Abstract
Objective
To analyze demographic, clinical, surgical, and audiometric factors that may affect hearing outcome following surgery for the semicircular canals (SCC).
Method
This is a retrospective case review of adults who underwent surgeries for superior SCC (SSCC), lateral SCC (LSCC), or posterior SCC (PSCC) and whose data were extracted and analyzed for factors affecting the hearing outcome in these procedures.
Results
Thirteen patients underwent surgery for SSCC, seven cases for the LSCC, one for the PSCC, and one case of combined PSCC/SSCC surgery. The mean age was 49.8 ± 12 years (21–66). There was no difference between the preoperative and postoperative pure tone average (PTA) thresholds at 0.5–3 kHz. Higher thresholds were noted at 4, 6, and 8 kHz postoperatively. Deterioration (>10 dB) in the bone‐conduction (BC) PTA was demonstrated in 3 of 22 (13.6%) cases with no significant difference in the demographic, clinical, surgical, and preoperative audiometric parameters relative to the cases without PTA BC change. A significantly larger difference in PTA BC (pre‐ vs. postoperative) was seen for males. Small effect size was noted for Air conduction (AC) PTA in males, and moderate effect size for Word Recognition Score (WRS) in surgery for the LSCC compare to SSCC.
Conclusions
SCC surgeries carry a relatively low risk of deterioration in PTA BC. High frequency thresholds should also be included in postoperative hearing outcome assessment. Cases of LSCC for intractable Meniere's disease and surgery in males carry higher risk of poor postoperative hearing outcomes.
Level of Evidence: 4
Keywords: Semicircular canals, hearing outcome, Meniere's disease, superior semicircular canal dehiscence
INTRODUCTION
While most vestibular pathologies can be managed with medical treatment and/or vestibular therapy, surgical intervention may be required in cases of intractable vertigo or rapidly progressive symptoms.1, 2, 3 In such cases, both patient and surgeon face certain decisions to correct or ablate the offending lesion, with the main goal to regain stability of the involved vestibular organ, thus allowing the central nervous system to achieve vestibular compensation.3, 4 The semi‐circular canals (SCC) are the organs of the inner ear responsible for sensing angular acceleration and are commonly involved in vestibular pathologies.3 The main operative interventions on the SCCs include: plugging and/or resurfacing of the superior SCC (SSCC) in cases of SSCC dehiscence (SSCCD), plugging the lateral SCC (LSCC) in cases of intractable Meniere's disease (MD), and plugging of the posterior SCC (PSCC) in rare cases of intractable benign paroxysmal positional vertigo (BPPV). The physiologic mechanisms so as the rationale behind these procedures was previously discussed.1, 2, 3, 5 Most of these procedures include the skeletonization of the bony labyrinth and compression of its membranous content without violating the integrity of the endolymph bearing cavity with a similar physiologic effect in any of the SCCs.3, 6 Reported improvement rates in vestibular symptoms with these procedures vary widely (33–100% for SSCCD [depending on approach and technique employed], 75% for LSCC plugging, and 100% for PSCC plugging).2, 7, 8 One of the major potential complications of SCC surgeries is sensorineural hearing loss (SNHL), presumably when the membranous labyrinth is penetrated, with documented rates of (2.2–40% for SSCCD [depending on approach and technique employed], 18% for LSCC plugging, and 0.8% for posterior SCC plugging).2, 7, 8 The objective of this study is to analyze demographic, clinical, surgical and preoperative audiometric factors that may predict the hearing outcome following surgeries of the SCC for various vestibular indications.
MATERIALS AND METHODS
Design
Retrospective review of medical records.
Subjects
An inquiry was conducted for all surgical encounters and outpatient visits associated with the procedure codes for SCC surgeries (Current Procedural Terminology [CPT]: 69905, 69910, 69801, 69802, 69979) performed in a single tertiary care referral center for the treatment of the vestibular pathologies described above between January 2010 and October 2016. Local institutional review board approval was obtained (University of Miami #20160869). All included cases were adults who had postoperative follow‐up and audiometric evaluation. Plugging of PSCC in BPPV and of LSCC in MD were kept as the last resort, and patient were offered to undergo the procedure when all other noninvasive and medical measures have failed. Exclusion criteria were: revision surgeries, multiple organs treated, prior ipsilateral ablative treatment, and insufficient surgical and/or audiometric data.
Though the main aim of the surgery was ablation or correction of vestibular pathology, we did not have quantification of the vestibular outcome (postoperatively) for all of our patients. Nevertheless, subjective reports from patients' follow‐up regarding the trend in their vestibular performance and complaints was documented.
Surgical Technique
Plugging and/or resurfacing of the SSC was performed by either transmastoid or middle fossa approaches (MFA). In one case, a combined plugging of the SSCC and PSCC was performed via transmastoid approach. In the transmastoid approach, a complete mastoidectomy was performed followed by identification of the bony labyrinth and skeletonization of the relevant SCC. Next, careful manual dissection of the skeletonized osseous labyrinth was performed, exposing the perilymph bearing cavity. The lumen of the osseous labyrinth was then plugged, compressing the membranous labyrinth with a combination of soft tissue grafts (temporalis fascia and muscle), bone pâté and bone wax. In the MFA, a standard craniotomy was performed and the dura was carefully dissected free from the petrous bone, exposing the dehiscent SSCC. The exposed canal was drilled, resurfaced and subsequently plugged in all cases.
Variables
The extracted data consisted of: demographic, clinical, surgical, and audiometric information. Demographic variables included: age, gender, and affected side. Clinical data consisted of presenting symptoms: hearing loss (HL), tinnitus, autophony, aural fullness/pressure, vertigo, dizziness, and imbalance. Surgical approach was recorded. Audiometric data consisted of preoperative and postoperative bone conduction (BC) pure tone average (PTA) thresholds (0.5, 1, 2, and 3 kHz), BC threshold at 4 kHz, air‐conduction (AC) PTA thresholds (0.5, 1, 2, and 3 kHz), AC threshold at 4, 6, and 8 kHz, presence of air bone gap (ABG; calculated as AC PTA minus BC PTA), and percentage WRS using the NU‐6 word list. The data was processed in Microsoft Excel (Microsoft, Redmond, WA), and the difference between the pre‐ and postoperative audiometric measures (ie, ▵) was calculated, to quantify the postsurgical hearing changes. Scatter plots of the baseline hearing characteristics and a posttreatment values were plotted, according to the Standardized Format for Reporting Hearing Outcome in Clinical Trials9 to determine audiometric deterioration or improvement. Audiometric deterioration was defined as decrease in BC PTA of ≥10 dB and/or decrease of ≥15% in WRS.
Statistical Analysis
The Shapiro–Wilk test was employed in order to assess the normality of the data distribution. Wilcoxon signed‐rank test was employed in order to compare the pre‐ and postoperative audiometric data (BC PTA and AC PTA, ABG, 4, 6, or 8 kHz pure tone thresholds, and WRS) which was found not to be normally distributed. The Mann‐Whitney U test was employed in order to compare demographic, clinical, surgical, and audiometric parameter differences between groups of deteriorated versus non‐deteriorated BC PTA and WRS (as defined earlier), and to compare difference (▵) between pre‐ and postoperative audiometric parameters for different demographic and surgical groups.
Due to the exploratory nature of this study our main interest was to look at the descriptive statistics (using median and interquartile range [IQR] for non‐normally distributed variables, and mean ± standard deviation for normally distributed variables). Effect size analysis was performed (using Cohen's d test after adjustments for non‐parametric data) in order to emphasizes the size of the difference that various factors is making on the hearing outcome in SCC surgeries, rather than confounding this with sample size.10, 11 This was done by comparing the difference (▵) between pre‐ and postoperative hearing parameters (BC and AC PTA, ABG, specific pure tone frequencies, and WRS) among several demographic and surgical groups (gender, ethnicity, canal operated upon, and surgical approach). We then performed a Spearman correlation coefficient test between age and the difference (▵) of each hearing parameter in order to assess the effect of age on these parameters. By convention, an effect size of 0.2 to 0.49 was considered small, 0.5 to 0.79 moderate, and > 0.8 a large effect.
SPSS 24.0 software (SPSS Inc., Chicago, IL) was used for statistical analysis. P values <.05 were considered statistically significant.
Correction for multiple testing was performed using Bonferroni correction.
RESULTS
Twenty‐two cases (21 patients, one patient had bilateral SSCCD) of SCC surgeries, between 2010 and 2016, were included in the cohort and analyzed. Additional two cases were excluded due to insufficient data. The mean age at surgery was 49.8 ± 12 years (21–66), 13 (59.1%) cases were females, the right side was operated in 12 (54.5%) cases. Mean follow‐up time was 14.1 ± 10.3 months (7–46). Thirteen cases (59.1%), underwent plugging of the SSCCD. LSCC plugging was performed for intractable Meniere disease in seven (31.8%) cases, all with functional level scale 4 or higher.12 A single case (4.5%) of PSCC for intractable BPPV was performed. One additional patient underwent plugging of both the SSCC and PSCC for intractable BPPV. Seventeen (77.3%) cases underwent transmastoid approach, MFA was utilized in five (22.7%) cases of SSCCD. Subjective resolution of the original complaint was achieved in all of the cases. No intraoperative complications occurred. Demographic, clinical and surgical data are summarized in Table 1. Preoperative symptoms, surgical approach used, and postoperative subjective outcome in cases with SSCCDS (N = 13) are summarized in Table 2. Preoperative symptoms and staging of hearing level of Meniere's disease cases (N = 7) are summarized in Table 3.12 A significant statistical deterioration was observed between the pre‐ and postoperative audiometric data at: 4 kHz AC, 6 kHz AC, and 8 kHz AC for the entire cohort (excluding cases of the PSCC [n = 2] due to their small number). When performing subgroup analysis for SSCC and LSCC plugging, significance was noted only for the SSCC plugging subgroup in 4 KHz and 6 KHz. (Table 4). No significant difference was noted between the pre‐ and postoperative BC PTA, AC PTA, 4 kHz BC thresholds, ABG, and WRS. Following Bonferroni correction for multiple testing, no significance was demonstrated between pre‐ and postoperative values. A pre‐ and a post‐treatment hearing scatter plot was constructed (Fig. 1A and B).
Table 1.
Demographic, Clinical, and Surgical Characteristics of the Cohort (N = 22).
| Characteristic | Value |
|---|---|
| Demographic | |
| Age | 49.8 ± 12 years (21–66); 95% CI 44.5–55.1 |
| Gender | Male: 9 (40.9%); Female: 13 (59.1%) |
| Side | Right: 12 (54.5%); Left: 10 (45.5%) |
| Ethnicity | White: 13 (59.1%); Non‐white, non‐black: 9 (40.9%) |
| Presenting symptoms | n (%) |
| Hearing loss | 12 (54.5%) |
| Tinnitus | 14 (63.6%) |
| Autophony | 4 (18.2%) |
| Aural fullness | 9 (40.9%) |
| Vertigo | 14 (63.6%) |
| Dizziness | 16 (72.7%) |
| Imbalance | 2 (9.1%) |
| Surgical parameters | |
| Semicircular canal operated | SSCC—13 (59.1%); LSCC—7 (31.8%); PSCC—1 (4.55%); SSCC+PSCC—1 (4.55%) |
| Surgical approach | Transmastoid: 17 (77.3%); Middle fossa: 5 (22.7%) |
CI = confidence interval; LSCC = lateral semicircular canal; PSCC = posterior semicircular canal; SSCC = superior semicircular canal.
Table 2.
Preoperative Symptoms, Aurgical Approach Used, and Postoperative Subjective Outcome in Cases With SSCCDS (N = 13).
| HL | Tinnitus | Autophony | Vertigo | Dizziness | Imbalance | Aural fullness | Aurgical approach | Postoperative subjective resolution | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | ‐ | + | ‐ | ‐ | ‐ | + | + | TMA | + |
| 2 | ‐ | + | + | ‐ | ‐ | ‐ | + | TMA | + |
| 3 | + | ‐ | + | ‐ | + | ‐ | ‐ | TMA | + |
| 4 | ‐ | ‐ | ‐ | + | ‐ | ‐ | ‐ | MFA | + |
| 5 | + | + | + | + | + | ‐ | ‐ | MFA | + |
| 6 | + | + | ‐ | + | + | ‐ | + | TMA | + |
| 7 | ‐ | + | ‐ | + | + | ‐ | ‐ | MFA | + |
| 8 | ‐ | + | + | ‐ | + | ‐ | + | TMA | + |
| 9 | + | + | ‐ | ‐ | ‐ | ‐ | + | MFA | + |
| 10 | ‐ | + | ‐ | + | + | ‐ | + | TMA | + |
| 11 | ‐ | ‐ | ‐ | ‐ | + | + | ‐ | MFA | + |
| 12 | + | + | ‐ | + | + | ‐ | ‐ | TMA | + |
| 13 | ‐ | + | ‐ | ‐ | + | ‐ | ‐ | TMA | + |
HL = hearing loss; MFA = middle fossa approach; SSCCDS = superior semicircular canal dehiscence syndrome; TMA = transmastoid approach.
Table 3.
Preoperative Symptoms and Staging of Hearing Level of Meniere's Disease Cases (N = 7).
| HL | Tinnitus | Autophony | Vertigo | Dizziness | Imbalance | Aural fullness | Initial hearing level four‐tone average (dB) stage 1–412 | |
|---|---|---|---|---|---|---|---|---|
| 1 | + | + | ‐ | + | ‐ | ‐ | ‐ | Stage 4 |
| 2 | + | ‐ | ‐ | + | + | ‐ | + | Stage 3 |
| 3 | + | ‐ | ‐ | ‐ | + | ‐ | + | Stage 2 |
| 4 | + | + | ‐ | + | + | ‐ | ‐ | Stage 2 |
| 5 | + | ‐ | ‐ | + | + | ‐ | + | Stage 2 |
| 6 | + | + | ‐ | + | + | ‐ | ‐ | Stage 4 |
| 7 | + | + | ‐ | + | + | ‐ | ‐ | Stage 3 |
HL = hearing loss.
Table 4.
Preoperative vs. Postoperative Audiometric Data of the Cohort (N = 20).
| Parameter | Preoperative (dB) Median (IQR) | Postoperative (dB) Median (IQR) | P value Wilcoxon signed‐rank test | ||||||
|---|---|---|---|---|---|---|---|---|---|
| SSCC | LSCC | SSCC+LSCC | SSCC | LSCC | SSCC+LSCC | SSCC | LSCC | SSCC+LSCC | |
| PTA BC | 12.5 (5) | 41.5 (31.6) | 18.1 (18.75) | 16 (8.8) | 60 (31.3) | 16.3 (21.9) | .22 | NS | .37 |
| 4 kHz BC | 15 (15) | 35 (55) | 20 (15) | 20 (20) | 60 (32.5) | 20 (25) | NS | NS | .58 |
| PTA AC | 17.5 (10.8) | 46.3 (35.4) | 23.8 (18.8) | 20 (11.5) | 61.3 (37.5) | 24.4 (25.9) | .16 | NS | .21 |
| 4 kHz AC | 20 (15) | 45 (35) | 20 (15) | 30 (20) | 60 (40) | 22.5 (23.8) | .03* † | NS | .01* † |
| 6 kHz AC | 20 (20) | 65 (40) | 22.5 (25) | 35 (25) | 70 (32.5) | 22.5 (30) | <.05* † | NS | .008* † |
| 8 kHz AC | 20 (15) | 70 (47.5) | 25 (40) | 35 (30) | 75 (35) | 25 (40) | NS | NS | .02* † |
| ABG | 3.8 (7.5) | 3.8 (11.9) | 3.4 (8.8) | 3.8 (7.5) | 10 (13.1) | 3.8 (8.8) | NS | NS | .73 |
| WRS | 100 (0) | 88 (34) | 100 (34) | 100 (0) | 68 (60.5) | 100 (0) | NS | NS | NS |
ABG = air‐bone gap; AC = air conduction; BC = bone conduction; IQR = interquartile range; NS = nonsignificant; PTA = pure tone average; WRS = word recognition score.
Statistically significant.
Nonsignificant following Bonferroni correction for multiple testing.
Figure 1.
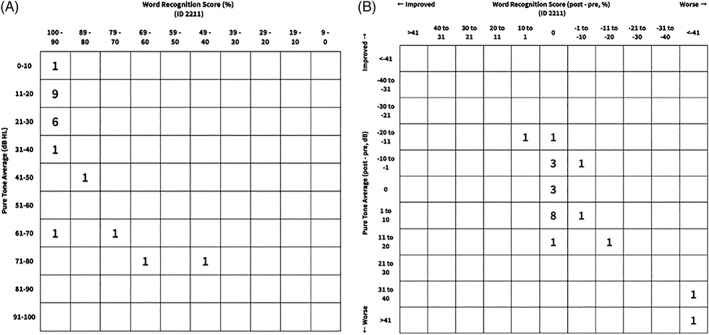
Pretreatment (A) and post‐treatment (B) audiometric scatter plot
Three out of 22 (13.6%) cases had BC PTA deterioration (≥10 dB), and three cases (13.6%) demonstrated WRS deterioration greater than 15% (only a single patient presented with both BC PTA and WRS deterioration). There were no differences in terms of age, gender, operated side, presenting symptoms, SCC operated, surgical approach, and preoperative audiometric parameters between cases with and without hearing deterioration of BC PTA and WRS. Comparison of the difference (▵) between pre‐ and postoperative audiometric parameters for different demographic and surgical groups demonstrated a significantly larger difference in BC PTA in males compared to females (median [IQR]: 6 dB [13.75] and ‐2.5 dB [12.25], respectively; P = .039; effect size 0.41 [small]). No significant difference was noted in AC PTA between males and females (7 dB [16.25] and 0 dB [13.5], respectively; P = .052; effect size 0.46 [small]). The effect size was found to be moderate when comparing the difference between the pre‐ and postoperative WRS of the LSCC compare to the SSCC (median [IQR]: ‐4% [32.1] and 0% [0], respectively; P = .2; effect size 0.64). No significant difference nor effect size was noted when comparing additional audiometric parameters between gender, ethnicity, age (using Spearman's correlation), SCC operated or operative approach (Table 5).
Table 5.
Factors Associated With Significantly Greater Difference/Relatively Larger Effect Size Between Pre‐ and Postoperative Audiometric Parameters.
| Factor | Audiometric parameter influenced | Value Median (IQR) | P value (relevant test) | Effect size |
|---|---|---|---|---|
| Gender | ▵PTA BC | Males: 6 dB (13.75) | .039* (Mann‐Whitney U Test) | 0.41 (small) |
| Females: ‐2.5 dB (12.25) | ||||
| ▵PTA AC | Males: 7 dB (16.25) | .052 (Mann‐Whitney U Test) | 0.46 (small) | |
| Females: 0 dB (13.5) | ||||
| Operated SCC | ▵WRS | LSCC: ‐4% (32.1) | .2 (Mann‐Whitney U Test) | 0.64 (moderate) |
| SSCC: 0% (0) |
AC = air conduction; BC = bone conduction; IQR = interquartile range; PTA = pure tone average; WRS = word recognition score; ▵ = difference between the pre‐ and postoperative values.
Statistically significant;
DISCUSSION
The main aim of SCC surgeries is the control of intractable vertigo following exhaustion of conservative nonsurgical measures to control these vestibular conditions. The assigned procedure should follow thorough and careful analysis regarding the involved vestibular organ and the correct side of the pathology. Hearing outcome is a critical dependent variable of these procedures, despite the fact that it is not the focus of the procedures, since the bony and membranous vestibular labyrinth are an extension of the bony and membranous cochlear labyrinth.
The present study demonstrated non‐significant differences in BC PTA and WRS (so as 4 kHz BC threshold, AC PTA, and ABG) between the pre‐ and postoperative values for the entire cohort. Similar results were demonstrated by Limb CJ et al.13 Nevertheless, significant threshold shift (which was found to be nonsignificant following Bonferroni correction for multiple testing), was noted between the pre‐ and postoperative values of 4, 6, and 8 kHz thresholds for the entire cohort and for the SSCC plugging subgroup in 4 kHz and 6 kHz thresholds. Of note, this mean threshold shifts were smaller than 10 dB in these frequencies. These changes might be attributed to high speed drilling while fenestrating the SCC due to the closer proximity of the SCC's to the basal turn of the cochlea, especially when dealing with the ampullary end of the SSCC, and can be overlooked when assessing only the PTA, ABG, and WRS following vestibular surgeries.7
Hearing deterioration in BC PTA (≥10 dB) occurred in only 3 of 22 cases (13.6%). This reinforces the relative safety of these procedures in terms of hearing outcome. No significant difference in demographic, clinical, surgical, and preoperative audiometric parameters was demonstrated between groups with and without hearing deterioration of BC PTA.
Two out of 13 cases who underwent surgery of the SSCC (15.4%) were associated with ABG deterioration. Both via middle fossa approach with resurfacing of the dehiscent SSCC, without plugging. ABG closure following surgery of SSCCD was previously demonstrated and was associated with the closure and cancelation of the “third window” effect that exist with SSCCD.7, 13, 14 ABG deterioration might be attributed to the dislodgement of the resurfaced dehiscent canal, or dural contact with the malleus head after middle fossa surgery. It is less clear why ABG deterioration occurred in additional two cases of plugging of LSCC (28.6%). The first case had preoperative ABG of 0 dB and postoperative ABG of 11 dB, while the second case had preoperative ABG of 15 dB and postoperative ABG of 40 dB. A combination of soft tissue (fascia graft) was used in all of these cases in conjunction with bone pâté and/or bone wax. Possible explanations in cases of deteriorated ABG with plugging of the LSCC is that while skeletonizing the LSCC in its ampullary end, drill contact or indirect vibratory forces led to ossicular chain disruption, or bone dust in the oval or round window, with consequent ABG deterioration. Either options can be avoided using adequate drill bit size in a low speed setting, while drilling the ampullary end of the LSCC. Another possibility with plugging of both LSCC and SSCC is inadequate plugging that either created or did not prevent the “third window” phenomenon, respectively. This can be avoided by placing fascia or gel‐foam on the fenestrated canal at the end of the procedure to prevent dislodgement of the plugging material.
Plugging of the LSCC is usually done as the last resort for patients with intractable MD, in order to decrease the frequency of vertigo attacks. Most of these patients have impaired hearing prior to the procedure. In our series, two out of seven cases (28.6%) demonstrated severe to profound hearing loss following plugging of the LSCC (with only single case [14.3%] of the two presenting initially with mild hearing loss). Similar pattern was observed by Charpiot et al.2 who demonstrated postoperative profound hearing loss in 18% of their cases and hypothesized that deafness could be induced either by a postoperative labyrinthitis or surgical injury of the ampulla which is dilated by endolymphatic hydrops, and recommended plugging the lateral canal 3 mm away from the ampulla in order to avoid injury to the membranous labyrinth. Gentine et al.15 demonstrated a 30‐dB decrease in PTA in 18% of their cases after LSCC plugging. In one of our cases of severe SNHL following plugging of the LSCC, who presented preoperatively with mild low‐frequency SNHL, a fenestration of the LSCC was performed from the ampullary end of the canal and 4 mm posteriorly. The canal was then plugged with a combination of soft tissue (fascia graft) and bone pâté. Postoperatively, the patient's vestibular symptoms resolved but a severe SNHL hearing loss was noted in the audiometric assessment. Hence, a possible explanation of the hearing loss in this case would be injury of the dilated ampulla while drilling the ampullary end of the canal.
Two other cases who underwent surgery for SSCCD were found to have postoperative significant deterioration in BC PTA without common denominator for these cases. A higher rate of postoperative SNHL was demonstrated with plugging the SSCC through the MFA7 and with plugging the SSCC in general compared to capping.16 The use of bone pâté was associated with lower rates of postoperative HL in SSCCD surgeries.17
Our study demonstrated that males have significantly larger deterioration between pre‐ and postoperative BC PTA compare to females with small effect size (small magnitude of the effect of gender on the BC PTA). Small effect size was noted for differences between pre‐ and postoperative AC PTA in males as well. No previous similar reports or anatomic studies can support or explain these findings and further investigation is warranted for clarification. Though not statistically significant, surgery of the LSCC was noted to be associated with larger differences between pre‐ and postoperative BC PTA compared to surgery for the SSCC with moderate effect size (moderate magnitude of the effect of LSCC on the postoperative BC PTA). This finding would reject and intuitive and reasonable explanation of ceiling effect in surgery of the LSCC in the already affected inner ear due to MD (Fig. 2). This finding supports previously reported data on the vulnerability of the dilated ampulla of the LSCC in patients with a natural history of endolymphatic hydrops in MD.2, 15
Figure 2.
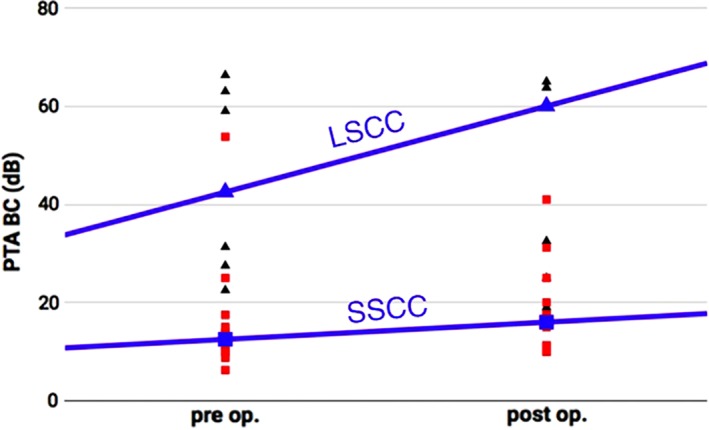
PTA BC, preoperative and postoperative trends in SSCC vs. LSCCLSCC = lateral semicircular canal; PTA BC = pure tone average bone conduction; SSCC = superior semicircular canal; Black triangle = LSCC; Red square = SSCC; Blue triangle = median values of LSCC; Blue square = median values of SSCC; Blue lines = trend lines.
There are several limitations to our study: first, this is a retrospective study with a relatively small cohort which might affect the statistical outcome, hence significant values (using conventional comparative statistical tests) should be interpreted with caution, with focus on the effect size which is describing the magnitude of the effect, regardless of sample size, hence it is more appropriate than P values for these relatively small numbers of cases.10, 11 Only two cases underwent surgeries of the PSCC (one of them in combination with the SSCC), hence it is difficult to draw conclusions on the pattern of hearing outcome for the PSCC. Our study cases presented clinically with multiple symptoms but it was not possible to assess retrospectively what were their most concerning subjective symptoms, hence it is possible that the significance of some presenting symptoms were overestimated and vice versa. Our plugging technique was consistent among the cohort cases, nevertheless it involves several materials (soft tissue, bone pâté, and bone wax) which make outcome assessment more diverse and complicated. We believe that given the uniformity of the surgical technique we were able to minimize the effect of this factor.
CONCLUSION
Surgery of the semicircular canals carries relatively low risk of hearing deterioration (BC PTA), seen in only 3 of 22 (13.6%) of our cases, with no demographic, clinical, surgical, or preoperative audiometric data differences between those affected and the remaining patients. Nevertheless, postoperative hearing thresholds were noted to be higher in the higher frequencies, which stresses the need to assess these frequencies postoperatively and avoid relying exclusively on BC PTA as a measure of hearing outcome. Drilling toward the Ampullary end of the LSCC should be done in low RPM and adequate size of the drill bit in order to minimize the risk of disruption of the ossicular chain. When operating on the LSCC for intractable MD, the patient should be counselled regarding the relatively higher risk for hearing loss following the surgery, especially for male patients.
CONFLICT OF INTEREST
The authors have no conflict of interest to disclose.
This work was presented as a poster presentation in the Combined Otolaryngology Spring Meeting, American Neurotology Society. April 26–30, 2017, San Diego, CA, U.S.A.
BIBLIOGRAPHY
- 1. Beyea JA, Sumit KA, Parnes LS. transmastoid semicircular canal occlusion: a safe and highly effectiv e treatment for benign paroxysmal positional vertigo and superior canal dehiscence. Laryngoscope 2012;122:1862–1866. [DOI] [PubMed] [Google Scholar]
- 2. Charpiot A, Rohmer D, Gentine A. lateral semicircular canal plugging in severe ménière's disease: a clinical prospective study about 28 patients. Otol Neurotol 2010;31(2):237–240. [DOI] [PubMed] [Google Scholar]
- 3. Daogong Z, Zhaomin F, Yuechen H, et al. Triple semicircular canal plugging: a novel modality for the treatment of intractable Meniere's disease. Acta Otolaryngol 2016;136(12):1230–1235. [DOI] [PubMed] [Google Scholar]
- 4. Lacombe H. Surgery for vertigo. Neurochirurgie 2009;55(2):268–271. [DOI] [PubMed] [Google Scholar]
- 5. Portmann D, Guindi S. Surgery of the semicircular canals. Rev Laryngol Otol Rhinol (Bord) 2008;129(1):3–9. [PubMed] [Google Scholar]
- 6. Goddard JC, Wilkinson EP. Outcomes following semicircular canal plugging. Otolaryngol Head Neck Surg 2014;151(3):478–483. [DOI] [PubMed] [Google Scholar]
- 7. Ziylan F, Kinaci, A , Beynon, AJ , et al. A comparison of surgical treatments for superior semicircular canal dehiscence: a systematic review. Otol Neurotol 2017;38(1):1–10. [DOI] [PubMed] [Google Scholar]
- 8. Toru S, Misako H, Naoki S, et al. Hearing and vestibular functions after plugging surgery for the posterior semicircular canal. Acta Otolaryngol 2009;129:1148–1152. [DOI] [PubMed] [Google Scholar]
- 9. Gurgel RK, Jackler RK, Dobie RA. A new standardized format for reporting hearing outcome in clinical trials. Otolaryngol Head Neck Surg 2012;147(5):803–807. [DOI] [PubMed] [Google Scholar]
- 10. Cohen J. Statistical Power Analysis for the Behavioral Sciences. New York, NY: Routledge Academic, 1988. [Google Scholar]
- 11. Omar A. Karadaghy BA, Hong Helena, et al. Reporting of effect size and confidence intervals in JAMA Otolaryngology–Head & Neck Surgery. JAMA Otolaryngol Head Neck Surg 2017;143(11):1075–1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Committee on Hearing and Equilibrium . Guidelines for the diagnosis and evaluation of therapy in Meniere's disease. Otolaryngol Head Neck Surg 1996;114:236–241. [DOI] [PubMed] [Google Scholar]
- 13. Limb CJ, Carey JP, Srireddy S, et al. Auditory function in patients with surgically treated superior semicircular canal dehiscence. Otol Neurotol 2006;27(7):969–980. [DOI] [PubMed] [Google Scholar]
- 14. Bi WL, Brewster R, Poe D, et al. Superior semicircular canal dehiscence syndrome. J Neurosurg 2017;13:1–9. [DOI] [PubMed] [Google Scholar]
- 15. Gentine A, Martin E, Schultz P, et al. Lateral semicircular canal plugging: a simple and effective surgical treatment against incapacitating Menière's disease. Rev Laryngol Otol Rhinol (Bord) 2008;129(1):11–16. [PubMed] [Google Scholar]
- 16. Gioacchini FM, Alicandri‐Ciufelli M, Kaleci S et al. Outcomes and complications in superior semicircular canal dehiscence surgery: a systematic review. Laryngoscope 2016;126(5):1218–1224. [DOI] [PubMed] [Google Scholar]
- 17. Agrawal SK, Parnes LS: Transmastoid superior semicircular canal occlusion. Otol Neurotol 2008;29:363–367. [DOI] [PubMed] [Google Scholar]


