Abstract
Background:
The survival in Iranian HIV/AIDS patients based on data from Iran National HIV/AIDS Case Registry System has not been evaluated. This study assessed the survival rates and associated factors among people living with HIV/AIDS in Iran.
Materials and Methods:
The population in this observational study included 32168 patients diagnosed with HIV/AIDS registered in Iran disease registry system between 1986 and 31 December 2015. Data until June 2016 (the cutoff date of our last data linkage) were investigated to estimate survival and related factors following HIV diagnosis.
Results:
Of registered patients, 17.7% were diagnosed at AIDS stage. By June 2016, 27.2% of study population progressed to AIDS, and 8081 (25.1%) of patients died. The survival rate was 88%, 85%, 77%, and 67% for 1, 2, 5, and 10 years, respectively. Cumulative proportion surviving was significantly lower in males than in females (P = 0.0001). A higher rate of survival was seen in female patients, who diagnosed after 2010, infected in sexual route, and had CD4 cell count more than 500, nonconfected patients with tuberculosis (TB), and those who received antiretroviral therapy (ART). Based on multivariate model, the mortality risk in female patients, those with CD4 cell count more than 500, patients who received ART, and those with TB and injection drug uses (IDUs) was higher.
Conclusion:
The survival in studied patients increased in recent time periods, and ART reduced AIDS-related mortality in these patients. The survival can be increased by focus on improvements in patient care among male patients, IDUs, and patients with TB coinfection.
Keywords: Antiretroviral therapy, HIV/AIDS, Iran, survival
INTRODUCTION
Worldwide, despite widespread efforts to control the disease, HIV/AIDS remains a serious public health challenge.[1] Based on the UNAIDS global estimation, by the end of 2016, there were 36.7 million people living with HIV, 1.0 million deaths from AIDS-related causes, and 1.8 million new HIV infections.[2]
Since the introduction of antiretroviral therapy (ART), AIDS-defining opportunistic infections and AIDS-related mortalities were decreased, and long-term survival in HIV-positive populations appears to be approaching that of the general population.[3] Studies have shown declining rates of AIDS-related death compared to non-AIDS-related death.[4,5] and describe a need for increasing focus on chronic disease management and health promotion.[6,7] This effective treatment increases survival following HIV infection from 10 to 12 years to 25 years,[8,9] and HIV infection can now be characterized as a manageable chronic condition.[10]
The accurate description of survival in HIV-positive populations today is therefore increasingly important in HIV management. The effectiveness of ART varies between countries.[11,12] However, most of the previous studies have shown that ART significantly reduced the rate of disease progression from HIV to death, but in some other studies, the discrepancy is reported in the survival rates of patients with HIV infection.[13,14]
Reporting treatment outcomes of patients enrolled in ART programs is important to demonstrate program effectiveness and justify continued funding that can help to identify opportunities for program improvement.[15] Few studies have reported survival in HIV patients in Iran, and there are no studies describing survival in total of Iranian people who lived with HIV/ADS. Therefore, the aim of the present study was to assess the 1-, 2-, 5-, and 10-year survival rate among people living with HIV/ADS based on Iran HIV/AIDS Surveillance Registry and clarify the determinants of survival rate in these patients.
MATERIALS AND METHODS
Study design and participants
This is an observational survival analysis, based on data from the Iran National HIV/AIDS Case Registry System, Centre of Communicable Disease Control, Ministry of Health and Medical Education. The study population included all patients (n = 32168) who were diagnosed and registered with HIV/AIDS in Iran between 1986 (the first diagnosed case of HIV) and 31 December 2015. The registry includes all demographic, laboratory, pharmacy, outpatient clinic visit, as well as dates of death. Data from these individuals until June 2016 (the cutoff date of our last data linkage) were investigated to estimate survival and related factors following HIV diagnosis. The study protocol was approved by the Institutional Review Board and Ethical Committee of Shiraz University of Medical Sciences (no, 11382-95).
Study variables
The demographic and clinical characteristics used in this study included; number of HIV/AIDS cases, date of HIV diagnosis (the date of positive test), age at diagnosis (patients years old at diagnosis time), gender (male and female), baseline CD4 count (cell/mm3), disease stage (HIV infection or AIDS stage), date of progression to AIDS, number of AIDS-related deaths, date of death, tuberculosis (TB) confection status, ART (the status of receive treatment in last visit), and route of transmission (injection drug use [IDU], sexual route, and blood transfusion other route). The time to event in months was the primary outcome in this study, and the time between the dates of HIV diagnosis and the date death or date of censoring was used to calculate the survival time in months.
Statistical analyses
Statistical analyses were done using SPSS software for Windows (SPSS, Inc., version 24, Chicago, IL, USA). Descriptive data are reported as mean ± standard deviation, mean (95% confidence interval [CI]) for length of life from diagnosis to death, median (interquartile range) for survival time, and number (percent) for categorical data. Chi-square test was used to assess the frequency of the disease between age groups, genders, disease stage, ART status, TB confection status, CD4 count, and route of transmission. Length of life from diagnosis to death was compared in the levels of other factors using Kruskal–Wallis test. Survival time was considered as the interval from the date of HIV/AIDS diagnosis to the date of death and was expressed in months. The Kaplan–Meier method was used to estimate cumulative survival probability, and comparisons between survival curves were performed with the log-rank test. The Cox proportional hazards regression model was applied to examine association between overall survival and the main factors. All statistical tests were two-sided and P < 0.05 was considered to be statistically significant.
RESULTS
Based on data from the national HIV/AIDS surveillance system, a total of 32168 HIV-infected patients had been identified and registered in Iran. The mean age of patients at diagnosis was 33.2 ± 9.6 years (range; newborn - 91 years). Majority of those (84.3%) were male and 15.7% were female. At the time of diagnosis, 17.7% of study population were at the AIDS stage. Progression rate to AIDS in the whole population was 27.2% (8756 patients) until the end of the follow-up period. Based on Chi-square test, the frequency of the disease progression was significantly different between both genders (26% and 45% for men and women, respectively; P < 0.0001).
By June 2016, 8081 of the 32168 (25.1%) registered cases died. The survival rate for whole population was 88%, 85%, 77%, and 67% for 1, 2, 5, and 10 years, respectively. Cumulative proportion surviving was remarkably lower in males than in females (1-, 2-, 5-, and 10-year survival rate was 87%, 83%, 75%, and 65% among men in comparison with 94%, 93%, 89%, and 83% among women, based on log-rank test).
Table 1 describes the analyses of the risk factors for death in the studied population. Age and sex were found to be risk factors with higher mortality within older patients and the male gender. The rate of mortality in HIV patients infected with TB and those with baseline CD4 count lower than 500 was higher. ART was a protective factor with lower mortality within patients who received ART. Furthermore, mortality rate in infected patients by blood transfusion routes or in IDUs was significantly higher than the other patients.
Table 1.
Risk factors associated with mortality in human immunodeficiency virus-positive individuals
| Characteristics | Frequency | Death* | Length of life from diagnosis to death (month)† | Survival time (month)†† |
|---|---|---|---|---|
| Overall | 32,168 | 7733 (25.7) | 27 (6-62) | 248.0 (244.3-251.7) |
| Age at diagnosis(year) | ||||
| ≤15 | 648 (2.39) | 102 (15.7) | 30.1 (23.2-37.0) | 253.7 (235.7-271.7) |
| 16-30 | 10,747 (39.67) | 2760 (25.7) | 46.9 (45.4-48.5) | 215.2 (211.5-219.0) |
| 31-45 | 13,613 (50.25) | 3934 (28.9) | 37.6 (36.4-38.8) | 196.0 (192.7-199.3) |
| 46-60 | 2509 (9.26) | 781 (31.1) | 26.9 (24.6-29.3) | 166.3 (160.4-172.1) |
| 61+ | 220 (0.81) | 72 (32.7) | 16.9 (10.3-23.5) | 143.6 (127.1-160.1) |
| Gender | ||||
| Male | 27,130 (84.34) | 7537 (27.8) | 39.9 (39.0-40.8) | 240.8 (236.8-244.9) |
| Female | 5038 (15.66) | 530 (10.5) | 33.0 (29.6-36.3) | 256.9 (249.5-264.3) |
| Baseline CD4 count (cell/mm3) | ||||
| <500 | 9801 (73.12) | 1964 (20.0) | 54.5 (52.5-56.4) | 214.5 (207.6-221.5) |
| ≥500 | 3603 (26.88) | 430 (11.9) | 64.6 (60.7-68.4) | 216.5 (210.1-222.8) |
| TB status | ||||
| Coinfection | 1028 (3.20) | 450 (43.8) | 56.0 (52.0-60.1) | 122.3 (115.8-128.9) |
| No TB | 31,140 (96.80) | 7617 (24.5) | 38.7 (37.8-39.6) | 251.6 (247.9-255.3) |
| ART status | ||||
| ART treatment | 9697 (32.24) | 1466 (15.1) | 55.1 (52.7-57.5) | 223.7 (214.1-233.3) |
| No treatment | 20,380(67.76) | 6266 (30.7) | 36.0 (35.1-36.9) | 243.2 (240.5-245.9) |
| Disease status | ||||
| HIV infection | 23,412 (72.78) | 6556 (28.0) | 36.8 (35.9-37.7) | 242.5 (238.5-246.6) |
| Progression to AIDS | 8756 (27.22) | 1511 (17.3) | 52.0 (49.8-54.3) | 225.1 (217.2-233.1) |
| MOT | ||||
| Injection drug use | 20,240 (69.02) | 6383 (31.5) | 40.3 (39.3-41.2) | 237.1 (234.1-240.1) |
| Sexual route | 6047 (20.62) | 774 (12.8) | 38.5 (35.4-41.5) | 239.6 (230.8-248.4) |
| Blood transfusion | 138 (0.47) | 79 (57.2) | 50.5 (40.5-60.5) | 167.1 (142.9-191.4) |
| Mother to child | 498 (1.70) | 72 (14.5) | 26.4 (18.2-34.6) | 162.6 (151.1-174.1) |
| Others | 2401 (8.19) | 421 (17.5) | 32.9 (28.9-36.9) | 203.5 (197.8-209.2) |
| Era of HIV diagnosis | ||||
| Before 1999 | 1550 (5.12) | 648 (41.8) | 72.4 (68.4-76.5) | 242.6 (234.8-250.5) |
| 2000-2009 | 17,394 (57.48) | 5723 (32.9) | 42.9 (41.9-43.9) | 143.1 (141.9-144.3) |
| ≥2010 | 11317 (37.40) | 1544 (13.6) | 13.9 (13.0-14.8) | 66.8 (66.3-67.3) |
All data except as noted are reported as number, n (%), Mean (95% CI) and Median (IQR). In some cases, numbers do not add up to totals because of missing values. *P values calculated by Chi-square test, all P <0.05, †P values calculated by Kruskal-Wallis test, all P <0.05, ††P values calculated by log-rank test, all P <0.05. AIDS=Acquired immunodeficiency syndrome; CI=Confidence interval; ART=Antiretroviral therapy; MOT=Mode of transmission; TB=Tuberculosis; HIV=Human immunodeficiency virus; IQR=Interquartile range
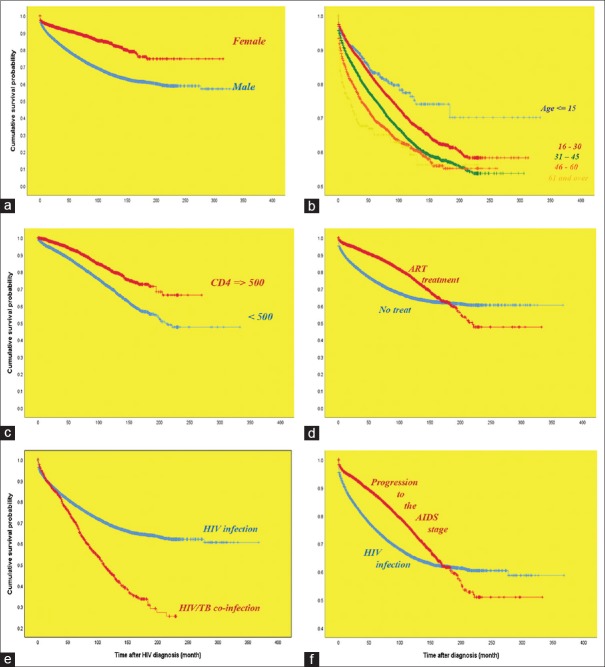
Figure 1 shows the Kaplan–Meier survival curves of all the patients and according to the mode of transmission and era of HIV diagnosis. A higher rate of survival was seen in patients infected in sexual route, and lower rate of survival was seen in IDUs and patients infected in blood transfusion route (P = 0.0001). Furthermore, the rate of survival in patients diagnosed after 2010 was significantly higher than those patients who were diagnosed between 2000 and 2009 or before 1999 (P = 0.0001).
Figure 1.
Kaplan–Meier product limits estimates for probability of survival (a) overall, (b) stratified by mode of transmission, and (c) stratified by era of HIV diagnosis
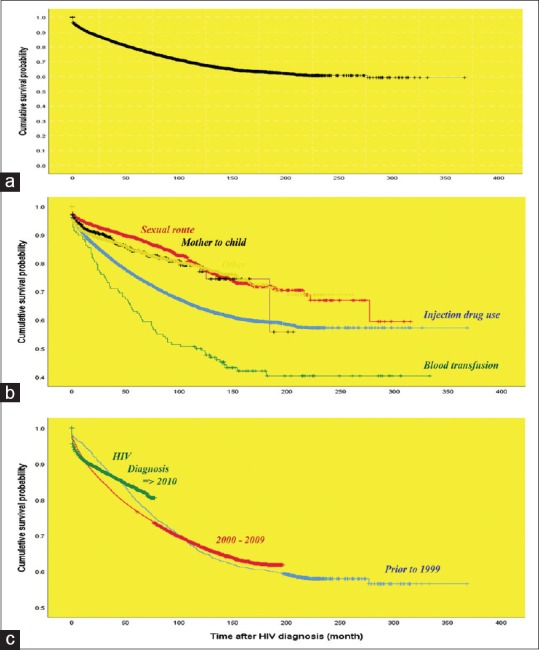
Figure 2 shows the survival analysis of studied patients according to sex, age group, CD4 cell count, ART, the presence of TB, and AIDS status. The rate of survival among females was significantly more than males. Patients in older age group had lower rate of survival than younger patients. Survival rate in patients with CD4 cell count more than 500 was significantly higher than patients with CD4 cell count lower than 500. Patients who received ART had significantly better survival than those patients that did not received ART. Furthermore, the survival rate among confected patients by TB was significantly more than nonconfected patients.
Figure 2.
Kaplan–Meier product limits estimates for probability of survival by (a) gender, (b) age at diagnosis, (c) baseline CD4 count, (d) antiretroviral treatment, (e) tuberculosis status, and (f) disease stage status
All the studied variables were statistically significant in univariate and therefore were entered in multivariable analyses. Table 2 shows the results for multivariable associations between mortality hazard and sex, age at diagnosis, CD4 cell count, AIDS diagnosis, ART, the presence of TB, and mode of transmission. The multivariate model shows a decreasing in the mortality risk in female patients (hazard ratio [HR], 0.701; 95% CI, 0.627–0.784), those with CD4 cell count more than 500 (HR, 0.046; 95% CI, 0.395–0.481), and patients who received ART (HR, 0.541; 95% CI, 0.501–0.585). In contrast, older patients at diagnosis time (HR, 1.019; 95% CI, 1.016–1.021) and those with TB (2.056; 95% CI, 1.860–2.272) were at risk of death. Furthermore, the risk of mortality in patients who infected in sexual mode was lower than IDUs, whereas mortality risk by mother-to-child mode as of transmission was increased compared to IDUs (HR, 1.699; 95% CI, 1.325–2.178).
Table 2.
Multivariate analysis of the baseline factors associated with mortality among human immunodeficiency virus-positive individuals
| Characteristics | HR | 95.0% CI | P |
|---|---|---|---|
| Sex (reference; male) | 0.701 | 0.627-0.784 | <0.0001 |
| Age at diagnosis | 1.019 | 1.016-1.021 | <0.0001 |
| CD4 count (ref; <500) | 0.436 | 0.395-0.481 | <0.0001 |
| AIDS (reference; HIV infection) | 0.823 | 0.760-0.890 | <0.0001 |
| Antiretroviral therapy | 0.541 | 0.501-0.585 | <0.0001 |
| TB | 2.056 | 1.860-2.272 | <0.0001 |
| Mode of transmission (reference; IDU) | |||
| Sexual | 0.664 | 0.605-0.729 | <0.0001 |
| Blood transfusion | 1.048 | 0.768-0.431 | 0.767 |
| Mother to child | 1.699 | 1.325-2.178 | <0.0001 |
| Others | 0.652 | 0.589-0.721 | <0.0001 |
HR=Hazard ratio; AIDS=Acquired immunodeficiency syndrome; TB=Tuberculosis, HIV=Human immunodeficiency virus; CI=Confidence interval; IDU=Injection drug use
DISCUSSION
The present study estimated the survival rate of patients with HIV/AIDS at several time intervals and related risk factors based on Iran's HIV registry system. Although like many other national surveillance systems, surveillance of communicable diseases, including AIDS, in Iran suffers from quality,[16] our results showed that from the beginning of the presence of HIV/AIDS in Iran, nearly one in four patients died, with the mean survival time of 248 months for all HIV/AIDS patients. The mortality decreased between 2000 and 2009, after the introduction of monotherapy regimens, in comparison to before 1999 period. Furthermore, after the introduction of triple therapy, mortality in HIV/AIDS patients was decreased after 2010 compared to 2000–2009 period. These findings are similar to other studies that have reported similar results in developed countries. These studies in France, Canada, Switzerland, and the United States have reported reducing mortality after the introduction of triple therapy; however, the decreased in mortality rate in these countries was higher than in our country and was occurred very sooner.[17,18,19,20] The poor ART program initiatives and low coverage of the program in Iran can explain the differences between our findings with studies in developed countries. Furthermore, studies in Asia and South Africa have shown similar results in mortality rate reduction during this period.[21,22,23] The use of earlier ART initiation and more tolerable regimens can be noted among main cause of increased survival in recent time periods.
The present study demonstrated that ART is associated with lower mortality rate, but being male, age at diagnosis, low CD4 cell count, and TB coinfection were among risk factors associated with higher mortality observed in this study. The risk of death among male patients was higher than that of the female patients, which was similar to other studies. Results of African cohorts show that male gender was independently predictive factor for mortality.[24] Other similar studies in China and Tanzania and a meta-analysis of observational studies in low- and middle-income counties reported that the risk of dying from AIDS-related diseases in male patients with HIV/AIDS was higher than that of the female patients.[24,25,26,27] The reason can be the fact that male patients have more advanced illness, fail to receive timely health-care and interventions, are more likely to drop out of the ART services system, and have poorer clinical outcomes. On the other hand, female patients have better adhere to the treatment delivered by community-based facility.
Our results show that patients who were infected with HIV through sexual route, blood transfusion, or mother to child had lower mortality than those patients infected by IDUs. This finding was similar to other studies that show higher morbidity in infected patients through IDUs than those patients infected by heterosexual transmission[25,28] or men who have sex with men.[29] This may be because of the presence of coinfection diseases such as hepatitis C and B and poor treatment among these patients, whereas poorer outcome is reported in infected patients with HIV/AIDS through IDU.[30]
We find that TB coinfection was also associated with higher risk of mortality (HR: 2.05). Studies conducted in Somali and Uganda show that relative hazard for death associated with TB were 2.30 and 1.81, respectively.[31,32] Manosuthi et al. reported that TB coinfection with HIV is a risk factor of death.[33] Some other studies have shown the similar relationship between TB coinfection with HIV and risk of death.[34,35] This can explain by the fact that the host's immune system in HIV infected patients is suppressed, which can cause to increase the virulence of the mycobacterium and much more severe immunodeficiency status in these patients.
Another risk factor in our study was lower CD4 count, where patients with a CD4 count of <500 cells/mL have a higher risk of mortality compared to those with higher CD4 count. Similar to our finding other studies show that the patients with lower CD4 count have higher risk of mortality compared to patients with lower CD4 count.[31,36,37,38] In contrast, one study shows that CD4 count was not associated with patients’ survival; however, the authors concluded that in their study, the number of patients with high CD4 was limited, and because of low statistical power of the study, they could not have found a significant association.[39]
There were limitations to our study. We used observational data from Iran National HIV/AIDS Case Registry System, and it should also be noted that missing data about CD4 cell count, retained in the ART program and other factors, could affect our results, so findings should be interpreted considering the nature of the study design. Furthermore, the survival rate estimated in our study may underestimate the real survival rate in these patients because the estimation was based on time of HIV infection diagnosis where late diagnosis can be occurred in patients who become infected years before they diagnosis time. On the other hand, the large sample size, as a strength of the study, may cause to find significance for any small relationships, and for this reason, interpretation with caution is warranted. Along with all these limitations, in consistent with the literature, our findings support ongoing improvement of HIV/AIDS control strategies in Iran.
CONCLUSION
The present study revealed that survival in Iranian HIV/AIDS patients increased in more recent time periods, and ART reduced AIDS-related mortality in these patients. Furthermore, male gender, age at diagnosis, low CD4 cell count, and TB coinfection were the risk factors associated with higher mortality and lower survival in studied population. So, improvements in patients care, increasing ART coverage, earlier ART initiation, more attention to male patients and who infected with HIV through IDU, and more attention to patients with TB confection are among strategies that can be effective in increasing patients’ survival. Further studies should explore the role of other effective factors in the survival of Iranian patient with HIV/AIDS.
Financial support and sponsorship
Nil.
Conflicts of interest
Dr. Ali-Akbar Haghdoost is the head Deputy of Strategic Planning and Coordination at Iran Ministry of Health and Medical Education, Dr. Mohammad-Mehdi Gooya is the Director General and Head of Center for Communicable Disease Control of the Ministry of Health, and Dr. Parvin Afsar-Kazerooni is the head of the National HIV/AIDS Control Committee.
Acknowledgments
The present study is a part of PhD. Thesis (Epidemiology of HIV/AIDS in Iran) written by Mojtaba Akbari under supervision of Dr. Mohamad Fararouie and was financially supported by Shiraz University of Medical Sciences, Shiraz, Iran.
REFERENCES
- 1.Pavlova-McCalla E, Trepka MJ, Ramirez G, Niyonsenga T. Socioeconomic status and survival of people with human immunodeficiency virus infection before and after the introduction of highly active antiretroviral therapy: A systematic literature review. J AIDS Clin Res. 2012;3:1–19. doi: 10.4172/2155-6113.1000163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.UNAIDS. UNAIDS DATA 2017. [Last accessed on 2018 Jun 11]. Available from: http://www. unaids.org/en/resources/documents/2017/2017_data_book .
- 3.Alencar WK, Duarte PS, Waldman EA. Survival analysis of acquired immune deficiency syndrome patients with and without hepatitis C virus infection at a reference center for sexually transmitted diseases/acquired immune deficiency syndrome in S~ao Paulo, Brazil. Braz J Infect Dis. 2014;18:150–7. doi: 10.1016/j.bjid.2013.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kee MK, Lee JH, Kim EJ, Lee J, Nam JG, Yoo BH, et al. Improvement in survival among HIV-infected individuals in the republic of Korea: Need for an early HIV diagnosis. BMC Infect Dis. 2009;9:128. doi: 10.1186/1471-2334-9-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mahy M, Stover J, Stanecki K, Stoneburner R, Tassie JM. Estimating the impact of antiretroviral therapy: Regional and global estimates of life-years gained among adults. Sex Transm Infect. 2010;86(Suppl 2):ii67–71. doi: 10.1136/sti.2010.046060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McManus H, O’Connor CC, Boyd M, Broom J, Russell D, Watson K, et al. Long-term survival in HIV positive patients with up to 15 years of antiretroviral therapy. PLoS One. 2012;7:e48839. doi: 10.1371/journal.pone.0048839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Banerjee T, Pensi T, Banerjee D, Grover G. Impact of HAART on survival, weight gain and resting energy expenditure in HIV-1-infected children in India. Ann Trop Paediatr. 2010;30:27–37. doi: 10.1179/146532810X12637745451915. [DOI] [PubMed] [Google Scholar]
- 8.Abebe N, Alemu K, Asfaw T, Abajobir AA. Survival status of hiv positive adults on antiretroviral treatment in debre markos referral hospital, Northwest Ethiopia: Retrospective cohort study. Pan Afr Med J. 2014;17:88. doi: 10.11604/pamj.2014.17.88.3262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yiannoutsos CT, Johnson LF, Boulle A, Musick BS, Gsponer T, Balestre E, et al. Estimated mortality of adult HIV-infected patients starting treatment with combination antiretroviral therapy. J Sex Transm Dis. 2012;88:i33–43. doi: 10.1136/sextrans-2012-050658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Molaeipoor L, Poorolajal J, Mohraz M, Esmailnasab N. Predictors of tuberculosis and human immunodeficiency virus co-infection: A case-control study. Epidemiol Health. 2014;36:e2014024. doi: 10.4178/epih/e2014024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moosavi S, Pokorny KL, Poorolajal J, Mahjub H. Fuzzy survival analysis of AIDS patients under ten years old in Hamadan-Iran. J Intell Fuzzy Syst. 2015;28:1385–92. [Google Scholar]
- 12.Tadesse K, Haile F, Hiruy N. Predictors of mortality among patients enrolled on antiretroviral therapy in Aksum hospital, Northern Ethiopia: A retrospective cohort study. PLoS One. 2014;9:e87392. doi: 10.1371/journal.pone.0087392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Celesia BM, Castronuovo D, Pinzone MR, Bellissimo F, Mughini MT, Lupo G, et al. Late presentation of HIV infection: Predictors of delayed diagnosis and survival in Eastern Sicily. Eur Rev Med Pharmacol Sci. 2013;17:2218–24. [PubMed] [Google Scholar]
- 14.Biadgilign S, Reda AA, Digaffe T. Predictors of mortality among HIV infected patients taking antiretroviral treatment in Ethiopia: A retrospective cohort study. AIDS Res Ther. 2012;9:15. doi: 10.1186/1742-6405-9-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dowdy DW, Geng EH, Christopoulos KA, Kahn JS, Hare CB, Wlodarczyk D, et al. Mortality among antiretroviral-eligible patients in an urban public clinic. J Acquir Immune Defic Syndr. 2011;57:297–300. doi: 10.1097/QAI.0b013e31822233aa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kazerooni PA, Fararouei M, Nejat M, Akbarpoor M, Sedaghat Z. Under-ascertainment, under-reporting and timeliness of iranian communicable disease surveillance system for zoonotic diseases. Public Health. 2018;154:130–5. doi: 10.1016/j.puhe.2017.10.029. [DOI] [PubMed] [Google Scholar]
- 17.Lima VD, Hogg RS, Harrigan PR, Moore D, Yip B, Wood E, et al. Continued improvement in survival among HIV-infected individuals with newer forms of highly active antiretroviral therapy. AIDS. 2007;21:685–92. doi: 10.1097/QAD.0b013e32802ef30c. [DOI] [PubMed] [Google Scholar]
- 18.Mouton Y, Alfandari S, Valette M, Cartier F, Dellamonica P, Humbert G, et al. Impact of protease inhibitors on AIDS defining events and hospitalizations in 10 French AIDS reference centres. Federation national des centres de lutte contre le SIDA. AIDS. 1997;11:101–5. doi: 10.1097/00002030-199712000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Egger M, Hirschel B, Francioli P, Sudre P, Wirz M, Flepp M, et al. Impact of new antiretroviral combination therapies in HIV infected patients in Switzerland: Prospective multicentre study. Swiss HIV cohort study. BMJ. 1997;315:1194–9. doi: 10.1136/bmj.315.7117.1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Walensky RP, Paltiel AD, Losina E, Mercincavage LM, Schackman BR, Sax PE, et al. The survival benefits of AIDS treatment in the United States. J Infect Dis. 2006;194:11–9. doi: 10.1086/505147. [DOI] [PubMed] [Google Scholar]
- 21.De La Mata NL, Kumarasamy N, Khol V, Ng OT, Van Nguyen K, Merati TP, et al. Improved survival in HIV treatment programmes in Asia. Antivir Ther. 2016;21:517–27. doi: 10.3851/IMP3041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cornell M, Grimsrud A, Fairall L, Fox MP, van Cutsem G, Giddy J, et al. Temporal changes in programme outcomes among adult patients initiating antiretroviral therapy across South Africa, 2002-2007. AIDS. 2010;24:2263–70. doi: 10.1097/QAD.0b013e32833d45c5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Boulle A, Van Cutsem G, Hilderbrand K, Cragg C, Abrahams M, Mathee S, et al. Seven-year experience of a primary care antiretroviral treatment programme in Khayelitsha, South Africa. AIDS. 2010;24:563–72. doi: 10.1097/QAD.0b013e328333bfb7. [DOI] [PubMed] [Google Scholar]
- 24.May M, Boulle A, Phiri S, Messou E, Myer L, Wood R, et al. Prognosis of patients with HIV-1 infection starting antiretroviral therapy in sub-saharan Africa: A collaborative analysis of scale-up programmes. Lancet. 2010;376:449–57. doi: 10.1016/S0140-6736(10)60666-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang G, Gong Y, Wang Q, Deng L, Zhang S, Liao Q, et al. Outcomes and factors associated with survival of patients with HIV/AIDS initiating antiretroviral treatment in liangshan prefecture, Southwest of China: A retrospective cohort study from 2005 to 2013. Medicine (Baltimore) 2016;95:e3969. doi: 10.1097/MD.0000000000003969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mageda K, Leyna GH, Mmbaga EJ. High initial HIV/AIDS-related mortality and-its predictors among patients on antiretroviral therapy in the Kagera region of Tanzania: A Five-year retrospective cohort study. AIDS Res Treat. 2012;2012:843598. doi: 10.1155/2012/843598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gupta A, Nadkarni G, Yang WT, Chandrasekhar A, Gupte N, Bisson GP, et al. Early mortality in adults initiating antiretroviral therapy (ART) in low-and middle-income countries (LMIC): A systematic review and meta-analysis. PLoS One. 2011;6:e28691. doi: 10.1371/journal.pone.0028691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yao ST, Duan S, Xiang LF, Ye RH, Yang YC, Li YL, et al. Survival analysis on 3103 HIV/AIDS patients receiving antiretroviral treatment in dehong prefecture, Yunnan Province. Chin J Epidemiol. 2010;31:1215–8. [PubMed] [Google Scholar]
- 29.Hall HI, McDavid K, Ling Q, Sloggett A. Determinants of progression to AIDS or death after HIV diagnosis, United States, 1996 to 2001. Ann Epidemiol. 2006;16:824–33. doi: 10.1016/j.annepidem.2006.01.009. [DOI] [PubMed] [Google Scholar]
- 30.Cescon A, Chan K, Raboud JM, Burchell AN, Forrest JI, Klein MB, et al. Significant differences in clinical outcomes between HIV-hepatitis C virus coinfected individuals with and without injection drug use history. AIDS. 2014;28:121–7. doi: 10.1097/QAD.0000000000000020. [DOI] [PubMed] [Google Scholar]
- 31.Damtew B, Mengistie B, Alemayehu T. Survival and determinants of mortality in adult HIV/Aids patients initiating antiretroviral therapy in Somali region, Eastern Ethiopia. Pan Afr Med J. 2015;22:138. doi: 10.11604/pamj.2015.22.138.4352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kigozi BK, Sumba S, Mudyope P, Namuddu B, Kalyango J, Karamagi C, et al. The effect of AIDS defining conditions on immunological recovery among patients initiating antiretroviral therapy at joint clinical research centre, Uganda. AIDS Res Ther. 2009;6:17. doi: 10.1186/1742-6405-6-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Manosuthi W, Chottanapand S, Thongyen S, Chaovavanich A, Sungkanuparph S. Survival rate and risk factors of mortality among HIV/tuberculosis-coinfected patients with and without antiretroviral therapy. J Acquir Immune Defic Syndr. 2006;43:42–6. doi: 10.1097/01.qai.0000230521.86964.86. [DOI] [PubMed] [Google Scholar]
- 34.Eyuel T, Alemayehu W. Assessment of antiretroviral treatment outcome in public hospitals, South nations nationalities and peoples region, Ethiopia. Ethiop J Health Dev. 2011;25:102–9. [Google Scholar]
- 35.Jerene D, Naess A, Lindtjørn B. Antiretroviral therapy at a district hospital in Ethiopia prevents death and tuberculosis in a cohort of HIV patients. AIDS Res Ther. 2006;3:10. doi: 10.1186/1742-6405-3-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ojikutu BO, Zheng H, Walensky RP, Lu Z, Losina E, Giddy J, et al. Predictors of mortality in patients initiating antiretroviral therapy in durban, South Africa. S Afr Med J. 2008;98:204–8. [PMC free article] [PubMed] [Google Scholar]
- 37.Sibhatu B, Ayalu AR, Tesfaye D. Predictors of mortality among HIV infected patients taking antiretroviral treatment in Ethiopia: A retrospective cohort study. AIDS Res Ther. 2012;9:15. doi: 10.1186/1742-6405-9-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Johansson KA, Robberstad B, Norheim OF. Further benefits by early start of HIV treatment in low income countries: Survival estimates of early versus deferred antiretroviral therapy. AIDS Res Ther. 2010;7:3. doi: 10.1186/1742-6405-7-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Alemu AW, Sebastián MS. Determinants of survival in adult HIV patients on antiretroviral therapy in oromiyaa, ethiopia. Glob Health Action. 2010;3:5398. doi: 10.3402/gha.v3i0.5398. [DOI] [PMC free article] [PubMed] [Google Scholar]