–378. doi: 10.1177/03635465980260030501. [DOI] [PubMed] [Google Scholar]
- 47.Tamai K., Higashi A., Tanabe T., Hamada J. Recurrences after the open Bankart repair: a potential risk with use of suture anchors. J Shoulder Elbow Surg. 1999;8(1):37–41. doi: 10.1016/s1058-2746(99)90052-6. [DOI] [PubMed] [Google Scholar]
- 48.Tan C.K., Guisasola I., Machani B. Arthroscopic stabilization of the shoulder: a prospective randomized study of absorbable versus nonabsorbable suture anchors. Arthroscopy. 2006;22(7):716–720. doi: 10.1016/j.arthro.2006.03.017. [DOI] [PubMed] [Google Scholar]
- 49.Warme W.J., Arciero R.A., Savoie F.H., 3rd, Uhorchak J.M., Walton M. Nonabsorbable versus absorbable suture anchors for open Bankart repair. A prospective, randomized comparison. Am J Sports Med. 1999;27(6):742–746. doi: 10.1177/03635465990270061001. [DOI] [PubMed] [Google Scholar]
- 50.Hovelius L. Anterior dislocation of the shoulder in teen-agers and young adults. Five-year prognosis. J Bone Joint Surg Am. 1987;69(3):393–399. [PubMed] [Google Scholar]
- 51.Wasserstein D.N., Sheth U., Colbenson K. The true recurrence rate and factors predicting recurrent instability after nonsurgical management of traumatic primary anterior shoulder dislocation: a systematic review. Arthroscopy. 2016;32(12):2616–2625. doi: 10.1016/j.arthro.2016.05.039. [DOI] [PubMed] [Google Scholar]
- 52.Grumet R.C., Bach B.R., Jr., Provencher M.T. Arthroscopic stabilization for first-time versus recurrent shoulder instability. Arthroscopy. 2010;26(2):239–248. doi: 10.1016/j.arthro.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 53.Gasparini G., De Benedetto M., Cundari A. Predictors of functional outcomes and recurrent shoulder instability after arthroscopic anterior stabilization. Knee Surg Sports Traumatol Arthrosc. 2016;24(2):406–413. doi: 10.1007/s00167-015-3785-3. [DOI] [PubMed] [Google Scholar]
- 54.Ozturk B.Y., Maak T.G., Fabricant P. Return to sports after arthroscopic anterior stabilization in patients aged younger than 25 years. Arthroscopy. 2013;29(12):1922–1931. doi: 10.1016/j.arthro.2013.09.008. [DOI] [PubMed] [Google Scholar]
- 55.Randelli P., Ragone V., Carminati S., Cabitza P. Risk factors for recurrence after Bankart repair a systematic review. Knee Surg Sports Traumatol Arthrosc. 2012;20(11):2129–2138. doi: 10.1007/s00167-012-2140-1. [DOI] [PubMed] [Google Scholar]
- 56.Porcellini G., Campi F., Pegreffi F., Castagna A., Paladini P. Predisposing factors for recurrent shoulder dislocation after arthroscopic treatment. J Bone Joint Surg Am. 2009;91(11):2537–2542. doi: 10.2106/JBJS.H.01126. [DOI] [PubMed] [Google Scholar]
- 57.Shah A.S., Karadsheh M.S., Sekiya J.K. Failure of operative treatment for glenohumeral instability: etiology and management. Arthroscopy. 2011;27(5):681–694. doi: 10.1016/j.arthro.2010.11.057. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.