INTRODUCTION
The uncertainty of skin–epidural space distance in the growing child and the fear of dural puncture in a narrower epidural space is a concern while performing lumbar epidurals in children.[1] Loss of resistance (LOR) technique which is most commonly performed for identification of epidural space is a blind procedure and success depends on many anatomical variations. This may be aided by having a pre-calculated approximate distance. It has been suggested that skin–epidural distance is 1 mm/kg body weight in the lumbar region in children of various ages.[2] We aimed to correlate skin–epidural distance with age, weight, and height in children.
METHODS
We conducted a prospective cohort study in 150 American Society of Anesthesiology (ASA) I and II patients between the age group of 6 months and 16 years, receiving lumbar epidurals for infraumbilical surgeries under general anaesthesia over a period of 1 year. This study was approved by Institutional Ethics Committee. Primary outcome measure was to correlate skin–epidural space distance with weight. Secondary outcome measures were to correlate skin–epidural distance with age and height, to derive a formula to predict skin–epidural distance in children based on weight, age, and height and to test the 1mm/kg body weight formula for lumbar epidurals. Participants were enrolled during the pre-anaesthetic check (PAC) a day prior to surgery after obtaining written informed parental consent and assent in children above 7 years of age. Anthropometric measurements were done during the PAC. General anaesthesia with endotracheal intubation and monitoring was instituted as per institutional protocol. The patient was positioned left lateral with the hip and knees flexed. Under all aseptic precautions, a 20-G, 5 cm Tuohy epidural needle (Perifix® One Paed set 20. B. Braun Melsungen AG, Germany) was introduced in the lumbar region in L3-L4 or L4-L5 interspinal levels in the midline perpendicular to the skin. All blocks were given by consultants having at least 2 years experience in paediatric anaesthesia. We used saline-filled syringe with an air bubble for appreciating LOR. When LOR was detected, the Tuohy needle was marked at the point where it emerged from the skin. The distance from this point to the beginning of the aperture nearest the tip was measured and recorded as skin–epidural space distance. About 0.25% bupivacaine in appropriate dosage was injected. A successful block evidenced by absence of an increase in heart rate and blood pressure on surgical stimulation constituted the end of the study.
Due to lack of evidence of any such data in India, we considered the patient load in our tertiary care center. Hence, we studied a convenience sample of 150 consecutive children who required epidural analgesia during the study duration.
Pearson's correlation coefficient (R2) was used for correlation. Linear regression with epidural space as the dependent variable and weight, age, and height as independent variables was used to derive equations for distance of epidural space from skin. P≤ 0.05 was considered statistically significant. Analysis was done with Microsoft Excel 2007 and SPSS version 16 (SPSS Inc., Chicago, IL, USA).
RESULTS
All 150 children (98 males and 52 females) had successful blocks and were included in the analysis. No dural tap or vascular puncture occurred. Age, weight, height, and BMI distribution is depicted in Table 1. Correlation between skin–epidural space (R2) with weight [Figure 1], age, and height was 0.565, 0.632, and 0.549, respectively (P < 0.001).
Table 1.
Demographic characteristics of children
| Parameter | Mean±SD |
|---|---|
| Age (months) | 68.3±48.3 |
| Weight (kg) | 16.4±9.7 |
| Height (cm) | 104.2±27.4 |
| BMI (kg/m2) | 14.5±5.20 |
SD – Standard deviation
Figure 1.
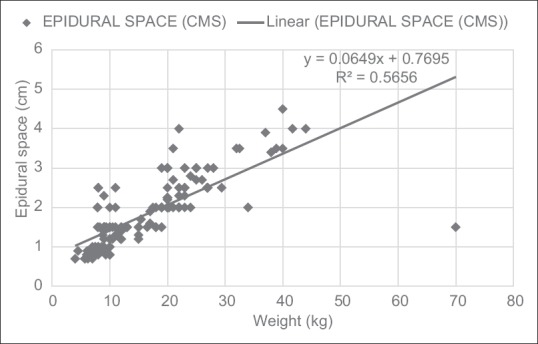
Graph showing linear correlation between skin–epidural space distance and weight. Weight in kg on x axis; skin–epidural space distance in cm on y axis. Correlation measured using Pearson's (R2) correlation coefficient. Mean weight (kg)=16.47,SE= 0.80; 95% CI = (14.90-18.05); mean epidural space (cm)=1.84,SE= 0.07; 95%CI = (1.70-1.97).
Using linear regression,
Epidural space (cm) = 0.77+ [0.0649 × weight (kg)]; P < 0.001
Epidural space (cm) = 0.892+ [0.0139 × age (months)]; P < 0.001
Epidural space (cm) = −0.532+ [0.022 × height (cm)]; P < 0.001
The combined formula derived was
Epidural space (cm) = 0.289+ [0.0301 × weight (kg)] + [0.00669 × age (months)] + [0.00571 × height (cm)].
In the age group 6 months to 10 years, 70% of children had 1mm/kg formula applicable; Cronbach's alpha = 0.865 reliability. In those older than 10 years, 85% were found to follow the rule closely; Cronbach's alpha = 0.958 reliability.
DISCUSSION
Our study showed a good positive correlation between skin- epidural distance with weight, age, and height of children. Similar results have been reported by other studies.[1,3,4,5] In the Bosenberg study, the regression equation found for weight was as follows: skin–epidural distance (mm) =0.80 weight (kg) + 3.93 (R2= 0.56). This did not apply to infants less than 6 months.[1] Because of the lower resistance offered by tissues, a caudal approach is preferred in infants.[1]
The clinician is also concerned with the closest possible depth when entry into the space might be encountered. Of particular note is an outlier at 1.5 cm in a 70 kg, 10-year-old boy and a 35 kg, 6-year-old boy where the epidural space was reached at just 2 cm [Figure 1]. There is a possibility of encountering epidural space earlier in obese children as body fat distribution may vary.
The old formula of 1 mm/kg is confirmed as a reasonable approximation in all populations to gauge the closest possible depth where entry into the epidural space might be encountered.
The distance from the point at which the needle emerged from the skin to the needle aperture was recorded. The size of the needle orifice which is approximately 2 mm should be excluded because for loss of resistance and free passage of the epidural catheter to occur, the orifice must lie beyond the ligamentum flavum.[1] This has not been defined by other studies.[3,4,5]
The complexity of the combined formula can be overcome by the use of smart phones. In case of unavailability of all parameters, individual formulae can be used. These formulae were derived when the needle was introduced perpendicular to the skin. Any angulation is likely to increase the distance.
With the advent of ultrasound, accurate real-time localization of epidural space is possible, and this technology requires further research.
CONCLUSION
Skin–epidural space distance correlated well with age, weight, and height of children.
Financial support and sponsorship
This study was supported by departmental resources.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Bosenberg AT, Gouws E. Skin-epidural distance in children. Anaesthesia. 1995;50:895–7. doi: 10.1111/j.1365-2044.1995.tb05859.x. [DOI] [PubMed] [Google Scholar]
- 2.Brown TCK, Schulte- Steinberg O. Neural blockade for pediatric surgery. In: Cousins MJ, Bridenbaugh PO, editors. Neural Blockade. 2nd ed. Philadelphia: J.B. Lippincott Co; 1988. pp. 669–92. [Google Scholar]
- 3.Hasan MA, Howard RF, Lloyd-Thomas AR. Depth of epidural space in children. Anaesthesia. 1994;49:1085–7. doi: 10.1111/j.1365-2044.1994.tb04361.x. [DOI] [PubMed] [Google Scholar]
- 4.Yamashita M, Tsuji M. Identification of the epidural space in children. Anaesthesia. 1991;46:872–4. doi: 10.1111/j.1365-2044.1991.tb09607.x. [DOI] [PubMed] [Google Scholar]
- 5.Bilić E, Bilić E, Dadić M, Boban M. Calculating lumbar puncture depth in children. Coll Antropol. 2003;27:623–6. [PubMed] [Google Scholar]


