Abstract
Objective
To investigate the potential of timing and displacement measures from fluoroscopic swallow studies for predicting aspiration in dysphagic patients.
Methods
Timing and displacement variables for a 20‐ml liquid bolus were extracted from fluoroscopic swallow studies of 5923 patients reflecting a variety of dysphagia etiologies. Patients were divided into aspirators and non‐aspirators, and variables were compared between groups, and to a group of 148 normal control subjects. The relationship of each variable to aspiration was determined. Odds ratios for aspiration were calculated for measures deviating more than two standard deviations from normal. Associations of variables with time of aspiration relative to airway closure were also examined.
Results
Regression analyses revealed that the pharyngeal constriction ratio (PCR) was the measure most predictive of aspiration (74.6%), with percentage of accuracy improving to 76.5% when all measures were considered. Odds Ratios ranging from two times to more than five times were identified for variables deviating more than two standard deviations from normal. Aspiration relative to maximum airway closure, ie, before, during, and after, was also investigated. In the current study, 53% of aspiration events occurred after maximum airway closure, on residue that remained after swallow. Some mechanical impairments appeared specific to timing of aspiration and provide further evidence of the utility of mechanical analysis.
Conclusions
Results of the review provide substantial support for the value of quantitative assessment of swallow mechanics, and for the role of such data in predicting aspiration risk in dysphagic patients.
Level of Evidence
3b (retrospective, individual case‐control)
Keywords: Fluoroscopy, quantitative measures, predicting aspiration
INTRODUCTION
Since Logemann's first descriptions of the modified barium swallow study,1 fluoroscopy has become a standard tool in the assessment of patients with oral‐pharyngeal dysphagia. Precisely how and to what extent fluoroscopy is used, however, varies from center to center. Minimally, clinicians use the tool to rule out aspiration during swallow. Others may use the instrument to assess strategies designed to increase both the safety and effectiveness of swallow when these functions are in jeopardy, or to consider the potential for advancing a patient's diet. At some sites, studies are not recorded, limiting observations to what the clinician perceives, in real time, during filming. At others, studies are recorded and carefully reviewed in slow motion, even frame by frame. At our own institution, fluoroscopy studies are recorded and carefully reviewed, and both subjective impressions and objective measures of timing and displacement are noted and documented, respectively.2 Increasingly, we have found that the objective data collected inform and enhance our assessments of individual patients.
The power of fluoroscopy notwithstanding, it is also the case that the tool must be used with careful acknowledgment of its invasive nature. The average fluoroscopic swallow study typically involves three‐four minutes of radiation, a relatively brief sample. If a patient is observed to aspirate, then a clear risk has been identified. If no aspiration is observed, however, questions may remain about a patient's ability to swallow safely. Patients who typically aspirate may not do so during the study. Aspiration events related to residue can occur seconds after a swallow and may be missed if the fluoroscopy unit has been turned off. In other cases, clinicians may avoid giving a patient a bolus they suspect will elicit aspiration in order to preclude this adverse event. Such conservatism is especially likely with patients who are fragile, or whose conditions are precarious.
In short, if other information available in the study allows us to anticipate aspiration, even when not observed, the value of fluoroscopy is enhanced. Previous research has demonstrated clear associations between impaired swallow mechanics, eg, hyoid and laryngeal movements,3, 4, 5, 6 pharyngeal constriction,7 bolus transit timing,8, 9 durations and timing of critical events,10, 11 and aspiration. In general, these studies have focused on particular patient groups, often with relatively small numbers of subjects (see Steele and Cichero3 for a systematic review of related research). The intent of the current paper is to describe the unique predictive potential of selected quantitative variables in a large number of dysphagic patients demonstrating a broad range of etiologies. Differences in measures between patients who did and did not aspirate, compared to each other, and to normal, and in aspirators relative to time of aspiration, ie, before, during, or after maximum airway closure, were investigated.
MATERIALS AND METHODS
Subjects
Permission to conduct this study was obtained from the institutional review board at the University of California, Davis. The records of all patients presenting to the ENT Voice and Swallowing Center with the chief complaint of dysphagia between January 1, 1997 and December 31, 2013 were retrospectively reviewed. Patients under the age of 18 years were excluded from consideration.
Data from patients were compared to studies of 148 normal, non‐dysphagic volunteers who underwent the same fluoroscopic protocol. Normal subjects included 74 who were under the age of 65 years, and 74 who were older than 65 years. Seventy‐four of this group were male and 74 were female. All normal subjects were carefully screened prior to their inclusion for evidence of dysphagia, or medical/surgical factors that may have predisposed them to dysphagia. Only one subject in the control group, a female over the age of 65 years, was observed to aspirate and then, only on a 1‐ml bolus. Consequently, her data were included in control group comparisons to non‐aspirators and aspirators. Statistical treatments of all data considered were adjusted for age and gender.
All radiographic studies were conducted at UC Davis in accordance with the routine radiographic protocols approved by the institution. Equipment used included a properly collimated OEC Medical Systems 9800 Radiographic/Fluoroscopic unit that provided a 63 kV, 1.2 mA type output for the full field of view mode (12 in. input phosphor diameter). In accordance with a standard protocol, patients swallowed, as possible, a 1‐ml, 3‐ to 5‐ml, and 15‐ to 20‐ml liquid bolus (EZ‐PAQUE Barium Sulfate Suspension, 60%w/v; 41%w/w, E‐Z‐EM, Inc., Westbury, NY), and a 3‐ to 5‐ml paste bolus (EZ‐PAQUE Barium Sulfate Esophageal Cream, 60% w/w, E‐Z‐EM, Inc., Westbury, NY) from a spoon or cup. Following the protocol, other tasks tailored to individual patients were introduced. For purposes of this study, only data for the largest liquid bolus, 20 ml, were considered.
Timing and displacement measures for the largest bolus swallowed were obtained using techniques previously validated and described briefly here.2 Fluoroscopic studies were evaluated for the following: 1) maximum displacement of the hyoid bone (Hmax), defined as the greatest anterior‐superior excursion of the hyoid during a swallow from its position with a 1‐mL bolus held in the oral cavity (Fig. 2a); 2) maximum approximation of the hyoid and larynx during swallow (HL), defined as the difference in distance between the two structures with the 1‐ml bolus held in the oral cavity (HLhold), and when maximally approximated during the swallow (HLmax) (Fig. 2a); 3) maximum opening of the pharyngoesophageal segment (upper esophageal sphincter), defined as the narrowest point in the aerodigestive tract between cervical vertebrae four and six (in lateral view) during this area's maximum distension during the swallow (PESmax) (Fig. 2c); 4) the pharyngeal constriction ratio (PCR), defined as the ratio of the pharyngeal area (and any visible contrast material) measured in the lateral view at the point of maximum pharyngeal constriction (PAmax), to the area measured with a 1‐mL bolus held in the oral cavity (PAhold) (Fig. 2c); and 5) total pharyngeal transit time (TPT), defined as the time between the first movement of the head of the bolus past the posterior nasal spine that leads to a swallow, and the time the bolus tail clears the upper esophageal sphincter.
Figure 2.
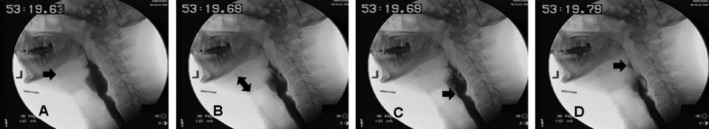
(A) maximum displacement of hyoid; (B) maximum approximation of hyoid and larynx; (C) maximum PES opening; and (D) maximum pharyngeal constriction. Positions of structures in A, B, and D are compared to their positions with a 1ml bolus held in the oral cavity (Fig. 1).
Figure 1.
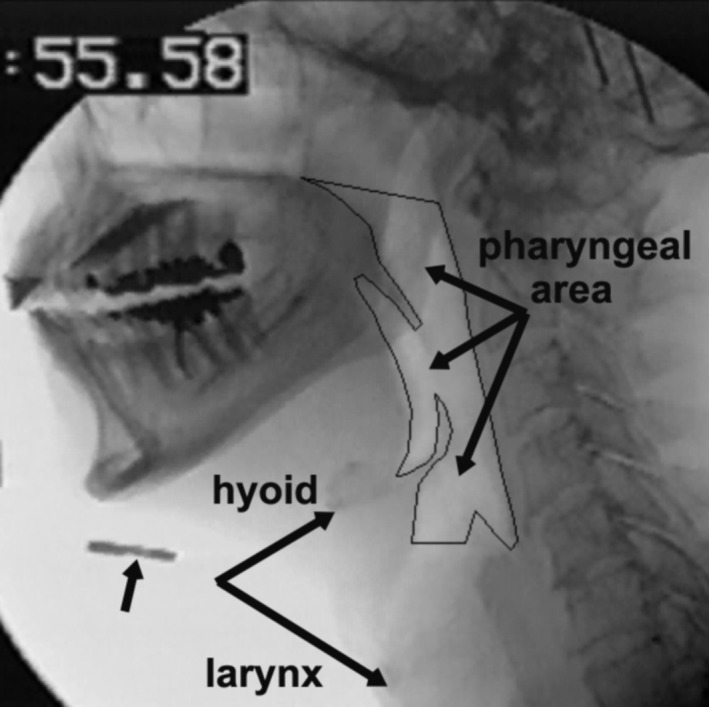
Displacement measures are referenced to position of structures with 1ml bolus held in oral cavity. Note position of hyoid, distance between hyoid and larynx, and pharyngeal area. Marker below chin, indicated by arrow, is 1.9 cm in diameter; this permits conversion of pixels to cm during measurement. Cricopharyngeus muscle at upper esophagus is tonically contracted; Pharyngoesophageal Segment (PES) is closed and not visible. Points of maximum displacement, approximation, opening and constriction are shown in Figure 2.
Displacement measures were calculated using Universal Desktop Ruler (http://avp.soft.com) and Image J software (available online from the National Institute of Mental Health, http://rsbweb.nih.gov/ij/). Timing information was determined from slow motion and frame by frame replay review of the recorded studies. Inter‐rater reliability for the measures considered has been previously established and found to be greater than 0.87 for all measures considered.2 Data for the aspirators and non‐aspirators, for the 20‐ml bolus, were compared to each other, and to normative data, for all measures noted.
All data were coded and recorded into SPSS 24 (SPSS, Inc., Chicago, IL). Data for the patient and control groups were compared with univariate analyses of variance statistical procedures for each variable, with age and gender as covariates. Post‐hoc Bonferroni adjustments were also determined for each measure. A probability of Type I error (α) = 0.05 was considered statistically significant for comparisons examined in the study. Logistic regression models including age and gender were used to classify objective measures, separately and collectively, to determine predictive capability. For each individual analysis, cutoff points were determined by the percentage of aspirators for whom data were available. Aspiration relative to maximum airway closure, ie, before (B), during (D), after (A), was also noted, and objective measures considered according to each of these variables.
RESULTS
A total of 5923 adult patients were identified who were able to take a large liquid bolus (15–20 ml). Of these patients, 3645 did not aspirate during the study and 2278 were observed to aspirate at least once during the study; 3526 patients were male and 2397 were female. Represented in this number were inpatients and outpatients reflecting a wide range of dysphagia etiologies. Among the largest categories were head and neck cancer and neurologic. A summary of major diagnoses or presenting complaints for patients is presented in Table 1.
Table 1.
Diagnoses, Presenting Complaints/Symptoms, or Immediate Findings on Fluoroscopy Study, for Patients Included in the Review.
| Diagnoses/Symptom/Complaint at Initial Evaluation | Percentage of Total Population |
|---|---|
| Dysphagia, foreign body sensation, chronic cough | 24% |
| Head and neck cancer | 22% |
| Cerebrovascular accident | 14% |
| Neuromuscular | 8% |
| Other neuro (eg, Traumatic Brain Injury, skull base tumor/surgery) | 8% |
| Cricopharyngeal bar (or web), Zenker diverticulum | 8% |
| Medical (eg, pneumonia, infectious disease, lung cancer, diabetes) | 7% |
| Trauma (eg, Motor Vehicle Accident, penetrating injury to head and neck, burn, intubation injury) | 7% |
| Other | 2% |
| TOTAL (5923 patients) | 100% |
Mechanical Measures
Results of univariate analyses of variance for the three subject groups are presented in Table 2. It is apparent that there is a general decline in function, ie, decreased displacement or constriction, increased transit time, from control subjects to non‐aspirators to aspirators, respectively. For four of the objective measures considered, Hmax, PESmax, PCR, and TPT, all group comparisons were significant (P ≤ .01). For HL, significant differences were noted between controls and aspirators (P < .001), and non‐aspirators and aspirators (P < .001), but not between controls and non‐aspirators. Cohen's effect sizes for each variable, based on t‐test comparisons for non‐aspirators and aspirators, ranged from ‐.36 (PESmax) to .76 (PCR).
Table 2.
Measures By Aspiration Category
| Measure | Aspiration Category | Mean | Std. Deviation | 95% Conf. Int. | No. Subjects | P value | Cohen's d (NonAspvs Asp) |
|---|---|---|---|---|---|---|---|
| Hyoid Displacement (Hmax) (cm) | NonAsp Asp |
1.94 | .76 | 1.91–1.96 | 2822 | <.001 | ‐.66 |
| 1.43 | .79 | 1.38–1.47 | 1022 | ||||
| Controls | 2.12 | .77 | 2.00–2.24 | 148 | |||
| Hyoid‐Larynx Approximation (HL) (cm) | NonAsp Asp |
1.21 | .58 | 1.19–1.23 | 2736 | <.001 | ‐.50 |
| .91 | .62 | .88–.95 | 1012 | ||||
| Controls | 1.27 | .58 | 1.18–1.37 | 148 | |||
| Pharyngoesophageal Segment Opening (PESmax) (cm) | NonAsp Asp |
.80 | .26 | .79–.80 | 3491 | .001 | ‐.36 |
| .70 | .29 | .67–.72 | 1155 | ||||
| Controls | .88 | .26 | .83–.92 | 148 | |||
| Pharyngeal Constriction Ratio (PCR) | NonAsp Asp |
.19 | .20 | .18–.20 | 2922 | <.001 | .75 |
| .38 | .30 | .37–.39 | 1036 | ||||
| Controls | .07 | .09 | .06–.08 | 148 | |||
| Pharyngeal Transit Time (TPT) (sec) | NonAsp Asp |
1.39 | .59 | 1.36–1.41 | 3557 | <.001 | .49 |
| 1.84 | 1.17 | 1.76–1.88 | 1180 | ||||
| Controls | 1.13 | .44 | 1.06–1.20 | 148 |
Means, standard deviations, and confidence intervals for each measure with age and gender as covariates. For all measures, significant differences are noted. It is apparent that the data for all measures reflect deterioration from control, to non‐aspirators, to aspirators, respectively. HL differed significantly between controls and aspirators (P < .001) and between aspirators and non‐aspirators (P < .001), but not between controls and non‐aspirators. All other measures differed significantly (P < .01) across the three groups. Cohen's d values were used to further compare differences between non‐aspirators and aspirators.
Presented in Table 3 are results of a classification of patients as aspirators or non‐aspirators using binary logistic regression analyses with a single objective measure, gender, and age. Highest prediction accuracy was achieved using PCR, age, and gender, with a prediction accuracy of 74.6%. All measures were significant (P < .001). With all variables combined in the analysis model, prediction accuracy improved to 76.5%. Each variable included in the combined analysis was also significant (Table 3).
Table 3.
Prediction Accuracy for Each Measure
| Variable | P‐Value | Prediction Accuracy (%) | Sensitivity (%) | Specificity (%) |
|---|---|---|---|---|
| Hyoid Displacement (Hmax) (cm) | <.001 | 69.6 | 60.6 | 72.8 |
| Hyoid‐Larynx Approximation (HL) (cm) | <.001 | 67.3 | 60.6 | 69.8 |
| Pharyngoesophageal Segment Opening (PESmax) (cm) | <.001 | 69.7 | 51.4 | 73.0 |
| Pharyngeal Constriction Ratio (PCR) | <.001 | 74.6 | 58.7 | 80.2 |
| Pharyngeal Transit Time (TPT) (secs) | <.001 | 65.9 | 59.7 | 67.9 |
| All Variables | P‐Value | Prediction Accuracy (%) | Sensitivity (%) | Specificity (%) |
|---|---|---|---|---|
| COMBINED | 76.5 | 76.5 | 65.1 | |
| Hyoid Displacement (Hmax) (cm) | <.001 | |||
| Hyoid‐Larynx Approximation (HL) (cm) | <.003 | |||
| Pharyngoesophageal Segment Opening (PESmax) (cm) | .053 | |||
| Pharyngeal Constriction Ratio (PCR) | <.001 | |||
| Pharyngeal Transit Time (TPT) (secs) | <.001 |
At top, results of binary regression analyses for individual objective measures, with age and gender as categorical covariates. At bottom, results for combined measures are presented, with age and gender as categorical variables. Cutoff point was proportion of patients who aspirated.
Odds Ratios
Odds ratios are measures of association between potential risk factors and an outcome. For the current data, the ratio represented the odds of aspiration when a mechanical measure was greater than two standard deviations from the normal mean, to the odds of aspiration when the measure was less than two standard deviations from the normal mean. Though these ratios can also be determined from regression analyses of patient data, our feeling was that relating them to normative data, controlled for age and gender, may enhance their clinical utility. As such, a value on any mechanical measure that was two standard deviations from the control group mean was considered to place a patient at risk for aspiration, again, even if aspiration was not identified during the patient's fluoroscopy study. The number of patients in each group, aspirators and non‐aspirators, who were above or below the two standard deviation referent point for each measure, was calculated. Resulting data for each measure were entered in a 2x2 Fisher's Exact contingency table and odds ratios were determined. Odds ratios for each measure are presented in Table 4. Confidence intervals and significance levels for each are also presented. Of measures considered, PCR (5.87) and Hmax (5.77) demonstrated the largest odds ratios; all Ratios were greater than 2, and all were significant at P < .01.
Table 4.
Odds Ratio for Each Measure
| Measure | Controls (148) (mean+/‐2sd) | No ASP (2800+) mean | ASP (1700+) mean | Odds Ratio (>2SD from Control Mean) (95% CI) |
|---|---|---|---|---|
| Hyoid Displacement (Hmax) (cm) | 2.12(1.5) | 1.94 | 1.43 | If < .62, OR = 5.77 (CI = 4.22–7.90) |
| Hyoid‐Larynx Approximation (HL) (cm) | 1.27(1.16) | 1.21 | .91 | If < .11, OR = 3.13 (CI = 2.09–4.67) |
| Pharyngoesophageal Segment Opening (PESmax) (cm) | .88(.52) | 0.80 | 0.70 | If < .35, OR = 2.48 (CI = 1.85–3.32) |
| Pharyngeal Constriction Ratio (PCR) | .07(.18) | 0.19 | 0.38 | If > .25, OR = 5.87 (CI = 5.08–6.83) |
| Pharyngeal Transit Time (TPT) (secs) | 1.13(.88) | 1.39 | 1.84 | If > 2.01, OR = 2.06 (CI = 1.77–2.39) |
Means ± 2 standard deviations, for each measure, are presented for the control group, non‐aspirators and aspirators. For each patient group, the number of individuals deviating more than two standard deviations from the control mean was calculated for all variables. Depending on the measure, eg, Hmax, HL, PESmax, the deviation considered was below the control mean; for TPT and \PCR, deviation more than two standard deviations above the control mean was used.
Aspiration Relative to Airway Closure
A total of 2278 patients reviewed were observed to aspirate. Time of aspiration relative to airway closure, ie, before, during, or after, was noted for all aspiration events. On the lateral view fluoroscopic image, airway closure is indicated by the most complete approximation of the arytenoid and epiglottis cartilages that closes the supraglottic airway. Aspiration that occurs before maximum airway closure is typically related to early loss of bolus material, possibly related to poor sensation, or to prolonged transit time. Aspiration that occurs during the time when the airway is maximally closed is most often related to a problem of airway protection, eg, vocal fold paralysis. Aspiration that occurs after maximum airway closure implies aspiration that occurs after the closed airway has relaxed, eg, on residue remaining after the swallow. Based on this definition, 18% of aspiration events documented in the current review occurred before (B) maximum airway closure, 6%, during (D), and 53%, after (A). 23% of patients aspirated at more than one time (Table 5).
Table 5.
Aspiration Relative to Airway Closure
| Measure | Non‐Aspirators | ASP. Before (18%) (mean, SD) | ASP. During (6%) (mean, SD) | ASP. After (53%) (mean, SD) | Sig. Diffs. by Aspiration Site (B,D,A) |
|---|---|---|---|---|---|
| Hyoid Displacement (Hmax) (cm) | 1.94 | 1.61* (.73) | 1.44* (82) | 1.45* (.83) | BxD, ns; BxA, ns; DxA, ns |
| Hyoid‐Larynx Approximation (HL) (cm) | 1.21 | 1.22 (.68) | .80*(.57) | .87* (.60) | BxD, P < .00; BxA, P < .00; DxA, ns |
| Pharyngoesophageal Segment Opening (PESmax) (cm) | .80 | .79 (.30) | .68 (.23) | .65* (.29) | BxD,ns; BxA, P < .00; DxA,ns |
| Pharyngeal Constriction Ratio (PCR) | .19 | .17 (.16) | .31* (.29) | .46* (.31) | BxD, P < .00; BxA, P < .00; DxA, P < .00 |
| Pharyngeal Transit Time (TPT) (secs) | 1.39 | 1.95* (.85) | 1.91* (.75) | 1.76* (.82) | BxD, ns; BxA, ns; DxA, ns |
Mean values of selected objective measures in non‐aspirators, and in aspirators according to time of aspiration relative to airway closure (before, during, after). Age and gender were covariates. Significant differences in each Aspirator group (B,D,A) as compared to non‐aspirators are indicated by asterisks. In the last column, differences between aspirator groups (B&D, B&A, D&A) are presented.
Mechanical Measures and Aspiration Relative to Airway Closure
Differences in objective measures between control subjects and patients who aspirated before (B), during (D), or after (A) maximum airway closure, respectively, were also determined and are presented in Table 5. Hyoid displacement (Hmax) and pharyngeal transit time (TPT) differed significantly in patients who aspirated before closure. All measures except maximum opening of the esophagus (PESmax) differed between controls and patients who aspirated during maximum airway closure, and all measures differed significantly between controls and patients who aspirated on residue, that is, after the airway relaxed post‐swallow.
DISCUSSION
Consistent with previous research,3, 4, 5, 6, 7, 8, 9, 10, 11 data from the current study support the value of objective measures in predicting aspiration risk in dysphagic patients. All variables declined from normal subjects, to non‐aspirators, to aspirators. Individual prediction accuracies ranged from 65% to 75%. For all measures, combined, prediction accuracy was 76.5%. As noted, PCR was the variable in the current review most predictive of aspiration, with an accuracy rate of 74.6% and an odds ratio of 5.87. Though the relative value of this measure is consistent with our clinical experience, it is also the case that data considered were based on a 20‐ml bolus. Larger volumes present a particular challenge for pharyngeal clearing when constriction is impaired and may help explain the substantial percentage of aspiration events related to post‐swallow residue and elevated PCR.
PCR is also dependent not only on the integrity of pharyngeal constrictor musculature and its contractile sequential activity during swallow, but on the activity of other structures. The tongue base, for example, forms the anterior wall of the constrictor complex, while the larynx plays a critical role in shortening, and thus reducing, the size of the pharynx. Further, If pharyngoesophageal segment opening is impaired, thus trapping bolus material above it, the true capability of the pharynx to constrict may be masked. This complexity likely further contributes to the significance of this measure, and its demonstrated potential for predicting aspiration.
Hmax was also associated with a substantial Odds Ratio, 5.77. Interestingly, hyoid displacement as calculated here reflects a compromise of its anterior and superior movements and was compared to normative data based on gender and approximate age (under or over 65 years). Other research has suggested that hyoid movement is more appropriately assessed when its anterior and superior movements are considered separately, and when it is normalized according to height of individuals studied.4 Our finding suggests, however, that even when the more rudimentary, and currently more expediently obtained measure is used, its potential to predict aspiration is still impressive.
Prediction accuracies for aspiration may have been even larger if not for the wide variability noted for each measure. Aspiration may not have occurred during a study, even in a patient who typically aspirated, or may have occurred and been unidentified. As noted, 53% of aspiration events were of residue remaining in the pharynx after a swallow. If the fluoroscopy unit is turned off immediately after a swallow to minimize radiation exposure, this type of aspiration can be missed. (Clinically, we attempt to avoid this consequence by turning the unit off if residue is present, waiting several seconds, and then turning it back on to see if aspirated material can be detected.) It is also the case that even a single impairment in swallow mechanics, with others remaining within normal limits, is sometimes sufficient to produce aspiration. If so, a patient categorized as an “aspirator” may have been within normal limits on most mechanical measures. The fluoroscopy study, however, is not conducted simply to identify aspiration, but also, to explain causes of dysphagia, as well as variables that may be helpful in remediating swallow impairment. Evidence of the general decline in all mechanical variables considered here, from normal to non‐aspirators, to aspirators, supports the utility of fluoroscopy for this purpose.
CONCLUSIONS
Fluoroscopy is considered a “gold standard” tool in the assessment of swallow safety and effectiveness. It is widely available (in the US), relatively inexpensive, and possible with most patients who are not bed‐restricted. A unique feature of fluoroscopy is that it permits quantification of dynamic swallow events, including structural movements and bolus transit times. Such information assists in explaining swallow impairment, but also provides evidence‐based treatment directions. Treatments considered may include rehabilitation techniques for restoring or improving critical muscle function, strategies for facilitating airway closure or bolus transit, management of bolus size or consistency to improve transit or clearance, even medical or surgical intervention. Evidence of mechanical characteristics that are intact provides additional insights into possibly useful rehabilitation strategies for safe and effective swallow.
Another value of quantitative mechanical measures, supported by the current review, is their potential to predict aspiration which, in addition to adequate nutrition, hydration, and other patient‐ and disease‐related factors, is a major concern in dysphagic patients. If we know values of measures typically associated with aspiration, then the identification of those values in patients suggests the possibility of aspiration, even when it isn't observed during the fluoroscopic study. In our experience, incorporation of this information in treatment planning has been of great utility, resulting in greater diligence in monitoring for evidence of aspiration in at‐risk patients, i.e. those with particularly fragile conditions, or multiple risk factors, and the application of strategies that would be appropriate if aspiration had been identified. Consideration of these variables relative to aspiration before, during or after airway closure is of further value, offering guidance to clinicians regarding which variables are likely to be most impaired depending on aspiration time.
The benefits of understanding swallow mechanics in dysphagic patients notwithstanding, it is also important for clinicians to consider apparent mechanical “impairments” in the context of other factors. Prolonged transit times may sometimes be an indication of increased effort in a patient who anticipates difficulty, for example, and early hyoid displacement, possibly related to caution or anticipation, will likely reduce the overall degree of displacement during the swallow. Awareness of such possibilities is important. And, of course, any consideration of swallow mechanics, and what they represent for treatment, must be in the context of the individual patient, i.e. diagnosis, prognosis, fragility. But the opportunity to assess mechanical characteristics of swallow with quantitative measures, only a few of which are considered in the current review, can add significantly to our understanding of dysphagia in individual patients. Beyond insights to treatment and assessment of risk and potential, they allow us to compare patients to normal, to other populations, and over time or treatment. Added to other diagnostic tools, they represent an extremely valuable inclusion in dysphagia assessment.
The author has no conflict of interest and no financial support to report.
BIBLIOGRAPHY
- 1. Logemann J. Evaluation and Treatment of Swallowing Disorders. San Diego: College‐Hill Press; 1983. [Google Scholar]
- 2. Leonard R and Kendall KA. Dysphagia Assessment and Treatment Planning. 4th ed. San Diego: Plural Publishing Co; 2018. [Google Scholar]
- 3. Steele CM, Cichero JA. Physiological factors related to aspiration risk: A systematic review. Dysphagia. 2014;29(3):295–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Steele CM, Bailey GL, Chau T, et al. The relationship between hyoid and laryngeal displacement and swallowing impairment. Clin Otolaryngol 2011;36(1):30–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Seo HG, Oh BM, Han TR. Swallowing kinematics and factors associated with laryngeal penetration and aspiration in stroke survivors with dysphagia. Dysphagia 2016;31(2):160–168. [DOI] [PubMed] [Google Scholar]
- 6. Choi KH, Ryu JS, Kim MY, Kang JY, Yoo SD. Kinematic analysis of dysphagia: significant parameters of aspiration related to bolus viscosity. Dysphagia 2011:26(4);392–398. [DOI] [PubMed] [Google Scholar]
- 7. Yip H, Leonard R, Belafsky PC. Can a fluoroscopic estimation of pharyngeal constriction predict aspiration? Otolaryngol Head Neck Surg 2006:135(2);215–217. [DOI] [PubMed] [Google Scholar]
- 8. Johnson ER, McKenzie SW, Sievers A. Aspiration pneumonia in stroke. Arch Phys Med Rehabil 1993:74(9);973–976. [PubMed] [Google Scholar]
- 9. Power ML, Hamdy S, Goulermas JY, Tyrrell PJ, Turnbull I, Thompson DG. Predicting aspiration after hemispheric stroke from timing measures of oropharyngeal bolus flow. Dysphagia 2009:24(3);257–264. [DOI] [PubMed] [Google Scholar]
- 10. Park T, Kim Y, Oh BM. Laryngeal closure duration during swallowing in stroke survivors with cortical or subcortical lesions. J Stroke Cerebrovasc Dis 2017;26(8):1766–1772. [DOI] [PubMed] [Google Scholar]
- 11. Lin CW, Chang YC, Chen WS, Chang K, Chang HY, Wang TG. Prolonged swallowing time in dysphagic Parkinsonism patients with aspiration pneumonia. Arch Phys Med Rehabil 2012;93(11):2080–2084. [DOI] [PubMed] [Google Scholar]


