Abstract
Introduction:
Patients undergoing the Norwood operation consume considerable healthcare resources; however, detailed information regarding factors impacting hospitalisation costs is lacking. We evaluated the association of postoperative complications with hospital costs.
Methods:
In the present study, we utilised a unique data set consisting of prospectively collected clinical data from the Pediatric Heart Network Single Ventricle Reconstruction trial linked at the patient level with cost data for 10 hospitals participating in the Children’s Hospital Association Case Mix database during the trial period. The relationship between complications and cost was modelled using linear regression, accounting for the skewed distribution of cost, adjusting for within-centre clustering and baseline patient characteristics.
Results:
A total of 334 eligible Norwood records (97.5%) were matched between data sets. Overall, 82% suffered from at least one complication (median 2; with a range from 0 to 33). Those with complications had longer postoperative length of stay (25 versus 12 days, p < 0.001), more total ventilator days (7 versus 5 days, p < 0.001), and higher in-hospital mortality (17.6 versus 3.4%, p < 0.006). Mean adjusted hospital cost in those with a complication was $190,689 (95% CI $111,344–$326,577) versus $120,584 (95% CI $69,246–$209,983) in those without complications (p = 0.002). Costs increased with the number of complications (1–2 complications = $132,800 versus 3–4 complications = $182,353 versus ⩾5 complications = $309,372 [p < 0.001]).
Conclusions:
This merged data set of clinical trial and cost data demonstrated that postoperative complications are common following the Norwood operation and are associated with worse clinical outcomes and higher costs. Efforts to reduce complications in this population may lead to improved outcomes and cost savings.
Keywords: Norwood operation, complications, resource utilisation, hypoplastic left heart syndrome
Survival following the Norwood operation for hypoplastic left heart syndrome and related single right ventricle anomalies has improved considerably over the past several decades with advances in surgical techniques and perioperative care;1,2 however, many of these infants experience a complicated postoperative course and prolonged length of hospital stay, accounting for significant resource utilisation.3 In fact, a recent analysis found the diagnosis of hypoplastic left heart syndrome to be associated with the highest hospital charges of any birth defect.4
The current healthcare environment places emphasis on both improving outcomes and reducing the cost of care.5 Although it is known that patients undergoing the Norwood operation account for significant resource utilisation, the specific factors accounting for high costs of care remain unclear.6 Postoperative complications have been demonstrated to influence hospital costs across a variety of surgical populations including children undergoing congenital heart surgery;7,8 however, detailed information regarding the impact of complications, independent of other baseline co-morbidities, in patients undergoing the Norwood operation is lacking. Previous studies, particularly those involving administrative data sets, have lacked granular data regarding the occurrence of specific complications in this patient population.3,9–11
The purpose of this study was to investigate the relationship between postoperative complications and hospital costs following the Norwood operation. This was achieved using a novel technique of linking prospectively collected clinical outcomes and complications data from the Pediatric Heart Network Single Ventricle Reconstruction trial with cost data from the Children’s Hospital Association Case Mix database.
Methods
Data sources
The Pediatric Heart Network, funded by the National Heart, Lung, and Blood Institute, recently conducted the Single Ventricle Reconstruction trial. Details of the trial design (ClinicalTrials.gov number NCT00115934) have been published previously.12 In brief, 555 infants undergoing the Norwood procedure for hypoplastic left heart syndrome or related single, morphological right ventricle anomalies from 2005 to 2008 were randomised to receive either a modified Blalock—Taussig shunt or a right ventricle-to-pulmonary artery shunt for provision of pulmonary blood flow. Randomisation occurred at 15 medium- and high-volume congenital heart surgery centres in North America.
The Children’s Hospital Association Case Mix database is an administrative data set containing resource utilisation data from 90 United States children’s hospitals. De-identified data are submitted by participating hospitals. Data quality is ensured through a joint effort between the Children’s Hospital Association and participating hospitals. This study was evaluated by the Medical University of South Carolina Institutional Review Board and did not meet qualifications for human subjects research.
Linkage
Prospectively collected clinical outcomes and complications data from the Single Ventricle Reconstruction trial were merged at the patient level with cost data from the Case Mix database for hospitals included in both data sets during the study period. A previously validated method13 of probabilistic matching of the following indirect identifiers was used to link records: centre, gender, date of admission (±1 day), date of discharge (±1 day), and date of birth (±1 day).
Study population
Any patient enrolled in the Single Ventricle Reconstruction trial undergoing the Norwood operation was eligible for inclusion. Patients undergoing Stage II palliation or heart transplantation during the same hospital admission were excluded from the analysis, as this study focussed on the post-Norwood hospitalisation.
Data collection
Detailed information regarding preoperative patient characteristics, surgical management, and postoperative course and outcomes following the Norwood operation, as previously described, were obtained from the Single Ventricle Reconstruction trial data.12 As described by Virzi et al14 complications in the Single Ventricle Reconstruction trial were assessed via a novel adverse event reporting strategy defined by the Pediatric Heart Network. The five Sentinel Serious Adverse Events in the Single Ventricle Reconstruction trial are listed in Supplementary table 1 and included the following: acute shunt failure requiring intervention, cardiac arrest requiring cardiopulmonary resuscitation and medications, cardiopulmonary insufficiency requiring extracorporeal membrane oxygenation, unplanned cardiovascular re-operation, and necrotising enterocolitis requiring laparotomy. Other complications recorded in the Single Ventricle Reconstruction trial as noted in Supplementary table 1 were also included in our analysis of complications for the purposes of this study; these included cardiac, vascular, respiratory, neurological, gastrointestinal, infectious, renal, and haematological complications.
Total hospital charges and payor type were obtained from the Case Mix database. Charges were converted to estimated costs using hospital-specific cost-to-charge ratios, adjusted for geographic region using the Centers for Medicare and Medicaid Services price wage index for the hospital’s location, and inflated to 2008 dollars using the medical component of the consumer price index.
Analysis
Study variables and complications were described using standard summary statistics. Continuous variables were summarised as median and interquartile range and categorical variables were depicted as frequencies and percentages. The distribution of complications across the study population was described, as well as outcomes in those with versus without a complication. The specific types of complications associated with increased hospital costs were also examined. For this portion of the analysis, patients were grouped into tertiles according to total cost (<$80,000, $80,000–$200,000, and >$200,000), and the frequency of complications across these cost tertiles was described.
The relationship between complications and cost, adjusting for baseline patient characteristics, was further evaluated using generalised linear mixed effects models. Cost was log transformed due to the skewed distribution, and a random intercept for each hospital was utilised to account for within-centre clustering. The model was adjusted for patient baseline characteristics found to be associated with cost (p < 0.1) in bivariate analyses, including preoperative intubation, pre-Norwood pulmonary artery banding, pre-Norwood atrial septectomy, presence of aberrant right subclavian artery, number of pre-Norwood surgeries, number of pre-Norwood complications, payor type, use of regional cerebral perfusion, cardiopulmonary bypass time, deep hypothermic circulatory arrest time, use of ultrafiltration, and presence of an open sternum. Both costs associated with any versus no complications as well as costs associated with the number of complications were modelled. Estimates were back-transformed to the original cost scale for ease of interpretability. All the analyses were performed using SAS version 9.3 (SAS Institute Incorporated, Cary, North Carolina, United States of America). A p-value <0.05 was considered to be statistically significant.
Results
Study population
A total of 10 out of 15 centres participating in the Single Ventricle Reconstruction trial submitted data to the Case Mix Database during the trial period. From these 10 centres, 344 of 353 patients were matched between databases, resulting in a 97.5% linkage rate.
Patient characteristics
Study population characteristics are displayed in Table 1. Overall, 78% of the patients had a prenatal diagnosis, and 62% of the patients were male. The median gestational age was 38 weeks, and the median birth weight was 3100 g. In the cohort, 95% carried an anatomical diagnosis of hypoplastic left heart syndrome, 65% with aortic atresia, and 4% had obstructed pulmonary venous return. Operative characteristics included randomisation to a right ventricle-to-pulmonary artery shunt in 51%, use of regional cerebral perfusion in 40%, and open sternum in 67% of the cases.
Table 1.
Study population characteristics.
| Total (n = 314) | |
|---|---|
| Preoperative | |
| Prenatal diagnosis | 245 (78%) |
| Male gender | 194 (62%) |
| Median gestational age at birth [IQR] | 38 [37–39] |
| Median birth weight in grams [IQR] | 3100 [2731–3410] |
| Anatomical diagnosis of HLHS (versus other single RV anomaly) | 298 (95%) |
| Aortic atresia | 205 (65%) |
| Obstructed pulmonary venous return | 11 (4%) |
| Payor group | |
| Government | 127 (40%) |
| Private | 128 (41%) |
| Other | 59(19%) |
| Preoperative intubation | 138 (44%) |
| Operative | |
| Randomised RV–PA shunt | 161 (51%) |
| Regional cerebral perfusion | 125 (40%) |
| Open sternum | 208 (67%) |
| Total cardiopulmonary bypass time in minutes [IQR] | 133 [91–163] |
| Deep hypothermic circulatory arrest time in minutes [IQR] | 36 [8–50] |
HLHS = hypoplastic left heart syndrome; IQR = interquartile range; PA = pulmonary artery; RV = right ventricle
Postoperative complications
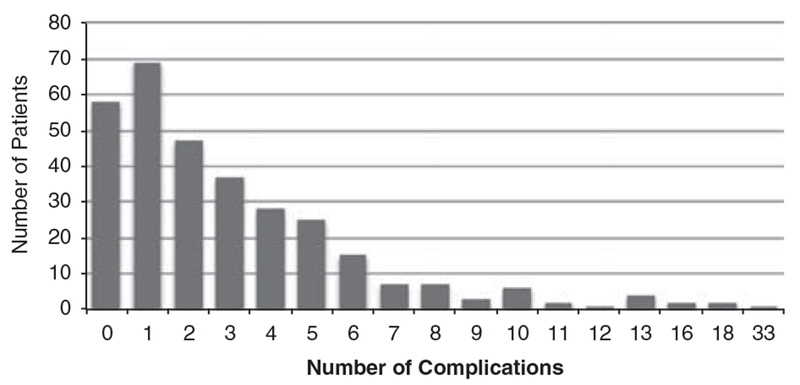
There were a total of 1066 postoperative complications identified. Figure 1 illustrates the distribution of complications per patient. Overall, 82% of the patients suffered at least one complication and 28% experienced four or more complications. The median number of complications per patient was 2, with a range from 0 to 33.
Figure 1.
Distribution of the number of post-Norwood complications. The Y-axis shows the number of patients, and the X-axis shows the number of complications.
In order to describe the specific types of complications associated with increased hospital costs, patients were grouped into tertiles according to total cost (<$80,000, $80,000–$200,000, and >$200,000). The most common complications occurring in those classified within the high-cost tertile included cardiopulmonary resuscitation (37%), chronic respiratory failure (37%), sepsis (33%), arrhythmia (32%), and need for extracorporeal membrane oxygenation (24%).
Unadjusted associations of postoperative complications with clinical outcomes are displayed in Table 2. Patients with complications had a longer postoperative length of stay (25 versus 12 days, p < 0.001), more total post-Norwood ventilator days (7 versus 5 days, p < 0.001), and higher in-hospital mortality (17.6 versus 3.4%, p = 0.006) compared with those patients with no complications.
Table 2.
The association of postoperative complications with clinical outcomes.
| No complication (n = 58) | ⩾1 Complication (n = 256) | p-value | |
|---|---|---|---|
| Median postoperative length of stay in days [IQR] | 17 [12–23] | 28.5 [19–44.5] | < 0.001 |
| Median postoperative ventilator days [IQR] | 5 [3–6] | 7 [4–12] | <0.001 |
| Survival to hospital discharge | 57 (98.3%) | 211 (82.4%) | 0.006 |
IQR = interquartile range
Costs associated with postoperative complications in adjusted analysis
Figure 2 displays the impact of complications on total hospital costs, adjusting for important baseline patient characteristics associated with cost in this cohort. Adjusted mean hospital costs in those with a complication were $190,689 (95% CI $111,344–$326,577) versus $120,584 (95% CI $69,246–$209,983) in those without complications (p = 0.002). Of note, those who died before hospital discharge were also significantly more likely to have higher costs (p < 0.0001).
Figure 2.
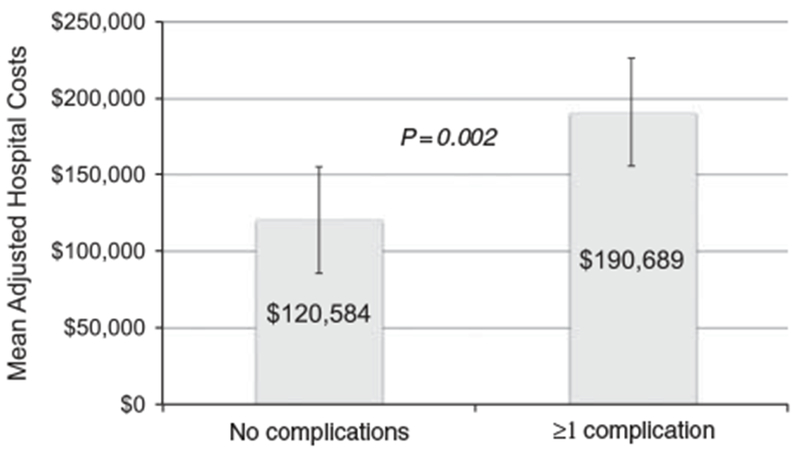
Association of complications and mean adjusted hospital costs following the Norwood operation. Hospital costs were adjusted for significant baseline patient characteristics. The X-axis separates patients into those with no complications versus those with at least one postoperative complication. The mean adjusted hospital costs are displayed on the Y-axis.
Figure 3 depicts the relationship between adjusted hospital costs and the number of postoperative complications after the Norwood procedure. Adjusted mean hospital costs increased with the total number of complications, although costs were not significantly higher until at least three complications had occurred. The mean hospital cost for patients with five or more postoperative complications was $309,372.
Figure 3.
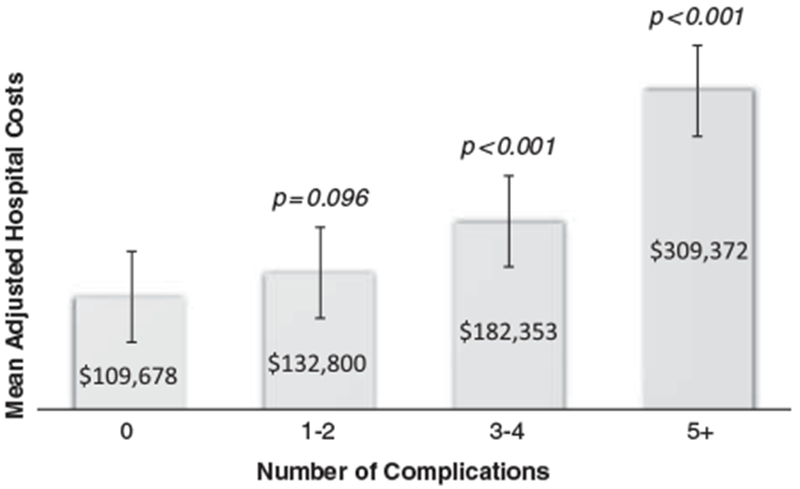
Mean adjusted hospital costs increase with complications rates following the Norwood operation. Total hospital costs were adjusted for baseline patient characteristics. Patients were grouped by the number of post-Norwood complications on the X-axis, and the mean adjusted hospital costs are displayed on the Y-axis.
Discussion
This multicentre analysis, leveraging a unique merged data set of prospectively collected clinical trial data and cost information from an administrative data set, describes the relationship between postoperative complications and hospital costs following the Norwood operation. We found that postoperative complications are common following the Norwood operation and associated with worse clinical outcomes and higher costs. These data suggest that efforts to reduce complications in this population may lead to both improved outcomes and cost savings.
This study utilised a unique data set of merged clinical trial and administrative data, successfully linking 97.5% of eligible records. This approach takes advantage of the strengths of both types of data sets – the prospectively collected detailed clinical information contained in the trial data set and the cost information in the administrative data set – and allows analyses not otherwise possible with the individual data sets alone. In paediatrics, the Children’s Oncology Group has previously demonstrated success with this technique by merging Children’s Oncology Group clinical trial data sets with the Pediatric Health Information System Database. The merged data set was utilised to examine toxicity monitoring and describe resource utilisation associated with chemotherapy and the treatment of paediatric cancer.15–17
In the paediatric cardiac disease population, these methods have also been utilised to link clinical registry data (from the Society of Thoracic Surgeons Congenital Heart Surgery Database) with administrative data (from the Pediatric Health Information System Database) to perform various analyses including several comparative effectiveness studies and analyses of the relationship between quality and costs of care;7,13,18 however, this study is the first to demonstrate that patients in a congenital heart surgery trial can be successfully linked to an administrative data set to describe resource utilisation along with clinical outcomes. This methodology is important as it allows investigators to leverage and utilise existing data sources to both answer important questions and to do this in an efficient manner. This is particularly important in the present era of declining research funding, and similar concepts have also been expanded to support merging and analysis of other types of data sets, as well as the use of existing registry data to support clinical trials.19 In a recent editorial, Lauer and D’Agostino20 proposed that this type of “randomised registry trial” design used in studies such as the Thrombus Aspiration in ST-Elevation Myocardial Infarction trial 9 may offer a method to resolve the current cost and time limitations in modern clinical trial designs.
Previous studies have demonstrated that patients with hypoplastic left heart syndrome and related single right ventricle anomalies account for the highest tier of resource utilisation across all birth defects and among those with CHD.4,18,21 Using merged data from the Society of Thoracic Surgeons and Pediatric Health Information Databases, Pasquali et al18 reported on hospital costs for patients undergoing nine common benchmark congenital heart surgeries at 27 US children’s hospitals from 2006 to 2010, and patients undergoing the Norwood operation accounted for the highest total hospital costs (median $165,168). In addition, in an analysis of 1941 patients at 48 centers using the University HealthSystem Consortium data set, Dean et al3 demonstrated that median hospital costs for this patient population appeared to be increasing over the time period of 1998–2007 (from $65,041 to $113,827) in parallel with increases in survival and hospital length of stay.
Our study adds to the growing body of literature across children and adults undergoing a variety of surgical procedures examining factors associated with increased hospital costs. We found that postoperative complications are common following the Norwood operation, with 82% of patients experiencing at least one of the complications captured in the Single Ventricle Reconstruction trial data set and more than a quarter experiencing four or more complications. Similar to studies in other patient populations,22,23 we found that complications were associated with worse clinical outcomes including prolonged length of stay. Interestingly, there was no statistically significant increase in cost until at least three complications were present.
The results of our study also support a previous investigation utilising merged Society of Thoracic Surgeons and Pediatric Health Information System data, which reported that post-Norwood complications were associated with ~ $119,303 as excess costs per surgical case, with major postoperative complications estimated to result in $210,865 as excess costs.7
In the current healthcare environment, there is a focus on both optimising clinical outcomes and minimising costs of care.5 The results of our study and other recent analyses suggest that efforts geared towards reducing postoperative complications may hold the potential to achieve both these objectives; however, further studies are necessary to elucidate care practices that may be associated with fewer complications. A previous Single Ventricle Reconstruction trial analysis22 identified considerable variation in perioperative management across centres for patients undergoing the Norwood operation. In addition, it has also been shown that both complication rates and costs are variable across centres;18 however, detailed information regarding the relationships between specific centre-level practices, complication rates, and costs have not been described. Such analyses could contribute to multicentre collaborative quality improvement in this area.
Limitations
This analysis was limited to patient data from medium- and high-volume centres participating in both the Pediatric Heart Network Single Ventricle Reconstruction trial and the Children’s Hospital Association Case Mix database during the study period. Therefore, these results may not be generalisable to all patients undergoing the Norwood operation. Further, we focussed on evaluating postoperative complications; however, complications and hospital length of stay are often intertwined, and the independent impact on cost is difficult to ascertain. In addition, it is not possible within our data set to assess which complications may be “preventable”, and, although the trial data set captured an extensive list of complications, not every possible complication was likely captured or was able to be evaluated in this study. Hospital costs in the overall population with single ventricle defects may have been underestimated as patients receiving Stage II palliation or a heart transplantation during the same hospitalisation were excluded for the purposes of this study. Finally, this analysis only examined inpatient costs during the Norwood hospitalisation, and further studies evaluating costs across multiple hospitalisations, staged surgeries, and outpatient care for hypoplastic left heart syndrome will be necessary to determine longitudinal costs for this population.
Conclusions
This study demonstrates the feasibility of linkages between clinical trial data and administrative data in the field of congenital heart surgery, allowing efficient analysis of both clinical outcomes and costs of care. The results of our analysis demonstrate that postoperative complications are common following the Norwood operation and are associated with worse clinical outcomes and higher costs. This suggests that initiatives to reduce postoperative complications in this population may lead to both improved clinical outcomes and cost savings. Further investigation is necessary to determine whether there are specific complications that drive the known cost variation across centres performing the Norwood operation, and to better understand specific practices that may be associated with fewer complications. These data could inform collaborative efforts to improve outcomes and reduce costs across hospitals in this patient population.
Supplementary Material
Acknowledgement:
Financial Support
The present study was conducted under a Scholar Award from the Pediatric Heart Network supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health under Award Number U10HL068270. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflicts of Interest:
None.
Ethical Standards
The authors assert that all procedures contributing to this retrospective study comply with ethical standards. These data were not considered human subjects research by the Medical University of South Carolina Institutional Review Board.
Supplementary material
For supplementary material referred to in this article, please visit http://dx.doi./org/10.1017/S1047951115002498
References
- 1.McHugh KE, Hillman DG, Gurka MJ, Gutgesell HP. Three-stage palliation of hypoplastic left heart syndrome in the University HealthSystem Consortium. Congenit Heart Dis 2010; 5: 8–15. [DOI] [PubMed] [Google Scholar]
- 2.Graham EM, Bradley SM, Atz AM. Preoperative management of hypoplastic left heart syndrome. Expert Opin Pharmacother 2005; 6: 687–693. [DOI] [PubMed] [Google Scholar]
- 3.Dean PN, Hillman DG, McHugh KE, Gutgesell HP. Inpatient costs and charges for surgical treatment of hypoplastic left heart syndrome. Pediatrics 2011; 128: e1181–e1186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease C, Prevention. Hospital stays, hospital charges, and in-hospital deaths among infants with selected birth defects – United States, 2003. Morbidity and Mortality Weekly Report 2007; 56: 25–29. [PubMed] [Google Scholar]
- 5.Porter ME. What is value in health care? N Engl J Med 2010; 363: 2477–2481. [DOI] [PubMed] [Google Scholar]
- 6.Jantzen DW, He X, Jacobs JP, et al. The impact of differential case ascertainment in clinical registry versus administrative data on assessment of resource utilization in pediatric heart surgery. World J Pediatr Congenit Heart Surg 2014; 5: 398–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pasquali SK, He X, Jacobs ML, et al. Excess costs associated with complications and prolonged length of stay after congenital heart surgery. Ann Thorac Surg 2014; 98: 1660–1666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Benavidez OJ, Connor JA, Gauvreau K, Jenkins KJ. The contribution of complications to high resource utilization during congenital heart surgery admissions. Congenit Heart Dis 2007; 2: 319–326. [DOI] [PubMed] [Google Scholar]
- 9.Pasquali SK, Peterson ED, Jacobs JP, et al. Differential case ascertainment in clinical registry versus administrative data and impact on outcomes assessment for pediatric cardiac operations. Ann Thorac Surg 2013; 95: 197–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gutgesell HP, Hillman DG, McHugh KE, Dean P, Matherne GP. Use of an administrative database to determine clinical management and outcomes in congenital heart disease. World J Pediatr Congenit Heart Surg 2011; 2: 593–596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pasquali SK, Sun JL, d’Almada P, et al. Center variation in hospital costs for patients undergoing congenital heart surgery. Circulation 2011; 4: 306–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ohye RG, Gaynor JW, Ghanayem NS, et al. Design and rationale of a randomized trial comparing the Blalock-Taussig and right ventricle-pulmonary artery shunts in the Norwood procedure. J Thorac Cardiovasc Surg 2008; 136: 968–975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pasquali SK, Jacobs JP, Shook GJ, et al. Linking clinical registry data with administrative data using indirect identifiers: implementation and validation in the congenital heart surgery population. Am Heart J 2010; 160: 1099–1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Virzi L, Pemberton V, Ohye RG, et al. Reporting adverse events in a surgical trial for complex congenital heart disease: the Pediatric Heart Network experience. J Thorac Cardiovasc Surg 2011; 142: 531–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aplenc R, Fisher BT, Huang YS, et al. Merging of the National Cancer Institute-funded cooperative oncology group data with an administrative data source to develop a more effective platform for clinical trial analysis and comparative effectiveness research: a report from the Children’s Oncology Group. Pharmacoepidemiol Drug Saf 2012; 21 (Suppl 2): 37–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Getz KD, Li Y, Alonzo TA, et al. Comparison of in-patient costs for children treated on the AAML0531 clinical trial: a report from the Children’s Oncology Group. Pediatr Blood Cancer 2015; 62: 1775–1781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Miller TP, Troxel AB, Li Y, et al. Comparison of administrative/ billing data to expected protocol-mandated chemotherapy exposure in children with acute myeloid leukemia: a report from the Children’s Oncology Group. Pediatr Blood Cancer 2015; 62: 1184–1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pasquali SK, Jacobs ML, He X, et al. Variation in congenital heart surgery costs across hospitals. Pediatrics 2014; 133: e553–e560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Frobert O, Lagerqvist B, Olivecrona GK, et al. Thrombus aspiration during ST-segment elevation myocardial infarction. N Engl J Med 2013; 369: 1587–1597. [DOI] [PubMed] [Google Scholar]
- 20.Lauer MS, D’Agostino RB Sr. The randomized registry trial – the next disruptive technology in clinical research? N Engl J Med 2013; 369: 1579–1581. [DOI] [PubMed] [Google Scholar]
- 21.Kogon BE, Kanter K, Alsoufi B, Maher K, Oster ME. Outcomes and hospital costs associated with the Norwood operation: beyond morbidity and mortality. Cardiol Young 2015; 25: 853–859. [DOI] [PubMed] [Google Scholar]
- 22.Pasquali SK, Ohye RG, Lu M, et al. Variation in perioperative care across centers for infants undergoing the Norwood procedure. J Thorac Cardiovasc Surg 2012; 144: 915–921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dimick JB, Chen SL, Taheri PA, Henderson WG, Khuri SF, Campbell DA Jr. Hospital costs associated with surgical complications: a report from the private-sector National Surgical Quality Improvement Program. Journal of the American College of Surgeons 2004; 199: 531–537. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.